Article processing charges
All articles published in our journals are open access and freely available online, immediately upon publication. This is made possible by an article-processing charge (APC) that covers the range of publishing services we provide. This includes provision of online tools for editors and authors, article production and hosting, liaison with abstracting and indexing services, and customer services. The APC, payable when your manuscript is editorially accepted and before publication, is charged to either you, or your funder, institution or employer.

Frequently-asked questions (FAQ)
Who is responsible for making or arranging the payment.
As the corresponding author of the manuscript you are responsible for making or arranging the payment (for instance, via your institution) upon editorial acceptance of the manuscript.
At which stage is the amount I will need to pay fixed?
The APC payable for an article will be determined from the date on which the article is accepted for publication.
When and how do I pay?
Upon editorial acceptance of an article, the corresponding author (you) will be notified that payment is due. You need to arrange payment unless a waiver has been granted, or your institution or employer is covering the cost through our Membership Program .
We advise prompt payment as we are unable to publish accepted articles until payment has been received.
Payment can be made by any of the following methods:
- Credit card - payment can be made online using a secure payment form as soon as the manuscript has been editorially accepted. We will we send a receipt by email once payment has been processed.
- Invoice - payment is due within 30 days of the manuscript receiving editorial acceptance. Receipts are available on request. Please note that payment other than by credit card carries an administrative surcharge of £50.
No taxes are included in this charge. If you are resident in any European Union country you have to add Value-Added Tax (VAT) at the rate applicable in the respective country. Institutions that are not based in the UK and are paying your fee on your behalf can have the VAT charge recorded under the EU reverse charge method, this means VAT does not need to be added to the invoice. Such institutions are required to supply us with their VAT registration number. If you are resident in Japan you have to add Japanese Consumption Tax (JCT) at the rate set by the Japanese government.
Can charges be waived if I lack funds?
Springer Nature will consider requests from authors in financial need on a case-by-case basis. For more information, please see our open access policies for journals .
Will I have to pay if my institution is a Member?
Over 500 institutions worldwide have joined our Membership Program and financially support open access by paying some or all of the APCs on behalf of their researchers. Check if your institution is a Member. If it is, you will have the option of highlighting this after editorial acceptance.
I am from a low-income country, do I have to pay an APC?
Springer Nature offers APC waivers to papers whose corresponding authors are based in countries classified by the World Bank as low-income economies. For more information, please see our publication policies .
What funding sources are available?
Many funding agencies allow the use of grants to cover APCs. An increasing number of funders and agencies strongly encourage open access publication. For more detailed information and to learn about our support service for authors, see our OA funding and policy support page .
APC waivers for substantial critiques of articles published in OA journals
Where authors are submitting a manuscript that represents a substantial critique of an article previously published in the same fully open access journal, they may apply for a waiver of the article processing charge (APC).
In order to apply for an APC waiver on these grounds, please contact the journal editorial team at the point of submission. Requests will not be considered until a manuscript has been submitted, and will be awarded at the discretion of the editor. Contact details for the journal editorial offices may be found on the journal website.
What is your APC refund policy?
Springer Nature will refund an article processing charge (APC) if an error on our part has resulted in a failure to publish an article under the open access terms selected by the authors. This may include the failure to make an article openly available on the journal platform, or publication of an article under a different Creative Commons licence from that selected by the author(s). A refund will only be offered if these errors have not been corrected within 30 days of publication.
If you become aware of an error in the open access status or licensing of your article, please contact the Global Open Research Support Team immediately ([email protected]).
APCs will not be refunded when articles are retracted as a result of author error or misconduct.
Fees and funding
Article processing charges (apc).
Authors who publish open access in BMC Medicine are required to pay an article processing charge (APC). The APC price will be determined from the date on which the article is accepted for publication.
The current APC, subject to VAT or local taxes where applicable, is: £2790.00/$3890.00/€3190.00*
*This journal is part of Springer Nature’s country-tiered APC pricing pilot. Find out more about the APC applicable to your country.
Visit our open access support portal and our Journal Pricing FAQs for further information.
Open access funding
Visit Springer Nature’s open access funding & support services for information about research funders and institutions that provide funding for APCs.
Springer Nature offers agreements that enable institutions to cover open access publishing costs. Learn more about our open access agreements to check your eligibility and discover whether this journal is included.
Requests for APC waivers and discounts from authors will be considered on a case-by-case basis, and may be granted in cases of financial need (see our open access policies for journals for more information). All applications for discretionary APC waivers and discounts should be made at the point of manuscript submission; requests made during the review process or after acceptance are unable to be considered.
- Editorial Board
- Call for papers
- Editor’s choice
- Sign up for article alerts and news from this journal
- Manuscript editing services
Annual Journal Metrics
Citation Impact 2023 Journal Impact Factor: 7.0 5-year Journal Impact Factor: 8.7 Source Normalized Impact per Paper (SNIP): 2.000 SCImago Journal Rank (SJR): 2.711 Speed 2023 Submission to first editorial decision (median days): 6 Submission to acceptance (median days): 145 Usage 2023 Downloads: 6,375,113 Altmetric mentions: 24,228
- More about our metrics
Announcements
medRxiv transfers
BMC Medicine is happy to consider manuscripts that have been, or will be, posted on a preprint server. Authors are able to submit their manuscripts directly from medRxiv , without having to re-upload files.
Registered reports
BMC Medicine is accepting Registered Reports. Find out more about this innovative format in our Submission Guidelines .
- Follow us on Twitter
BMC Medicine
ISSN: 1741-7015
- General enquiries: [email protected]
This website uses cookies to ensure you get the best experience. Learn more about DOAJ’s privacy policy.
Hide this message
You are using an outdated browser. Please upgrade your browser to improve your experience and security.
The Directory of Open Access Journals
Quick search, bmc medical research methodology this journal has been awarded the doaj seal..
1471-2288 (Online)
- ISSN Portal
Publishing with this journal
The journal charges up to:
as publication fees (article processing charges or APCs).
There is a waiver policy for these charges.
Look up the journal's:
- Aims & scope
- Instructions for authors
- Editorial Board
- Open peer review
→ This journal checks for plagiarism .
Expect on average 23 weeks from submission to publication.
Best practice
This journal began publishing in open access in 2001 . What does DOAJ define as Open Accesss?
This journal uses a CC BY or a CC0 license.
Attribution Public Domain
→ Look up their open access statement and their license terms .
The author retains unrestricted copyrights and publishing rights.
→ Learn more about their copyright policy .
Articles digitally archived in:
- A national library: British Library; National Library of the Netherlands
- A national library: Library of Congress
→ Find out about their archiving policy .
Deposit policy with:
- Sherpa/Romeo
Permanent article identifier:
Journal metadata
Publisher BMC , United Kingdom Manuscripts accepted in English
LCC subjects Look up the Library of Congress Classification Outline Medicine: Medicine (General) Keywords research methodology review methodology clinical trial methodology
WeChat QR code

BMC Medical Research Methodology
Subject Area and Category
- Epidemiology
- Health Informatics
BioMed Central Ltd
Publication type
Information.
How to publish in this journal
The set of journals have been ranked according to their SJR and divided into four equal groups, four quartiles. Q1 (green) comprises the quarter of the journals with the highest values, Q2 (yellow) the second highest values, Q3 (orange) the third highest values and Q4 (red) the lowest values.
| Category | Year | Quartile |
|---|---|---|
| Epidemiology | 2002 | Q4 |
| Epidemiology | 2003 | Q4 |
| Epidemiology | 2004 | Q3 |
| Epidemiology | 2005 | Q2 |
| Epidemiology | 2006 | Q2 |
| Epidemiology | 2007 | Q2 |
| Epidemiology | 2008 | Q2 |
| Epidemiology | 2009 | Q2 |
| Epidemiology | 2010 | Q2 |
| Epidemiology | 2011 | Q2 |
| Epidemiology | 2012 | Q2 |
| Epidemiology | 2013 | Q2 |
| Epidemiology | 2014 | Q2 |
| Epidemiology | 2015 | Q1 |
| Epidemiology | 2016 | Q1 |
| Epidemiology | 2017 | Q1 |
| Epidemiology | 2018 | Q2 |
| Epidemiology | 2019 | Q2 |
| Epidemiology | 2020 | Q2 |
| Epidemiology | 2021 | Q1 |
| Epidemiology | 2022 | Q1 |
| Epidemiology | 2023 | Q1 |
| Health Informatics | 2002 | Q3 |
| Health Informatics | 2003 | Q3 |
| Health Informatics | 2004 | Q1 |
| Health Informatics | 2005 | Q1 |
| Health Informatics | 2006 | Q1 |
| Health Informatics | 2007 | Q1 |
| Health Informatics | 2008 | Q1 |
| Health Informatics | 2009 | Q1 |
| Health Informatics | 2010 | Q1 |
| Health Informatics | 2011 | Q1 |
| Health Informatics | 2012 | Q1 |
| Health Informatics | 2013 | Q1 |
| Health Informatics | 2014 | Q1 |
| Health Informatics | 2015 | Q1 |
| Health Informatics | 2016 | Q1 |
| Health Informatics | 2017 | Q1 |
| Health Informatics | 2018 | Q1 |
| Health Informatics | 2019 | Q1 |
| Health Informatics | 2020 | Q1 |
| Health Informatics | 2021 | Q1 |
| Health Informatics | 2022 | Q1 |
| Health Informatics | 2023 | Q1 |
The SJR is a size-independent prestige indicator that ranks journals by their 'average prestige per article'. It is based on the idea that 'all citations are not created equal'. SJR is a measure of scientific influence of journals that accounts for both the number of citations received by a journal and the importance or prestige of the journals where such citations come from It measures the scientific influence of the average article in a journal, it expresses how central to the global scientific discussion an average article of the journal is.
| Year | SJR |
|---|---|
| 2002 | 0.231 |
| 2003 | 0.283 |
| 2004 | 0.728 |
| 2005 | 1.099 |
| 2006 | 1.259 |
| 2007 | 1.053 |
| 2008 | 1.458 |
| 2009 | 1.768 |
| 2010 | 1.299 |
| 2011 | 1.431 |
| 2012 | 1.417 |
| 2013 | 1.524 |
| 2014 | 1.589 |
| 2015 | 2.123 |
| 2016 | 2.577 |
| 2017 | 2.221 |
| 2018 | 1.735 |
| 2019 | 1.614 |
| 2020 | 1.820 |
| 2021 | 1.933 |
| 2022 | 1.778 |
| 2023 | 1.632 |
Evolution of the number of published documents. All types of documents are considered, including citable and non citable documents.
| Year | Documents |
|---|---|
| 2001 | 14 |
| 2002 | 15 |
| 2003 | 27 |
| 2004 | 29 |
| 2005 | 37 |
| 2006 | 58 |
| 2007 | 53 |
| 2008 | 80 |
| 2009 | 87 |
| 2010 | 113 |
| 2011 | 175 |
| 2012 | 192 |
| 2013 | 152 |
| 2014 | 138 |
| 2015 | 103 |
| 2016 | 166 |
| 2017 | 175 |
| 2018 | 177 |
| 2019 | 243 |
| 2020 | 292 |
| 2021 | 280 |
| 2022 | 335 |
| 2023 | 292 |
This indicator counts the number of citations received by documents from a journal and divides them by the total number of documents published in that journal. The chart shows the evolution of the average number of times documents published in a journal in the past two, three and four years have been cited in the current year. The two years line is equivalent to journal impact factor ™ (Thomson Reuters) metric.
| Cites per document | Year | Value |
|---|---|---|
| Cites / Doc. (4 years) | 2001 | 0.000 |
| Cites / Doc. (4 years) | 2002 | 1.286 |
| Cites / Doc. (4 years) | 2003 | 1.448 |
| Cites / Doc. (4 years) | 2004 | 1.982 |
| Cites / Doc. (4 years) | 2005 | 2.918 |
| Cites / Doc. (4 years) | 2006 | 3.417 |
| Cites / Doc. (4 years) | 2007 | 3.444 |
| Cites / Doc. (4 years) | 2008 | 3.458 |
| Cites / Doc. (4 years) | 2009 | 3.759 |
| Cites / Doc. (4 years) | 2010 | 3.845 |
| Cites / Doc. (4 years) | 2011 | 3.823 |
| Cites / Doc. (4 years) | 2012 | 3.248 |
| Cites / Doc. (4 years) | 2013 | 3.259 |
| Cites / Doc. (4 years) | 2014 | 3.367 |
| Cites / Doc. (4 years) | 2015 | 3.726 |
| Cites / Doc. (4 years) | 2016 | 4.398 |
| Cites / Doc. (4 years) | 2017 | 4.834 |
| Cites / Doc. (4 years) | 2018 | 4.541 |
| Cites / Doc. (4 years) | 2019 | 3.977 |
| Cites / Doc. (4 years) | 2020 | 4.666 |
| Cites / Doc. (4 years) | 2021 | 6.551 |
| Cites / Doc. (4 years) | 2022 | 7.288 |
| Cites / Doc. (4 years) | 2023 | 5.239 |
| Cites / Doc. (3 years) | 2001 | 0.000 |
| Cites / Doc. (3 years) | 2002 | 1.286 |
| Cites / Doc. (3 years) | 2003 | 1.448 |
| Cites / Doc. (3 years) | 2004 | 1.982 |
| Cites / Doc. (3 years) | 2005 | 2.915 |
| Cites / Doc. (3 years) | 2006 | 3.161 |
| Cites / Doc. (3 years) | 2007 | 2.565 |
| Cites / Doc. (3 years) | 2008 | 3.466 |
| Cites / Doc. (3 years) | 2009 | 3.702 |
| Cites / Doc. (3 years) | 2010 | 3.055 |
| Cites / Doc. (3 years) | 2011 | 3.361 |
| Cites / Doc. (3 years) | 2012 | 2.976 |
| Cites / Doc. (3 years) | 2013 | 2.846 |
| Cites / Doc. (3 years) | 2014 | 3.170 |
| Cites / Doc. (3 years) | 2015 | 3.627 |
| Cites / Doc. (3 years) | 2016 | 4.455 |
| Cites / Doc. (3 years) | 2017 | 4.027 |
| Cites / Doc. (3 years) | 2018 | 3.180 |
| Cites / Doc. (3 years) | 2019 | 3.544 |
| Cites / Doc. (3 years) | 2020 | 4.612 |
| Cites / Doc. (3 years) | 2021 | 6.330 |
| Cites / Doc. (3 years) | 2022 | 5.075 |
| Cites / Doc. (3 years) | 2023 | 4.462 |
| Cites / Doc. (2 years) | 2001 | 0.000 |
| Cites / Doc. (2 years) | 2002 | 1.286 |
| Cites / Doc. (2 years) | 2003 | 1.448 |
| Cites / Doc. (2 years) | 2004 | 1.786 |
| Cites / Doc. (2 years) | 2005 | 2.714 |
| Cites / Doc. (2 years) | 2006 | 2.258 |
| Cites / Doc. (2 years) | 2007 | 2.368 |
| Cites / Doc. (2 years) | 2008 | 3.378 |
| Cites / Doc. (2 years) | 2009 | 2.752 |
| Cites / Doc. (2 years) | 2010 | 2.515 |
| Cites / Doc. (2 years) | 2011 | 2.975 |
| Cites / Doc. (2 years) | 2012 | 2.559 |
| Cites / Doc. (2 years) | 2013 | 2.504 |
| Cites / Doc. (2 years) | 2014 | 2.765 |
| Cites / Doc. (2 years) | 2015 | 3.569 |
| Cites / Doc. (2 years) | 2016 | 3.747 |
| Cites / Doc. (2 years) | 2017 | 2.770 |
| Cites / Doc. (2 years) | 2018 | 2.686 |
| Cites / Doc. (2 years) | 2019 | 3.295 |
| Cites / Doc. (2 years) | 2020 | 4.181 |
| Cites / Doc. (2 years) | 2021 | 4.383 |
| Cites / Doc. (2 years) | 2022 | 4.096 |
| Cites / Doc. (2 years) | 2023 | 3.917 |
Evolution of the total number of citations and journal's self-citations received by a journal's published documents during the three previous years. Journal Self-citation is defined as the number of citation from a journal citing article to articles published by the same journal.
| Cites | Year | Value |
|---|---|---|
| Self Cites | 2001 | 0 |
| Self Cites | 2002 | 3 |
| Self Cites | 2003 | 11 |
| Self Cites | 2004 | 5 |
| Self Cites | 2005 | 10 |
| Self Cites | 2006 | 15 |
| Self Cites | 2007 | 11 |
| Self Cites | 2008 | 13 |
| Self Cites | 2009 | 31 |
| Self Cites | 2010 | 25 |
| Self Cites | 2011 | 48 |
| Self Cites | 2012 | 50 |
| Self Cites | 2013 | 51 |
| Self Cites | 2014 | 55 |
| Self Cites | 2015 | 35 |
| Self Cites | 2016 | 41 |
| Self Cites | 2017 | 60 |
| Self Cites | 2018 | 49 |
| Self Cites | 2019 | 55 |
| Self Cites | 2020 | 82 |
| Self Cites | 2021 | 109 |
| Self Cites | 2022 | 111 |
| Self Cites | 2023 | 87 |
| Total Cites | 2001 | 0 |
| Total Cites | 2002 | 18 |
| Total Cites | 2003 | 42 |
| Total Cites | 2004 | 111 |
| Total Cites | 2005 | 207 |
| Total Cites | 2006 | 294 |
| Total Cites | 2007 | 318 |
| Total Cites | 2008 | 513 |
| Total Cites | 2009 | 707 |
| Total Cites | 2010 | 672 |
| Total Cites | 2011 | 941 |
| Total Cites | 2012 | 1116 |
| Total Cites | 2013 | 1366 |
| Total Cites | 2014 | 1645 |
| Total Cites | 2015 | 1748 |
| Total Cites | 2016 | 1751 |
| Total Cites | 2017 | 1639 |
| Total Cites | 2018 | 1412 |
| Total Cites | 2019 | 1836 |
| Total Cites | 2020 | 2744 |
| Total Cites | 2021 | 4507 |
| Total Cites | 2022 | 4136 |
| Total Cites | 2023 | 4047 |
Evolution of the number of total citation per document and external citation per document (i.e. journal self-citations removed) received by a journal's published documents during the three previous years. External citations are calculated by subtracting the number of self-citations from the total number of citations received by the journal’s documents.
| Cites | Year | Value |
|---|---|---|
| External Cites per document | 2001 | 0 |
| External Cites per document | 2002 | 1.071 |
| External Cites per document | 2003 | 1.069 |
| External Cites per document | 2004 | 1.893 |
| External Cites per document | 2005 | 2.775 |
| External Cites per document | 2006 | 3.000 |
| External Cites per document | 2007 | 2.476 |
| External Cites per document | 2008 | 3.378 |
| External Cites per document | 2009 | 3.539 |
| External Cites per document | 2010 | 2.941 |
| External Cites per document | 2011 | 3.189 |
| External Cites per document | 2012 | 2.843 |
| External Cites per document | 2013 | 2.740 |
| External Cites per document | 2014 | 3.064 |
| External Cites per document | 2015 | 3.554 |
| External Cites per document | 2016 | 4.351 |
| External Cites per document | 2017 | 3.880 |
| External Cites per document | 2018 | 3.070 |
| External Cites per document | 2019 | 3.438 |
| External Cites per document | 2020 | 4.474 |
| External Cites per document | 2021 | 6.177 |
| External Cites per document | 2022 | 4.939 |
| External Cites per document | 2023 | 4.366 |
| Cites per document | 2001 | 0.000 |
| Cites per document | 2002 | 1.286 |
| Cites per document | 2003 | 1.448 |
| Cites per document | 2004 | 1.982 |
| Cites per document | 2005 | 2.915 |
| Cites per document | 2006 | 3.161 |
| Cites per document | 2007 | 2.565 |
| Cites per document | 2008 | 3.466 |
| Cites per document | 2009 | 3.702 |
| Cites per document | 2010 | 3.055 |
| Cites per document | 2011 | 3.361 |
| Cites per document | 2012 | 2.976 |
| Cites per document | 2013 | 2.846 |
| Cites per document | 2014 | 3.170 |
| Cites per document | 2015 | 3.627 |
| Cites per document | 2016 | 4.455 |
| Cites per document | 2017 | 4.027 |
| Cites per document | 2018 | 3.180 |
| Cites per document | 2019 | 3.544 |
| Cites per document | 2020 | 4.612 |
| Cites per document | 2021 | 6.330 |
| Cites per document | 2022 | 5.075 |
| Cites per document | 2023 | 4.462 |
International Collaboration accounts for the articles that have been produced by researchers from several countries. The chart shows the ratio of a journal's documents signed by researchers from more than one country; that is including more than one country address.
| Year | International Collaboration |
|---|---|
| 2001 | 28.57 |
| 2002 | 13.33 |
| 2003 | 14.81 |
| 2004 | 13.79 |
| 2005 | 29.73 |
| 2006 | 27.59 |
| 2007 | 30.19 |
| 2008 | 30.00 |
| 2009 | 22.99 |
| 2010 | 27.43 |
| 2011 | 28.00 |
| 2012 | 25.00 |
| 2013 | 29.61 |
| 2014 | 31.16 |
| 2015 | 35.92 |
| 2016 | 40.36 |
| 2017 | 26.86 |
| 2018 | 29.94 |
| 2019 | 37.04 |
| 2020 | 36.64 |
| 2021 | 42.14 |
| 2022 | 35.22 |
| 2023 | 38.70 |
Not every article in a journal is considered primary research and therefore "citable", this chart shows the ratio of a journal's articles including substantial research (research articles, conference papers and reviews) in three year windows vs. those documents other than research articles, reviews and conference papers.
| Documents | Year | Value |
|---|---|---|
| Non-citable documents | 2001 | 0 |
| Non-citable documents | 2002 | 0 |
| Non-citable documents | 2003 | 0 |
| Non-citable documents | 2004 | 0 |
| Non-citable documents | 2005 | 0 |
| Non-citable documents | 2006 | 0 |
| Non-citable documents | 2007 | 0 |
| Non-citable documents | 2008 | 0 |
| Non-citable documents | 2009 | 0 |
| Non-citable documents | 2010 | 1 |
| Non-citable documents | 2011 | 1 |
| Non-citable documents | 2012 | 1 |
| Non-citable documents | 2013 | 0 |
| Non-citable documents | 2014 | 0 |
| Non-citable documents | 2015 | 0 |
| Non-citable documents | 2016 | 0 |
| Non-citable documents | 2017 | 0 |
| Non-citable documents | 2018 | 1 |
| Non-citable documents | 2019 | 1 |
| Non-citable documents | 2020 | 1 |
| Non-citable documents | 2021 | 0 |
| Non-citable documents | 2022 | 3 |
| Non-citable documents | 2023 | 4 |
| Citable documents | 2001 | 0 |
| Citable documents | 2002 | 14 |
| Citable documents | 2003 | 29 |
| Citable documents | 2004 | 56 |
| Citable documents | 2005 | 71 |
| Citable documents | 2006 | 93 |
| Citable documents | 2007 | 124 |
| Citable documents | 2008 | 148 |
| Citable documents | 2009 | 191 |
| Citable documents | 2010 | 219 |
| Citable documents | 2011 | 279 |
| Citable documents | 2012 | 374 |
| Citable documents | 2013 | 480 |
| Citable documents | 2014 | 519 |
| Citable documents | 2015 | 482 |
| Citable documents | 2016 | 393 |
| Citable documents | 2017 | 407 |
| Citable documents | 2018 | 443 |
| Citable documents | 2019 | 517 |
| Citable documents | 2020 | 594 |
| Citable documents | 2021 | 712 |
| Citable documents | 2022 | 812 |
| Citable documents | 2023 | 903 |
Ratio of a journal's items, grouped in three years windows, that have been cited at least once vs. those not cited during the following year.
| Documents | Year | Value |
|---|---|---|
| Uncited documents | 2001 | 0 |
| Uncited documents | 2002 | 4 |
| Uncited documents | 2003 | 9 |
| Uncited documents | 2004 | 20 |
| Uncited documents | 2005 | 19 |
| Uncited documents | 2006 | 18 |
| Uncited documents | 2007 | 33 |
| Uncited documents | 2008 | 36 |
| Uncited documents | 2009 | 48 |
| Uncited documents | 2010 | 50 |
| Uncited documents | 2011 | 58 |
| Uncited documents | 2012 | 96 |
| Uncited documents | 2013 | 120 |
| Uncited documents | 2014 | 109 |
| Uncited documents | 2015 | 112 |
| Uncited documents | 2016 | 80 |
| Uncited documents | 2017 | 104 |
| Uncited documents | 2018 | 107 |
| Uncited documents | 2019 | 125 |
| Uncited documents | 2020 | 147 |
| Uncited documents | 2021 | 143 |
| Uncited documents | 2022 | 180 |
| Uncited documents | 2023 | 196 |
| Cited documents | 2001 | 0 |
| Cited documents | 2002 | 10 |
| Cited documents | 2003 | 20 |
| Cited documents | 2004 | 36 |
| Cited documents | 2005 | 52 |
| Cited documents | 2006 | 75 |
| Cited documents | 2007 | 91 |
| Cited documents | 2008 | 112 |
| Cited documents | 2009 | 143 |
| Cited documents | 2010 | 170 |
| Cited documents | 2011 | 222 |
| Cited documents | 2012 | 279 |
| Cited documents | 2013 | 360 |
| Cited documents | 2014 | 410 |
| Cited documents | 2015 | 370 |
| Cited documents | 2016 | 313 |
| Cited documents | 2017 | 303 |
| Cited documents | 2018 | 337 |
| Cited documents | 2019 | 393 |
| Cited documents | 2020 | 448 |
| Cited documents | 2021 | 569 |
| Cited documents | 2022 | 635 |
| Cited documents | 2023 | 711 |
Evolution of the percentage of female authors.
| Year | Female Percent |
|---|---|
| 2001 | 33.33 |
| 2002 | 17.95 |
| 2003 | 32.39 |
| 2004 | 40.91 |
| 2005 | 45.22 |
| 2006 | 40.54 |
| 2007 | 43.22 |
| 2008 | 42.39 |
| 2009 | 45.33 |
| 2010 | 42.88 |
| 2011 | 42.71 |
| 2012 | 42.72 |
| 2013 | 44.80 |
| 2014 | 48.68 |
| 2015 | 47.80 |
| 2016 | 53.77 |
| 2017 | 47.55 |
| 2018 | 52.69 |
| 2019 | 45.90 |
| 2020 | 49.16 |
| 2021 | 48.50 |
| 2022 | 46.00 |
| 2023 | 46.61 |
Evolution of the number of documents cited by public policy documents according to Overton database.
| Documents | Year | Value |
|---|---|---|
| Overton | 2001 | 11 |
| Overton | 2002 | 9 |
| Overton | 2003 | 10 |
| Overton | 2004 | 20 |
| Overton | 2005 | 17 |
| Overton | 2006 | 32 |
| Overton | 2007 | 22 |
| Overton | 2008 | 33 |
| Overton | 2009 | 40 |
| Overton | 2010 | 41 |
| Overton | 2011 | 55 |
| Overton | 2012 | 56 |
| Overton | 2013 | 55 |
| Overton | 2014 | 48 |
| Overton | 2015 | 32 |
| Overton | 2016 | 38 |
| Overton | 2017 | 41 |
| Overton | 2018 | 45 |
| Overton | 2019 | 48 |
| Overton | 2020 | 44 |
| Overton | 2021 | 22 |
| Overton | 2022 | 14 |
| Overton | 2023 | 1 |
Evoution of the number of documents related to Sustainable Development Goals defined by United Nations. Available from 2018 onwards.
| Documents | Year | Value |
|---|---|---|
| SDG | 2018 | 56 |
| SDG | 2019 | 84 |
| SDG | 2020 | 92 |
| SDG | 2021 | 105 |
| SDG | 2022 | 121 |
| SDG | 2023 | 104 |
Leave a comment
Name * Required
Email (will not be published) * Required
* Required Cancel
The users of Scimago Journal & Country Rank have the possibility to dialogue through comments linked to a specific journal. The purpose is to have a forum in which general doubts about the processes of publication in the journal, experiences and other issues derived from the publication of papers are resolved. For topics on particular articles, maintain the dialogue through the usual channels with your editor.
Follow us on @ScimagoJR Scimago Lab , Copyright 2007-2024. Data Source: Scopus®
Cookie settings
Cookie Policy
Legal Notice
Privacy Policy

Keep up to date with the top stories from the 60th EASD Annual Meeting with our congress hub page.
Springer Medicine
Bmc medical research methodology.

Latest issues

BMC Medical Research Methodology 1/2024

BMC Medical Research Methodology 1/2023

BMC Medical Research Methodology 1/2022

BMC Medical Research Methodology 1/2021

BMC Medical Research Methodology 1/2020

BMC Medical Research Methodology 1/2019

BMC Medical Research Methodology 1/2018

BMC Medical Research Methodology 1/2017

BMC Medical Research Methodology 1/2016

Data sharing in pharma
scroll for more
use your arrow keys for more
scroll or use arrow keys for more
About this journal
Focusing on manuscripts describing a rigorous methodological approach to healthcare research, BMC Medical Research Methodology is in the top quartile of journals publishing research on health care sciences. Peer-review is overseen by our experienced editorial board composed of active researchers who are enthusiastic about making methodology studies openly available. This journal is part of the BMC series, a research community-focused collection publishing scientifically valid studies based on community-agreed standards of questioning, methods and analysis.
- Medical Journals
- Webcasts & Webinars
- CME & eLearning
- Newsletters
- Clinical Trial Summaries
- Advances in Alzheimer’s
- About Springer Medicine
- Anesthesiology
- Dermatology
- Diabetology
- Endocrinology
- Gastroenterology
- General Medicine
- Geriatrics and Gerontology
- Infectious Disease
- Internal Medicine
- Gynecology and Obstetrics
- Psychiatry and Psychosomatics
- Respiratory Medicine
- Rheumatology
Aims and scope
BMC Methods is an open-access, peer-reviewed journal that focuses on publishing lab protocols and methodology papers in the natural sciences; including biology, chemistry, physics, computational and biomedical sciences. The journal serves as a platform for researchers to disseminate experimental procedures, novel techniques, and innovative methodologies, promoting reproducibility, transparency, and the advancement of scientific methods.
BMC Methods welcomes submissions of both lab protocols and methodology articles. We particularly welcome lab protocols that have a strong emphasis on providing comprehensive explanations for each step and robust supporting data to facilitate the wider adoption of the described methods. Submissions should address relevant questions within each discipline. Authors are encouraged to demonstrate their method's performance compared to existing approaches. BMC Methods also considers manuscripts that explore the theoretical foundations of methods and propose enhancements or optimizations. For lab protocols, we welcome detailed step-by-step procedures.
Please note that study protocols are not within the journal's scope but are considered in the main medical and veterinary subject-specific BMC Series journals.
Articles on the methodology of epidemiological research, clinical trials and meta-analysis/systematic review, and empirical studies of the associations between choice of methodology and study outcomes are considered at BMC Medical Research Methodology.
The journal considers manuscripts in the following broad subject-specific sections:
- Molecular biology
- Genomic and transcriptomic
- Metabolomics and lipidomics
- Microscopy and imaging
- Genome editing
- Model systems and organisms
- Computational biology and bioinformatics
- Structural Biology
- Plant biology, ecology and evolution
- Tissue engineering and regenerative medicine
Open access
All articles published by BMC Methods are made freely and permanently accessible online immediately upon publication, without subscription charges or registration barriers. Further information about open access can be found here .
As authors of articles published in BMC Methods you are the copyright holders of your article and have granted to any third party, in advance and in perpetuity, the right to use, reproduce or disseminate your article, according to the BMC license agreement .
For those of you who are US government employees or are prevented from being copyright holders for similar reasons, BMC can accommodate non-standard copyright lines. Please contact us if further information is needed.
Article processing charges (APC)
Authors who publish open access in BMC Methods are required to pay an article processing charge (APC). The APC price will be determined from the date on which the article is accepted for publication.
The current APC, subject to VAT or local taxes where applicable, is: £0.00/$0.00/€0.00
Visit our open access support portal and our Journal Pricing FAQs for further information.
Open access funding
Visit Springer Nature’s open access funding & support services for information about research funders and institutions that provide funding for APCs.
Springer Nature offers agreements that enable institutions to cover open access publishing costs. Learn more about our open access agreements to check your eligibility and discover whether this journal is included.
Springer Nature offers APC waivers and discounts for articles published in our fully open access journals whose corresponding authors are based in the world’s lowest income countries (see our APC waivers and discounts policy for further information). Requests for APC waivers and discounts from other authors will be considered on a case-by-case basis, and may be granted in cases of financial need (see our open access policies for journals for more information). All applications for discretionary APC waivers and discounts should be made at the point of manuscript submission; requests made during the review process or after acceptance are unable to be considered.
Peer-review policy
Peer-review is the system used to assess the quality of a manuscript before it is published. Independent researchers in the relevant research area assess submitted manuscripts for originality, validity and significance to help editors determine whether the manuscript should be published in their journal. You can read more about the peer-review process here .
Editorial policies
All manuscripts submitted to BMC Methods should adhere to BMC's editorial policies .
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appeals and complaints
Authors who wish to appeal a rejection or make a complaint should follow the procedure outlined in the BMC Editorial Policies .
Benefits of publishing with BMC
High visibility.
BMC Methods 's open access policy allows maximum visibility of articles published in the journal as they are available to a wide, global audience.
Speed of publication
BMC Methods offers a fast publication schedule whilst maintaining rigorous peer review; all articles must be submitted online, and peer review is managed fully electronically (articles are distributed in PDF form, which is automatically generated from the submitted files). Articles will be published with their final citation after acceptance, in both fully browsable web form, and as a formatted PDF.
Flexibility
Online publication in BMC Methods gives you the opportunity to publish large datasets, large numbers of color illustrations and moving pictures, to display data in a form that can be read directly by other software packages so as to allow readers to manipulate the data for themselves, and to create all relevant links (for example, to PubMed , to sequence and other databases, and to other articles).
Promotion and press coverage
Articles published in BMC Methods are included in article alerts and regular email updates. Some may be highlighted on BMC Methods ’s pages and on the BMC homepage.
In addition, articles published in BMC Methods may be promoted by press releases to the general or scientific press. These activities increase the exposure and number of accesses for articles published in BMC Methods . A list of articles recently press-released by journals published by BMC is available here .
As an author of an article published in BMC Methods you retain the copyright of your article and you are free to reproduce and disseminate your work (for further details, see the BMC license agreement ).
For further information about the advantages of publishing in a journal from BMC, please click here .
In partnership with:

BMC Methods works in partnership with protocols.io .
Discover more here .
Important information
For authors
For editorial board members
For reviewers
- Editorial Board
- Manuscript editing services
BMC Methods
ISSN: 3004-8729
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Sustaining the Knowledge Commons / Soutenir les savoirs communs
Open access scholarship / littérature savante en libre accès, biomed central in 2019: sharp increase in article processing charge.
by Hamid Pashaei and Heather Morrison
Update May 1, 2019:
Based on an inquiry from Christopher Pym from Springer Nature (owner of BioMedCentral) on the Global Open Access List I (Heather) have re-calculated the observed BMC pricing changes from 2018 – 2019, in GBP rather than USD. BMC reports pricing in 3 currencies (a common practice for large publishers). We use GBP for historical purposes. In brief, this re-analysis confirms our original finding of a sharp increase in APCs. 66% of BMC journals for which we have APC data in GBP for both 2018 and 2019 have increased their APCs; 61% have increased their APCs at far beyond inflationary levels, causing the overall average (including journals that did not change APCs or lowered APCs) to increase by 15%, a rate far beyond inflationary levels. We thank Christopher Pym for his interest in our research.
We have APC data for both 2018 and 2019 for 260 BMC journals. The average APC for these journals was 1,416 GBP in 2018, 1,555 GBP in 2019, an average increase of 139 GBP or an average 9% increase. The pricing changes are more complex, however, as some BMC journals have maintained or lowered their prices. In USD (using XE currency converter May 1, 2019), the average APC for these journals rose from 1,852 USD to 2,034 USD, an increase of 181 USD (note rounding error of $1).
Of the 260 BMC journals for which we have 2018 and 2018 APCs:
- 172 (66%) increased in price
- 55 (21%) maintained the same price
- 33 (13%) decreased in price
Of the journals that increased in price, the range of percentage increase was from under 1% to 55%. 158 journals (61% of all journals) had APC price increases clearly beyond inflationary levels, ranging from 7% – 55%.
Because of this challenge, I have re-downloaded the BMC APC list from https://www.biomedcentral.com/getpublished/article-processing-charges/biomedcentral-prices and checked GBP pricing for several journals, finding no difference from our data gathering date of April 4.
On the basis of this selective re-analysis of 260 BMC journals for which we have price data I conclude that the average APC price increase for BMC journals is 15%, (factoring in journals that did not change APC or lowered APC), a rate far above inflation, and that the majority of BMC journals (61%) increased their APCs. This confirms our original findings of a sharp APC increase for BMC in 2019. Please note that this re-analysis using the same basic dataset but slightly different methods. The re-analysis is limited to journals for which we have data in both 2018 and 2019, and is limited to GBP. When new journals and journals no longer published by BMC are factored in, this changes the averages; there can also be differences in findings based on which currency is selected for analysis.
A list of BMC APCs in GBP in 2018 and 2019 follows, in order by percentage change (highest price increase first).
| Journal Title | 2019 APC (GBP) | 2018 APC (GBP) | 2019-2018 change in GBP (amount) | 2019 – 2018 change in GBP (percentage) |
| Tropical Medicine and Health | 1570 | 705 | 865 | 55% |
| Molecular Cancer | 2490 | 1,470 | 1,020 | 41% |
| Acta Neuropathologica Communications | 1570 | 950 | 620 | 39% |
| Particle and Fibre Toxicology | 2170 | 1,370 | 800 | 37% |
| Molecular Autism | 2170 | 1,370 | 800 | 37% |
| Journal of Experimental & Clinical Cancer Research | 2290 | 1,470 | 820 | 36% |
| Journal of Hematology & Oncology | 2490 | 1,650 | 840 | 34% |
| BMC Pulmonary Medicine | 1990 | 1,370 | 620 | 31% |
| Immunity & Ageing | 1990 | 1,370 | 620 | 31% |
| Journal of Translational Medicine | 1990 | 1,370 | 620 | 31% |
| World Journal of Emergency Surgery | 1990 | 1,370 | 620 | 31% |
| Cardiovascular Diabetology | 2170 | 1,540 | 630 | 29% |
| Journal of Nanobiotechnology | 1870 | 1,370 | 500 | 27% |
| Pediatric Rheumatology | 1870 | 1,370 | 500 | 27% |
| Cell Division | 1990 | 1,470 | 520 | 26% |
| Genome Medicine | 2570 | 1,900 | 670 | 26% |
| BMC Veterinary Research | 1570 | 1,165 | 405 | 26% |
| Annals of Clinical Microbiology and Antimicrobials | 1790 | 1,370 | 420 | 23% |
| Behavioral and Brain Functions | 1790 | 1,370 | 420 | 23% |
| Cardiovascular Ultrasound | 1790 | 1,370 | 420 | 23% |
| Cell Communication and Signaling | 1790 | 1,370 | 420 | 23% |
| Diagnostic Pathology | 1790 | 1,370 | 420 | 23% |
| Genes & Nutrition | 1790 | 1,370 | 420 | 23% |
| Molecular Cytogenetics | 1790 | 1,370 | 420 | 23% |
| Reproductive Health | 1790 | 1,370 | 420 | 23% |
| Theoretical Biology and Medical Modelling | 1790 | 1,370 | 420 | 23% |
| Antimicrobial Resistance and Infection Control | 1790 | 1,370 | 420 | 23% |
| International Journal of Pediatric Endocrinology | 1790 | 1,370 | 420 | 23% |
| Thyroid Research | 1790 | 1,370 | 420 | 23% |
| Clinical Epigenetics | 2040 | 1,565 | 475 | 23% |
| Retrovirology | 1990 | 1,565 | 425 | 21% |
| Journal of Physiological Anthropology | 1270 | 1,000 | 270 | 21% |
| Journal of NeuroEngineering and Rehabilitation | 1790 | 1,430 | 360 | 20% |
| Nutrition & Metabolism | 1790 | 1,430 | 360 | 20% |
| BMC Complementary and Alternative Medicine | 1690 | 1,370 | 320 | 19% |
| BMC Geriatrics | 1690 | 1,370 | 320 | 19% |
| BMC Medical Research Methodology | 1690 | 1,370 | 320 | 19% |
| BMC Musculoskeletal Disorders | 1690 | 1,370 | 320 | 19% |
| BMC Neurology | 1690 | 1,370 | 320 | 19% |
| Child and Adolescent Psychiatry and Mental Health | 1690 | 1,370 | 320 | 19% |
| Clinical Sarcoma Research | 1690 | 1,370 | 320 | 19% |
| Conflict and Health | 1690 | 1,370 | 320 | 19% |
| Fluids and Barriers of the CNS | 1690 | 1,370 | 320 | 19% |
| Globalization and Health | 1690 | 1,370 | 320 | 19% |
| Head & Face Medicine | 1690 | 1,370 | 320 | 19% |
| International Breastfeeding Journal | 1690 | 1,370 | 320 | 19% |
| International Journal of Health Geographics | 1690 | 1,370 | 320 | 19% |
| Microbial Cell Factories | 1690 | 1,370 | 320 | 19% |
| Neural Development | 1690 | 1,370 | 320 | 19% |
| Patient Safety in Surgery | 1690 | 1,370 | 320 | 19% |
| Radiation Oncology | 1690 | 1,370 | 320 | 19% |
| Reproductive Biology and Endocrinology | 1690 | 1,370 | 320 | 19% |
| Substance Abuse Treatment, Prevention, and Policy | 1690 | 1,370 | 320 | 19% |
| Virology Journal | 1690 | 1,370 | 320 | 19% |
| Hereditary Cancer in Clinical Practice | 1690 | 1,370 | 320 | 19% |
| Journal of Ovarian Research | 1690 | 1,370 | 320 | 19% |
| Breast Cancer Research | 2290 | 1,860 | 430 | 19% |
| Genome Biology | 2380 | 1,950 | 430 | 18% |
| Cancer Cell International | 1790 | 1,470 | 320 | 18% |
| Journal of Inflammation | 1790 | 1,470 | 320 | 18% |
| Journal of Cardiothoracic Surgery | 1690 | 1,390 | 300 | 18% |
| Stem Cell Research & Therapy | 1690 | 1,390 | 300 | 18% |
| BMC Research Notes | 990 | 825 | 165 | 17% |
| Biological Procedures Online | 1870 | 1,565 | 305 | 16% |
| Biotechnology for Biofuels | 1870 | 1,565 | 305 | 16% |
| Human Genomics | 1870 | 1,565 | 305 | 16% |
| Microbiome | 1870 | 1,565 | 305 | 16% |
| International Journal for Equity in Health | 1690 | 1,420 | 270 | 16% |
| Alzheimer’s Research & Therapy | 1650 | 1,390 | 260 | 16% |
| Nutrition Journal | 1790 | 1,510 | 280 | 16% |
| Journal of Occupational Medicine and Toxicology | 1690 | 1,445 | 245 | 14% |
| Gut Pathogens | 1790 | 1,540 | 250 | 14% |
| Orphanet Journal of Rare Diseases | 1790 | 1,540 | 250 | 14% |
| BMC Cancer | 1590 | 1,370 | 220 | 14% |
| BMC Health Services Research | 1590 | 1,370 | 220 | 14% |
| BMC Public Health | 1590 | 1,370 | 220 | 14% |
| BMC Medicine | 2170 | 1,880 | 290 | 13% |
| AIDS Research and Therapy | 1690 | 1,470 | 220 | 13% |
| Biomarker Research | 1690 | 1,470 | 220 | 13% |
| Archives of Public Health | 1570 | 1,370 | 200 | 13% |
| Basic and Clinical Andrology | 1570 | 1,370 | 200 | 13% |
| BMC Anesthesiology | 1570 | 1,370 | 200 | 13% |
| BMC Biotechnology | 1570 | 1,370 | 200 | 13% |
| BMC Cardiovascular Disorders | 1570 | 1,370 | 200 | 13% |
| BMC Evolutionary Biology | 1570 | 1,370 | 200 | 13% |
| BMC Gastroenterology | 1570 | 1,370 | 200 | 13% |
| BMC International Health and Human Rights | 1570 | 1,370 | 200 | 13% |
| BMC Medical Genetics | 1570 | 1,370 | 200 | 13% |
| BMC Medical Imaging | 1570 | 1,370 | 200 | 13% |
| BMC Medical Informatics and Decision Making | 1570 | 1,370 | 200 | 13% |
| BMC Microbiology | 1570 | 1,370 | 200 | 13% |
| BMC Palliative Care | 1570 | 1,370 | 200 | 13% |
| BMC Pediatrics | 1570 | 1,370 | 200 | 13% |
| BMC Pharmacology and Toxicology | 1570 | 1,370 | 200 | 13% |
| BMC Psychiatry | 1570 | 1,370 | 200 | 13% |
| BMC Sports Science, Medicine and Rehabilitation | 1570 | 1,370 | 200 | 13% |
| BMC Surgery | 1570 | 1,370 | 200 | 13% |
| BMC Systems Biology | 1570 | 1,370 | 200 | 13% |
| Cardio-Oncology | 1570 | 1,370 | 200 | 13% |
| Clinical Proteomics | 1570 | 1,370 | 200 | 13% |
| Cost Effectiveness and Resource Allocation | 1570 | 1,370 | 200 | 13% |
| Health and Quality of Life Outcomes | 1570 | 1,370 | 200 | 13% |
| Infectious Diseases of Poverty | 1570 | 1,370 | 200 | 13% |
| International Journal of Mental Health Systems | 1570 | 1,370 | 200 | 13% |
| Population Health Metrics | 1570 | 1,370 | 200 | 13% |
| Thrombosis Journal | 1570 | 1,370 | 200 | 13% |
| Epigenetics & Chromatin | 1790 | 1,565 | 225 | 13% |
| Harm Reduction Journal | 1790 | 1,565 | 225 | 13% |
| Journal of Neuroinflammation | 1790 | 1,565 | 225 | 13% |
| Biology of Sex Differences | 1790 | 1,565 | 225 | 13% |
| Molecular Medicine | 1790 | 1,565 | 225 | 13% |
| Critical Care | 1990 | 1,750 | 240 | 12% |
| Experimental Hematology & Oncology | 1690 | 1,495 | 195 | 12% |
| Molecular Brain | 1570 | 1,395 | 175 | 11% |
| Implementation Science | 1690 | 1,510 | 180 | 11% |
| Respiratory Research | 1790 | 1,615 | 175 | 10% |
| Journal of Biological Engineering | 1570 | 1,430 | 140 | 9% |
| Journal of Pharmaceutical Policy and Practice | 1570 | 1,430 | 140 | 9% |
| Journal for ImmunoTherapy of Cancer | 1690 | 1,540 | 150 | 9% |
| BMC Infectious Diseases | 1490 | 1,370 | 120 | 8% |
| Trials | 1490 | 1,370 | 120 | 8% |
| Annals of Occupational and Environmental Medicine | 1370 | 1,265 | 105 | 8% |
| Asthma Research and Practice | 1480 | 1,370 | 110 | 7% |
| BioData Mining | 1480 | 1,370 | 110 | 7% |
| BMC Biochemistry | 1480 | 1,370 | 110 | 7% |
| BMC Bioinformatics | 1480 | 1,370 | 110 | 7% |
| BMC Clinical Pathology | 1480 | 1,370 | 110 | 7% |
| BMC Ear, Nose and Throat Disorders | 1480 | 1,370 | 110 | 7% |
| BMC Ecology | 1480 | 1,370 | 110 | 7% |
| BMC Hematology | 1480 | 1,370 | 110 | 7% |
| BMC Nephrology | 1480 | 1,370 | 110 | 7% |
| BMC Nursing | 1480 | 1,370 | 110 | 7% |
| BMC Ophthalmology | 1480 | 1,370 | 110 | 7% |
| BMC Oral Health | 1480 | 1,370 | 110 | 7% |
| BMC Physiology | 1480 | 1,370 | 110 | 7% |
| BMC Pregnancy and Childbirth | 1480 | 1,370 | 110 | 7% |
| BMC Structural Biology | 1480 | 1,370 | 110 | 7% |
| BMC Urology | 1480 | 1,370 | 110 | 7% |
| Cancers of the Head & Neck | 1480 | 1,370 | 110 | 7% |
| Clinical and Molecular Allergy | 1480 | 1,370 | 110 | 7% |
| Clinical Diabetes and Endocrinology | 1480 | 1,370 | 110 | 7% |
| Contraception and Reproductive Medicine | 1480 | 1,370 | 110 | 7% |
| Disaster and Military Medicine | 1480 | 1,370 | 110 | 7% |
| Fertility Research and Practice | 1480 | 1,370 | 110 | 7% |
| Journal of Clinical Movement Disorders | 1480 | 1,370 | 110 | 7% |
| Lipids in Health and Disease | 1480 | 1,370 | 110 | 7% |
| Maternal Health, Neonatology and Perinatology | 1480 | 1,370 | 110 | 7% |
| Movement Ecology | 1480 | 1,370 | 110 | 7% |
| Proteome Science | 1480 | 1,370 | 110 | 7% |
| Translational Medicine Communications | 1480 | 1,370 | 110 | 7% |
| Tropical Diseases, Travel Medicine and Vaccines | 1480 | 1,370 | 110 | 7% |
| Women’s Midlife Health | 1480 | 1,370 | 110 | 7% |
| Addiction Science and Clinical Practice | 1480 | 1,370 | 110 | 7% |
| Annals of General Psychiatry | 1690 | 1,565 | 125 | 7% |
| Cancer & Metabolism | 1690 | 1,565 | 125 | 7% |
| Journal of Ethnobiology and Ethnomedicine | 1690 | 1,565 | 125 | 7% |
| Journal of Neurodevelopmental Disorders | 1690 | 1,565 | 125 | 7% |
| Arthritis Research & Therapy | 1870 | 1,750 | 120 | 6% |
| Veterinary Research | 1175 | 1,150 | 25 | 2% |
| BMC Biophysics | 1390 | 1,370 | 20 | 1% |
| BMC Genetics | 1390 | 1,370 | 20 | 1% |
| Cerebellum & Ataxias | 1390 | 1,370 | 20 | 1% |
| Fungal Biology and Biotechnology | 1390 | 1,370 | 20 | 1% |
| Multiple Sclerosis and Demyelinating Disorders | 1390 | 1,370 | 20 | 1% |
| pneumonia | 1390 | 1,370 | 20 | 1% |
| Research Integrity and Peer Review | 1390 | 1,370 | 20 | 1% |
| Sleep Science and Practice | 1390 | 1,370 | 20 | 1% |
| Irish Veterinary Journal | 1390 | 1,370 | 20 | 1% |
| Cellular & Molecular Biology Letters | 1390 | 1,420 | -30 | -2% |
| World Journal of Surgical Oncology | 1570 | 1,650 | -80 | -5% |
| Research Involvement and Engagement | 1480 | 1,565 | -85 | -6% |
| Bioelectronic Medicine | 1480 | 1,565 | -85 | -6% |
| Big Data Analytics | 1290 | 1,370 | -80 | -6% |
| Hereditas | 1290 | 1,370 | -80 | -6% |
| Marine Biodiversity Records | 1290 | 1,370 | -80 | -6% |
| Porcine Health Management | 1290 | 1,370 | -80 | -6% |
| Source Code for Biology and Medicine | 1290 | 1,370 | -80 | -6% |
| Journal of Biomedical Semantics | 1290 | 1,370 | -80 | -6% |
| Journal of Biological Research-Thessaloniki | 1390 | 1,510 | -120 | -9% |
| Pilot and Feasibility Studies | 1390 | 1,565 | -175 | -13% |
| Systematic Reviews | 1390 | 1,565 | -175 | -13% |
| Environmental Evidence | 1290 | 1,470 | -180 | -14% |
| BMC Dermatology | 1180 | 1,370 | -190 | -16% |
| BMC Emergency Medicine | 1180 | 1,370 | -190 | -16% |
| Journal of Congenital Cardiology | 1180 | 1,370 | -190 | -16% |
| Diagnostic and Prognostic Research | 1480 | 1,745 | -265 | -18% |
| EvoDevo | 1690 | 1,995 | -305 | -18% |
| Agriculture & Food Security | 1290 | 1,565 | -275 | -21% |
| Cilia | 1290 | 1,565 | -275 | -21% |
| Diabetology & Metabolic Syndrome | 1420 | 1,810 | -390 | -27% |
| Sustainable Earth | 690 | 900 | -210 | -30% |
| Animal Biotelemetry | 1180 | 1,565 | -385 | -33% |
| European Journal of Medical Research | 1480 | 1,995 | -515 | -35% |
| BMC Medical Ethics | 990 | 1,370 | -380 | -38% |
| BMC Nutrition | 990 | 1,370 | -380 | -38% |
| BMC Obesity | 990 | 1,370 | -380 | -38% |
| Philosophy, Ethics, and Humanities in Medicine | 990 | 1,370 | -380 | -38% |
| BMC Psychology | 860 | 1,370 | -510 | -59% |
| Canine Genetics and Epidemiology | 860 | 1,370 | -510 | -59% |
| Journal of Eating Disorders | 860 | 1,370 | -510 | -59% |
| BMC Zoology | 790 | 1,370 | -580 | -73% |
| Acta Veterinaria Scandinavica | 1510 | 1,510 | 0 | |
| Advances in Simulation | 1565 | 1,565 | 0 | |
| Allergy, Asthma & Clinical Immunology | 1370 | 1,370 | 0 | |
| Biological Research | 1430 | 1,430 | 0 | |
| Biology Direct | 1370 | 1,370 | 0 | |
| Biomaterials Research | 1370 | 1,370 | 0 | |
| BioPsychoSocial Medicine | 1370 | 1,370 | 0 | |
| BMC Biology | 1780 | 1,780 | 0 | |
| BMC Developmental Biology | 1370 | 1,370 | 0 | |
| BMC Endocrine Disorders | 1370 | 1,370 | 0 | |
| BMC Family Practice | 1370 | 1,370 | 0 | |
| BMC Genomics | 1370 | 1,370 | 0 | |
| BMC Immunology | 1370 | 1,370 | 0 | |
| BMC Medical Education | 1370 | 1,370 | 0 | |
| BMC Medical Genomics | 1370 | 1,370 | 0 | |
| BMC Molecular Biology | 1370 | 1,370 | 0 | |
| BMC Neuroscience | 1370 | 1,370 | 0 | |
| BMC Plant Biology | 1370 | 1,370 | 0 | |
| BMC Women’s Health | 1370 | 1,370 | 0 | |
| Borderline Personality Disorder and Emotion Dysregulation | 1370 | 1,370 | 0 | |
| Cell & Bioscience | 1370 | 1,370 | 0 | |
| Chinese Medicine | 1370 | 1,370 | 0 | |
| Clinical and Translational Allergy | 1470 | 1,470 | 0 | |
| Emerging Themes in Epidemiology | 1370 | 1,370 | 0 | |
| Environmental Health | 1420 | 1,420 | 0 | |
| European Review of Aging and Physical Activity | 1370 | 1,370 | 0 | |
| Fisheries and Aquatic Sciences | 1370 | 1,370 | 0 | |
| Frontiers in Zoology | 1510 | 1,510 | 0 | |
| Genetics Selection Evolution | 1175 | 1,175 | 0 | |
| Gynecologic Oncology Research and Practice | 1370 | 1,370 | 0 | |
| Health Research Policy and Systems | 1565 | 1,565 | 0 | |
| Human Resources for Health | 1565 | 1,565 | 0 | |
| Infectious Agents and Cancer | 1370 | 1,370 | 0 | |
| International Journal of Behavioral Nutrition and Physical Activity | 1650 | 1,650 | 0 | |
| Journal of Cardiovascular Magnetic Resonance | 1600 | 1,600 | 0 | |
| Journal of Ecology and Environment | 1370 | 1,370 | 0 | |
| Journal of Foot and Ankle Research | 1370 | 1,370 | 0 | |
| Journal of Health, Population and Nutrition | 1370 | 1,370 | 0 | |
| Journal of Medical Case Reports | 825 | 825 | 0 | |
| Journal of Pharmaceutical Health Care and Sciences | 1420 | 1,420 | 0 | |
| Journal of the International Society of Sports Nutrition | 1370 | 1,370 | 0 | |
| Malaria Journal | 1430 | 1,430 | 0 | |
| Mobile DNA | 1370 | 1,370 | 0 | |
| Molecular Neurodegeneration | 1650 | 1,650 | 0 | |
| Multidisciplinary Respiratory Medicine | 1370 | 1,370 | 0 | |
| Parasites & Vectors | 1370 | 1,370 | 0 | |
| Perioperative Medicine | 1565 | 1,565 | 0 | |
| Plant Methods | 1430 | 1,430 | 0 | |
| Public Health Reviews | 1370 | 1,370 | 0 | |
| Revista Chilena de Historia Natural | 1240 | 1,240 | 0 | |
| Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine | 1485 | 1,485 | 0 | |
| Cancer Imaging | 1370 | 1,370 | 0 | |
| Journal of Otolaryngology : Head and Neck Surgery | 1370 | 1,370 | 0 | |
| The Italian Journal of Pediatrics | 1370 | 1,370 | 0 | |
| Cancer Communications | 1370 | 1,370 | 0 | |
| BioMedical Engineering OnLine | 1375 | 1,370 | 5 | |
| Journal of Orthopaedic Surgery and Research | 1570 | 1,565 | 5 | |
| Skeletal Muscle | 1570 | 1,565 | 5 | |
| Algorithms for Molecular Biology | 1390 | 1,370 | 20 |
Our recent analysis of BioMed Central publishing company journals reveals a sharp increase both in number of open access journals and also article processing fees.
BMC currently publishes 330 open access journals that comparing to 2018 data shows an increase of 11% in number of journals. While 25 journals have no article processing fee for authors to publish their articles, there has been a 57% increase in average article processing charge comparing to the last year, as the average processing fee was $1402 in 2018 and now it is $2200.
Comparing to the last year, 264 journals have increased and 5 journals have decreased in APC (article processing charge). The average APC increase for journals is $917 and the average decrease is $124.

The raw data for BMC in 2019 is provided below:
Similar posts:
Ceased and transferred publications and archiving: best practices and room for improvement
Recent APC price changes for 4 publishers (BMC, Hindawi, PLOS, PeerJ)
Pashaei, H., & Morrison, H. (2019). BioMed Central in 2019: Sharp increase in article processing charge. Sustaining the Knowledge Commons / Soutenir Les Savoirs Communs . Retrieved from https://sustainingknowledgecommons.org/2019/04/30/biomed-central-in-2019-sharp-increase-in-article-processing-charge/
Share this:
Leave a comment cancel reply.
This site uses Akismet to reduce spam. Learn how your comment data is processed .
- Already have a WordPress.com account? Log in now.
- Subscribe Subscribed
- Copy shortlink
- Report this content
- View post in Reader
- Manage subscriptions
- Collapse this bar
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
The PMC website is updating on October 15, 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- BMC Med Res Methodol

| 2020 to 2024 |
 Try the new-look Sherpa Our new site consolidates Sherpa Services (Romeo, Juliet, Fact and OpenDOAR) in to one handy tool, and brings you Open Access policy, compliance and Transitional Agreement information. Go to the new website >  Sherpa Romeo BMC Medical Research MethodologyPublication information, publisher policy. Open Access pathways permitted by this journal's policy are listed below by article version. Click on a pathway for a more detailed view. Published Version [pathway a]
Published Version [pathway b]Accepted version, submitted version.
Record InformationSherpa Romeo information is accurate to the best of our knowledge but should not be relied upon for legal advice.
Training healthcare professionals in assessment of health needs in older adults living at home: a scoping review
BMC Medical Education volume 24 , Article number: 1019 ( 2024 ) Cite this article Metrics details Interprofessional assessment and management of health needs for older adults living at home can help prioritize community service resources and enhance health, yet there is a shortage of professionals with the necessary competencies. Therefore, support and training for healthcare professionals in community settings to assess older adults’ health with the aim of for health promotion are needed. To identify and provide an overview of published papers describing approaches for training healthcare professionals in assessing physical, mental, and social health needs in older adults living at home. A systematic literature search of the Cinahl, Medline, Academic Search Ultimate, Scopus, Embase, and British Nursing Index databases was performed. We considered studies focusing on the training of healthcare professionals in assessing a single or multiple health needs of older adults aged 65 and above living at home. We considered studies published between 1990 – and March 2024. The review evaluated qualitative, quantitative, and mixed methods studies published in English-language peer-reviewed academic journals. A quality appraisal was conducted via the Mixed Methods Appraisal Tool (MMAT). Twenty-three studies focused on training healthcare professionals to assess health needs and plan care for older adults living at home were included. The majority of the included studies combined teacher-driven pedagogical approaches consisting of educational sessions, written materials or e-learning, and more participant-engaging pedagogical approaches such as knowledge exchange or various forms of interactive learning. Healthcare professionals were trained to detect and manage single and multiple health needs, and some studies additionally incorporated interprofessional collaboration. Healthcare professionals were satisfied with the training content and it increased their confidence and competencies in health needs assessment and care planning for older adults. Moreover, some studies have reported that training interventions foster the implementation of new and effective ways of working and lead to positive outcomes for older adults. Healthcare professionals were satisfied with a combination of participant-engaging and teacher-driven pedagogical approaches used to train them in assessing health needs and planning care for older adults living at home. Such training can lead to enhanced assessment skills and facilitate improvements in practice and health promotion for older adults. Future research is recommended on interprofessional simulation training for conducting structured and comprehensive health needs assessments of older adults living at home, as well as on the implementation of such assessments and health-promoting interventions. Peer Review reports IntroductionThe globally growing and diverse aging population will impact the sustainability of healthcare systems and the independent living of older adults. To support the health needs of older adults, the World Health Organization (WHO) underscores the necessity of effectively training the healthcare workforce [ 1 , 2 ]. However, the complexity of health needs in older adults, coupled with an increased risk of frailty and adverse health outcomes, challenges the provision of tailored care [ 3 ]. Healthcare professionals in homecare settings are well-positioned to assess the health needs of home-living older adults [ 4 , 5 ] and facilitate the interprofessional management of these needs within the community [ 5 ]. Health needs assessment should offer a comprehensive understanding of individuals’ physical, mental, and social health needs, and address the constantly changing needs with increasing age. The assessments aim to identify those who can benefit from healthcare services, such as health education, disease prevention, treatment, and rehabilitation [ 6 ]. The assessment can help set service priorities and allocate service resources effectively, guide clinical decision-making [ 7 ] and design targeted, health promoting interventions [ 4 , 7 , 8 , 9 ] to prevent or delay frailty [ 10 ], enhance overall outcomes for those with complex health needs [ 11 ] and enable them to remain at home for as long as possible [ 12 ]. Given its importance, the task of health needs assessment, is becoming increasingly crucial in homecare settings [ 13 ]. However, there is a scarcity of adequately trained professionals proficient in conducting interprofessional health needs assessments [ 4 , 5 , 9 , 14 , 15 ], including depression [ 16 ], cognitive function [ 17 ], social needs [ 18 ], sensory function (i.e. hearing and vision) [ 19 ], geriatric healthcare [ 20 , 21 ], and multidimensional frailty [ 22 , 23 ]. Frailty, as a dynamic state, affects an individual who experiences losses in one or more domains of human functioning (physical, mental, social) that are caused by the influence of a range of variables, and which increase the risk of adverse outcomes [ 24 ]. A comprehensive understanding of how to train healthcare professionals in health needs assessment of the physical, mental, and social health needs of older adults living at home is crucial. This review understands training as “planned and systematic activities designed to promote the acquisition of the knowledge, skills, and attitudes” [ 25 , p77]. Training can take place as “on-the-job training,” with practicing tasks with a mentor or receiving feedback, or through “off-the-job training,” in a classroom setting with lectures, discussions, and exercises [ 26 ]. It is essential to consistently update and expand knowledge and skills throughout healthcare professionals’ careers [ 27 ]. Mentorship and support are highly valued as pedagogical approaches [ 28 ]. Another approach is implementing interprofessional team-based training [ 29 ] focused on health needs assessment for older adults, which can be complemented by practical, supervised training with a mentor in real-world settings [ 9 ]. Interprofessional simulation training can support healthcare professionals developing communication and collaborative skills and improving patient outcomes [ 2 ]. Additionally, opportunities to share and exchange experiences and new learning with peers and seniors, along with tailored, role-focused teaching, are effective approaches training strategies in community healthcare [ 30 ]. Practical training through simulation, case studies, and role-playing influences skill development by creating experiences that promote individual understanding and learning [ 31 ] and it is based on Vygotsky’s sociocultural learning theory [ 32 ]. Tailored simulation training in use of systematic assessment tools enhanced nurses’ competencies to assess and treat complex symptoms among older adults in long-term care facilities [ 33 ]. Therefore, this scoping review aimed to identify and provide an overview of published papers describing approaches for training healthcare professionals in assessing physical, mental, and social health needs in older adults living at home. Three research questions guided the review: (1) what pedagogical approaches are used when training healthcare professionals to assess the health needs of older adults living at home, (2) what is the content and foci in the health needs assessment training provided in the studies, and (3) what are the outcomes of training reported by healthcare professionals and older adults living at home? Scoping review designThis study followed the Joanna Briggs Institute (JBI) methodology [ 34 ] for conducting and reporting scoping reviews built on Arksey and O’Malley’s framework [ 35 ]: (1) Define and align the objectives (2) develop and align the inclusion criteria with the objectives (3) describe the planned approach to evidence searching, selection, data extraction, and presentation of the evidence (4) search for the evidence (5) select the evidence (6) extract the evidence (7) analyze the evidence (8) present the results (9) summarize the evidence in relation to the purpose of the review, draw conclusions and note the implications of the findings [ 36 ]. In addition, the PRISMA-ScR [ 37 ] was used as a checklist to report the scoping review data charting, data synthesis and presentation of the data (Additional file 1). Selection of studiesTo be eligible for inclusion in the review, the study had to focus on the training of healthcare professionals in assessing physical, mental and social health needs [ 24 ], specifically assessing frailty, physical function, depression, cognition, social health, and sensory function of older adults aged 65 and above living at home [ 38 ]. Healthcare professionals from diverse fields were included, whether engaging in one-to-one interactions where individual healthcare professionals work directly with patients or working collaboratively in interprofessional teams of members from different professional backgrounds [ 29 ]. The review included qualitative, quantitative, and mixed methods studies published in English-language peer-reviewed academic journals. The inclusion and exclusion criteria are specified in Table 1 below. Search strategyThe authors and an experienced research librarian collaboratively developed the search strategy and search terms. The search strategy followed the recommendation of JBI [ 34 ]. In June 2022, a limited search of PubMed and CINAHL was conducted to identify relevant articles. To develop a more comprehensive search strategy, we subsequently analyzed the titles and abstracts of the retrieved papers, as well as the index terms used to describe the articles. A systematic literature search was performed on October 6, 2022, in the CINAHL (EBSCO), MEDLINE (EBSCO), Academic Search Ultimate (EBSCO), Scopus (Elsevier), Embase (OVID) and British Nursing Index (ProQuest) databases. The updated search was conducted on the 7th of March 2024. The search terms employed in the different databases to represent training healthcare professionals to assess health needs in older adults living at home are described in Table 2 . We considered studies published between 1990 – and March 2024. Ultimately, the reference lists of all included studies were reviewed to identify any additional studies aligned with the scoping review’s aim. Identification and selection of studiesThe search yielded a total of 2266 records. The study selection process is illustrated in Fig. 1 according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram [ 39 ]. The search results were uploaded into the citation management system EndNote, where duplicates were removed. A total of 1722 records remained for screening. We used the web application Rayyan [ 40 ] to screen studies for inclusion or exclusion. The screening involved all the authors working in pairs, independently assessing eligibility on the basis of the inclusion and exclusion criteria. Discrepancies were resolved through discussions until consensus by all authors in arranged meetings. All the records were independently screened by the authors (BHL, DND, HKF, PD and MS), and 1452 records were excluded. Two hundred seventy abstracts were reviewed in blinded pairs, leading to the exclusion of 212 records. Next, the full texts of 58 studies were read. This process resulted in the exclusion of 38 studies whose reasons are provided in the flow chart. The remaining 20 studies were included in this review (Fig. 1 ). The primary reason for exclusion was the lack of content related to training in health needs assessment ( n = 13) or incorrect populations ( n = 12). Eight studies were excluded because they focused on training for medical or bachelor’s degree students. Additionally, four publications were not peer-reviewed studies ( n = 4). BHL and MS independently screened the reference lists from the 20 included studies to identify additional eligible studies. After all the blinded titles were read, 28 titles of records were identified for abstract review. Following this, 22 titles were excluded, leaving 6 abstracts included in the full-text examination. The full-text reading further excluded four studies because they did not focus on training in health needs assessment. Finally, two studies [ 41 , 42 ] were added to this scoping review, resulting in a total of 22 included studies. An updated search was conducted on the 7th of March 2024, including publications from 2022 to 2024, following the procedure above. After removing duplicates, 173 titles and abstracts were screened for eligibility. The full texts of nine articles were read. Six studies were excluded because they did not include training for healthcare professionals. One had incorrect population, and the others were in a language other than English. This led to the inclusion of one new study [ 43 ], bringing the total number of included studies for the scoping review to 23.  Search results, study selection and inclusion process [ 39 ] Extraction and analysis of the dataIn line with the updated JBI methodological guidelines for scoping reviews [ 34 ], we extracted and coded descriptive details from the 23 included records. The extraction table covered the publication year, country of origin, study purpose, research design, study population, context/setting, training intervention content and assessment tools, pedagogical approaches and training duration, and outcomes for healthcare professionals and older adults. A test was conducted to ensure that the coauthors were aligned in their understanding of what type of data to extract for the table. Feedback from the test guided essential refinements to the extraction table before the authors collaborated to extract and organize pertinent information. We applied a basic thematic analysis to code the data and identify, analyze, and interpret patterns, ultimately deriving themes that addressed our research questions [ 44 , 45 ]. The analysis utilized NVivo 12 Pro software [ 46 ]. Quality appraisalWe performed a quality evaluation of the included studies via the Mixed Methods Appraisal Tool (MMAT) in blinded pairs. This tool is designed for a structured and standardized evaluation of methodological quality and risk of bias in systematic reviews that include qualitative, quantitative, and mixed methods studies [ 47 ]. Although quality evaluation is optional in a scoping review, it can provide valuable insights [ 48 ] and enhance the interpretability of the included studies [ 49 ]. All studies were evaluated according to five quality criteria specific to each research design (qualitative, quantitative descriptive, nonrandomized, randomized, and mixed methods studies). Each criterion received a response score of either “Yes,” indicating that the study met the quality criteria, or “No,” indicating that it did not meet the quality criteria or that it was unclear (see Table 4 ). It is discouraged to calculate an overall score. Any disagreements in scoring were resolved through discussion. The quality scores were not used to exclude articles from the review; instead, they were reported and discussed [ 49 ]. In accordance with the JBI scoping review guidance [ 44 ], the extracted data are presented in a table format (Tables 3 and 5 ) and a narrative summary is provided to respond to the three research questions. Table 3 provides a description of the study characteristics, while Table 5 outlines overarching categories along with relevant extracted information [ 44 ]. Characteristics of the included studiesTable 3 shows that the 23 studies were published between 1990- and 2023. Eight studies were conducted in the United States [ 16 , 42 , 43 , 50 , 51 , 52 , 53 , 54 ], three in Canada [ 55 , 56 , 57 ], three in Australia [ 58 , 59 , 60 ], three in the United Kingdom [ 41 , 61 , 62 ], and one each in Ireland [ 63 ], Italy [ 64 ], Brazil [ 65 ], France [ 66 ], Singapore [ 67 ], and Belgium [ 68 ]. Ten studies meticulously examined training interventions tailored for primary nurses [ 43 , 50 , 51 , 54 , 55 , 60 , 61 , 63 , 66 , 68 ], one study specifically targeted the training of community health workers [ 65 ] and another presented an educational session tailored for case managers and agency supervisors [ 42 ]. The remaining studies indicated that training was provided to interprofessional teams or various distinct professions, such as nurses, physical therapists, occupational therapists, general practitioners, social workers and psychologists [ 16 , 41 , 52 , 53 , 56 , 57 , 58 , 59 , 62 , 64 , 67 ]. The study participants were in home healthcare or primary/community care [ 16 , 41 , 43 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 68 ], community and social services [ 42 , 64 ], mental health care [ 61 ], eldercare centers/daycare [ 67 ], residential settings [ 58 , 59 , 64 ], hospitals [ 53 , 56 ], rehabilitation [ 56 ] and acute care [ 61 ]. Quality evaluation resultsThe quality appraisal procedure revealed variations in the quality of the 23 included studies. The detailed quality evaluation results for each study are presented in Table 4 , and an overview of the methodological quality criteria is presented in Additional file 3. Each study was evaluated on five criteria appropriate to its study design category. Overall, only one study, which was a mixed methods study, met al.l five quality criteria in the MMAT [ 62 ]. Additionally, one mixed methods study met four criteria [ 61 ], and another met three criteria [ 65 ]. The most common criterion that mixed methods studies failed to meet was 5.2: whether the different components of the study were effectively integrated to answer the research question. Among the quantitative randomized studies, one study met four quality criteria [ 50 ], whereas the other was of low quality, meeting only one criterion [ 59 ]. None of these studies met the quality criterion for proper randomization. In the quantitative nonrandomized studies, six met four criteria [ 41 , 55 , 56 , 58 , 64 , 68 ], one met three [ 63 ], and one met only one criterion [ 16 ], indicating low quality. All studies met the criterion regarding whether the intervention was administered as intended. The most common criteria they failed to meet were 3.3: whether there were complete data and 3.4: whether confounders were accounted for in the study design and analysis. Among the descriptive studies, seven met four criteria [ 42 , 43 , 54 , 57 , 60 , 66 , 67 ], one met three criteria [ 53 ], and two met only one criterion [ 51 , 52 ], demonstrating low quality. The majority of these studies met the criterion regarding whether the measurements were appropriate. However, the criterion most studies did not meet (only one out of ten) was whether the risk of nonresponse bias was low. Notably, no qualitative methods studies were included in our scoping review. Training interventions in assessment of older adults living at homeThe next section presents a narrative overview of three major themes related to the three research questions. The themes concerned the training provided for healthcare professionals in assessing the physical, mental, and social health needs of older adults living at home: pedagogical approaches, content and foci of health needs assessment training for healthcare professionals and outcomes and evaluation of health needs assessment training for healthcare professionals and older adults living at home. The findings are summarized in Table 5 [ 44 ]. Pedagogical approachesThe included studies employed diverse pedagogical approaches to train healthcare professionals in assessing the health needs of older adults living at home. The spectrum of pedagogical approaches observed in the studies was categorized into teacher-driven and participant-engaging pedagogical approaches. Twenty-one studies [ 16 , 42 , 43 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 67 , 68 ] combined teacher-driven and participant-engaging pedagogical approaches, reflecting a multifaceted training strategy. Mayall et al. [ 41 ] opted for a more singular pedagogical approach, exclusively relying on lecture-based education, whereas the training method used in the Piau et al. [ 66 ] study remained unspecified. The training interventions varied in duration, from one-hour sessions [ 68 ] to an ongoing training program spanning 21 months [ 57 ]. In two studies, the specific duration of the training interventions was not specified [ 53 , 57 ]. The most common duration for training was 4–8 h [ 16 , 43 , 50 , 52 , 54 , 56 , 58 , 59 , 62 , 67 ]. Teacher-driven pedagogical approachesAlmost all studies utilized teacher-driven pedagogical approaches, including educational sessions, written materials or e-learning [ 16 , 41 , 42 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 67 , 68 ]. Educational sessions were evident in 14 studies [ 16 , 41 , 42 , 50 , 51 , 52 , 53 , 56 , 57 , 58 , 59 , 62 , 64 , 65 ], providing healthcare professionals with information about relevant topics through lectures [ 16 , 41 , 42 , 51 , 62 , 64 , 65 ], slides [ 16 , 64 ] and instructions [ 50 , 52 , 53 ], as well as demonstrations of the use of assessment tools [ 41 , 42 , 51 , 56 , 58 , 59 ]. Additionally, Abbasi et al. [ 57 ] and Quijano et al. [ 42 ] offered ongoing sessions during the post training implementation period. Written materials were provided to the participants in nine studies [ 16 , 42 , 50 , 52 , 54 , 58 , 59 , 63 , 64 ]. This included training manuals containing examples and case studies [ 58 , 59 ], written documents about the training pack and the assessment forms [ 63 ], course textbooks and instruction manuals [ 64 ], educational materials including the program manual and articles [ 42 ], a CD-ROM (a data-disc for computer) containing written educational material [ 52 ] and toolkits derived from the educational material [ 16 , 50 , 54 ]. Brown et al. [ 54 ] reported that toolkits included key intervention components for seamless application of learned concepts [ 54 ]. Furthermore, some described follow-up emails to provide participants with information post training [ 50 , 54 ]. E-learning as a preplaying online module or videoclip appeared in nine studies [ 16 , 42 , 43 , 50 , 53 , 54 , 61 , 64 , 68 ]. Naughton et al. [ 61 ] delivered prerecorded lectures [ 61 ], Landi et al. [ 64 ] used video recordings presenting real cases to test participants’ assessments- and decision-making skills, and Quinlan and Ryer [ 43 ] offered online modules on aging epidemiology, fall risk factors, and age-friendly health systems [ 43 ]. Participants watched video recordings portraying late-life depression [ 42 , 53 , 54 ], and patient interactions illustrating approaches to depression assessment [ 50 , 54 , 68 ] via standardized questions and follow-up questions [ 16 ]. Professional actors were used in three studies [ 16 , 53 , 68 ]. Participant-engaging pedagogical approachesThe majority of the included studies utilized participant-engaging pedagogical approaches involving knowledge exchange or various forms of interactive learning [ 16 , 42 , 43 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 67 , 68 ]. Sixteen studies employed various forms of knowledge exchange such as discussion, questioning and coaching, between training participants and teachers [ 43 , 51 , 52 , 53 , 54 , 55 , 56 , 58 , 59 , 60 , 61 , 63 , 64 , 65 , 67 , 68 ]. Peer-to-peer learning and dialog facilitated the exchange of knowledge and insights [ 65 ], which enriched the overall learning experience [ 61 ]. The participants were included in discussions following lectures [ 55 ], after watching scripted videos [ 53 ], and during patient case reviews [ 56 , 67 ]. Additionally, three studies included both discussions and allowed participants questions [ 52 , 54 , 68 ]. Discussions allowed participants to delve into case management techniques [ 51 ], explore experiences related to assessing the health of older adults [ 54 , 60 , 64 ] and solve problems and discuss alternative strategies regarding depression screening [ 54 ]. A few studies have provided ongoing coaching in the post training phase to support healthcare professionals in applying newly acquired skills [ 42 , 55 , 57 ]. This included three months of feedback and support [ 42 ], mentorship for skill integration [ 57 ], and a six-month collaborative approach between resource staff and case managers involving home visits and clinical consultations [ 55 ]. Interactive training was employed in fifteen studies through skills training, role-playing, simulations, and hands-on training in real-world settings [ 16 , 42 , 43 , 51 , 52 , 54 , 55 , 57 , 58 , 59 , 60 , 62 , 63 , 64 , 65 ]. Skill training allows nurses to practice patient interviews and assessments and receive instructor feedback [ 54 ]. The participants practiced by assessing their colleagues’ health and responding to assessment [ 16 , 51 ], with faculty staff offering assistance, encouragement, and feedback throughout [ 51 ]. Landi et al. [ 64 ] provided practice exercises followed by presentations, and Quinlan and Ryer [ 43 ] provided a virtual training session in motivational interviewing technique and assessment. Roleplay as a teaching strategy was used to address practical aspects of administering depression screening [ 50 , 52 , 60 ], and Butler and Quayle [ 63 ] incorporated case scenarios, roleplay, and practical skills training for assessing depression in older adults [ 63 ]. Simulation training was used to immerse participants in the experience of living with sight and hearing impairments performing everyday tasks such as filling out forms or managing medications using sight impairment spectacles. Training was followed by a debriefing session [ 62 ]. Hands-on training in the assessment of older adults’ health in real-world settings was conducted in ten studies [ 42 , 51 , 54 , 55 , 57 , 58 , 59 , 60 , 64 , 65 ]. Healthcare professionals gained clinical experience through assessments of home dwelling older adults [ 55 , 58 , 59 , 60 , 64 , 65 ] and through participation in a rotational preceptorship for community health nurses. This enabled them to practice newly acquired assessment skills and collaborate in a real-life setting [ 51 ]. Additionally, two other studies emphasized practical training in communication with other professionals in real-world settings [ 58 , 59 ], while Brown et al. [ 54 ] encouraged participants to practice assessments in a real-world setting between educational sessions. Content and foci of health needs assessment training for health care professionalsAll the included studies offered insights into the content and foci of health neesd assessment training interventions for healthcare professionals. The studies were divided into those aimed at training healthcare professionals to understand and assess either single or multiple physical, mental, and social health needs in older adults living at home. Additionally, some training sessions focused on interprofessional collaboration. Single health need assessment trainingThe focus of twelve studies involved enhancing the skills of healthcare professionals in assessing, planning and conducting interventions for a specific, single health need in older adults, with each addressing either the assessment of mental or physical health [ 16 , 41 , 43 , 52 , 53 , 54 , 58 , 59 , 60 , 62 , 63 , 68 ]. Two of these studies [ 43 , 62 ] focused solely on physical health factor training. Smith et al. [ 62 ] emphasized training in assessing and detecting sight and hearing impairments without specifying whether any assessment tools were used [ 62 ]. Quinlan and Ryer [ 43 ] provided fall risk assessment training, which included the use of assessment tools to evaluate the physical function of older adults and to assess their home environments. The other ten studies [ 16 , 41 , 52 , 53 , 54 , 58 , 59 , 60 , 63 , 68 ] focused on training to assess depression in older adults living at home. The training encompassed understanding and detecting the condition, and all of them included the use of assessment tools. Van Daele et al. [ 68 ] included skills such as actively listening to patients and motivating them to seek expert assistance when needed. Delaney et al. [ 16 ] incorporated skills in asking follow-up questions, and Mellor et al. [ 59 ] offered training in appropriate communication with older adults to identify masked, early signs of depression. Multiple health needs assessment trainingEleven studies [ 42 , 50 , 51 , 55 , 56 , 57 , 61 , 64 , 65 , 66 , 67 ] described training interventions for healthcare professionals aimed at assessing, planning, and conducting interventions for multiple health needs in older adults living at home. The training content ranged from learning to performing a holistic health assessment of older adults encompassing physical, mental, cognitive, and social factors [ 42 , 51 , 55 , 56 , 57 , 61 , 64 , 66 ] to a more nuanced assessment of two or three of these factors [ 50 , 65 , 67 ]. All studies described the use of assessment tools or checklists. A holistic assessment and understanding of older adults’ health context and needs enables interventions to be tailored to their health and care needs, priorities, and levels of frailty [ 57 ]. Within the realm of holistic assessment, only two of these studies addressed alcohol and medication usage [ 55 , 56 ], whereas two other studies focused on evaluating sensory status [ 57 , 66 ]. For studies with more nuanced assessment training, three studies [ 42 , 50 , 67 ] primarily tailored their training to focus on depression assessment and intervention in older adults, but Quijano et al. [ 42 ] also included training in assessing general physical health status, social function, and cognitive function. Sin et al. [ 67 ] included dementia assessment and Bruce et al. [ 50 ] addressed factors that commonly complicate depression in homecare patients, such as health conditions, disability in activities of daily living, and cognitive function. The training included how to ask follow-up questions and observe nonverbal language [ 50 ]. Neto et al. [ 65 ] provided training for healthcare professionals in rural areas to screen for geriatric risk factors such as caregiver overburden, general health, social health, risk of falling, or difficulties in activities of daily living. Interprofessional collaboration and communication skills in health needs assessment trainingBeyond the focus on training for assessing the health needs of older adults, sixteen studies [ 42 , 50 , 51 , 52 , 53 , 54 , 55 , 57 , 58 , 59 , 60 , 61 , 62 , 64 , 65 , 68 ] have incorporated training elements to increase interprofessional collaboration and communication skills among healthcare professionals. Health needs assessment training for interprofessional teams was evident in eight of the included studies [ 51 , 55 , 57 , 58 , 59 , 61 , 64 , 65 ]. Two studies [ 58 , 59 ] outlined an advanced session to teach skills for interacting with other healthcare providers, including general practitioners and mental health specialists, whereas Couser et al. [ 51 ] stressed the importance of effectively communicating the assessment results to physicians and other healthcare providers. Training in writing referrals was emphasized in ten studies [ 42 , 50 , 52 , 53 , 54 , 58 , 59 , 60 , 62 , 68 ]. In addition, Stolee et al. [ 55 ] trained healthcare professionals in writing reports and making recommendations to the referring case manager. Only two studies [ 61 , 65 ] included collaboration with family in their training programs. Naughton et al. [ 61 ] designed training programs to support healthcare professionals in navigating the complexities of collaboration with multidisciplinary teams, older adults, and their families. They also developed a network among nurses to facilitate the exchange of expertise, experience, and innovative ideas [ 61 ]. Neto et al. [ 65 ] aimed to increase the capacity of care workers to effectively collaborate with family caregivers and social services for dependent older adults in rural areas. Stolee et al. [ 55 ] provided training for case managers to extend this knowledge to their teams and strengthen connections with specialized geriatric services. Similarly, Abbasi et al. [ 57 ] emphasized team-based care delivery training, with active and holistic discussions among patients, caregivers, and interprofessional teams. Diverse skill sets within teams can effectively meet the holistic care needs of patients. In parallel, Piau et al. [ 66 ] focused on training nurses to collaborate with general practitioners to develop comprehensive care plans. Landi et al. [ 64 ] trained case managers who collaborated in supervised teams to assess older adults and present care plans. They watched videos of simulated team discussions to enhance their understanding of the assessment process and teamwork [ 64 ]. Evaluation and outcomes of health needs assessment training for healthcare professionals and older adultsAll of the studies provided insight into the experiences or outcomes of healthcare professionals participating in the training interventions. This included their satisfaction and experiences with health needs assessment training, improved confidence and competencies in health assessment and care planning and shifts in work practices. Additionally, some studies have reported outcomes for older adults following health needs assessment training, such as appropriate referrals, tailored interventions, fall prevention, symptom reduction, and improved overall function. The evaluation of these outcomes relied to a small extent on models or frameworks, with only three studies incorporating them [ 43 , 61 , 62 ]. Smith et al. [ 62 ] utilized Kirkpatrick’s four-level training evaluation model to assess the relevance and impact of educational intervention. Naughton et al. [ 61 ] adopted Alvarez et al.’s (2004) framework of an integral model of training evaluation and effectiveness. Quinlan and Ryer [ 43 ] presented their findings following the Revised Standards for Quality Improvement Reporting Excellence (SQUIRE) framework. Healthcare professionals’ satisfaction and experiences with assessment trainingTen studies provided insights into healthcare professionals’ experiences with participating in training interventions [ 16 , 41 , 43 , 54 , 55 , 56 , 60 , 61 , 62 , 65 ], where most of the participants expressed satisfaction with both the content and format of the courses. The participants in Brymer, Cormack and Spezowka [ 56 ] expressed a high level of satisfaction with the presenter’s content, pacing, and format, and in Mayall et al. [ 41 ], the training met the participants’ needs and expectations. The participants in Naughton et al. [ 61 ] particularly valued the peer-to-peer learning aspect, whereas Smith et al. [ 62 ] emphasized the effectiveness of simulations. Neto et al. [ 65 ] rated classroom sessions and supervised home visits very positively and found them useful. Furthermore, participants in four of the studies [ 16 , 60 , 61 , 65 ] offered suggestions to enhance the number of educational sessions. They suggested allocating more time for training [ 16 , 65 ], a greater focus on skills training [ 60 , 61 ], additional training in managing complex and technically challenging issues [ 65 ] and incorporating more time for case studies and discussions [ 16 ]. Improved confidence and competence in health assessment and care planningImprovements in assessment competencies following training interventions among healthcare professionals were reported in nineteen studies [ 16 , 41 , 42 , 51 , 52 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 62 , 63 , 64 , 65 , 66 , 67 , 68 ]. Among these, nine studies explicitly reported increased confidence among healthcare professionals in assessing older adults’ health needs [ 16 , 41 , 54 , 55 , 58 , 59 , 63 , 67 , 68 ]. The health need sassessment and use of assessment tools or checklists led to the identification of health needs. Quinlan and Ryer [ 43 ] noted that without screening in a fall prevention program, the identification of fall risk among older adults would be missed. Piau et al. [ 66 ] noted that a high proportion of assessments effectively identified frailty and suggested interventions and referrals. One comment was that they “were previously skirting around the problem, now asked about mental health directly” [ 61 , p. 33]. Naughton et al. [ 61 ] reported that performing a comprehensive geriatric assessment helped when raising issues with general practitioners because they were talking about their language. Nunn, Annells and Sims [ 60 ] acknowledged the use of Geriatric Depression Screening (GDS) tool raised awareness of depression. A total of 62.5% felt that the GDS helped identify depression that might otherwise be overlooked, but some questioned its universal usefulness [ 60 ]. Abbasi et al. [ 57 ] reported that having an evaluation framework helped healthcare professionals guide meaningful measures [ 57 ]. Conversely, some participants also expressed that they relied more on observation than direct questions when assessing depression [ 54 ]. According to Landi et al. [ 64 ], careful assessments is deemed essential for effective care planning, and Stolee et al. [ 55 ] emphasize the critical role of assessment training in identifying health needs and equitably distributing community service resources. Two studies reported one year of retention of knowledge and skills without the inclusion of a refresher course [ 54 , 62 ]. Twenty studies documented a better understanding of appropriate interventions and referrals [ 16 , 41 , 42 , 50 , 51 , 52 , 53 , 55 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 ]. According to Delaney et al. [ 16 ], 50% of the participants noted that a key aspect they learned was understanding the significance of the assessment results and the corresponding interventions [ 16 ]. The participants in the study by Neto et al. [ 65 ] demonstrated significantly improved capacity in responding to the health and care needs of older adults. The participant reported increased confidence in making referrals and consulting resources [ 51 ], increased knowledge about managing depression, making referrals, and accessing available local services [ 41 ] and enhanced self-efficacy in providing care for older adults [ 16 , 58 ]. Nunn, Annells and Sims [ 60 ] reported that 50% of participants felt prepared to address older adults’ depression after training. Smith et al. [ 62 ] observed increased referral practices and improved ability to advise patients about sensory services, whereas Mellor et al. [ 59 ] noted a slight increase over time in specialist referrals, and senior staff reported increased confidence in interacting with health specialists. Shift in healthcare professionals’ work practices after assessment trainingThe training intervention resulted in either a change or potential for change in work practices in ten studies [ 16 , 42 , 43 , 52 , 53 , 55 , 57 , 62 , 63 , 64 ]. Butler and Quayle [ 63 ] reported that prior to receiving training, nurses did not utilize any formal assessment measures to screen for depression in older adults. However, following training, some nurses continue to use screening measures for depression in their clinical practice [ 63 ]. Similarly, case managers in Stolee et al. [ 55 ] stated that the major change in their assessment practice was greater consistency in the use of assessment tools. Smith et al. [ 62 ] reported a shift in practice toward incorporating more detailed information about patients’ impairments and implementing supportive strategies, and in Marcus et al. [ 53 ], communication of depression screening results to patients, physicians, or mental health specialists became a standard protocol. Landi et al. [ 64 ] reported that training was proven feasible and may be implemented on a broader scale, and Luptak et al. [ 52 ] outlined an implementation period of the ADAPT—Assuring Depression Assessment and Proactive Treatment protocol for depression care in rural healthcare—with the potential to achieve the outlined goals in various clinical settings [ 52 ]. Delaney et al. [ 16 ] reported that project participants were interested in implementing the program in their homecare setting and developed a train-the-trainer model. Abbasi et al. [ 57 ] provided results and experiences regarding the Seniors Community Hub (SCH) through the ADKAR (awareness, desire, knowledge, ability, reinforcement) evaluation framework to assist others interested in implementing a similar integrated care model [ 57 ]. Quinlan and Ryer [ 43 ] stated that fall assessment practices are currently implemented and continuous; similarly, Quijano et al. [ 42 ] reported that depression interventions continue to be offered by participating agency offices. On the other hand, Butler and Quayle [ 63 ] noted the challenge of implementing assessment tools due to competing demands such as holidays, working part-time or being too busy, and Sin et al. [ 67 ] outlined one participant with difficulties in applying new knowledge owing to manpower shortages and constraints in time and space. Outcomes for older adults following the health needs assessment trainingSeven studies [ 42 , 43 , 50 , 53 , 57 , 66 , 68 ] detailed outcomes for older adults following health needs assessment training for healthcare professionals. These outcomes included appropriate referrals, tailored interventions, fall prevention, symptom reduction, and improved overall function. Bruce et al. [ 50 ] highlighted that depressed older adults in the intervention group were more likely to receive appropriate referrals for mental health evaluation [ 50 ], aligning with findings where a minimal intervention significantly increased the detection of depression and further referrals to general practitioners [ 68 ]. The findings in two studies demonstrated that patients were referred to tailored resources designed to address their identified problems [ 53 , 57 ]. Furthermore, Quijano et al. [ 42 ] revealed that older adults’ awareness of seeking help and the significance of physical activity for maintaining health improved. Quinlan and Ryer [ 43 ] stated that after providing care plans to 83 older adults, most implemented fall prevention strategies during a two-week follow-up call with 29 older adults, with only one fall reported. Piau et al. [ 66 ] identified the main causes of frailty and reported effective intervention recommendations and referrals [ 66 ]. Most physicians in Stolee et al. [ 55 ] reported better general function for older adults due to comprehensive geriatric assessment. Findings in two studies [ 42 , 57 ] documented reductions in depression severity at the follow-up assessment due to appropriate referrals and interventions [ 42 , 57 ], and significantly more older adults felt better and experienced pain reduction, followed by increased activity [ 42 ]. Additionally, Abbasi et al. [ 57 ] reported a slight improvement in health-related quality of life, including mobility, usual activities, pain/discomfort, and anxiety and depression, suggesting enhanced function [ 57 ]. This scoping review provides insights into training interventions for healthcare professionals assessing the physical, mental, and social health needs of older adults living at home. The analysis of 23 studies revealed that nearly all training interventions used a multifaceted training strategy combining teacher-driven and participant-engaging pedagogical approaches to teach healthcare professionals theoretical and practical knowledge. Health needs assessment training focuses on the skills needed to conduct single or multiple health needs assessments in older adults. Interprofessional collaboration was an essential part of most training interventions. Multiple studies noted that participants were satisfied with the training content and had increased confidence and competencies in health needs assessment and care planning. Studies have also reported a shift in work practices for health care professionals and some included results have shown improved health outcomes for older adults. Our study revealed that most of the included studies blended the use of teacher-driven and participant-engaging pedagogical approaches [ 16 , 42 , 43 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 67 , 68 ]. These approaches provide participants with confidence and competencies in health needs assessment [ 16 , 41 , 42 , 51 , 52 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 62 , 63 , 64 , 65 , 66 , 67 , 68 ]. Skilled healthcare professionals are crucial in facilitating the implementation of health assessments for older adults [ 69 ]. Lectures can be highly effective for learning, especially when they stimulate thinking and active engagement. Their effectiveness depends on the lecturer’s skill and can be improved by incorporating learner feedback, performance results, self-reflection, and peer feedback [ 70 ]. Another way to improve lecture quality is by including interactive elements such as practical skill training, following John Dewey’s “learning by doing” philosophy [ 32 ]. In our review, we identified fifteen studies that utilized participant-engaging approaches such as skills training, role-playing, simulations, hands-on training in real-world settings [ 16 , 42 , 43 , 51 , 52 , 54 , 55 , 57 , 58 , 59 , 60 , 62 , 63 , 64 , 65 ], and sixteen studies employed discussion, questioning and coaching [ 43 , 51 , 52 , 53 , 54 , 55 , 56 , 58 , 59 , 60 , 61 , 63 , 64 , 65 , 67 , 68 ]. The integration of teacher-driven sessions, interactive training, and knowledge exchange resembles simulation training, which typically includes briefing, simulation exercises, and debriefing phases. These phases allow participants to reflect, enhance their learning, and deepen their educational experience [ 71 ]. Debriefing is a valuable tool for reflecting on and discussing experiences in training and real-world settings. This helps individuals and teams identify strengths, areas for improvement, and lessons learned, thereby enhancing learning and future performance [ 72 ]. However, effective debriefing relies on facilitators with strong skills to maximize learning outcomes [ 73 ]. The WHO advocates interprofessional simulation training to enhance healthcare professionals’ competencies and improve patient outcomes [ 2 ]. Even if several studies combined teacher-driven approaches, interactive training and knowledge exchange, our review included only one study utilizing simulation training [ 62 ]. Health needs assessment training for interprofessional teams was evident in eight of the studies included in our review [ 51 , 55 , 57 , 58 , 59 , 61 , 64 , 65 ]. Such training has been proven to provide valuable insights into the health of older adults, leading to improved care delivery [ 74 , 75 ], improved patient outcomes [ 76 ] and reduced hospitalization [ 74 ]. It can improve conflict management skills and team functioning [ 76 ] and play a critical role in equitably distributing community service resources [ 55 ]. Interprofessional simulation training is an engaging method for training clinical skills, procedures, teamwork, and communication in a safe, realistic environment [ 77 ]. It promotes critical thinking, reflection [ 78 ], and effective learning [ 79 ] enhancing the application of knowledge in clinical practice [ 80 ]. The use of participant engaging pedagogical approaches aligns with the sociocultural view of training, which emphasizes active engagement and collaboration in the learning process. It enables knowledge exchange and reflection, and participants can integrate their experiences with new information, internalize it, and construct new knowledge [ 32 , 81 ]. Practical training such as simulations, can push participants out of their comfort zones, foster collaborative learning and enrich the educational experience [ 82 ]. However, to achieve optimal learning, it is crucial to balance skill development with an appropriate level of challenge as learners acquire new concepts. At the same time, temporary support from more experienced learners should be available. This balance is known as the zone of proximal development, which represents the space between a learner’s current skill level and their potential skill level with guidance. Tasks within this zone promote growth [ 83 ]. Our review reports a distinction in training content with a focus on assessing single versus multiple health needs in older adults. Ten studies [ 16 , 41 , 52 , 53 , 54 , 58 , 59 , 60 , 63 , 68 ] focused solely on assessing depression. There is a strong correlation between late-life depression and reduced quality of life, as well as comorbidities such as physical illness, disability [ 58 , 84 ] and physical frailty [ 85 , 86 ]. However, single health need assessment training may inadvertently lead to the overlooking of broader health needs among older adults. A multiple health assessment of older adults is recommended [ 7 ], as it can serve as the foundation for developing holistic interventions to enhance overall health [ 10 , 12 , 87 , 88 , 89 ], promote health [ 90 ], foster positive health behaviors [ 91 ], and reduce frailty [ 92 , 93 ]. Our review included eight studies [ 42 , 51 , 55 , 56 , 57 , 61 , 64 , 66 ] providing training in physical, cognitive, mental, and social health needs assessment, alongside care planning on the basis of these assessments. Research indicates that both healthcare professionals and frail older adults participating in an interdisciplinary care approach were satisfied with the improved structure of care and appreciated the emphasis on health promotion [ 94 ]. On the other hand, a comprehensive health needs assessment is a multifaceted and complex intervention, with uncertainties surrounding its effectiveness and underlying mechanisms [ 95 ]. Some research findings indicate that there is no conclusive evidence that it reduces disability, prevents functional decline [ 96 ], impacts mortality, or supports independent living in older adults [ 97 ]. These results underscore the complexity and challenges in conducting and implementing comprehensive health needs assessments and tailoring interventions to promote health in older adults. Our review revealed that almost all [ 16 , 41 , 42 , 43 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 63 , 64 , 65 , 66 , 67 , 68 ] health needs assessment training programs included the use of assessment tools or checklists, leading to the identification of health needs. Only one of these studies reported that participants relied more on observation than on direct questioning when assessing depression [ 54 ]. Additionally, another study found that healthcare professionals using assessment tools felt that this approach led to asking overly personal and intrusive questions without first establishing trust or explaining the purpose of the assessment [ 98 ]. On the other hand, some older adults reported that using assessment tools made it difficult to discuss issues outside the predefined domains of the comprehensive health needs assessment [ 99 ]. Research indicates that current assessment practices heavily rely on professional judgment and intuition, and healthcare professionals in community settings often lack adequate knowledge and training regarding the health needs assessment of older adults [ 22 , 100 ]. This can be seen as problematic because these professionals are ideally positioned to assess older adults early in their health trajectories [ 105 ]. Proper assessment in these settings can facilitate the early recognition of functional decline [ 101 , 102 ] and vulnerability, enable timely intervention to mitigate frailty’s adverse effects [ 105 ], and support effective care planning [ 64 ]. Even if several healthcare professionals have endorsed the integration of frailty assessment tools into primary care [ 22 ], they need a simple, efficient assessment tool [ 105 ] that empowers them to identify older adults’ health needs [ 9 , 88 , 103 , 104 ]. This is particularly critical due to the essential role that assessments play in equitably distributing community service resources [ 105 ]. As such, this review underscores the importance of educating healthcare professionals in community care to effectively assess the physical, mental, and social health needs of older adults. Furthermore, understanding the learning process of healthcare professionals [ 78 ], evaluating the effects of training [ 106 ], and establishing evidence-based standards for skills training are crucial for high-quality teaching [ 107 ]. Additionally, further research is necessary to assess the feasibility, effectiveness, and acceptability of interprofessional interventions targeting multiple health needs aimed at health promotion [ 90 ] and experiences using comprehensive health assessment tools [ 108 ]. Methodological considerationsThis review included studies employing various methods to obtain comprehensive insights into training healthcare professionals in assessing the health needs of older adults living at home [ 47 ]. We utilized a validated mixed-methods appraisal tool to assess the quality of the included studies [ 47 , 49 ]. We did not include reporting on screening questions regarding the clarity of the research question or whether the collected data addressed the research questions, as our review focused exclusively on empirical studies. Additionally, we chose not to calculate an overall score from the ratings of each criterion, as this practice is discouraged. We provide an overview of each study’s quality by presenting the ratings of each criterion [ 49 ]. Our findings revealed that only one study met all the quality criteria, fifteen studies met four criteria, three studies met three criteria, and four studies met only one criterion. High-quality studies employ rigorous and robust methods, leading to reliable and valid findings [ 109 ]. While most studies met 3–4 quality criteria, they provide a relatively strong evidence base and offer valuable insights, although some concerns remain. Several studies did not meet the quality criteria for nonresponse bias or complete outcome data. It is crucial to describe and evaluate a low response rate for its potential impact, as this can limit the generalizability of findings [ 110 ]. Many studies also failed to account for confounders in their design and analysis. Confounding factors may bias results by distorting the interpretation of findings [ 49 ], masking actual associations or creating false associations, potentially leading to incorrect conclusions [ 111 ]. The randomization of study subjects and rigorous statistical analyses can mitigate the impact of confounding variables [ 112 ]. Nonetheless, conducting a quality assessment increases awareness of these biases and limitations, thereby enhancing our confidence in the study findings. Strengths and limitationsOur scoping review has several limitations. Initially, our search strategy involved the use of six databases and various relevant search terms related to training healthcare professionals in assessing the health needs of older adults. We excluded gray literature to focus on mapping existing published research and identifying any research gaps. The search was conducted by an experienced librarian. Despite our efforts to comprehensively map the research literature, we may have overlooked some studies. Second, our exclusion criteria, which encompassed, for example, general practitioners, students, and institutional settings, restricted the scope of the study. Additionally, we focused on health needs assessment, excluding studies that assessed the environment, an important factor in enabling older adults to stay at home as long as possible. However, based on the findings and limitations of the included studies, we believe our review provides valuable insights into the research context. These findings can inform future research, practice, policymaking, and the development of training programs for healthcare professionals in community settings to assess older adults’ health needs. Healthcare professionals require training in assessing physical, mental, and social health needs in older adults living at home to ensure tailored interventions that enhance their health and independence. Our study revealed that healthcare professionals were satisfied with the combination of participant-engaging and teacher-driven pedagogical approaches when training in physical, mental, and social health needs assessment. Such training is beneficial and strengthens healthcare professionals’ confidence and competency in assessment and care planning for older adults living at home. Additionally, some studies reported that following health needs assessment training, there was a shift in work practices and improved health outcomes for older adults. We suggest that health needs assessment training programs are valuable for improving health and care for older adults living at home and contribute to increased sustainability in healthcare. Furthermore, we propose additional research on interprofessional simulation training for the structured assessment of multiple health needs in older adults, ensuring comprehensive coverage of all significant health issues in these assessments. We also recommend research on the implementation of such assessments and health promoting interventions. Data availabilityNo datasets were generated or analysed during the current study. Avallone M, Perweiler E, Pacetti S. Using the 4Ms framework to teach geriatric competencies in a community clinical experience. Nurs Forum [Internet]. 2021; 56(1):[83 – 8 pp.]. https://doi.org/10.1111/nuf.12511 World Health Organization W. Transforming and scaling up health professionals’ education and training. World Health Organization guidelines 2013. Geneva: World Health Organization; 2013. p. 122. Google Scholar World Health Organization W. Ageing and health Geneva: World Health Organization, WHO. 2022 [ https://www.who.int/news-room/fact-sheets/detail/ageing-and-health Thiyagarajan JA, Araujo de Carvalho I, Peña-Rosas JP, Chadha S, Mariotti SP, Dua T et al. Redesigning care for older people to preserve physical and mental capacity: WHO guidelines on community-level interventions in integrated care. PLoS Med [Internet]. 2019; 16(10):[e1002948-e pp.]. https://doi.org/10.1371/journal.pmed.1002948 World Health Organization W. Integrated care for older people (ICOPE): Guidance for person-centred assessment and pathways in primary care Geneva. World Health Organization,;; 2019. (WHO/FWC/ALC/19.1). Wright J, Williams R, Wilkinson JR. Development and importance of health needs assessment. Bmj [Internet]. 1998; 316(7140):[1310-3 pp.]. https://doi.org/10.1136/bmj.316.7140.1310 Ravaghi H, Guisset A-L, Elfeky S, Nasir N, Khani S, Ahmadnezhad E, Abdi Z. A scoping review of community health needs and assets assessment: concepts, rationale, tools and uses. BMC Health Services Research [Internet]. 2023; 23(1):[44 p.]. https://doi.org/10.1186/s12913-022-08983-3 Karlsson S, Ridbäck A, Brobeck E, Norell Pejner M. Health Promotion Practices in Nursing for Elderly Persons in Municipal Home Care: An Integrative Literature Review. Home Health Care Management & Practice [Internet]. 2020; 32(1):[53–61 pp.]. https://doi.org/10.1177/1084822319863308 Schain A, Rees C, Medina C, Eyler R, Glenney S, Rodko E et al. Reducing Risks for Older Adults With an Interprofessional Community-Academic Partnership: A Case Study. Home Healthc Now [Internet]. 2018; 36(6):[362-8 pp.]. https://doi.org/10.1097/nhh.0000000000000696 van Assen MALM, Helmink JHM, Gobbens RJJ. Associations between lifestyle factors and multidimensional frailty: a cross-sectional study among community-dwelling older people. BMC Geriatrics [Internet]. 2022; 22(1):[1–13 pp.]. https://doi.org/10.1186/s12877-021-02704-x Kennedy MA, Hatchell KE, DiMilia PR, Kelly SM, Blunt HB, Bagley PJ et al. Community health worker interventions for older adults with complex health needs: A systematic review. Journal of the American Geriatrics Society [Internet]. 2021; 69(6):[1670-82 pp.]. https://doi.org/10.1111/jgs.17078 de Carvalho IA, Epping-Jordan J, Pot AM, Kelley E, Toro N, Thiyagarajan JA, Beard JR. Organizing integrated health-care services to meet older people’s needs. Bull World Health Organ [Internet]. 2017; 95(11):[756 – 63 pp.]. https://doi.org/10.2471/BLT.16.187617 Rusli KDB, Tan AJQ, Ong SF, Speed S, Lau Y, Liaw SY. Home-based nursing care competencies: A scoping review. Journal of Clinical Nursing [Internet]. 2023; 32(9–10):[1723-37 pp.]. https://doi.org/10.1111/jocn.16169 World Health Organization W. Integrated care for older people (ICOPE) Geneva: World Health Organization, WHO. 2024 [ https://www.who.int/teams/maternal-newborn-child-adolescent-health-and-ageing/ageing-and-health/integrated-care-for-older-people-icope Adhikari P. Geriatric health care in India -Unmet needs and the way forward. Archives of Medicine and Health Sciences [Internet]. 2017; 5:[112 p.]. https://doi.org/10.4103/2321-4848.208215 Delaney C, Fortinsky RH, Doonan L, Grimes RLW, Terra-Lee P, Rosenberg S, Bruce ML. Depression Screening and Interventions for Older Home Health Care Patients: Program Design and Training Outcomes for a Train-the-Trainer Model. Home Health Care Management & Practice [Internet]. 2011 2011/12/01; 23(6):[435 – 45 pp.]. https://doi.org/10.1177/1084822311405459 Briskie Semeniuk P, Bier N, Couture M, Vachon B, Belchior P. Perceived knowledge needs of occupational therapists for evaluating seniors with cognitive impairments. Physical & Occupational Therapy in Geriatrics [Internet]. 2023; 41(4):[515 – 37 pp.]. https://doi.org/10.1080/02703181.2023.2180566 Galvez-Hernandez P, González-de Paz L, Muntaner C. Primary care-based interventions addressing social isolation and loneliness in older people: a scoping review. BMJ Open [Internet]. 2022; 12(2):[e057729-e pp.]. https://doi.org/10.1136/bmjopen-2021-057729 Mathisen TS, Eilertsen G, Ormstad H, Falkenberg HK. Barriers and facilitators to the implementation of a structured visual assessment after stroke in municipal health care services. BMC Health Services Research. 2021;21(1):497. https://doi.org/10.1186/s12913-021-06467-4 Li S, Zhang J, Liu Y, Wang A-P, Qiu G. Survey of the demand for care services for older people and the training needs of their care workers: a cross-sectional study in Northeast China. BMC Nurs [Internet]. 2022; 21(1):[25- pp.]. https://doi.org/10.1186/s12912-022-00809-1 Fulmer T, Reuben DB, Auerbach J, Fick DM, Galambos C, Johnson KS, Actualizing Better Health And Health Care For Older Adults. Health Affairs [Internet]. 2021; 40(2):[219 – 25 pp.]. https://doi.org/10.1377/hlthaff.2020.01470 Kennedy F, Galvin R, Horgan NF. Managing frailty in an Irish primary care setting: A qualitative study of perspectives of healthcare professionals and frail older patients. Journal of Frailty, Sarcopenia & Falls [Internet]. 2021; 6(1):[1–8 pp.]. https://doi.org/10.22540/JFSF-06-001 Frost R, Robinson K, Gordon AL, Caldeira de Melo R, Villas Boas PJF, Azevedo PS et al. Identifying and Managing Frailty: A Survey of UK Healthcare Professionals. Journal of Applied Gerontology [Internet]. 2023; 43(4):[402 – 12 pp.]. https://doi.org/10.1177/07334648231206321 Gobbens RJ, Luijkx KG, Wijnen-Sponselee MT, Schols JM. Toward a conceptual definition of frail community dwelling older people. Nursing Outlook [Internet]. 20102010/03/01/; 58(2):[76–86 pp.]. https://doi.org/10.1016/j.outlook.2009.09.005 Salas E, Tannenbaum SI, Kraiger K, Smith-Jentsch KA. The Science of Training and Development in Organizations:What Matters in Practice. Psychological Science in the Public Interest [Internet]. 2012; 13(2):[74–101 pp.]. https://doi.org/10.1177/1529100612436661 Armstrong M, Taylor S. Armstrong’s handbook of human resource management practice: A guide to the theory and practice of people management. Kogan Page; 2023. World Health Organization W. Building a skilled health workforce World Health Organization, Europe: World Health Organization, WHO. 2024. https://www.who.int/europe/activities/building-a-skilled-health-workforce Ganann R, Weeres A, Lam A, Chung H, Valaitis R. Optimization of home care nurses in Canada: A scoping review. Health & Social Care in the Community [Internet]. 2019; 27(5):[e604-e21 pp.]. https://doi.org/10.1111/hsc.12797 Reeves S, Lewin S, Espin S, Zwarenstein M. Interprofessional teamwork for health and social care. Wiley; 2011. Cunningham N, Cowie J, Watchman K, Methven K. Understanding the training and education needs of homecare workers supporting people with dementia and cancer: A systematic review of reviews. Dementia (London) [Internet]. 2020; 19(8):[2780 – 803 pp.]. https://doi.org/10.1177/1471301219859781 Kolb DA. Experiential learning: Experience as the source of learning and development. Second edition ed. Upper Saddle River, New Jersey Pearson Education, Inc.; 2015. Säljö R, Moen S. Læring og kulturelle redskaper: om læreprosesser og den kollektive hukommelsen. Oslo: Cappelen akademisk forl.; 2006. Myrvang T, Rokstad AMM. Simulering og ferdighetstrening kombinert med bruk av systematiske verktøy i sykehjem – en kvalitativ studie av sykepleieres erfaringer. Nordisk sygeplejeforskning [Internet]. 2022; 12(2):[1–14 pp.]. https://doi.org/10.18261/nsf.12.2.1 Peters M, Godfrey C, McInerney P, Munn Z, Tricco A, Khalil H. In: E A, Munn Z, editors. Chapter 11: scoping reviews. JBI Manual for Evidence Synthesis: JBI; 2020. Arksey H, O’Malley L. Scoping studies: towards a methodological framework. International journal of social research methodology [Internet]. 2005; 8(1):[19–32 pp.]. https://doi.org/10.1080/1364557032000119616 Peters MDJ, Marnie C, Tricco AC, Pollock D, Munn Z, Alexander L, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synthesis [Internet]. 2020;18(10):2119. 26 pp.]. Article Google Scholar Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Annals of internal medicine [Internet]. 2018; 169(7):[467 – 73 pp.]. https://www.acpjournals.org/doi/full/ https://doi.org/10.7326/M18-0850 Singh S, Bajorek B. Defining ‘elderly’ in clinical practice guidelines for pharmacotherapy. Pharm Pract (Granada) [Internet]. 2014; 12(4):[489 p.]. https://doi.org/10.4321/s1886-36552014000400007 Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ [Internet]. 2009; 339(7716):[332-6 pp.]. https://doi.org/10.1136/bmj.b2535 Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Systematic reviews [Internet]. 2016; 5(1):1–10 pp.]. https://link.springer.com/article/ https://doi.org/10.1186/s13643-016-0384-4 Mayall E, Oathamshaw S, Lovell K, Pusey H. Development and piloting of a multidisciplinary training course for detecting and managing depression in the older person. Journal of Psychiatric and Mental Health Nursing [Internet]. 2004; 11(2):[165 – 71 pp.]. https://doi.org/10.1111/j.1365-2850.2003.00702.x Quijano LM, Stanley MA, Petersen NJ, Casado BL, Steinberg EH, Cully JA, Wilson NL. Healthy IDEAS:A Depression Intervention Delivered by Community-Based Case Managers Serving Older Adults. Journal of Applied Gerontology [Internet]. 2007; 26(2):[139 – 56 pp.]. https://doi.org/10.1177/0733464807299354 Quinlan S, Ryer S. Implementing a Fall Prevention Initiative in Nurse-Facilitated Annual Wellness Visits: A Quality Improvement Project. Journal of Nursing Care Quality [Internet]. 2023; 38(3):[243 – 50 pp.]. https://doi.org/10.1097/NCQ.0000000000000690 Pollock D, Peters MDJ, Khalil H, McInerney P, Alexander L, Tricco AC et al. Recommendations for the extraction, analysis, and presentation of results in scoping reviews. JBI Evidence Synthesis [Internet]. 2023; 21(3):[520 – 32 pp.]. https://doi.org/10.11124/jbies-22-00123 Braun V, Clarke V. Thematic analysis: a practical guide. Los Angeles, California: SAGE; 2022. Book Google Scholar Phillips M, Lu J. A quick look at NVivo. Journal of Electronic Resources Librarianship [Internet]. 2018 2018/04/03; 30(2):[104-6 pp.]. https://doi.org/10.1080/1941126X.2018.1465535 Pace R, Pluye P, Bartlett G, Macaulay AC, Salsberg J, Jagosh J, Seller R. Testing the reliability and efficiency of the pilot Mixed Methods Appraisal Tool (MMAT) for systematic mixed studies review. Int J Nurs Stud [Internet]. 2012; 49(1):[47–53 pp.]. https://doi.org/10.1016/j.ijnurstu.2011.07.002 Kazi MR, Chowdhury N, Chowdhury M, Turin TC. Conducting comprehensive scoping reviews to systematically capture the landscape of a subject matter. Population Medicine [Internet]. 2021; 3(December):[1–9 pp.]. https://doi.org/10.18332/popmed/143831 Hong QN, Pluye P, Fàbregues S, Bartlett G, Boardman F, Cargo M et al. Mixed methods appraisal tool (MMAT), version 2018. Registration of copyright [Internet]. 2018; 1148552(10). Bruce ML, Brown EL, Raue PJ, Mlodzianowski AE, Meyers BS, Leon AC et al. A randomized trial of depression assessment intervention in home health care. J Am Geriatr Soc [Internet]. 2007; 55(11):[1793 – 800 pp.]. Couser S, Moehrlin BA, Deitrich C, Hess L. Expanding community health nursing roles to meet health-care needs of frail elderly. An adult learning model. J Community Health Nurs [Internet]. 1990;7(1):3–13. pp.]. Luptak M, Kaas MJ, Artz M, McCarthy T, Project ADAPT. A program to assess depression and provide proactive treatment in rural areas. Gerontologist [Internet]. 2008; 48(4):[542-8 pp.]. https://doi.org/10.1093/geront/48.4.542 Marcus P, Kennedy GJ, Wetherbee C, Korenblatt J, Dorta H, Lantz MS. Training professional home care staff to help reduce depression in elderly home care recipients. Clin Geriatr [Internet]. 2006; 14(7):[13 – 6 pp.]. Brown EL, Raue PJ, Roos BA, Sheeran T, Bruce ML. Training nursing staff to recognize depression in home healthcare. J Am Geriatr Soc [Internet]. 2010; 58(1):[122-8 pp.]. https://doi.org/10.1111/j.1532-5415.2009.02626.x Stolee P, Patterson ML, Wiancko DC, Esbaugh J, Arcese ZA, Vinke AM et al. An enhanced role in comprehensive geriatric assessment for community-nurse case managers. Can J Aging [Internet]. 2003; 22(2):[177 – 84 pp.]. Brymer C, Cormack C, Spezowka K. Improving the care of the elderly in a rural county through education. Gerontology & Geriatrics Education [Internet]. 1998; 19(1):[55–64 pp.]. https://doi.org/10.1300/j021v19n01_05 Abbasi M, Khera S, Dabravolskaj J, Chevalier B, Parker K. The seniors’ community hub: An integrated model of care for the identification and management of frailty in primary care. Geriatrics (Switzerland) [Internet]. 2021; 6(1):[1–15 pp.]. https://doi.org/10.3390/geriatrics6010018 McCabe MP, Russo S, Mellor D, Davison TE, George K. Effectiveness of a training program for carers to recognize depression among older people. International Journal of Geriatric Psychiatry [Internet]. 2008; 23(12):[1290-6 pp.]. https://doi.org/10.1002/gps.2067 Mellor D, Kiehne M, McCabe MP, Davison TE, Karantzas G, George K. An evaluation of the beyondblue Depression Training Program for aged care workers. International Psychogeriatrics [Internet]. 2010; 22(6):[927 – 37 pp.]. https://doi.org/10.1017/S1041610210000153 Nunn R, Annells M, Sims J. Screening for depression in older district nursing clients: feasibility study. British Journal of Community Nursing [Internet]. 2007; 12(3):[108 – 14 pp.]. https://doi.org/10.12968/bjcn.2007.12.3.23037 Naughton C, Hayes N, Zahran Z, Norton C, Lee G, Fitzpatrick JM et al. The development of the Older Person’s Nurse Fellowship: Education concept to delivery. Nurse Education Today [Internet]. 2016; 44:[1–7 pp.]. https://doi.org/10.1016/j.nedt.2016.04.022 Smith A, Shepherd A, Macaden L, Macleod KL. Raising awareness of sensory impairment among community nurses: a brief intervention in a remote island setting. Rural & Remote Health [Internet]. 2018 08; 18(3):[4548 p.]. https://doi.org/10.22605/RRH4548 Butler M, Quayle E. Training primary care nurses in late-life depression: knowledge, attitude and practice changes. International Journal of Older People Nursing [Internet]. 2007 2023-10-26; 2(1):[25–35 pp.]. https://doi.org/10.1111/j.1748-3743.2007.00054.x Landi F, Sgadari A, Cipriani L, Castellani M, Pahor M, Carbonin PU, Bernabei R. A simple program to train case managers in community elderly care. Aging Clinical and Experimental Research [Internet]. 1996; 8(3):[211-8 pp.]. https://doi.org/10.1007/bf03339679 Neto JBF, de Moraes GLA, de Souza Aredes J, Giacomin KC, de Melo LP, Sempe L, Lloyd-Sherlock P. Building the capacity of community health workers to support health and social care for dependent older people in Latin America: a pilot study in Fortaleza, Brazil. BMC Geriatrics [Internet]. 2021 10 02; 21(1):[526 p.]. https://doi.org/10.1186/s12877-021-02477-3 Piau A, Sourdet S, Toulza O, Bernon C, Tavassoli N, Nourhashemi F. Frailty Management in Community-Dwelling Older Adults: Initial Results of a Trained Nurses Program. Journal of the American Medical Directors Association [Internet]. 2019; 20(5):[642-3 pp.]. https://doi.org/10.1016/j.jamda.2018.11.011 Sin GL, Yeo D, Koh HJ, Lee J, Ng LL. Training eldercare workers in mental healthcare. Singapore Med J [Internet]. 2018 01; 59(1):[28–32 pp.]. https://doi.org/10.11622/smedj.2017052 Van Daele T, Vansteenwegen D, Hermans D, Van den Bergh O, Van Audenhove C. Home nurses and patient depression. Attitudes, competences and the effects of a minimal intervention. Journal of Advanced Nursing (John Wiley & Sons, Inc) [Internet]. 2015; 71(1):[126 – 35 pp.]. https://doi.org/10.1111/jan.12476 King AII, Boyd ML, Dagley L, Raphael DL. Implementation of a gerontology nurse specialist role in primary health care: Health professional and older adult perspectives. J Clin Nurs [Internet]. 2018; 27(3–4):[807 – 18 pp.]. https://doi.org/10.1111/jocn.14110 Di Leonardi BC. Tips for facilitating learning: the lecture deserves some respect. J Contin Educ Nurs [Internet]. 2007 Jul-Aug; 38(4):[154 – 61; quiz 62 – 3, 75 pp.]. https://doi.org/10.3928/00220124-20070701-09 Dieckmann P. Using Simulations for Education, Training and Research. Pabst Science; 2009. Tannenbaum SI, Cerasoli CP. Do Team and Individual Debriefs Enhance Performance? A Meta-Analysis. Human Factors [Internet]. 2013; 55(1):[231 – 45 pp.]. https://doi.org/10.1177/0018720812448394 Tannenbaum SI, Greilich PE. The debrief imperative: building teaming competencies and team effectiveness. BMJ Quality & Safety [Internet]. 2023; 32(3):[125-8 pp.]. https://doi.org/10.1136/bmjqs-2022-015259 Montano AR, Shellman J, Malcolm M. Outcomes From an Interprofessional Geriatric Outreach and Training Program. Innov Aging [Internet]. 2022; 6(6):[igac044 p.]. https://doi.org/10.1093/geroni/igac044 Ostertag S, Bosic-Reiniger J, Migliaccio C, Zins R. Promoting Older Adult Health with Interprofessional Education through Community Based Health Screening. Int J Environ Res Public Health [Internet]. 2022; 19(11). https://doi.org/10.3390/ijerph19116513 Park MK, Taylor JA, Biernot J, Martin DJ, The Virtual Geriatric Assessment Interdisciplinary Team Project.: Interprofessional Geriatric Training Against the Backdrop of COVID-19. Journal of Applied Gerontology [Internet]. 2024; 0(0):[07334648241234496 p.]. https://doi.org/10.1177/07334648241234496 Decker S, Sportsman S, Puetz L, Billings L. The Evolution of Simulation and Its Contribution to Competency. The Journal of Continuing Education in Nursing [Internet]. 2008; 39(2):[74–80 pp.]. Available from: https://doi.org/10.3928/00220124-20080201-06 Rutherford-Hemming T. Simulation Methodology in Nursing Education and Adult Learning Theory. Adult Learning [Internet]. 2012; 23(3):[129 – 37 pp.]. https://doi.org/10.1177/1045159512452848 Husebø SE, O’Regan S, Nestel D. Reflective practice and its role in simulation. Clinical Simulation in Nursing [Internet]. 2015; 11(8):[368 – 75 pp.]. https://doi-org.ezproxy.uis.no/ https://doi.org/10.1016/j.ecns.2015.04.005 Acosta DJ, Rinfret A, Plant J, Hsu AT. Using Patient Simulation to Promote Best Practices in Fall Prevention and Postfall Assessment in Nursing Homes. Journal of Nursing Care Quality [Internet]. 2022; 37(2):[117 – 22 pp.]. https://doi.org/10.1097/NCQ.0000000000000599 Vygotskij LS, Roster MT, Bielenberg T-J, Skodvin A, Kozulin A. Tenkning og tale. Oslo: Gyldendal akademisk; 2001. Owen L, Steel A, Goffe K, Pleming J, Sampson EL. A multidisciplinary simulation programme to improve advance care planning skills and engagement across primary and secondary care. Clinical Medicine. 2022; 22(1):[51 – 7 pp.]. https://doi.org/10.7861/clinmed.2021-0240 Vygotskij LS, Cole MG, John-Steiner V, Scribner S, Souberman E. Mind in society: the development of higher psychological processes. Cambridge, Mass: Harvard University Press; 1978. Nelson JC, Clary CM, Leon AC, Schneider LS. Symptoms of Late-Life Depression: Frequency and Change During Treatment. The American Journal of Geriatric Psychiatry [Internet]. 2005 Jun 2005; 13(6):[520-6 pp.]. http://ezproxy.uis.no/login?url=https://www-proquest-com.ezproxy.uis.no/scholarly-journals/symptoms-late-life-depression-frequency-change/docview/195983951/se-2 Mulasso A, Roppolo M, Giannotta F, Rabaglietti E. Associations of frailty and psychosocial factors with autonomy in daily activities: a cross-sectional study in Italian community-dwelling older adults. Clinical Interventions in Aging [Internet]. 2016 2023-11-22; 11:[37–45 pp.]. https://doi.org/10.2147/CIA.S95162 Oyon J, Serra-Prat M, Ferrer M, Llinares A, Pastor N, Limón E et al. Psychosocial factors associated with frailty in the community-dwelling aged population with depression. A cross-sectional study. Atención Primaria [Internet]. 2021 2021/05/01/; 53(5):[102048 p.]. https://doi.org/10.1016/j.aprim.2021.102048 Agredano RS, Masclans JG, Guix-Comellas EM, Fraile VM, Sarria-Guerrero JA, Pola MS, Fabrellas N. Older Adults With Complex Chronic Conditions Who Receive Care at Home: The Importance of Primary Care Assessment. Journal of gerontological nursing [Internet]. 2021; 47(11):[31 – 8 pp.]. https://doi.org/10.3928/00989134-20211013-02 Seematter-Bagnoud L, Büla C. Brief assessments and screening for geriatric conditions in older primary care patients: a pragmatic approach. Public Health Rev [Internet]. 2018; 39:[8 p.]. https://doi.org/10.1186/s40985-018-0086-7 Piccoliori G, Gerolimon E, Abholz HH. Geriatric assessment in general practice using a screening instrument: is it worth the effort? Results of a South Tyrol Study. Age Ageing [Internet]. 2008; 37(6):[647 – 52 pp.]. https://doi.org/10.1093/ageing/afn161 Prince MJ, Acosta D, Guerra M, Huang Y, Jacob KS, Jimenez-Velazquez IZ et al. Intrinsic capacity and its associations with incident dependence and mortality in 10/66 Dementia Research Group studies in Latin America, India, and China: A population-based cohort study. PLoS Med [Internet]. 2021; 18(9):[e1003097-e pp.]. https://doi.org/10.1371/journal.pmed.1003097 Seah B, Kowitlawakul Y, Jiang Y, Ang E, Chokkanathan S, Wang W. A review on healthy ageing interventions addressing physical, mental and social health of independent community-dwelling older adults. Geriatric Nursing [Internet]. 2019; 40(1):[37–50 pp.]. https://doi.org/10.1016/j.gerinurse.2018.06.002 Macdonald SHF, Travers J, Éidín Ní S, Bailey J, Romero-Ortuno R, Keyes M et al. Primary care interventions to address physical frailty among community-dwelling adults aged 60 years or older: A meta-analysis. PLoS One [Internet]. 2020; 15(2). https://doi.org/10.1371/journal.pone.0228821 Li C-M, Chen C-Y, Li C-Y, Wang W-D, Wu S-C. The effectiveness of a comprehensive geriatric assessment intervention program for frailty in community-dwelling older people: a randomized, controlled trial. Archives of Gerontology and Geriatrics [Internet]. 2010; 50:[S39-S42 pp.]. https://doi.org/10.1016/S0167-4943(10)70011-X Metzelthin SF, Daniëls R, van Rossum E, Cox K, Habets H, de Witte LP, Kempen GIJM. A nurse-led interdisciplinary primary care approach to prevent disability among community-dwelling frail older people: A large-scale process evaluation. Int J Nurs Stud [Internet]. 2013; 50(9):[1184-96 pp.]. https://doi.org/10.1016/j.ijnurstu.2012.12.016 Fox ST, Janda M, Hubbard R. Understanding how comprehensive geriatric assessment works: the importance of varied methodological approaches. Aging Clinical and Experimental Research [Internet]. 2023 2023/02/01; 35(2):[417 – 23 pp.]. https://doi.org/10.1007/s40520-022-02305-7 Metzelthin SF, van Rossum E, de Witte LP, Ambergen AW, Hobma SO, Sipers W, Kempen GIJM. Effectiveness of interdisciplinary primary care approach to reduce disability in community dwelling frail older people: cluster randomised controlled trial. BMJ [Internet]. 2013; 347(7926):[12- pp.]. https://doi.org/10.1136/bmj.f5264 Mayo-Wilson E, Grant S, Burton J, Parsons A, Underhill K, Montgomery P. Preventive home visits for mortality, morbidity, and institutionalization in older adults: a systematic review and meta-analysis. PLoS One [Internet]. 2014 PMC3951196]; 9(3):[e89257 p.]. https://doi.org/10.1371/journal.pone.0089257 Lagerin A. District nurses’ experiences of preventive home visits to 75-year-olds in Stockholm: a qualitative study. Primary Health Care Research & Development (Cambridge University Press / UK) [Internet]. 2016; 17(5):[464 – 78 pp.]. https://doi.org/10.1017/S1463423615000560 Rietkerk W, Smit MF, Wynia K, Slaets JPJ, Zuidema SU, Gerritsen DL. Explaining experiences of community-dwelling older adults with a pro-active comprehensive geriatric assessment program - a thorough evaluation by interviews. BMC Geriatr [Internet]. 2019; 19(1):[12 p.]. https://doi.org/10.1186/s12877-018-1025-7 Papadopoulou C, Barrie J, Andrew M, Martin JC, Birt A, Raymond Duffy FJ, Hendry A. Perceptions, practices and educational needs of community nurses to manage frailty. Br J Community Nurs [Internet]. 2021; 26(3):[136 – 42 pp.]. https://doi.org/10.12968/bjcn.2021.26.3.136 Lang D, Hoey C, O’Shea D, Whitty H. National Frailty Education Programme Report: the fundamentals of Frailty. Republic of Ireland: Health Service Executive; 2023. Donoghue OA, O’Shea M, McGarrigle CA, Lang D, Hoey C, Whitty H et al. Translating frailty assessment methodologies and research-based evidence to clinical education and practice. Journal of Aging & Social Policy [Internet]. 2022; 34(4):[537 – 51 pp.]. https://doi-org.ezproxy.uis.no/10.1080/08959420.2020.1777825 Obbia P, Graham C, Duffy FJR, Gobbens RJJ. Preventing frailty in older people: An exploration of primary care professionals’ experiences. Int J Older People Nurs [Internet]. 2020; 15(2):[e12297 p.]. https://doi.org/10.1111/opn.12297 Hoogendijk EO, Afilalo J, Ensrud KE, Kowal P, Onder G, Fried LP. Frailty: implications for clinical practice and public health. Lancet [Internet]. 2019; 394(10206):[1365-75 pp.]. https://doi.org/10.1016/S0140-6736(19)31786-6 Carroll C, Sworn K, Booth A, Tsuchiya A, Maden M, Rosenberg M. Equity in healthcare access and service coverage for older people: a scoping review of the conceptual literature. Integr Healthc J [Internet]. 2022; 4(1):[e000092 p.]. https://doi.org/10.1136/ihj-2021-000092 Dieckmann P. The unexpected and the non-fitting - considering the edges of simulation as social practice. Adv Simul (Lond) [Internet]. 2020; 5(1):[2- pp.]. https://doi.org/10.1186/s41077-020-0120-y Reierson IA, Ravik M, Blomberg K, Bjork IT, Boelenius K, Stenholt BV, Husebo SE. Comparing didactic approaches for practical skills learning in Scandinavian nursing simulation centres: A qualitative comparative study. J Adv Nurs [Internet]. 2024. https://doi.org/10.1111/jan.16150 Stoop A, Lette M, van Gils PF, Nijpels G, Baan CA, de Bruin SR. Comprehensive geriatric assessments in integrated care programs for older people living at home: A scoping review. Health Soc Care Community [Internet]. 2019; 27(5):[e549-e66 pp.]. https://doi.org/10.1111/hsc.12793 Ahmed I, Ishtiaq S. Reliability and validity: Importance in Medical Research. J Pak Med Assoc [Internet]. 2021; 71(10):[2401-6 pp.]. https://doi.org/10.47391/jpma.06-861 Mölenberg FJM, de Vries C, Burdorf A, van Lenthe FJ. A framework for exploring non-response patterns over time in health surveys. BMC Medical Research Methodology [Internet]. 2021 2021/02/18; 21(1):[37 p.]. https://doi.org/10.1186/s12874-021-01221-0 Skelly AC, Dettori JR, Brodt ED. Assessing bias: the importance of considering confounding. Evid Based Spine Care J [Internet]. 2012; 3(1):[9–12 pp.]. https://doi.org/10.1055/s-0031-1298595 Pourhoseingholi MA, Baghestani AR, Vahedi M. How to control confounding effects by statistical analysis. Gastroenterol Hepatol Bed Bench [Internet] 2012 Spring; 5(2):79–83 pp.]. Download references AcknowledgementsThe authors express gratitude to librarian Kari Hølland, Division of Research, Stavanger University Library for performing the systematic literature searches. This article stems from the research project “More good days at home - Advancing health promoting practices in municipal healthcare services for older recipients of homecare” (HEIME), specifically related to Work Package 3, “Simulation and training for health needs assessment in home-living older adults”. HEIME is funded by the Research Council of Norway (grant 320622), University of Southeastern-Norway, University of Stavanger, Stavanger, Horten, Porsgrunn and Nome municipality (2021–2025). Dr. Grethe Eilertsen is the project director. Drs. Siri Tønnessen, Anette Hansen and Professor Marianne Storm are the principal researchers and work package leaders. Open access funding provided by University of Stavanger & Stavanger University Hospital Author informationAuthors and affiliations. Faculty of Health Sciences, Department of Public Health, University of Stavanger, Postbox 8600, Stavanger, 4036, Norway Bente Hamre Larsen & Marianne Storm Faculty of Health Sciences, Department of Quality and Health Technology, University of Stavanger, Stavanger, Norway Dagrunn Nåden Dyrstad & Peter Dieckmann National Centre for Optics, Vision and Eye Care, Faculty of Health and Social Sciences, University of South-Eastern Norway, Kongsberg, Norway Helle K. Falkenberg USN Research Group of Older Peoples’ Health, University of South-Eastern Norway, Drammen, Norway Center for Human Resources and Education, Copenhagen Academy for Medical Education and Simulation (CAMES), Capital Region of Denmark, Copenhagen, Denmark Peter Dieckmann Department of Public Health, Copenhagen University, Copenhagen, Denmark Faculty of Health Sciences and Social Care, Molde University College, Molde, Norway Marianne Storm Research Department, Research Group of Nursing and Health Sciences, Stavanger University Hospital, Stavanger, Norway You can also search for this author in PubMed Google Scholar ContributionsAll authors (BHL, DND, HKF, PD and MS) contributed to the design and development of the study, research questions, and literature search. BHL conducted the literature search in collaboration with MS and research librarian. All authors participated in the screening and quality assessment processes. Data analysis and manuscript writing and preparation was led by BHL in collaboration with MS. All authors were involved in reading, commenting and reviewing the text, and approving the final manuscript. Corresponding authorCorrespondence to Bente Hamre Larsen . Ethics declarationsEthics approval and consent to participate. This scoping review article does not contain any studies with human participants performed by any of the authors. Consent for publicationNot applicable. Conflict of interestNone declared. Competing interestsThe authors declare that they have no competing interests. Additional informationPublisher’s note. Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Electronic supplementary materialBelow is the link to the electronic supplementary material. Supplementary Material 1Supplementary material 2, supplementary material 3, rights and permissions. Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . Reprints and permissions About this articleCite this article. Larsen, B.H., Dyrstad, D.N., Falkenberg, H.K. et al. Training healthcare professionals in assessment of health needs in older adults living at home: a scoping review. BMC Med Educ 24 , 1019 (2024). https://doi.org/10.1186/s12909-024-06014-9 Download citation Received : 28 June 2024 Accepted : 11 September 2024 Published : 17 September 2024 DOI : https://doi.org/10.1186/s12909-024-06014-9 Share this articleAnyone you share the following link with will be able to read this content: Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative
BMC Medical EducationISSN: 1472-6920
Efficacy of hepatic arterial infusion chemotherapy in patients with primary liver cancer with portal vein tumor thrombosis: a comparative analysis of different perfusion chemotherapeutic regimens
European Journal of Medical Research volume 29 , Article number: 465 ( 2024 ) Cite this article Metrics details Portal vein tumor thrombosis (PVTT) commonly occurs in patients with primary liver cancer (PLC). Transarterial chemoembolization (TACE) is a treatment for patients with PLC and PVTT. Some studies have shown that combining TACE therapy with hepatic arterial infusion chemotherapy (HAIC) might improve the survival rate of PLC patients with PVTT. However, few studies have compared the different regimens of PLC with PVTT. We aimed to compare the differences between the oxaliplatin + raltetrexed regimen and FOLFOX regimen. We divided the 248 patients into two groups. There were 60 patients in the oxaliplatin + ratitetrexed group and 74 patients in the FOLFOX group. The primary endpoints were OS and PFS. The secondary endpoints were ORR and adverse events. We used SPSS software, the Kaplan–Meier method, the t test, and the rank sum test to compare the differences between the two groups. The median OS was 10.82 months in the oxaliplatin + raltitrexed group and 8.67 months in the FOLFOX group. The median PFS time was greater in the oxaliplatin + raltitrexed group (10.0 months) than that in the FOLFOX group (7.1 months). The ORR was greater in the oxaliplatin + raltitrexed group than that in the FOLFOX group (18.3% vs. 13.5%; P = 0.445). The DCR in the oxaliplatin + raltitrexed group was higher than that in the FOLFOX group (70.0% vs. 64.8%; P = 0.529). However, in the subgroup analysis, the difference between them was more significant in the type II PVTT subgroup. The OS was 12.08 months in the oxaliplatin + raltitrexed group and 7.26 months in the FOLFOX group ( P = 0.008). The PFS was 11.68 months in the oxaliplatin + raltitrexed group and 6.26 months in the FOLFOX group ( P = 0.014). In the right branch of type II PVTT, the OS was 13.54 months in the oxaliplatin + raltitrexed group and 6.89 months in the FOLFOX group ( P = 0.015), and the PFS was 13.35 months in the oxaliplatin + raltitrexed group and 6.27 months in the FOLFOX group ( P = 0.030). The incidence of adverse reactions was similar between the two groups. ConclusionsCompared with the FOLFOX regimen, the oxaliplatin + raltitrexed chemoembolization regimen had longer OS, PFS time and ORR and DCR and it was safe and tolerable. Primary liver cancer (PLC) is a common malignancy and the fourth leading cause of cancer-related death worldwide [ 1 ]. There are two types of hepatic vascular invasion: macroscopic and microscopic. Portal vein tumor thrombosis (PVTT) is the most common form of macrovascular invasion of the PLC [ 2 ]. Patients with PVTT usually lose the opportunity for surgery and have an aggressive disease course, decreased liver function reserve, limited treatment options, higher recurrence rates after treatment, and, therefore, worse overall survival [ 3 , 4 , 5 ]. Clinically, PVTT is related to tumor size, tumor number, tumor stage, Child–Pugh score, and serum alpha-fetoprotein (AFP) levels [ 6 ]. Some studies have shown that combining transarterial chemoembolization (TACE) therapy with hepatic arterial infusion chemotherapy (HAIC) might improve the survival rate of patients with PLC with PVTT [ 7 ]. TACE is a treatment in which embolic agents and chemotherapy drugs are mixed together and injected from the hepatic artery to the tumor site, serving to embolize the tumor-feeding arteries and induce ischemic necrosis in the tumor tissue and it is one of the most commonly recommended first-line treatments for PLC, especially combined with PVTT [ 8 , 9 , 10 ]. Many studies have shown that TACE combined with HAIC is superior to TACE alone in terms of overall survival (OS) and progression-free survival (PFS), and the treatment-associated toxicities are generally well tolerated [ 7 , 11 , 12 ]. Other studies have shown that in the unresectable and advanced PLC, compared with those in patients treated with two chemoembolization regimens [oxaliplatin + raltetrexed and oxaliplatin + fluorouracil + leucovorin calcium regimen (FOLFOX)], the disease control rates (DCRs) of patients treated with oxaliplatin and realtitrexed were greater than those in patients in the FOLFOX group, and the incidence of adverse reactions was similar [ 13 , 14 ]. However, the clinical data on the use of raltitrexed in TACE for treating PLC are compared with those on specific chemotherapeutic drug regimens and related effectiveness comparisons [ 15 ]. To date, there are still arguments about the effectiveness of different drug regimens for HAIC combined with TACE in patients with PLC with PVTT. Therefore, we designed this retrospective study to compare the effectiveness and safety of different drug regimens for patients with PLC with PVTT treated with HAIC combined with TACE. Section of patientsPatients were recruited from the Second Affiliated Hospital of Chongqing Medical University. The inclusion criteria were as follows: (1) patients aged > 18 years with PLC who were unsuitable for resection or percutaneous ablation, (2) the Barcelona Clinic Liver Cancer (BCLC) stage is the B–C, or Chinese liver cancer (CNLC) stage is Ib, IIa and llb, (3) Eastern Cooperative Oncology Group (ECOG) performance status is less than or equal to 2, (4) preserved liver function (Child–Pugh) class A or B, (5) a life expectancy greater 12 weeks, (6) a leukocyte count of > 3.0 × 10 9 /L, platelet count ≥ 80 × 10 9 /L, hemoglobin (Hb) ≥ 80 g/L; creatinine (Cr) ≤ 2.0 × UNL (upper normal limits), bilirubin (BIL) ≤ 2.0 × UNL, alanine transaminase (ALT) and aspartate transaminase (AST) ≤ 7.0 × UNL and (7) treatment with programmed cell death protein 1 (PD1) or programmed cell death-ligand 1 (PD-L1) before. All patients were excluded if they had any other primary tumors, severe liver dysfunction, Child–Pugh class C disease, including severe jaundice, hepatic encephalopathy, refractory intraperitoneal effusion, or hepatorenal syndrome. Patients were also excluded if they had coagulation dysfunction that could not be corrected, if the main portal vein was completely embolized by cancer thrombolysis, if the portal vein collateral compensation was insufficient, if the portal vein could not flow back through the portal vein, if it was combined with severe infection and could not be effectively controlled, or if other serious illnesses or medical conditions occurred. In addition to TACE and HAIC, patients receiving other invasive therapies [radiofrequency, liver resection, high-intensity focused ultrasound (HIFU), etc.] were also excluded. A total of 248 patients with PLC and PVTT were selected from the Department of Hepatobiliary Surgery, Gastroenterology and Hepatic Disease Center from January 2019 to October 2022. All patients underwent contrast-enhanced ultrasound (CEUS) imaging. It represents an important tool for the identification of PVTT, particularly for identifying differentiating neoplastic and nonneoplastic thrombosis through the analysis of the ultrasound enhancement characteristics of the thrombosis (malignant findings are characterized by intraluminal arterial hyperenhancement during the arterial phase and washout in the portal or late phase, while benign thrombosis lacks contrast enhancement in any phase) [ 16 ]. The 248 patients were divided into the oxaliplatin + raltitrexed group and FOLFOX groups. After excluding 26 patients with metastatic tumors from other sites and 88 patients who were lost to follow-up after one treatment session, there were 60 patients in the oxaliplatin + ratitetrexed regimen group and 74 patients in the FOLFOX regimen group were included (Fig. 1 ). The primary endpoints were OS and PFS. The secondary endpoints were ORR and adverse events.  Flow diagram showing patient selection. Abbreviations PLC, primary liver cancer; PVTT, portal vein tumor thrombosis; TACE, transarterial chemoembolization; HAIC, hepatic arterial infusion chemotherapy Treatment planUsing the Seldinger technique, we punctured the 5Fr micropuncture into the right femoral artery of patients and placed the 5F vascular sheath. The tumor nourishing arteries were hyperselectively intubated with a microcatheter and a superslip wire. Then, we injected chemicals (3 mg of realtitrexed, 50 mg of loplatin, 20 mg of pyrorubicin mixed with 5–20 ml of iodized oil or loplatin combined with pyrorubicin mixed with iodized oil) into the tumor nourishing arteries. The actual dose was determined based on the size and number of target tumors and the patients’ liver function. Polyvinyl alcohol (PVA) particles were used after embolization of the iodooil emulsions, and digital subtraction angiography (DSA) was performed 5 min after embolization to confirm stagnant blood flow in the feeding artery. We placed an arterial catheter after TACE and performed perfusion chemotherapy in the general ward. We intravenously administered dexamethasone (5 mg i. v) and micropumped oxaliplatin (85 mg/m 2 ) through the catheter sheath artery for 3 h and raltetrexed (3 mg/m 2 ) for 5 h in the oxaliplatin + raltitrexed group. We intravenously administered dexamethasone (5 mg i. v) and micropumped oxaliplatin (85 mg/m 2 ) through the catheter sheath artery for 3 h, calcium folinate (200 mg/m 2 ) for 2 h and fluorouracil (2500 mg/m 2 ) for 46 h in the FOLFOX group. All patients were followed up every 4–6 weeks after the last TACE and then every 1–3 months if there was no significant recurrence or metastasis. If new lesions or residual tumors were identified, TACE was repeated until untreatable progression occurred. Statement of ethicsThis retrospective study was conducted in accordance with the Declaration of Helsinki. This study was approved by the Chongqing Medical University, the Second Affiliated Hospital of Chongqing Medical University. All patients provided written informed consent form. The data were statistically analyzed using the SPSS 26.0 software. The measurement data were expressed as the mean ± standard deviation (x ± s), with groups compared utilizing the t test and χ 2 test for count data, OS and PFS were analyzed via Kaplan–Meier curves, with statistically significant indicated by P < 0.05. Study subjectBetween January 2019 and October 2022, 248 patients were received HAIC combined with TACE treatment. After excluding 26 patients with metastatic tumors from other sites and 88 patients who were lost to follow-up after one treatment session, there were 60 patients in the oxaliplatin + ratitetrexed regimen group and 74 patients in the FOLFOX regimen group (Fig. 1 ). The median tumor size was 9.4 cm (range 3.0–18.7 cm). The baseline characteristics of the two groups are summarized in Table 1 ; none of these characteristics differed significantly between the two groups. Most patients were diagnosed with hepatitis B virus (HBV) related PLC, and most of them were male (Table 1 ). Safety and toxicityToxic and adverse reactions were evaluated according to the standards for toxicity and side reactions of World Health Organization (WHO) anticancer drugs [ 17 ]. There were no cases of procedure-related mortality or 30-day mortality. The complications are listed in Table 2 . The most common complications were postembolization syndrome and liver dysfunction. Six of the 60 patients in the oxaliplatin + raltitrexed group and ten of the 74 patients in the FOLFOX group experienced grade 3–4 adverse events. Pain adverse effects occurred in 24 (40.0%) patients in the oxaliplatin + raltitrexed group and 42 (56.7%) patients in the FOLFOX group ( P = 0.034). The other adverse reactions were similar between the two groups (Table 2 ). Tumor responseWe evaluated the therapeutic efficacy of PLC according to the WHO modified Response Evaluation Criteria in Solid Tumors (mRECEIST) [ 18 ] divided into complete remission (CR) (no enhancement of the intratumoral artery), partial remission (PR) (the tumor was reduced by 30%), stable disease (SD), and progressive disease (PD) (tumor diameter increase of 20% or new tumors). CR + PR was the objective response rate (ORR) and CR + PR + SD was the disease control rate (DCR). Efficacy was evaluated by review after 2 cycles of chemotherapy. A physical examination was performed before the start of each cycle of chemotherapy and routine blood routine, liver and kidney function, AFP, electrocardiogram, computed tomography (CT) or magnetic resonance imaging (MRI), and color ultrasound examinations were performed. Follow-up visits were used to assessed the median survival time. Tumor response was assessed at 4–6 weeks. The results for the two groups are shown in Table 3 . The ORR and DCR were higher in the oxaliplatin + raltitrexed group than that in the FOLFOX group (ORR: 18.3% vs. 13.5%; P = 0.445; DCR: 70.0% vs. 64.8%; P = 0.529). Survival analysisAt the end of the study period, 12 (20.0%) patients in the oxaliplatin + raltitrexed group and 6 (8.1%) patients in the FOLFOX group were still alive. The median follow-up time was 6 months, and the total follow-up time was 20 months. The median OS was 10.82 months in the oxaliplatin + raltitrexed group [95% confidence interval (CI) 8.80, 12.85] and 8.67 months in the FOLFOX group (95% CI 7.11, 10.22; P = 0.066) (Fig. 2 a). The median PFS time was slightly longer in the oxaliplatin + raltitrexed group (10.02 months, 95% CI 7.69, 12.36) than in the FOLFOX group (7.07 months, 95% CI 5.28, 8.85; P = 0.102) (Fig. 2 b). The ORR was greater in the oxaliplatin + raltitrexed group than that in the FOLFOX group (18.3% vs. 13.5%; P = 0.445). The DCR of the oxaliplatin + raltitrexed group was also greater thanthat of the FOLFOX group (70.0% vs. 64.8%; P = 0.529).  Survival analysis function of the two groups. The median follow-up time was 6 months, and the total follow-up time was 20 months. A Kaplan–Meier curves of OS in patients with unresectable primary liver cancer who underwent TACE in the two groups. B Kaplan–Meier curves of PFS in patients with unresectable primary liver cancer who underwent TACE in the two groups Univariate and multivariate logistic regression analysesWe used univariate and multivariate logistic regression analyses to assess risk factors for each variable (Table 4 ). We found that age, the type of PVTT, tumor size and extrahepatic metastasis were independent risk factors affecting the prognosis of patients with PLC. Subgroup analysisSubgroup analysis by age. Previous studies have indicated a better protective effect of ralterexed on myocardial function [ 19 ], so our study divided patients into four subgroups by age (< 36 years, 36–50 years, 51–65 years and > 65 years). In the 1st subgroup, the OS was 4.00 months in the oxaliplatin + raltitrexed group (95% CI 2.04, 5.96) and 4.50 months in the FOLFOX group (95% CI 3.90, 5.10; P = 0.695); the PFS was 1.50 months in the oxaliplatin + raltitrexed group (95% CI 0.00, 4.44) and 3.75 months in the FOLFOX group (95% CI 1.78, 5.72; P = 0.107). In the 2nd subgroup, the OS was 13.80 months in the oxaliplatin + raltitrexed group (95% CI 10.01, 17.58) and 8.44 months in the FOLFOX group (95% CI 6.65, 10.43; P = 0.080); the PFS was 13.23 months in the oxaliplatin + raltitrexed group (95% CI 8.98, 17.48) and 6.47 months in the FOLFOX group (95% CI 4.52, 8.41; P = 0.072). In the 3rd subgroup, the OS was 12.95 months in the oxaliplatin + raltitrexed group (95% CI 10.06, 15.83) and 9.17 months in the FOLFOX group (95% CI 6.12, 12.21; P = 0.128); the PFS was 12.32 months in the oxaliplatin + raltitrexed group (95% CI 8.93, 15.72) and 7.71 months in the FOLFOX group (95% CI 4.35, 11.07; P = 0.095). In the 4th subgroup, the OS was 10.03 months in the oxaliplatin + raltitrexed group (95% CI 6.42, 13.64) and 8.27 months in the FOLFOX group (95% CI 5.36, 11.19; P = 0.951); the PFS was 9.68 months in the oxaliplatin + raltitrexed group (95% CI 5.66, 13.70) and 8.28 months in the FOLFOX group (95% CI 5.36, 11.19; P = 0.728) (Table 5 ). Overall, the OS and PFS of the oxaliplatin + raltitrexed group were longer than those of the FOLFOX group, but there were no significant differences between the two groups, and the examination indices of myocardial enzyme levels, cardiac color ultrasound results and other indicators did not appear significantly differ among the age groups. Therefore, the cardioprotective effect of raltetrexed needs to be further verified. Subgroup analysis by PVTT classificationThe more conventional and better-known classification of PVTT was proposed by the Liver Cancer Study Group of Japan (LCSGJ) [ 20 , 21 ]. Chen et al. proposed Cheng's classification type: Type I0: microscopic tumor thrombosis formation; Type I: tumor thrombosis involving secondary level and above portal vein branch (type Ia: tumor thrombosis involving portal vein grade i and j level and above branch; type Ib: tumor thrombosis involving portal vein secondary branch); Type II: tumor thrombosis involving primary portal branch [type IIa: primary portal branch (such as left or right portal stem); type IIb: secondary primary portal branch (involving left and right portal stem)]; Type III: tumor thrombolysis involving the main portal vein (type IIIa: tumor thrombolysis involving the main portal vein, portal vein trunk confluence below no more than 2 cm; type IIIb: tumor thrombolysis involving the main portal vein, portal vein trunk trunk confluence below more than 2 cm); Type IV: tumor thrombolysis involving superior mesenteric vein or inferior vena cava (type IVa: tumor thrombolysis involving superior mesenteric vein; type IVb: cancer thrombolysis involving inferior vena cava) [ 22 ]. We subjected all patients to PVTT subgroup analysis by Cheng's classification type. In the type II PVTT subgroup, the OS was 12.08 months in the oxaliplatin + raltitrexed group (95% CI 9.18, 14.98) and 7.26 months in the FOLFOX group (95% CI 5.79, 8.72; P = 0.008) (Fig. 3 a); the PFS was 11.68 months in the oxaliplatin + raltitrexed group (95% CI 8.46, 14.90) and 6.26 months in the FOLFOX group (95% CI 4.80, 7.73; P = 0.014) (Fig. 3 b). The ORR and DCR were greater in the oxaliplatin + raltitrexed group than in the FOLFOX group (ORR: 24.1% vs. 15.2%; P = 0.357; DCR: 75.8% vs. 60.9%; P = 0.221) (Table 6 ).  Survival analysis function of patients in the type II PVTT subgroup. A Kaplan–Meier curves of OS in patients with type II PVTT who underwent TACE in the two groups. B Kaplan–Meier curves of PFS in patients with type II PVTT who underwent TACE in the two groups Subgroup analysis by tumor numberIn the baseline comparison, there were significant differences between the number of tumors in the two groups, so we performed Cox multivariate regression analysis. All patients were divided into two subgroups: a single-tumor subgroup and a multiple-tumor subgroup. In the single-tumor subgroup, the OS was 11.25 months in the oxaliplatin + raltitrexed group (95% CI 8.58, 13.91) and 7.81 months in the FOLFOX group (95% CI 5.27, 10.35; P = 0.044) (Fig. 4 a); the PFS was 10.66 months in the oxaliplatin + raltitrexed group (95% CI 7.53, 13.80) and 5.95 months in the FOLFOX group (95% CI 3.34, 8.56; P = 0.041) (Fig. 4 b). In the multiple-tumor subgroup, the OS was 12.96 months in the oxaliplatin + raltitrexed group (95% CI 9.83, 16.08) and 9.10 months in the FOLFOX group (95% CI 7.10, 11.09; P = 0.046) (Fig. 4 c); the PFS was 12.54 months in the oxaliplatin + raltitrexed group (95% CI 9.10, 15.87) and 8.24 months in the FOLFOX group (95% CI 5.90, 10.57; P = 0.047) (Fig. 4 d) (Table 7 ).  Survival analysis function of subgroups by tumor numbers. A Kaplan–Meier curves of OS in patients with a single tumor who underwent TACE in the two groups. B Kaplan–Meier curves of PFS in patients with a single tumor who underwent TACE in the two groups. C Kaplan–Meier curves of OS in patients with a multiple tumor who underwent TACE in the two groups. D Kaplan–Meier curves of OS in patients with a multiple tumor who underwent TACE in the two groups Subgroup analysis by the position of type II PVTTIn the type II PVTT subgroup, the oxaliplatin + raltitrexed regimen showed better efficacy than FOLFOX, and we again divided all patients into left, right and bilateral type II PVTT groups according to the location of the PVTT.In the right group, the OS was 13.54 months in the oxaliplatin + raltitrexed group (95% CI 9.52, 17.56) and 6.89 months in the FOLFOX group (95% CI 5.17, 8.60; P = 0.015) (Fig. 5 a); the PFS was 13.35 months in the oxaliplatin + raltitrexed group (95% CI 9.08, 17.63) and 6.27 months in the FOLFOX group (95% CI 4.48, 8.07; P = 0.030) (Fig. 5 b). These two drug treatment modalities were significant different (Table 8 ).  Survival analysis of subgroups stratified by the location of type II PVTT. A Kaplan–Meier curves of OS in patients with type II PVTT in the right branch who underwent TACE in the two groups. B Kaplan–Meier curves of PFSS in patients with type II PVTT in the right branch who underwent TACE in the two groups In our study, after a 20-month follow-up time, the OS and PFS in the oxaliplatin + raltitrexed group were slightly longer than those in the FOLFOX group. However, neither of the two groups exhibited statistically significant differences. The ORR was 18.3% in the oxaliplatin + raltitrexed group and 13.5% in the FOLFOX group ( P = 0.445). The DCR was 70.0% in the oxaliplatin + raltitrexed group and 64.8% in the FOLFOX group ( P = 0.529). Pain adverse effects occurred in 24 (40.0%) patients in the oxaliplatin + raltitrexed group and 42 (56.7%) patients in the FOLFOX group ( P = 0.034). However, the other adverse reactions were almost the same between the two groups. The FOLFOX treatment modality was previously used to treat gastrointestinal tumors (including primary and metastatic liver cancer, biliary tract system tumors, pancreatic tumors, and colorectal tumors.) [ 23 , 24 ]. According to previous reports, FOLFOX-HAIC significantly improved OS compared with TACE in patients with unresectable large hepatocellular carcinoma [ 25 , 26 ]. However, fluorouracil should be administered intra-arterially for approximately 44 h, and a higher incidence of pain, catheter thrombosis and catheter-associated infection has been reported [ 27 ]. The oxaliplatin + raltitrexed regimen had been gradually used for HAIC treatment after TACE due to its advantages of less cardiotoxicity and shorter perfusion time in recent years [ 28 ]. The OS and PFS were longer than those of the FOLFOX group in previous studies not only for HCC but also for colorectal cancer (CRC) liver metastasis (CRCLM) [ 29 , 30 ]. There are few studies on perfusion chemotherapy for liver cancer combined with PVTT. Cui et al. proposed that the PFS of patients treated with raltitrexed was longer in unresectable hepatocellular carcinoma complicated with PVTT, but no significant statistical difference was observed between the two groups [ 13 ]. However, this finding did not further explain the reason for the longer PFS of the oxaliplatin + raltitrexed regimen. OS and PFS were also longer in the oxaliplatin + raltitrexed group than those in the FOLFOX group, but there was no significant difference between the two groups in our study. Unlike previous studies, our drug dose was calculated by body weight in order to obtain the best results for each patient and decrease toxic side effects. In addition, we also conducted subgroup analysis through age, type of PVTT, and the number of tumors and still concluded that oxaliplatin + raltitrexed was superior to FOLFOX, and there were significant differences in the subgroups of type II PVTT and the number of tumors. Moreover, the sample size was somewhat larger than that in previous studies. It can be seen that oxaliplatin + raltitrexed regimen has beneficial advantages and safety for PLC in combination with PVTT. According to our subgroup analysis by PVTT classification, oxaliplatin + raltitrexed showed better efficacy than FOLFOX in the type II PVTT subgroup. The OS was 12.08 months in the oxaliplatin + raltitrexed group (95% CI 9.18, 14.98) and 7.26 months in the FOLFOX group (95% CI 5.79, 8.72; P = 0.008); the PFS was 11.68 months in the oxaliplatin + raltitrexed group (95% CI 8.46, 14.90) and 6.26 months in the FOLFOX group (95% CI 4.80, 7.73; P = 0.014). Moreover, oxaliplatin + raltitrexed was more effective for type II PVTT located in the right branch in our study. Theoretically speaking, there may be two reasons for this. First, the efficacy of chemotherapy drugs may be related to the location of the PVTT. When the PVTT is located in the right branch of the portal vein and the tumor is located on the same side, the drug can be better transported to the target vessel through the right hepatic artery, while when the PVTT is located in the left or bilateral or even the main portal vein (MPV), the perfusion effect of the drug through the arteriae hepatica propria (AHP) may be slightly attenuated. On the other hand, this is due to the pharmacokinetic difference between ratitetrexed and fluorouracil. Raltitrexed can directly or specifically cause DNA chain breakage and apoptosis by inhibiting thymidylate synthase (TS), a key enzyme in the synthesis of deoxythymidine 5-triphosphate (TTP). However, fluorouracil was first converted to a 5-fluorine-deoxyuracil nucleotide at first in vivo after which TS was inhibited to inhibit DNA. Nevertheless, further prospective studies are needed to determine the possible advantages of the right-branch type II PVTT will in the oxaliplatin + raltitrexed group. Previous studies reported that fluorouracil has some cardiotoxic effects, such us fluoropyrimidine-induced cardiotoxicity (FIC), including coronary artery vasospasm, endothelial or cardiomyocyte damage, toxic metabolites, and dihydropyrimidine dehydrogenase deficiency and so on [ 31 ]. Compared with fluorouracil, raltitrexed is less cardiotoxic [ 32 ]. According to our subgroup analysis by age, the OS and PFS of the oxaliplatin + raltitrexed group were longer than those of the FOLFOX group in every subgroup, but neither the OS nor PFS of the two groups in the subgroups were significantly different. All patients in our study underwent accessory examinations including myocardial enzyme spectrum, type B natriuretic peptide precursor (BNP), cardiac color ultrasound and electrocardiogram before and after TACE, and none of the findings showed significant cardiac damage. Therefore, the cardioprotective effect of raltetrexed needs to be further verified. According to the subgroup analysis by tumor number, the OS and PFS in the oxaliplatin + raltitrexed group were grater than those in the FOLFOX group and there were significant differences regardless of the number of tumors. The study of Rong et al. noted that as the number of tumors increased, the OS decreased [ 33 ], while the OS of our study was slightly longer in multiple tumor groups than in a single tumor group. Therefore, further studies on the impact of tumor number on patient prognosis are needed, but these studies did not reveal an obvious prognostic benefit of raltitrexed. Our study also evaluated the safety and tolerability of these two treatments. We found that the incidence of major complications was not significantly different between the two groups. Only a greater proportion of pain response in the FOLFOX group may be associated with a longer drug perfusion time, but all complications were reversible and adequately controlled by medical treatment. These results indicate that the combination of raltitrexed and oxaliplatin in TACE in patients with unresectable PLC is safe and tolerable. Our study also had some limitations. First, because it was retrospective, some selection biases were unavoidable. Second, this study was conducted at a single center with a relatively small number of patients, a large number of whom carried hepatitis B (82.8%), and the proportion of males was high (89.5%). Third, the included subjects in this study had no type IV PVTT. Currently, the treatment of type IV PVTT for TACE + HAIC is still being explored currently, and further studies on this topic may be needed. Finally, the sample size of the oxaliplatin + raltitrexed group was small. If we increase the sample size, reduce the loss to follow-up and extend the follow-up time, we can obtain better results. Moreover, the number of TACE procedures differed among individuals, which may also have affected the results of our study. Larger prospective trials are needed to confirm this conclusion. Despite no significant difference between the oxaliplatin + raltitrexed group and the FOLFOX group, the oxaliplatin + raltitrexed chemoembolization regimen had a longer OS, PFS, ORR and DCR than the FOLFOX regimen. This regimen was safe and tolerable, especially for PLCs with type II PVTT. Our findings suggest that the combination therapy of TACE and HAIC bvia oxaliplatin plus raltitrexed regimen confers more benefits to patients with unresectable PLC than other regimens. Availability of data and materialsThe data supporting the findings of this study are available from the corresponding author upon reasonable request. AbbreviationsPortal vein tumor thrombosis
Overall survival Progression-free survival Oxaliplatin + fluorouracil + leucovorin calcium Objective remission rate Disease control rate Transarterial chemoembolization plus hepatic arterial infusion chemotherapy Confidence interval Alpha-fetoprotein Barcelona clinic liver cancer Eastern Cooperative Oncology Group Upper normal limits Aminotransferase Programmed cell death protein 1 Programmed cell death-ligand 1 High intensity focused ultrasound Polyvinyl alcohol particles Digital subtraction angiography Hepatitis B surface antigen Carbohydrate antigen 125 Carbohydrate antigen 199 Carbohydrate antigen 242 Carbohydrate antigen 50 Carbohydrate antigen 724 International normalized ratio White blood cell Alkaline phosphatase γ-Glutamyl transferase World Health Organization Modified response evaluation criteria in solid tumors Complete remission Partial remission Stable disease Progressive disease Objective response rate Computed tomography Magnetic resonance imaging Liver Cancer Study Group of Japan Colorectal cancer Colorectal cancer liver metastasis Main portal vein Arteriae Hepatica Propria Thymidylate synthase Deoxythymidine 5-triphosphate Fluoropyrimidine-induced cardiotoxicity B naturetic peptide precursor Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. https://doi.org/10.3322/caac.21492 . Article PubMed Google Scholar Mähringer-Kunz A, Meyer FI, Hahn F, et al. Hepatic vein tumor thrombosis in patients with hepatocellular carcinoma: prevalence and clinical significance. United Eur Gastroenterol J. 2021;9(5):590–7. https://doi.org/10.1002/ueg2.12098 . Article CAS Google Scholar Zhang XF, Lai L, Zhou H, et al. Stereotactic body radiotherapy plus transcatheter arterial chemoembolization for inoperable hepatocellular carcinoma patients with portal vein tumour thrombus: a meta-analysis. PLoS ONE. 2022;17(5):e0268779. https://doi.org/10.1371/journal.pone.0268779 . Article CAS PubMed PubMed Central Google Scholar Liu PH, Huo TI, Miksad RA. Hepatocellular carcinoma with portal vein tumor involvement: best management strategies. Semin Liver Dis. 2018;38(3):242–51. https://doi.org/10.1055/s-0038-1666805 . Article CAS PubMed Google Scholar Kokudo T, Hasegawa K, Matsuyama Y, et al. Liver resection for hepatocellular carcinoma associated with hepatic vein invasion: a Japanese nationwide survey. Hepatology. 2017;66(2):510–7. https://doi.org/10.1002/hep.29225 . Khan AR, Wei X, Xu X. Portal vein tumor thrombosis and hepatocellular carcinoma—the changing tides. Hepatocell Carcinoma. 2021;8:1089–115. https://doi.org/10.2147/jhc.S318070 . Article Google Scholar Liu BJ, Gao S, Zhu X, et al. Combination therapy of chemoembolization and hepatic arterial infusion chemotherapy in hepatocellular carcinoma with portal vein tumor thrombosis compared with chemoembolization alone: a propensity score-matched analysis. Biomed Res Int. 2021;2021:6670367. https://doi.org/10.1155/2021/6670367 . Chen R, Li Y, Song K, et al. Efficacy and safety of transarterial chemoembolization-lenvatinib sequential therapy for the treatment of hepatocellular carcinoma with portal vein tumor thrombus: a retrospective study. Gastrointest Oncol. 2022;13(2):780–6. https://doi.org/10.21037/jgo-22-239 . Lu J, Zhang XP, Zhong BY, et al. Management of patients with hepatocellular carcinoma and portal vein tumour thrombosis: comparing east and west. Lancet Gastroenterol Hepatol. 2019;4(9):721–30. https://doi.org/10.1016/s2468-1253(19)30178-5 . Zhang X, Wang K, Wang M, et al. Transarterial chemoembolization (TACE) combined with sorafenib versus TACE for hepatocellular carcinoma with portal vein tumor thrombus: a systematic review and meta-analysis. Oncotarget. 2017;8(17):29416–27. https://doi.org/10.18632/oncotarget.15075 . Article PubMed PubMed Central Google Scholar Cai YS, Wu H. Is FOLFOX-HAIC superior to transarterial chemoembolization in treating large hepatocellular carcinoma? Hepatobil Surg Nutr. 2022;11(1):164–5. https://doi.org/10.21037/hbsn-21-503 . Si T, Huang Z, Khorsandi SE, et al. Hepatic arterial infusion chemotherapy versus transarterial chemoembolization for unresectable hepatocellular carcinoma: a systematic review with meta-analysis. Front Bioeng Biotechnol. 2022;10:1010824. https://doi.org/10.3389/fbioe.2022.1010824 . Cui W, Fan W, Zhang Q, et al. Comparison of two transarterial chemoembolization regimens in patients with unresectable hepatocellular carcinoma: raltitrexed plus oxaliplatin versus 5-fluorouracil plus oxaliplatin. Oncotarget. 2017;8(45):79165–74. https://doi.org/10.18632/oncotarget.16298 . Gravalos C, Salut A, García-Girón C, et al. A randomized phase II study to compare oxaliplatin plus 5-fluorouracil and leucovorin (FOLFOX4) versus oxaliplatin plus raltitrexed (TOMOX) as first-line chemotherapy for advanced colorectal cancer. Clin Transl Oncol. 2012;14(8):606–12. https://doi.org/10.1007/s12094-012-0843-x . Omata M, Cheng AL, Kokudo N, et al. Asia-Pacific clinical practice guidelines on the management of hepatocellular carcinoma: a 2017 update. Hepatol Int. 2017;11(4):317–70. https://doi.org/10.1007/s12072-017-9799-9 . Cerrito L, Ainora ME, Di Francesco S, et al. The role of contrast-enhanced ultrasound (CEUS) in the detection of neoplastic portal vein thrombosis in patients with hepatocellular carcinoma. Tomography. 2023;9(5):1976–86. https://doi.org/10.3390/tomography9050154 . Morey J, Llinás P, Bueno-Costa A, et al. Raltitrexed-modified gold and silver nanoparticles for targeted cancer therapy: cytotoxicity behavior in vitro on A549 and HCT-116 human cancer cells. Materials (Basel). 2021. https://doi.org/10.3390/ma14030534 . Aras M, Erdil TY, Dane F, et al. Comparison of WHO, RECIST 1.1, EORTC, and PERCIST criteria in the evaluation of treatment response in malignant solid tumors. Nucl Med Commun. 2016;37(1):9–15. https://doi.org/10.1097/mnm.0000000000000401 . Zhao C, Fan L, Qi F, et al. Raltitrexed plus oxaliplatin-based transarterial chemoembolization in patients with unresectable hepatocellular carcinoma. Anticancer Drugs. 2016;27(7):689–94. https://doi.org/10.1097/cad.0000000000000371 . Kudo M, Kitano M, Sakurai T, et al. General rules for the clinical and pathological study of primary liver cancer, nationwide follow-up survey and clinical practice guidelines: the outstanding achievements of the liver cancer study group of Japan. Digestive Dis. 2015;33(6):765–70. https://doi.org/10.1159/000439101 . Kokudo N, Hasegawa K, Akahane M, et al. Evidence-based clinical practice guidelines for hepatocellular carcinoma: the Japan society of hepatology 2013 update (3rd JSH-HCC guidelines). Hepatol Res. 2015. https://doi.org/10.1111/hepr.12464 . Shuqun C, Mengchao W, Han C, et al. Tumor thrombus types influence the prognosis of hepatocellular carcinoma with the tumor thrombi in the portal vein. Hepatogastroenterology. 2007;54(74):499–502. PubMed Google Scholar Hebbar M, Chibaudel B, André T, et al. FOLFOX4 versus sequential dose-dense FOLFOX7 followed by FOLFIRI in patients with resectable metastatic colorectal cancer (MIROX): a pragmatic approach to chemotherapy timing with perioperative or postoperative chemotherapy from an open-label, randomized phase III trial. Ann Oncol. 2015;26(2):340–7. https://doi.org/10.1093/annonc/mdu539 . Chi Y, Yang J, Yang S, et al. Phase I dose-finding study of sorafenib with FOLFOX4 as first-line treatment in patients with unresectable locally advanced or metastatic gastric cancer. Chin J Cancer Res. 2015;27(3):239–46. https://doi.org/10.3978/j.issn.1000-9604.2015.06.08 . Li QJ, He MK, Chen HW, et al. Hepatic arterial infusion of oxaliplatin, fluorouracil, and leucovorin versus transarterial chemoembolization for large hepatocellular carcinoma: a randomized phase III trial. J Clin Oncol. 2022;40(2):150–60. https://doi.org/10.1200/jco.21.00608 . Zhang P, Wen F, Li Q. FOLFOX4 or sorafenib as the first-line treatments for advanced hepatocellular carcinoma: a cost-effectiveness analysis. Digest Liv Dis. 2016;48(12):1492–7. https://doi.org/10.1016/j.dld.2016.07.007 . Kemeny NE, Niedzwiecki D, Hollis DR, et al. Hepatic arterial infusion versus systemic therapy for hepatic metastases from colorectal cancer: a randomized trial of efficacy, quality of life, and molecular markers (CALGB 9481). Clin Oncol. 2006;24(9):1395–403. https://doi.org/10.1200/jco.2005.03.8166 . Ransom D, Wilson K, Fournier M, et al. Final results of Australasian Gastrointestinal Trials Group ARCTIC study: an audit of raltitrexed for patients with cardiac toxicity induced by fluoropyrimidines. Ann Oncol. 2014;25(1):117–21. https://doi.org/10.1093/annonc/mdt479 . Guo JH, Zhang HY, Gao S, et al. Hepatic artery infusion with raltitrexed or 5-fluorouracil for colorectal cancer liver metastasis. World J Gastroenterol. 2017;23(8):1406–11. https://doi.org/10.3748/wjg.v23.i8.1406 . Liu B, Zhu X, Gao S, et al. Safety and efficacy of hepatic arterial infusion chemotherapy with raltitrexed and oxaliplatin post-transarterial chemoembolization for unresectable hepatocellular carcinoma. J Interv Med. 2019;2(2):91–6. https://doi.org/10.1016/j.jimed.2019.07.006 . Khan K, Rane JK, Cunningham D, et al. Efficacy and cardiotoxic safety profile of raltitrexed in fluoropyrimidines-pretreated or high-risk cardiac patients with GI malignancies: large single-center experience. Clin Colorectal Cancer. 2019;18(1):64–7161. https://doi.org/10.1016/j.clcc.2018.09.010 . Depetris I, Marino D, Bonzano A, et al. Fluoropyrimidine-induced cardiotoxicity. Crit Rev Oncol Hematol. 2018;124:1–10. https://doi.org/10.1016/j.critrevonc.2018.02.002 . Rong W, Yu W, Wu F, et al. Effect of resection margin and tumor number on survival of patients with small liver cancer. Zhonghua Zhong Liu Za Zhi. 2015;37(12):928–31. Download references AcknowledgementsWe are grateful to the Department of Hepatobiliary Surgery at the Second Affiliated Hospital of Chongqing Medical University. This study was supported by the National Natural Science Foundation of China (No. 82173117), Natural Science Foundation of Chongqing (No. CSTB2023NSCQ-MSX0214) and Kuanren Talents Program of the Second Affiliated Hospital of Chongqing Medical University (NO. kryc-yq-2209). This study was supported by the National Natural Science Foundation of China (No. 82173117), Natural Science Foundation of Chongqing (No. CSTB2023NSCQ-MSX0214) and Kuanren Talents Program of the Second Affiliated Hospital of Chongqing Medical University (NO. kryc-yq-2209). Author informationXinxin Tu and Wenfeng Zhang have contributed equally to this work. Authors and AffiliationsDepartment of Hepatobiliary Surgery, the Second Affiliated Hospital of Chongqing Medical University, Chongqing, No. 74, Linjiang Road, Yuzhong District, Chongqing Municipality, 400010, People’s Republic of China Xinxin Tu, Wenfeng Zhang, Qi He & Yue Li Department of Hepatobiliary Pancreatic Tumor Center, Chongqing University Cancer Hospital, Chongqing, No. 181, Hanyu Road, Shapingba District, Chongqing Municipality, 400010, People’s Republic of China You can also search for this author in PubMed Google Scholar ContributionsStudy conception and experimental design, collection and analysis of data, and manuscript writing, Xinxin Tu; collection and analysis of data, Xinxin Tu, Wenfeng Zhang, Sipeng Li, Qi He; study conception, design, and supervision, Wenfeng Zhang, Yue Li; supervision, manuscript writing, and final approval of the manuscript; Yue Li. All authors read and approved the final manuscript. Corresponding authorCorrespondence to Yue Li . Ethics declarationsEthics approval and consent to participate. This retrospective study was conducted in accordance with the Declaration of Helsinki. This study was approved by Chongqing Medical University, the Second Affiliated Hospital of Chongqing Medical University. All patients provided written informed consent. Consent for publicationNot applicable. Competing interestsThe authors declare no competing interests. Additional informationPublisher's note. Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Rights and permissionsOpen Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ . Reprints and permissions About this articleCite this article. Tu, X., Zhang, W., Li, S. et al. Efficacy of hepatic arterial infusion chemotherapy in patients with primary liver cancer with portal vein tumor thrombosis: a comparative analysis of different perfusion chemotherapeutic regimens. Eur J Med Res 29 , 465 (2024). https://doi.org/10.1186/s40001-024-02053-6 Download citation Received : 08 February 2023 Accepted : 08 September 2024 Published : 19 September 2024 DOI : https://doi.org/10.1186/s40001-024-02053-6 Share this articleAnyone you share the following link with will be able to read this content: Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative
European Journal of Medical ResearchISSN: 2047-783X
Investigating academic dishonesty and its relationship with moral competence and professional identity of nursing students: a cross-sectional study
BMC Nursing volume 23 , Article number: 662 ( 2024 ) Cite this article Metrics details Academic dishonesty as a fundamental challenge in adherence of ethical principles in providing care to patients has caused concern to the scientific community of nurses. In addition, positive professional identity and high moral competence are important for nurses to perform multiple care roles in high quality care of patients. The purpose of the present study is of investigating academic dishonesty and its relationship with moral competence and professional identity of master’s and PhD nursing students. This descriptive-analytical study was conducted by census method on 65 master’s and PhD nursing students in Shiraz University of Medical Sciences, Iran in 2023. Data collection tools included 4 questionnaires (Demographic information, Academic Dishonesty Scale (DAS), Nurses’ moral competence and Professional Identity Scale for Nursing Students (PISNS)). Data collection was done within 2 months. Descriptive and inferential analyzes including independent t-test, Pearson correlation coefficient and linear regression were used to analyze the data. The collected data were analyzed by SPSS.V.22 software. P -value less than 0.05 was considered significant. The average age of 65 participants was 31.5 ± 5.61 years. The majority of the participants in this study were women 48 (73.8%). There is a significant and negative correlation between academic dishonesty and moral competence ( r =-0.260, P -value = 0.036). There is no significant correlation between academic dishonesty and professional identity ( r = 0.154, P -value = 0.22). Also, a significant positive correlation was found between moral competence and professional identity ( r = 0.294, P -value = 0.018). Therefore, considering that the fact that students have a great impact on patient care, Researchers suggest that educational institutions should prevent the increase of academic dishonesty among students by establishing new rules and regulations. Peer Review reports One of the important issues in the health system is providing ethical care. Ethical care is an essential part of the nursing profession The actual academic dishonesty is a fundamental challenge in adherence to ethical principles in providing care to the patient [ 1 ]. Honesty is considered a fundamental moral value in all educational environments, and academic honesty is of unquestionable importance in educational environments, academic dishonesty and theft have been one of the most challenging and controversial ethical issues in academic debates for years [ 2 , 3 ]. Academic dishonesty is defined as the use of illegal aid to deceive an instructor or professor, a deliberate attempt by a student to falsify data, or any other fraud on campus. Globally, more than 80% of students agree that cheating is necessary to progress at higher levels [ 4 ] And more than 70% of students admit that they have been involved in various forms of academic dishonesty [ 2 ]. The study of Alotaibi and et al., (2024) showed that the prevalence of dishonesty among nursing students is at a high level [ 5 ] This is a concern for the scientific community of nurses, because there is a positive correlation between academic dishonesty and ethical behavior in the future [ 6 , 7 ]. Students who engage in academic immorality will have difficulty in acquiring the necessary skills for their future jobs [ 8 ] and these inefficient and unskilled people will cause irreparable problems in the clinical environment. In addition, paying attention to ethical competence in the nursing profession is essential, because the quality of patient care depends on the ethics of nurses [ 9 ]. Ethical competence is an ethical imperative that health care professionals must embody in their day-to-day functioning in order to identify ethical dimensions in their decisions. Ethical competence helps healthcare professionals find the best solution for their patients. Therefore, it is an essential component for providing high-quality care [ 10 , 11 ]. Moral competence is an abstract concept that consists of cognitive, emotional and behavioral components [ 12 ]. The results of a qualitative study in Iran showed that the ethical competence of nursing includes wide dimensions such as moral character, moral decision-making and moral care [ 9 ]. Since most of the decisions and procedures that are made in the nursing profession have an ethical dimension [ 13 ], developing students’ ethical competence is of great importance. Today’s students are future nurses who will make decisions about human health and life. Therefore, these students should attain an appropriate level of moral competence during their studies, which is a good opportunity for learning and both ethical and professional development [ 14 ] In this regard, the study of Haghighat, et al. stated there is a significant relationship between the formation of professional identity and the development of ethics in nursing students, so that by strengthening the professional values of students, their moral competences grow [ 12 ]. In addition to individual effects, unethical acts can have a negative impact on both the patient and the profession. Therefore, investing in nursing students’ moral competency improves professional identity and quality of nursing services [ 15 ]. Another factor that has a significant impact on the quality of patient care is professional identity. In fact, professional identity is a fundamental element in nursing [ 16 ]. The professional identity of “perception of the professional self” is based on attitudes, beliefs, feelings, values, motivations and experiences related to a particular profession [ 16 , 17 , 18 ]. Professional identity is a part of the care structure and is the main consequence of the education and socialization of nurses [ 19 , 20 ]. Positive and flexible professional identity is important for performing multiple roles of nurses in quality care of patients and reducing workplace stress [ 19 , 20 ]. It is also one of the most important factors affecting employees’ commitment to their profession [ 16 ]. The formation of professional identity is a dynamic process that starts from the time of training students for a future job and continues throughout one’s professional life [ 21 , 22 , 23 ]. Positive professional identity will ultimately increase the quality of care and negative professional identity and decrease the quality of care and motivation for professional learning of nursing students [ 20 ]. The results of a systematic review study showed that the most important factors related to the formation of nursing professional identity include poor team and communication activities, role of clinical instructors, educational methods, individual characteristics (age, sex, self-confidence, job satisfaction, etc.) and the role of culture and media [ 24 ]. In another study, the gap and lack of coordination between theoretical and clinical education, the amount of support that students receive from the educational system and lack of a clear and acceptable picture of nursing profession in the community are the factors affecting the development of professional identity [ 25 ]. On the other hand, academic dishonesty affects the formation of professional identity in nursing students, so the results of the study of the Krueger(2014) study reported that more than half of the nursing students reported academic dishonesty in the classroom and almost the same number of cheating in the clinical environment, which reflects the unprofessional behavior of the students in the clinical environment [ 26 ]. Also, in Bloomfield et al.(2021)’s study, the participants stated that academic dishonesty is a violation of the code of conduct, and a high percentage of them stated that academic dishonesty should be considered as a professional offense [ 27 ]. Considering the importance of academic honesty and the negative consequences of engaging in academic dishonesty, as well as the importance of moral competence and professional identity in nursing students, so far no study has investigated the relationship between academic dishonesty and the moral competence and professional identity of nursing students. Most of the studies conducted in the field of academic dishonesty have investigated its situation and methods [ 6 , 28 , 29 ] and the effective factors in creating academic dishonesty and cheating [ 2 , 29 ]. Therefore, this study aimed to determining the relationship between academic dishonesty with moral competence and professional identity of nursing students was accomplished. Study design and subjectsIn The present study 70 students (Master and PhD) participated in the study. Five students were excluded from the study due to the failure to complete the questionnaire and the analysis was done on the data of 65 students of Shiraz School of Nursing and Midwifery, Iran from June to November 2023. The Sampling method used in this study was census and all nursing students in master and PhD nursing students with inclusion and exclusion criteria were enrolled. Inclusion criteria included at least one semester of study. Exclusion criteria were deficiency in filling out the questionnaire, unwillingness to participate in the study and presence of self-reported mental illness. The current study was designed based on the STROBE guidelines for observational studies. The present study has been approved by the ethics committee of Shiraz University of Medical Sciences with the Code of Ethics (IR). SUMS. NUMIMG. REC.1401.054 and access link (B2n.ir/z74571). After receiving the code of ethics, the researcher received a list of names along with the contact numbers of MS and PhD nursing students who met the inclusion and exclusion criteria. In the next step, the link of online questionnaires (all questionnaires were designed in one link) was sent to the target group via short message service (a system used for sending text messages to and from mobile phones). The online questionnaire link was sent up to 3 times. In the design of the online questionnaire, IP filtering was used to prevent repeated responses, and the participants could refuse to complete the questionnaire at any time. Before completing the questionnaire, participants were informed of the objectives of the study and informed written consent was obtained from each participant electronically before completing the questionnaire. There are 80 students nursing (master’s and PhD degree) in college. Finally, 70 of 80 nursing students participated in the study and after collecting questionnaires, 5 questionnaires were excluded due to failed to completion. Finally, data from 65 participants were analyzed. Data collection toolsIn this study, 4 questionnaires were used, including: Demographic information questionnaire (age, gender, grade point average), Academic Dishonesty Scale (DAS) [ 30 ], Nurses’ moral competence [ 9 ]and Professional Identity Scale for Nursing Students (PISNS) [ 16 ]. Academic dishonesty scaleThe scale was designed by Bashir & Bala in 2018 in 23 items and 6 dimensions. Dimensions of the scale include Cheating in examination (items 1 to 5), Plagiarism (items 6 to 9), Outside help (items 10 to 13), Prior cheating (14 to 16), Falsification (items 17 to 19), and lying about academic assignments (items 20 to 23). The items of this scale are scored on a 5-degree Likert range from never (score 0) to always (score 4) [ 31 ]. The upper limit of the score in this questionnaire is 92 and the lower limit is 0. (Low range: 0–30, Intermediate range: 31–60, High range: 61–90) This scale has been Translation and validated in Iran. Validity and reliability of the questionnaire were confirmed by face, content and construct validity (confirmatory factor analysis and internal consistency) and Cronbach’s alpha. Confirmatory factor analysis with fitting indices (2X = 317, 1.63 × 2/df, 0.81 NFI, 0.93 TLI:, 0.89 GFI:, 0.95 CFI:, 0.05 RMR:, 0.68 PNFI:, 0.73 PCFI:, 0.63 PGFI:, 0.86 AGFI:, 0.95 IFI:, 0.06 RMSEA:, 0.19 PCLOSE: ) showed the fit of academic dishonesty scale with the data. In order to investigate the internal consistency of academic dishonesty scale, correlation between the scores of academic dishonesty dimensions with each other and with the total score of the scale was used [ 30 ]. Cronbach’s alpha was 0.93 in the version Translation and validated in Iran. Nurses’ moral competenceThis questionnaire was designed in 2017 by Zafarnia et al. in Iran. The questionnaire consists of 46 items, including 6 domains including Responsible Behavior (item 1 to 15), Reliability (16 to 23), Service Enthusiasm (24 to 28), Utility (29 to 33), Client-centered (4 to 42) and Ethical Knowledge (43 to 46). The questionnaire is based on a 4-point Likert scale with always (score 4), often (score 3), sometimes (score 2) and never [ 1 ]. Therefore, the minimum score on this scale is 46 and its maximum is 184 (Low range: 46–92, Intermediate range: 93–138, High range: 139–184). A higher score indicates greater moral competence. The content validity of this questionnaire was 92% by researchers [ 9 ]. Internal consistency was used to determine the reliability and Cronbach’s alpha was 0.93. To determine the reliability of the test-retest with a two-week interval, the nurses’ moral competency scale was administered again. Test-retest reliability was found to be 0.84 with CI 0.71–0.92 [ 9 ].  Professional identity scale for nursing studentsThe scale was created by Hufang Hao in 2011 and consists of 17 questions and 5 dimensions. Professional self-image, benefit of retention and risk of turnover, social comparison and self-reflection, independence of career choice, and social modeling. Items were graded from 1 (completely disagree) to 5 (completely agree), with scores ranging from 17 to 85. (Low range:17–39, Intermediate range: 40–62, High range:63–85) A high score denoted a high professional identity. In his study, the reliability coefficient of the total scale was 0.926 and the reliability coefficients of all subscales were more than 0.7 [ 32 , 33 ]. Translation and validated of tools in Iran has been confirmed by Haghighat et al. in 2017 with Cronbach’s alpha (α: 0.787) [ 16 ]. Statistical analysisData were analyzed using descriptive analysis including frequency, percentage, mean and standard deviation. Pearson correlation coefficient was used to determine the relationship between academic dishonesty and professional competence and academic dishonesty with students’ professional identity. Independent t-test was used to determine the relationship between demographic variables and academic dishonesty. Linear regression model was used for modeling. In this model, the dependent variable was professional competency and predictor variable were academic dishonesty, gender, grade, and grade point average. The collected data were analyzed using SPSS software version 22. P -value less than 0.05 was considered statistically significant. The average age of 65 participants was 31.5 ± 5.61 years. The majority of the participants in this study were women (48, 73.8%). The mean GPA for nursing PhD students was18.09 ± 0.63 and 17.09 ± 1.15 in MS students. The details of frequency, percentage, mean and standard deviation of variables based on demographic information are reported in Table 1 . According to the findings of this study, the mean and standard deviation for academic dishonesty was 7.82 ± 8.84, which is lower than average. Also, the mean and standard deviation for total moral competency was 158 ± 19.1 (High average) and total professional identity was 58 ± 11.5 (Intermediate average). The mean and standard deviation of the dimensions of all three variables are given in Table 2 . The results of data analysis showed that there was a significant and negative correlation between academic dishonesty and moral competence ( r =-0.260, P -value = 0.036, df = 63). On the other hand, there was no significant correlation between academic dishonesty and professional identity ( r = 0.154, P -value = 0.22). Also, there was a significant positive correlation between moral competence and professional identity ( r = 0.294, P -value = 0.018). The analytical results of the relationship between academic dishonesty, moral competence and professional identity are shown in Table 3 . In the linear regression model, first, the relationship between each independent variable (academic dishonesty, gender, grade, average) with the dependent variable (moral competence) was measured by simple linear regression. If the p -value was below 0.2, the variable was included in the multiple model. In this model, a significant relationship was found between moral competence and academic dishonesty ( P -value = 0.002). The model shows that for every increase in academic dishonesty, moral competence decreases by an average of 0.829 points. Details are shown in Table 4 . The aim of this study was to investigate academic dishonesty and its relationship between moral competence and professional identity of nursing students. In this study, less than half of these nursing students reported academic dishonesty. By comparison, the results of the Amutairi et al.study also -found that more than half of nursing students had academic integrity and a smaller percentage of them reported academic dishonesty with half of them saying that they participated in more than two cases of academic dishonesty during their education [ 34 ]. Maracle et al.‘s study stated that nursing students got used to doing dishonest behaviors and they think those behaviors are acceptable and normal, and this has caused an increase in dishonest behaviors among them [ 6 ]. Conversely, the results of the Alotaibi et al. study, contradicted the results of the current study, They found that a high percentage of students cheated on exams and assignments, and reported that more than three-quarters of students cheated before and during exams [ 5 ]. A study conducted in Saudi Arabia by Alnjjar et al. also found that a high percentage of nursing students reported at least one case of academic dishonesty in exams and homework [ 35 ]. In the other part of the study, the results showed that the moral competency of nursing students was moderate to high. In this regard, in the study of Alnajjar et al., it also indicated that nursing students had a moderate level of academic moral awareness and moral sensitivity [ 35 ]. On the other hand, Choi’s study emphasized that it is necessary for students to be given reasonable explanations about academic ethical standards at the same time as the beginning of academic enrollment to ensure that they are aware of their responsibilities and adherence these principles during their studies [ 36 ]. Therefore, ethical principles should be institutionalized during nursing students’ education in order to ensure safe and optimal care for patients in the future. The results of another study indicate that professional identity of nursing students is higher than average. In this regard, the Amutairi study was similar to the results of the current study, with more than half of the students having a high professional understanding [ 34 ]. The Gilvari study showed that students had a high professional identity [ 37 ]. The study in Iran also showed the professional identity score of nursing students was higher than half of the expected score [ 16 ]. The correlation between variables showed that there is a significant and negative relationship between academic dishonesty and moral competence of nursing students. That is, the less academic honesty students had, the less moral competency they showed. In this regard, Chang’s study is in line with the results of this study. This study showed that students with high ethical attitude were less involved in academic dishonesty, In this study the ethical behavior of participants showed a significant relationship with academic dishonesty [ 38 ]. Therefore, doing unethical activities may lead to normalization of this behavior and nursing students’ interest in ethical behaviors after graduation decreases. Academic honesty is usually an issue earlier in life than being specifically taught about ethical behavior. In the course of their training and clinical practice , nursing students like other professionals will encounter ethical dilemmas in professional life. Therefore, universities should plan to promote students’ culture of academic honesty in order to prevent unethical activities, and take necessary measures and inform students of existing policies. In another part of the study, no significant relationship was found between academic dishonesty and professional identity. Bloomfield et al.‘s study stated that high percentage of participants stated that academic dishonesty should be attended as a Professional misconduct [ 27 ]. Also, a study showed that there is a positive relationship between academic dishonesty and professional dishonesty [ 39 ]. On the other hand, most of the available studies are in the field of professional identity formation and ethical growth [ 40 , 41 ], which considering that academic dishonesty can have adverse effects on ethical and professional behaviors, therefore, with the help of professional identity formation, it can be expected that ethical competencies can be developed in students. In this regard, nursing education has an important impact on the development of nursing students’ professional identity and values [ 12 ]. Professional values are one of the important parts of professional identity. In the process of forming professional identity, a system of norms and values is formed in students and nurses. Nursing students learn these values from educators and other nurses as well as from other students. Their experiences of faculty and hospitals also play an important role in the development of professional values [ 42 ]. Therefore, it seems that by forming professional identity, indirectly the desire for students’ moral performance will be formed, and ultimately students will not go to unethical acts such as academic dishonesty. Ethical values in nursing students are affected by different factors in a process [ 40 ]. Perhaps this is because in this study no significant relationship was found between academic dishonesty and professional identity and on the other hand, nursing schools and educational system have an important role in the formation of professional identity if educational centers focus solely on increasing knowledge and skills, graduate nurses may be able to Do not have appropriate internalized professional values, which include moral and ethical values. The emphasis on professional values from the beginning of the study helps students develop the competencies they need to work in accordance with ethical and professional values. The study by Alnajjar et al. showed that academic dishonesty has adverse effects on workplace honesty and health care system quality [ 35 ] Therefore, given that academic honesty is a serious issue in nursing and nursing students who are involved in academic dishonesty have the potential to conduct deceptive and unethical behaviors in clinical settings [ 43 ]. Nursing requires high professional and ethical standards for protecting people’s lives and a reliable profession is known, so lack of academic honesty such as cheating in exams in nursing students can have inappropriate consequences in developing unethical behaviors and have adverse effects on the future of the profession [ 27 ]. Therefore, the academic honesty of students should be examined from different dimensions, and nursing teachers will be effective in reducing academic dishonesty by implementing specific educational programs in this field, therefore they will provide a basis for patient safety and will prevent dishonest behaviors in the professional future of students. This study has limitations. One of the limitations of the study is that due to the fact that the sampling was done from a nursing school, the number of samples is small, so the generalizability of the data should be taken into account. Therefore, it is suggested that future studies be conducted with a higher sample size and sampling from several nursing schools. It is also suggested to conduct studies considering the variables of the current research in undergraduate nursing and various levels of other medical fields. It is also recommended to conduct qualitative studies in this field. In the present study, there is a significant relationship between academic dishonesty and moral competencies, but there is no relationship between academic dishonesty and professional identity. Therefore, considering that students will work as nurses and nursing instructors in the future, if it becomes a habit for students to do dishonest things during their studies, it can cause harm to the patient and reduce the quality of nursing care. Researchers suggest that educational institutions should prevent the increase of academic dishonesty among students by establishing new rules and regulations, and professors should try to focus more on moral issues and honest academic activities in addition to increasing the level of knowledge and skills of students. Data availabilityThe datasets generated and/or analyzed during the current study are not publicly available but are available from the corresponding author on reasonable request. AbbreviationsAcademic Dishonesty Scale Nurses’ moral competence and Professional Identity Scale for Nursing Students Doctor of Philosophy Mokhtari Lakeh N, Nafar M, Ghanbari Khanghah A, Kazemnezhad Leili E. Nursing students’ views on code of ethics, commitment to the ethic of, academic dishonesty and neutralization behaviors. J Holist Nurs Midwifery. 2014;24(3):64–71. Google Scholar Wamalwa EM, Okoth JM, Ochanda D. Factors Contributing To Academic Dishonesty Among Nursing Students In Kenya Medical Training College Western Kenya. 2020. Lin W-YC. Self-plagiarism in academic journal articles: from the perspectives of international editors-in-chief in editorial and COPE case. Scientometrics. 2020;123(1):299–319. Article Google Scholar McKibban AR, Burdsal CA. Academic dishonesty: an in-depth investigation of assessing measurable constructs and a call for consistency in scholarship. J Acad Ethics. 2013;11(3):185–97. Alotaibi AM, Alotaibi JS, Alanazy W, Alqahtani M, Nambi G, Shaphe M et al. Nursing Students’ Perspectives on Academic Dishonesty During Examinations and Assignments: A Cross-Sectional Study. Cureus. 2024;16(1). Macale L, Ghezzi V, Rocco G, Fida R, Vellone E, Alvaro R. Academic dishonesty among Italian nursing students: a longitudinal study. Nurse Educ Today. 2017;50:57–61. Article PubMed Google Scholar Woith W, Jenkins SD, Kerber C, editors. Perceptions of academic integrity among nursing students. Nursing forum. Wiley Online Library; 2012. Isakov M, Tripathy A. Behavioral correlates of cheating: environmental specificity and reward expectation. PLoS ONE. 2017;12(10):e0186054. Article PubMed PubMed Central Google Scholar zafarnia.n. Designing and psychometricsproperties of moral competency questionnaire in nurses. kerman medical science; 2017. Hemberg J, Hemberg H. Ethical competence in a profession: Healthcare professionals’ views. Nurs Open. 2020;7(4):1249–59. Kulju K, Stolt M, Suhonen R, Leino-Kilpi H. Ethical competence: a concept analysis. Nurs Ethics. 2016;23(4):401–12. Haghighat S, Borhani F, Ranjbar H. Is there a relationship between moral competencies and the formation of professional identity among nursing students? BMC Nurs. 2020;19(1):1–7. Solum EM, Maluwa VM, Tveit B, Severinsson E. Enhancing students’ moral competence in practice: challenges experienced by Malawian nurse teachers. Nurs Ethics. 2016;23(6):685–97. Torabizadeh C, Homayuni L, Moattari M. Impacts of socratic questioning on moral reasoning of nursing students. Nurs Ethics. 2018;25(2):174–85. Erami E, Adib HM, Dianati M. Ethical competence in nursing: A concept analysis with Walker and Avans approach. 2019. Haghighat S, Borhani F, Ranjbar H, Naseri P. Evaluating the formation of professional identity in Iranian nursing students after implementation of a new curriculum. J Nurs Midwifery Sci. 2019;6(3):138. Slay HS, Smith DA. Professional identity construction: using narrative to understand the negotiation of professional and stigmatized cultural identities. Hum Relat. 2011;64(1):85–107. Johnson M, Cowin LS, Wilson I, Young H. Professional identity and nursing: contemporary theoretical developments and future research challenges. Int Nurs Rev. 2012;59(4):562–9. Article PubMed CAS Google Scholar Hensel D, Middleton MJ, Engs RC. A cross-sectional study of drinking patterns, prelicensure nursing education, and professional identity formation. Nurse Educ Today. 2014;34(5):719–23. Baraz-Pordanjani S, Memarian R, Vanaki Z. Damaged professional identity as a barrier to Iranian nursing students’ clinical learning: a qualitative study. J Clin Nurs Midwifery. 2014;3. Crigger N, Godfrey N. From the inside out: a new approach to teaching professional identity formation and professional ethics. J Prof Nurs. 2014;30(5):376–82. Kruse JA, Didion J, Perzynski K. Strengthening Student nurses’ sense of belonging through attendance at a professional nursing conference. AORN J. 2020;112(3):227–36. Gusar I, Tokić A, Lovrić R. Psychometric analysis of the Professional identity questionnaires in Croatian nursing student context. SAGE Open Nurs. 2021;7:23779608211044600. PubMed PubMed Central Google Scholar Nehrir B. Factors affecting nursing Professional Identity: a systematic review. Iran J Syst Rev Med Sci. 2020;1(2):0. Vaismoradi M, Salsali M, Ahmadi F. Perspectives of Iranian male nursing students regarding the role of nursing education in developing a professional identity: a content analysis study. Japan J Nurs Sci. 2011;8(2):174–83. Krueger L. Academic dishonesty among nursing students. J Nurs Educ. 2014;53(2):77–87. Bloomfield JG, Crawford T, Fisher M. Registered nurses understanding of academic honesty and the perceived relationship to professional conduct: findings from a cross-sectional survey conducted in Southeast Asia. Nurse Educ Today. 2021;100:104794. Allen C. Academic dishonesty among undergraduate nursing students. International Archives of Nursing and Health Care; 2017. Emmanuel E, Fielden J, Miller-Rosser K. Why should we care about academic integrity in nursing students. J Nurs Educ Pract. 2021;11(5):46–53. Barani H, Fooladchang M. Psychometric properties of academic dishonesty scale. Stud Learn Instruction. 2021;12(2):61–84. Bashir H, Bala R. Development and validation of academic dishonesty scale (ADS): presenting a multidimensional scale. Int J Instruction. 2018;11(2):57–74. Hao Y-F, Niu H-J, Li L-P, Yue S-J, Liu X-H. Measurement of professional identity in Chinese nursing students. Int J Nurs Sci. 2014;1(2):137–44. Hao YF. Study the model of self-education in enhancing the level of professional identity and professional self-efficacy in nurse students. (Docter) 2011. Almutairi M, Alharbi TAF, Timmins F. Perceptions of nursing students and faculty members towards academic integrity and professionalism in Saudi Arabia: a cross-sectional study. Nurse Educ Today. 2023;130:105942. Alnajjar P, Hend Abdu, Abou Hashish P, Ebtsam A. Academic ethical awareness and moral sensitivity of undergraduate nursing students: assessment and influencing factors. SAGE open Nurs. 2021;7:23779608211026715. Choi J. Cheating behaviors and related factors at a Korean dental school. Korean J Med Educ. 2019;31(3):239. Gilvari T, Babamohamadi H, Paknazar F. Perceived professional identity and related factors in Iranian nursing students: a cross-sectional study. BMC Nurs. 2022;21(1):279. Cheng Y-C, Hung F-C, Hsu H-M. The relationship between academic dishonesty, ethical attitude and ethical climate: the evidence from Taiwan. Sustainability. 2021;13(21):11615. Bezek SM. Who is taking care of you? A study of the correlation of academic and professional dishonesty. Capella University; 2014. Ranjbar H, Joolaee S, Vedadhir A, Abbaszadeh A, Bernstein C. Becoming a nurse as a moral journey: a constructivist grounded theory. Nurs Ethics. 2017;24(5):583–97. Rahimaghaee F, Nayeri D, Mohammadi E. Iranian nurses perceptions of their professional growth and development. OJIN: Online J Issues Nurs. 2011;16(1):10. Parandeh A, Khaghanizade M, Mohammadi E, Nouri JM. Factors influencing development of professional values among nursing students and instructors: a systematic review. Global J Health Sci. 2015;7(2):284. Lynch J, Everett B, Ramjan LM, Callins R, Glew P, Salamonson Y. Plagiarism in nursing education: an integrative review. J Clin Nurs. 2017;26(19–20):2845–64. Download references AcknowledgementsThe authors would like to thank all nursing students who voluntarily participated in the study. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. Author informationAuthors and affiliations. Student Research Committee , Shiraz University of Medical Sciences, Shiraz, Iran Leila Homayouni Department of E-Learning in Medical Sciences, Virtual School and Center of Excellence in E-Learning, Shiraz University of Medical Sciences, Shiraz, Iran PhD in nursing, Assistant professor, Medical – Surgical department, School of Nursing, Fasa University of Medical Sciences, Fasa, Iran Department of Operating room technology, Community Based Psychiatric Care Research Center, School of Nursing and Midwifery, Shiraz University of Medical Sciences, Fatemeh (PUBH) Nursing Midwifery School, Nemazee Square, Shiraz, 71936-13119, Iran Armin Fereidouni Student Research Committee, Shiraz University of Medical Sciences, Shiraz, Iran Zahra Padam You can also search for this author in PubMed Google Scholar ContributionsStudy conception and design: L.H and AF, Data collection: Z.P, Statistical analysis: A.F.M and Z.P and A.Z, Interpretation of results: A.Z and LH, Drafting of the manuscript: All authors, Revision of the final manuscript: A.F, L.H. Corresponding authorCorrespondence to Armin Fereidouni . Ethics declarationsEthics approval and consent to participate. The present study has been approved by the ethics committee of Shiraz University of Medical Sciences with the Code of Ethics (IR). SUMS. NUMIMG. REC.1401.054 and access link (B2n.ir/z74571). Before completing the questionnaire, participants were informed of the objectives of the study and informed written consent was obtained from each participant electronically before completing the questionnaire. In this study, the participants were not required to mention their names and surnames and the participants were assured of confidentiality and confidentiality. Consent for publicationNot Applicable. Competing interestsThe authors declare no competing interests. Additional informationPublisher’s note. Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Rights and permissionsOpen Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ . Reprints and permissions About this articleCite this article. Homayouni, L., Zare, A., Padam, Z. et al. Investigating academic dishonesty and its relationship with moral competence and professional identity of nursing students: a cross-sectional study. BMC Nurs 23 , 662 (2024). https://doi.org/10.1186/s12912-024-02335-8 Download citation Received : 10 April 2024 Accepted : 09 September 2024 Published : 18 September 2024 DOI : https://doi.org/10.1186/s12912-024-02335-8 Share this articleAnyone you share the following link with will be able to read this content: Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative
BMC NursingISSN: 1472-6955
Exploring the trend of age-standardized mortality rates from cardiovascular disease in Malaysia: a joinpoint analysis (2010–2021)
BMC Public Health volume 24 , Article number: 2519 ( 2024 ) Cite this article Metrics details IntroductionCardiovascular disease (CVD) is a major health concern worldwide, particularly in low- and middle-income countries. The COVID-19 pandemic that emerged in late 2019 may have had an impact on the trend of CVD mortality. This study aimed to investigate the trend and changes in CVD mortality rates in Malaysia, using age-standardized mortality rates (ASMR) from 2010 to 2021. The Malaysian population and mortality data from 2010 to 2021 were obtained from the Department of Statistics Malaysia (DOSM). ASMRs from CVD per 100,000 population were calculated based on the World Health Organization (2000–2025) standard population using the direct method. The ASMRs were computed based on sex, age groups (including premature mortality age, 30–69 years), and CVD types. The annual percent change (APC) and average annual percent change (AAPC) of the ASMR with corresponding 95% confidence intervals (95% CI) were estimated from joinpoint regression model using the Joinpoint Regression Program, Version 4.9.1.0. Throughout the study period (2010–2021), ASMRs for CVD exhibited an increase from 93.1 to 147.0 per 100,000, with an AAPC of 3.6% (95% CI: 2.1 to 5.2). The substantial increase was observed between 2015 and 2018 (APC 12.6%, 95% CI: 5.4%, 20.3%), with significant changes in both sexes, and age groups 50–69, 70 years and over, and 30–69 (premature mortality age). Notably, the ASMR trend remained consistently high in the premature mortality age group across other age groups, with males experiencing higher rates than females. No significant changes were detected before or after the COVID-19 pandemic (between 2019 and 2021), except for females who died from IHD (10.3% increase) and those aged 0–4 (25.2% decrease). Overall, our analysis highlights the persistently high burden of CVD mortality in Malaysia, particularly among the premature mortality age group. These findings underscore the importance of continued efforts to address CVD risk factors and implement effective prevention and management strategies. Further research is needed to fully understand the impact of the COVID-19 pandemic on CVD mortality rates and to inform targeted interventions to reduce the burden of CVD in Malaysia. Peer Review reports Cardiovascular disease (CVD) is the leading cause of death worldwide, responsible for approximately one-third of all deaths globally [ 1 , 2 ]. Low- and middle-income countries (LMICs) bear a disproportionate burden of CVD, accounting for 32% of all CVD deaths [ 3 ]. Despite declining age-standardized mortality rates (ASMR) in high-income regions, most LMICs have not experienced similar reductions [ 4 , 5 ]. Instead, there has been an increase in premature mortality (deaths that occur at a younger age than expected) from CVD in LMICs [ 6 ]. Recognizing this alarming trend, there is a global commitment to reducing premature CVDs by 25% by the year 2025 [ 7 ]. While significant progress has been made in preventing and treating CVD, there are notable disparities among different subpopulations, and the trend for CVD mortality has been inconsistent globally [ 5 , 8 , 9 , 10 , 11 , 12 ]. Malaysia, classified as an LMIC, also faces a significant burden of CVD, particularly ischemic heart disease (IHD) and stroke [ 13 ]. Changes in CVD mortality trends can be attributed to several factors. Adverse conditions or behaviours related to modifiable risk factors such as diabetes, obesity, lack of physical activity, hypertension, an unhealthy diet, smoking, and excessive alcohol consumption are associated with an increase in CVD mortality trends [ 4 , 14 , 15 , 16 ]. Without reducing these risk factors, it is predicted that almost 23.6 million people will die from CVDs by 2030 [ 17 ]. Other factors, including an aging population [ 18 ], environmental factors [ 19 ], and changes in healthcare access and quality [ 15 ], may contribute to these disparities in the trend for CVD mortality. In addition to these factors, the COVID-19 pandemic, which began in late December 2019 [ 20 ] has had a significant impact on the healthcare system and may have affected the trend for CVD mortality. For example, the pandemic resulted in excess all-cause mortality in the USA [ 21 ] and in a multi-country study using data from 74 countries worldwide [ 22 ]. In Poland, in-hospital mortality for acute heart failure increased [ 23 ], whereas in Sweden, CVD mortality, particularly from IHD and myocardial infarction, decreased substantially during 2020 [ 24 ]. Several countries reported a decrease in hospitalizations and percutaneous coronary interventions during the COVID-19 pandemic, likely leading to a reduction in recorded mortality from cardiac events [ 25 , 26 , 27 ]. Lockdowns and prioritization of COVID-19 care may have indirectly affected diseases like CVDs that require a functional healthcare system [ 28 , 29 ]. Thus, analysing mortality trends allows for understanding the indirect impacts of the pandemic on health outcomes, identifying gaps in healthcare delivery, and developing strategies to mitigate these impacts. Joinpoint analysis is a statistical method that is commonly used to detect changes in trends or patterns in data over time, and it has been used in many previous studies to investigate the burden of various diseases, including CVD [ 30 , 31 , 32 , 33 ]. Investigating the trend for CVD mortality within a country is crucial, particularly in LMICs like Malaysia. However, to date, the trend and any change in trend of ASMR from CVD in Malaysia have not been investigated over the past decade, including the impact of COVID-19 on CVD mortality rates. Using joinpoint analysis to analyse Malaysian data will provide valuable insights into the temporal patterns of CVD mortality occurrence in Malaysia and help inform policy and intervention strategies to reduce the burden of CVD in the country. Moreover, it will contribute to the literature on CVD mortality trends and change point analysis, particularly in LMICs, and provide a basis for future studies on CVD mortality in the region. Therefore, this study aims to explore the change in trend of ASMR from CVD in Malaysia from 2010 to 2021. Specifically, we aim to identify any changes in trends according to sex, major CVD types, and age group, including premature mortality. Furthermore, we aim to assess any changes in the CVD mortality trend within each subgroup before and after the COVID-19 pandemic. Source of dataData on CVD mortality and Malaysian population (census and inter-census years) were obtained from the Department of Statistics Malaysia (DOSM) for the period 2010–2021. Malaysian law mandates that all deaths be registered with the National Registration Department (NRD), which issues death certificates [ 34 ]. Deaths in Malaysia are categorized into medically certified deaths, which occur in health facilities and are determined by medical officers based on symptoms and examination, and non-medically certified deaths, which occur outside health facilities. While death registration quality is an issue in many countries [ 35 ]. Malaysia stands out as one of the few Asian countries with a functioning vital registration system. Analysing trends from 1995 to 2010, medically certified deaths increased over time, while non-medically certified deaths remained stable [ 36 ]. In 1995, non-medically certified deaths were 55%, surpassing medically certified deaths at 45% [ 36 ]. In 2021, DOSM reported an improvement, with medically certified deaths at 70.0% and non-medically certified deaths at 30.0% [ 37 ]. In Malaysia, death certificates document a clear sequence of events leading to death. The cause of death listed on the lowermost line of the sequence, which initiated the train of events leading to death, is defined as the underlying cause of death. All other causes listed on the lines between the underlying cause (on the lowermost line) and the immediate cause (on the topmost line) are referred to as antecedent causes of death [ 38 ]. DOSM is responsible for cleaning and classifying cause-of-death information for all medically certified deaths obtained from the NRD, coding them based on the 10th International Classification of Diseases (ICD-10) [ 39 ]. This process is carried out by specialized coders at DOSM. To ensure the study’s quality and enhance the accuracy of cause-of-death information, only medically certified deaths for CVD as indicated by ICD-10 (code I01-I99) were used for this analysis. The unknown cause of death and missing information on age and sex were excluded. Statistical analysisWe estimated ASMRs per 100,000 population for all medically certified deaths from CVD. The World (WHO 2000–2025) Standard population [ 40 ] was used as the reference population to calculate ASMR, based on the direct method of age-standardization. The use of a standard population is important to enable comparability between relevant years and rates from other countries. To calculate the ASMR using direct standardization, we first aggregated the number of CVD deaths into 5-year age intervals (0–4, 5–9, 10–14, 15–19, 20–24, 25–29, 30–34, 35–39, 40–44, 45–49, 50–54, 55–59, 60–64, 65–69, 70–74, 75–79 and 80+) for each year of study. Next, we calculated the age-specific mortality rates by dividing the number of deaths in a specific age group by the number of people in that age group and then multiplying the result by 100,000. Finally, the ASMR was calculated by multiplying the age-specific death rate by the weight of that age group in the standard population [ 40 ]. This direct standardization method was applied to calculate the overall ASMR, and stratified by gender (male and female), CVD type (IHD and stroke), and selected specific age ranges (e.g., 0–1, 30–49, 50–59 years). To explore the trend for premature CVD mortality, we also selected a specific age group of 30–69 years, in accordance with the WHO definition of premature mortality [ 41 ]. The descriptive statistics of ASMR and trend plots were analysed using R software. Joinpoint regression analysis was utilized to detect the significant changes in annual ASMR for CVD mortality from 2010 to 2021 according to sex, age groups and CVD types. A joinpoint regression model was employed to estimate the magnitude of change in the trend of CVD mortality rates over time. This model allows us to identify points in time, where significant changes occur in the trend. Additionally, the model provides a confidence measure around these estimated changes. We used the Joinpoint Regression Program, Version 4.9.1.0 for this analysis [ 42 ]. The Joinpoint program fits a series of straight lines to the ASMRs on a log scale and detects the best fitting points, called ‘joinpoints’ [ 43 ]. This program selects the final model using two methods; the Monte Carlo permutation tests and the Bayesian Information Criterion (BIC) [ 43 ]. The analysis starts with the minimum number of joinpoints (e.g., zero joinpoints, which is a straight line), and tests whether one or more joinpoints are significant and must be added to the model. Based on the recommendation of the Joinpoint program, a maximum of two joinpoints can be selected for the given 12 data points [ 42 ]. Permutation tests determine the number of joinpoints by comparing different hypotheses until the final number is reached. Starting with ka = minimum number of joinpoint and kb = maximum number of joinpoint, each test compares the null hypothesis H0: number of joinpoints = ka against the alternative Ha: number of joinpoints = kb, where ka < kb. If the null hypothesis is rejected, ka is increased by 1; otherwise, kb is decreased by 1. This process continues until ka = kb, and the final value is the selected number of joinpoints. Then, models with this number of joinpoints are compared using BIC, and the model with the minimum BIC value is selected as the optimal model [ 44 ]. To describe changes in CVD mortality rates, the annual percent change (APC) of the ASMR between the trend-change point and the average annual percent change (AAPC) in the whole period studied was calculated with corresponding 95% confidence intervals (95% CI). We applied the log transformation to calculate the APC. This approach assumes that CVD mortality rates change at a constant percentage relative to the rate of the previous year, and the log transformation allows for linear changes on a logarithmic scale. To derive the APC for a given data series, the following regression model is employed [ 45 ]; where \(\text{log}\left({R}_{y}\right)\) is the natural log of the rate in year \(y\) . \({b}_{0}\) is the intercept, representing the value of the natural log of the rate when \(y=0,\) and \({b}_{1}\) is the slope, indicating the rate of change in the natural log of the rate per year. The APC from year \(y\) to year \(y\) + 1 is derived from this formula The formula is further transformed to represent an annual percent change;. The AAPC was calculated to summarize the trend over a specific fixed interval (2010–2021), allowing for the use of a single number to describe the APCs over multiple years. The AAPC is computed by taking a weighted average of the APCs from the joinpoint model, with the weights determined by the length of each APC interval. The AAPC over any fixed interval is calculated by taking a weighted average of the slope coefficients of the underlying joinpoint regression model, where the weights correspond to the length of each segment within the interval [ 46 ]. APC i = {exp(b i ) − 1} x 100. where b i is the slope coefficient for the i th segment (within the desired range of years). In the calculation, the weighted average of slope coefficients is further transformed to represent an average annual percent change [ 46 ]; where w i is the length of each segment within that range. The Joinpoint Regression Program performs a series of hypothesis tests. These tests compare the null hypothesis (the assumption of no trend or no joinpoints) against alternative hypotheses with different numbers of joinpoints. A small p -value indicates strong evidence against the null hypothesis, suggesting significant trends or joinpoints. The trend was considered to be significantly increasing (positive change) or decreasing (negative change) when the p -value was below 0.05 ( p < 0.05). Table 1 shows the demographic structure of the Malaysian population and the age standardized mortality rate from CVD. The Malaysian population is systematically increasing for the period 2010–2021 from 28.6 million to 32.6 million [ 47 ]. During the observed period, 1.9 million deaths (from all causes) were recorded in Malaysia, of which 318,268 deaths (16.6%) were caused by CVD. Age standardised mortality rateThe ASMR ranged from 88.1 to 147.0 per 100,000 population (Table 1 ). The overall ASMR showed an increase trend from 93.1 to 147.0 deaths per 100,000 population from 2010 to 2021, but with small variation between years. During the study period, the rates were almost twice as high in men as in women. The trend shown increases in both sexes and the main CVD types (IHD and stroke). Although all of the rates increased over the period of study, the pattern of increase varied across age groups. Figure 1 shows that the ASMR trend in males was highest among those aged 30–69 years (defined as premature mortality), whereas in females, the highest rate was observed in those over 70 years of age. We detected that the trend for both sexes was rising and peaking in 2018, particularly among the premature mortality age group and those over 50. Meanwhile, the mortality trend among adolescents and children below the age of 15 for both sexes has almost plateaued over the years.  The ASMR trend from CVD in Malaysia from 2010 to 2021; ( A ) Overall population by age group; ( B ) Male by age group and ( C ) Female by age group Joinpoint regression modelTable 2 shows the joinpoint regression analysis of ASMR for total CVD and the model for both sexes stratified by age group and CVD type. The jointpoint model demonstrated a statistically significant increase in ASMR for CVD, with an AAPC of 3.6% (95% CI: 2.1, 5.2) during the entire study period (2010 to 2021). However, when we looked at a specific segment, the trend was slightly decreasing between 2010 and 2015, with an APC of -2.2% (95% CI: -3.6, -0.7), and a substantial increase between 2015 and 2018, with an APC of 12.6% (95% CI: 5.4, 20.3). Between 2018 and 2021, the rate increased slightly (APC: 5.0%, 95% CI: 1.6%, 8.6%), and no significant changes were detected before or after the COVID-19 pandemic (2019–2021). These changes in ASMRs exhibited similar patterns in both men and women, with large increments occurring between 2015 and 2018. The analysis of trends by age strata (Table 2 ) demonstrated the large increase between 2015 and 2018 was contributed by the age groups 50–59, ≥ 70 years, and premature mortality group, with APCs of 9.5%, 16.7%, and 9.3%, respectively. Meanwhile, the reduction in trend between 2010 and 2015 was notable among females aged 50–69 (reduced by -2.3%) and both male and female aged ≥ 70 age groups (reduced by -3.6% in females and − 3.9% in males). Interestingly, among premature CVD mortality (age 30–69), the trend was systematically increasing throughout the study period, where the reduction slopes between 2010 and 2015 were not statistically significant. In addition, the AAPC during the observed study (2010–2021) only significantly increased among the aged group over 30 years. Meanwhile, the mortality rate in the age group below 30 years was nearly constant, and the trend in this subgroup was not statistically significant, except for those aged 0–4 years, who showed a significant decline in trend (reduced by 25.5%) from 2019 to 2021. Figures 2 and 3 present the joinpoint model plots illustrating the overall ASMR trend from CVD, as well as the trends by sex and age group. In terms of CVD subtype, both IHD and stroke showed an upward trend between 2010 and 2021, with AAPC rates of 3.9% and 3.4%, respectively (Table 2 ). Although females reported lower ASMR from IHD and stroke than males, females had a greater increase in trend for IHD and stroke. Specifically, the AAPC for females was 4.5% for IHD and 3.6% for stroke, whereas for males it was 3.8% for IHD and 3.3% for stroke. During the period from 2019 to 2021, which encompasses the pre- and post-COVID-19 pandemic eras, our joinpoint analysis revealed significant changes in CVD mortality rates among females. Specifically, there was a notable increase in the mortality rate due to IHD among females, with an APC of 10.3%. Additionally, there was a significant decrease in mortality among female children aged 0–4, with an APC of -25.2%. However, it’s important to note that significant changes among males were detected between 2018 and 2021, which falls outside the defined pre- and post-COVID-19 pandemic period of 2019–2021.  Joinpoint regression model of age standardised mortality rate (ASMR) per 100,000 from CVD in Malaysia, 2010–2021 for overall CVD ( a ) and by sex ( b )  Joinpoint regression model of age standardised mortality rate (ASMR) per 100,000 from CVD in Malaysia, 2010-2021by age group in male ( a ) and female ( b ) In this study, we conducted joinpoint analysis to identify and measure temporal patterns of ASMR on CVD mortality in Malaysia from 2010 to 2021. These analytical methods proved useful in understanding the underlying drivers of the observed trends and their implications for policies and interventions. Our findings indicated an overall increase in ASMR from CVD over the study period (AAPC of 3.6%) with a large increment occurring between 2015 and 2018 (APC of 12.6%). Interestingly, we detected a slight decrease in the trend between 2010 and 2015 (APC of -2.2%). This descending trend in CVD mortality aligns with other reports worldwide. For example, the findings from the GBD Study 2017 reported that nearly all countries, including developing countries and regions like Southeast Asia, experienced a significant declining trend in age-standardized CVD mortality rates from 1990 to 2017 [ 48 ]. A study by Khan et al. revealed that the global mortality trend of IHD decreased slowly but progressively from 1990 to 2017 [ 49 ]. They suggested that this reduction may be partly due to increasing global awareness of lifestyle factors. Another study showed that the ASMR of stroke decreased sharply by 33.4% over the same period [ 50 ]. However, several epidemiological studies have reported a global trend of age-standardized CVD mortality rates either slightly declining or increasing in most LMICs, while high-income regions have experienced a significant reduction [ 4 , 18 ]. For example, a study in Central Asia (comprising LMICs) found that CVD mortality trends have risen over the past two decades [ 51 ]. The researchers attributed this rise to factors such as inadequate preventive care, low awareness of disease signs and symptoms, reduced physical activity, elevated blood pressure, and insufficient utilization of healthcare services. Although a slight reduction occurred before 2015, our joinpoint model suggests that the ASMR for CVD in Malaysia increased throughout the study period (2010–2021). The observed increase in ASMR from CVD in this country may be attributed to a combination of factors, including urbanization, changes in lifestyle and dietary habits, and a shift towards more sedentary lifestyles [ 52 , 53 , 54 ]. These factors have contributed to unhealthy, high-calorie diets, leading to the development of metabolic disorders like obesity and diabetes, which are well-known risk factors for CVD. Over the past decade, Malaysia has experienced a significant increase in the prevalence of several metabolic disorders, including obesity, diabetes, hypertension, and hypercholesterolemia. According to the National Health and Morbidity Survey (NHMS), the prevalence of obesity among adults in Malaysia has risen from 14.0% in 2006 [ 55 ] to 17.7% in 2019 [ 56 ], while the prevalence of diabetes has increased from 11.6% in 2006 [ 55 ] to 18.3% in 2019 [ 56 ]. The survey also showed that the prevalence of hypertension and hypercholesterolemia among adults in Malaysia has been increasing from 32.2% and 20.6% in 2006 [ 55 ] to 43.5% and 47.7% in 2019 [ 56 ], respectively. These trends are concerning, as these metabolic disorders are significant risk factors for CVD, which could contribute to the observed increase in ASMR from CVD in Malaysia. Additionally, Malaysia is experiencing a demographic transition due to an increasing aged population ≥ 60 years and increased life expectancy [ 57 ]. Population aging is becoming the most important driver of the CVD epidemic [ 58 ]. On the other hand, increased access to healthcare and better medical treatment for CVD [ 59 , 60 ] may have also led to higher reported CVD mortality rates. Firstly, increased access to healthcare can lead to better detection and diagnosis of CVD cases, including previously undiagnosed or asymptomatic cases. As a result, more individuals with CVD are identified and included in mortality statistics, thus contributing to higher reported mortality rates. Secondly, better medical treatment for CVD can prolong the lives of individuals with the condition. While this is beneficial for improving individual health outcomes, it can also increase the pool of individuals living with CVD, who are at risk of dying from CVD-related complications in the long term. This, in turn, can lead to higher reported mortality rates. While there has been an overall upward trend in CVD mortality rates, our joinpoint regression analysis only identified significant changes pre- and post-COVID-19 outbreak (2019–2021) among females who died from IHD and females aged 0–4 years, with no significant changes detected in other subgroups during this period (2019–2021). It is important to note that the impact of COVID-19 on CVD mortality rates during the early phases of the pandemic is inconsistent, with some countries reporting a decrease in CVD mortality [ 61 , 62 , 63 ] and others having observed an increase or excess mortality [ 64 , 65 , 66 ]. While our data is limited to one-year post-COVID-19 pandemic (2021), the study by Jayaraj et al. [ 67 ] on all-cause mortalities in Malaysia between January 2016 and September 2021 also utilized similar post-COVID data points up to 2021. Their results show a reduction in all-cause mortality in 2020, especially during the first Movement Control Order, followed by a significant increase between July and September 2021. This pattern supports our findings and might explain why the APC did not show significant changes between 2019–2021 in our study, despite an overall significant increase in the APC between 2018–2021. Additionally, the use of monthly data points with all causes of death in their study might have allowed for more precise detection of changes in trends during the COVID-19 pandemic compared to our study, which used yearly data points with specific causes of death. On the other hand, our study highlights the persistent burden of premature CVD mortality (age 30–69) in Malaysia, which is in line with the trend of increasing global premature CVD mortality observed in LMICs [ 1 ]. Furthermore, there are notable sex disparities, with higher rates of premature CVD mortality among males compared to females. This finding is consistent with the results of Zhang et al. (2021) [ 68 ], who reported a 35.6% higher overall premature CVD mortality rate among men than women, based on global data from the WHO Global Health Estimates (GHE). Other studies [ 69 , 70 , 71 ] have also highlighted sex disparities related to premature CVD mortality. In addition, our study revealed that while males had a higher overall ASMR than females, the magnitude of increase during the entire study period (2010–2021) was greater among females (AAPC 3.8% in females versus 3.5% in males). Notably, females aged over 70 years exhibited the highest ASMR over time compared to other age groups. These findings are consistent with the observations of Roth et al. [ 1 ], who reported a rapid increase in the proportion of CVD-related deaths among women after the age of 70, surpassing that among men. However, Roth et al. found that this trend is driven predominantly by stroke mortality, whereas our findings show that IHD had a higher increment among Malaysian females. These findings highlight the importance of targeted interventions and policies to address sex-specific CVD types and age-related disparities in ASMR from CVD mortality in Malaysia. Study limitationsThe study had some limitations that should be taken into consideration when interpreting the results. Firstly, the use of yearly data points and the lack of post-COVID-19 outbreak observation may have contributed to the insignificant findings of changes in the overall CVD mortality trend and most of the subgroup during the pre- and post-COVID-19 outbreak period (2019–2021). Therefore, the true burden of the effect of COVID-19 on CVD deaths should be interpreted with caution. Despite this limitation, our intention to examine the potential impact of the early COVID-19 pandemic on CVD mortality remains relevant, as evidenced by the significant APC detected during the pre- and post-COVID-19 period (2019–2021) in certain groups (e.g., females with IHD). Additionally, the study was limited by the variables available in the death registry, which did not include information on other modifiable risk factors such as diabetes, hypertension, and alcohol use, as well as important sociodemographic factors such as ethnic group, regional area, income level, and employment status. These variables may have been important to adjust or stratify in the joinpoint regression analysis. Furthermore, the study may not have represented the total CVD deaths in Malaysia, as it relied only on medically certified deaths. However, the use of the most complete and accurate data on CVD death, with ICD-10 coding conducted by specialist coders from DOSM and validated by independently certified coders, is a strength of the study. In conclusion, this study highlights the increasing trend in ASMR from CVD in Malaysia, with a substantial increase observed between 2015 and 2018. The findings also underscore the ongoing burden of premature CVD mortality in the country, particularly among males. Efforts to address CVD risk factors and implement effective prevention and management strategies should be continued, including public health campaigns to raise awareness about healthy lifestyle behaviours, enhancing access to affordable and quality healthcare services, strengthening primary healthcare systems, investing in community-based interventions, and promoting multi-sectoral collaboration. Further research is warranted to explore the specific impact of the COVID-19 pandemic on CVD mortality rates in Malaysia and to guide the development of targeted interventions to mitigate its effects. Data availabilityThe mortality data used in this study were obtained from a restricted source (Department of Statistics Malaysia). The population structure in Malaysia is available online ( https://pqi.stats.gov.my ). We confirm that all methods were carried out in accordance with the relevant guidelines and regulations. Abbreviationsthe average annual percent change. the annual percent change. Ischemic heart disease (ICD-10 code: I20-I25). including all cerebrovascular disease. Roth GA, Huffman MD, Moran AE, Feigin V, Mensah GA, Naghavi M, et al. Global and regional patterns in cardiovascular mortality from 1990 to 2013. Circulation. 2015;132:1667–78. Article PubMed Google Scholar Vos T, Lim SS, Abbafati C, Abbas KM, Abbasi M, Abbasifard M, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of Disease Study 2019. Lancet. 2020;396:1204–22. Article Google Scholar WHO. Cardiovascular diseases (CVDs): Key Facts. In: Word Health Organization (WHO) [Internet]. 2021 [cited 9 Oct 2022]. Available: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds ). Jagannathan R, Patel SA, Ali MK, Narayan KMV. Global updates on Cardiovascular Disease Mortality trends and Attribution of traditional risk factors. Curr Diab Rep. 2019;19:44. https://doi.org/10.1007/s11892-019-1161-2 Levi F, Lucchini F, Negri E, La Vecchia C. Trends in mortality from cardiovascular and cerebrovascular diseases in Europe and other areas of the world. Heart. 2002;88:119–24. Article PubMed PubMed Central CAS Google Scholar Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J Am Coll Cardiol. 2020;76:2982–3021. Article PubMed PubMed Central Google Scholar WHO. Global action plan for the prevention and control of noncommunicable diseases 2013–2020. World Health Organization (WHO); 2013. Wang H, Naghavi M, Allen C, Barber R, Bhutta M. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the global burden of Disease Study 2015. Lancet. 2016;388:1459–544. https://doi.org/10.1016/S0140-6736(16)31012-1 Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the global burden of Disease Study 2010. Lancet. 2012;380:2095–128. https://doi.org/10.1016/S0140-6736(12)61728-0 Global regional. National age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the global burden of Disease Study 2013. Lancet. 2015;385:117–71. https://doi.org/10.1016/S0140-6736(14)61682-2 Moran AE, Forouzanfar MH, Roth GA, Mensah GA, Ezzati M, Murray CJL, et al. Temporal trends in ischemic heart disease mortality in 21 world regions, 1980 to 2010: the global burden of Disease 2010 study. Circulation. 2014;129:1483–92. Hartley A, Marshall DC, Salciccioli JD, Sikkel MB, Maruthappu M, Shalhoub J. Trends in mortality from ischemic heart disease and cerebrovascular disease in Europe: 1980 to 2009. Circulation. 2016;133:1916–26. Global Burden of Disease. The Global Burden of Disease Study 2010 (GBD 2010): GBD profile Malaysia. 2010 p. 131. Zhang Y-B, Pan X-F, Chen J, Cao A, Xia L, Zhang Y, et al. Combined lifestyle factors, all-cause mortality and cardiovascular disease: a systematic review and meta-analysis of prospective cohort studies. J Epidemiol Community Health. 2021;75:92–9. Ezzati M, Obermeyer Z, Tzoulaki I, Mayosi BM, Elliott P, Leon DA. Contributions of risk factors and medical care to cardiovascular mortality trends. Nat Rev Cardiol. 2015;12:508–30. Yusuf S, Hawken S, Ôunpuu S, Dans T, Avezum A, Lanas F, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:937–52. https://doi.org/10.1016/S0140-6736(04)17018-9 Mathers CD, Loncar D. Projections of global mortality and Burden of Disease from 2002 to 2030. PLoS Med. 2006;3:e442. https://doi.org/10.1371/journal.pmed.0030442 Roth GA, Forouzanfar MH, Moran AE, Barber R, Nguyen G, Feigin VL, et al. Demographic and epidemiologic drivers of global cardiovascular mortality. N Engl J Med. 2015;372:1333–41. Cosselman KE, Navas-Acien A, Kaufman JD. Environmental factors in cardiovascular disease. Nat Rev Cardiol. 2015;12:627–42. Article PubMed CAS Google Scholar WHO. WHO announces COVID-. 19 outbreak a pandemic – WHO Director- General’s opening remarks at the media briefing on COVID- 19. In: World Health Organization (WHO) [Internet]. 2020 [cited 26 Mar 2022]. Available: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 Woolf SH, Chapman DA, Sabo RT, Weinberger DM, Hill L. Excess deaths from COVID-19 and other causes, March-April 2020. JAMA. 2020;324:510. https://doi.org/10.1001/jama.2020.11787 Wang H, Paulson KR, Pease SA, Watson S, Comfort H, Zheng P, et al. Estimating excess mortality due to the COVID-19 pandemic: a systematic analysis of COVID-19-related mortality, 2020–21. Lancet. 2022. https://doi.org/10.1016/S0140-6736(21)02796-3 Kubica J, Ostrowska M, Stolarek W, Kasprzak M, Grzelakowska K, Kryś J, et al. Impact of COVID-19 pandemic on acute heart failure admissions and mortality: a multicentre study (COV‐HF‐SIRIO 6 study). ESC Heart Fail. 2022;9:721–8. https://doi.org/10.1002/ehf2.13680 Axenhus M, Schedin-Weiss S, Winblad B, Wimo A. Changes in mortality trends amongst common diseases during the COVID-19 pandemic in Sweden. Scand J Public Health. 2021;140349482110646. https://doi.org/10.1177/14034948211064656 Solomon MD, McNulty EJ, Rana JS, Leong TK, Lee C, Sung S-H, et al. The Covid-19 pandemic and the incidence of acute myocardial infarction. N Engl J Med. 2020;383:691–3. De Filippo O, D’Ascenzo F, Angelini F, Bocchino PP, Conrotto F, Saglietto A, et al. Reduced rate of hospital admissions for ACS during Covid-19 outbreak in Northern Italy. N Engl J Med. 2020;383:88–9. Garcia S, Albaghdadi MS, Meraj PM, Schmidt C, Garberich R, Jaffer FA, et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75:2871–2. Driggin E, Madhavan MV, Bikdeli B, Chuich T, Laracy J, Biondi-Zoccai G, et al. Cardiovascular considerations for patients, Health Care Workers, and Health systems during the COVID-19 pandemic. J Am Coll Cardiol. 2020;75:2352–71. https://doi.org/10.1016/j.jacc.2020.03.031 Doupis J, Avramidis K. Managing diabetes during the COVID-19 pandemic. Eur Endocrinol. 2020;16:85. https://doi.org/10.17925/EE.2020.16.2.85 Qiu D, Katanoda K, Marugame T, Sobue T. A joinpoint regression analysis of long-term trends in cancer mortality in Japan (1958–2004). Int J Cancer. 2009;124:443–8. Wong MCS, Fung FDH, Leung C, Cheung WWL, Goggins WB, Ng CF. The global epidemiology of bladder cancer: a joinpoint regression analysis of its incidence and mortality trends and projection. Sci Rep. 2018;8:1129. Wilson L, Bhatnagar P, Townsend N. Comparing trends in mortality from cardiovascular disease and cancer in the United Kingdom, 1983–2013: joinpoint regression analysis. Popul Health Metr. 2017;15:23. https://doi.org/10.1186/s12963-017-0141-5 Gawryszewski VP, de Souza M. FM de. Mortality due to cardiovascular diseases in the Americas by region, 2000–2009. Sao Paulo Medical Journal. 2014;132: 105–110. Malaysian Legislation. Births and Deaths Registration Act 1957 (Revised 1983). In: Commissioner of Law Revision, Malaysia under the authority of the Revision of Laws Act 1968 in collaboration with Percetakan Nasional Malaysia Bhd [Internet]. 2006 [cited 21 Aug 2023]. Available: http://www.commonlii.org/my/legis/consol_act/badra19571983376/ Mathers CD, Ma Fat D, Inoue M, Rao C, Lopez AD. Counting the dead and what they died from: an assessment of the global status of cause of death data. Bull World Health Organ. 2005;83:171–c177. PubMed PubMed Central Google Scholar Adnan TH, Bujang MA, Supramaniam P, Mustaâ N, Lazim SSMAT, Haniff J et al. Trend Analysis of medically certified death in Malaysia, 1995–2010. J Health Inf Dev Ctries. 2012;6. DOSM. Statistics on Cause of Death, Malaysia, 2022. In: Copyright ©2023 Department of Statistics Malaysia (DOSM) [Internet]. 2023 [cited 21 Aug 2023]. Available: https://www.dosm.gov.my/site/downloadrelease?id=statistics-on-causes-of-death-malaysia-2022&=English Malaysia DCDM. of H. Manual for Cause of Death Assignment: Verification of Non-Medically Certified Death Data. Ministry of Health Malaysia, Malaysia; Available: https://www.moh.gov.my/moh/resources/Penerbitan/Rujukan/NCD/Kanser/Manual_for_Cause_of_Death_Assignment.pdf National Center for Health Statistics. International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM). In: National Center for Health Statistics, CDC [Internet]. 2022 [cited 26 Mar 2022]. Available: https://www.cdc.gov/nchs/icd/icd10cm.htm Ahmad OB, Boschi-Pinto C, Lopez AD, Murray CJL, Lozano R, Inoue M et al. Age standardization of rates: a new WHO standard. Geneva: World Health Organization. 2001;9: 1–14. WHO. Indicator Metadata Registry List. Premature mortality from noncommunicable disease. In: World Health Organization (WHO) [Internet]. 2023 [cited 30 Mar 2023]. Available: https://www.who.int/data/gho/indicator-metadata-registry/imr-details/3411 National Cancer Institute. Joinpoint Regression Program, Version 4.0. 4. Statistical methodology and Applications Branch. Surveillance Research; 2013. Kim H-J, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19:335–51. Zhang NR, Siegmund DO. A modified Bayes Information Criterion with Applications to the Analysis of Comparative Genomic Hybridization Data. Biometrics. 2007;63:22–32. https://doi.org/10.1111/j.1541-0420.2006.00662.x National Cancer Institute. Joinpoint Regression Program: Annual Percent Change (APC) and Confidence Interval. 2013. Available: https://surveillance.cancer.gov/help/joinpoint/setting-parameters/method-and-parameters-tab/apc-aapc-tau-confidence-intervals/estimate-average-percent-change-apc-and-confidence-interval National Cancer Institute. Joinpoint Regression Program: Average Annual Percent Change (AAPC) and Confidence Interval. 2013. Available: https://surveillance.cancer.gov/help/joinpoint/setting-parameters/method-and-parameters-tab/apc-aapc-tau-confidence-intervals/average-annual-percent-change-aapc DOSM. Population Projection (Revised), Malaysia, 2010–2040. In: Department of Statistics Malaysia (DOSM) [Internet]. 2022 [cited 30 Mar 2023]. Available: https://www.dosm.gov.my/v1/index.php?r=column/ctheme&menu_id=L0pheU43NWJwRWVSZklWdzQ4TlhUUT09&bul_id=Y3kwU2tSNVFDOWp1YmtZYnhUeVBEdz09 Amini M, Zayeri F, Salehi M. Trend analysis of cardiovascular disease mortality, incidence, and mortality-to-incidence ratio: results from global burden of disease study 2017. BMC Public Health. 2021;21:1–12. Khan MAB, Hashim MJ, Mustafa H, Baniyas MY, Al Suwaidi SKBM, AlKatheeri R et al. Global epidemiology of ischemic heart disease: results from the global burden of disease study. Cureus. 2020;12. Avan A, Digaleh H, Di Napoli M, Stranges S, Behrouz R, Shojaeianbabaei G, et al. Socioeconomic status and stroke incidence, prevalence, mortality, and worldwide burden: an ecological analysis from the global burden of Disease Study 2017. BMC Med. 2019;17:1–30. Altyn, Aringazina Tleuberdi, Kuandikov Viktor, Arkhipov. Burden of the cardiovascular diseases in central Asia Central Asian J Global Health. 2018;7(1). https://doi.org/10.5195/cajgh.2018.321 Goh E, Von, Azam-Ali S, McCullough F, Roy Mitra S. The nutrition transition in Malaysia; key drivers and recommendations for improved health outcomes. BMC Nutr. 2020;6:1–14. Hawkes C, Chopra M, Friel S. Globalization, trade, and the nutrition transition. Globalization and health. Routledge; 2009. pp. 257–284. Popkin BM, Adair LS, Ng SW. Global nutrition transition and the pandemic of obesity in developing countries. Nutr Rev. 2012;70:3–21. Institute for Public Health. The Third National Health and Morbidity Survey (NHMS III). 2006: General Findings. 2008. Available: https://iku.gov.my/images/IKU/Document/REPORT/2006/GeneralFindings.pdf Institute for Public Health. National Health and Morbidity Survey (NHMS). 2019: Vol. I: NCDs–Non-Communicable Diseases: Risk Factors and Other Health Problems. Ministry of Health Malaysia Setia Alam, Malaysia; 2020. Jacob R. Aging and current trends in Malaysia. Int J Social Work Hum Serv Pract. 2016;4:57–61. Google Scholar Dominguez LJ, Galioto A, Ferlisi A, Pineo A, Putignano E, Belvedere M, et al. Ageing, lifestyle modifications, and cardiovascular disease in developing countries. J Nutr Health Aging. 2006;10:143. PubMed CAS Google Scholar Merican I, bin Yon R. Health care reform and changes: the Malaysian experience. Asia Pac J Public Health. 2002;14:17–22. Thomas S, Beh L, Nordin R, Bin. Health care delivery in Malaysia: changes, challenges and champions. J Public Health Afr. 2011;2. Banerjee A, Chen S, Pasea L, Lai AG, Katsoulis M, Denaxas S, et al. Excess deaths in people with cardiovascular diseases during the COVID-19 pandemic. Eur J Prev Cardiol. 2021;28:1599–609. Normando PG, Araujo-Filho J, de Fonseca A, de Rodrigues G, Oliveira REF, Hajjar VA. LA, Reduction in hospitalization and increase in mortality due to cardiovascular diseases during the COVID-19 pandemic in Brazil. Arq Bras Cardiol. 2021. Santos AM dos, de Souza BF, de Carvalho CA, Campos MAG, de Oliveira BLCA, Diniz EM et al. Excess deaths from all causes and by COVID-19 in Brazil in 2020. Rev Saude Publica. 2021;55. Roth GA, Emmons-Bell S, Alger HM, Bradley SM, Das SR, De Lemos JA, et al. Trends in patient characteristics and COVID-19 in-hospital mortality in the United States during the COVID-19 pandemic. JAMA Netw Open. 2021;4:e218828–218828. Zhu D, Ozaki A, Virani SS. Disease-specific excess mortality during the COVID-19 pandemic: an analysis of weekly US death data for 2020. Am J Public Health. 2021;111:1518–22. Gobiņa I, Avotinš A, Kojalo U, Strele I, Pildava S, Villeruša A, et al. Excess mortality associated with the COVID-19 pandemic in Latvia: a population-level analysis of all-cause and noncommunicable disease deaths in 2020. BMC Public Health. 2022;22:1–12. Jayaraj VJ, Chong DW-Q, Wan K-S, Hairi NN, Bhoo-Pathy N, Rampal S, et al. Estimating excess mortalities due to the COVID-19 pandemic in Malaysia between January 2020 and September 2021. Sci Rep. 2023;13:86. Zhang J, Jin Y, Jia P, Li N, Zheng Z-J. Global gender disparities in premature death from Cardiovascular Disease, and their associations with Country Capacity for Noncommunicable Disease Prevention and Control. Int J Environ Res Public Health. 2021;18. https://doi.org/10.3390/ijerph181910389 Connelly PJ, Azizi Z, Alipour P, Delles C, Pilote L, Raparelli V. The importance of gender to understand sex differences in cardiovascular disease. Can J Cardiol. 2021;37:699–710. Humphries KH, Izadnegahdar M, Sedlak T, Saw J, Johnston N, Schenck-Gustafsson K, et al. Sex differences in cardiovascular disease–impact on care and outcomes. Front Neuroendocrinol. 2017;46:46–70. Kontis V, Mathers CD, Bonita R, Stevens GA, Rehm J, Shield KD, et al. Regional contributions of six preventable risk factors to achieving the 25$\times$ 25 non-communicable disease mortality reduction target: a modelling study. Lancet Glob Health. 2015;3:e746–57. Download references AcknowledgementsWe thank the Department of Statistics Malaysia (DOSM) for providing the mortality data with ICD-10 codes for cause of death and population structure. No funding was obtained for this study. Author informationAuthors and affiliations. Department of Community Medicine, School of Medical Sciences, Universiti Sains Malaysia, Kubang Kerian, Kelantan, 16150, Malaysia Wan Shakira Rodzlan Hasani & Kamarul Imran Musa Biostatistics and Research Methodology Unit, School of Medical Sciences, Universiti Sains Malaysia, Kubang Kerian, Kelantan, 16150, Malaysia Kueh Yee Cheng School of Mathematical and Computer Sciences, Heriot-Watt University Malaysia, Putrajaya, 62200, Malaysia Sarat Chandra Dass You can also search for this author in PubMed Google Scholar ContributionsConceptualization: Wan Shakira Rodzlan Hasani, Kamarul Imran Musa, Kueh Yee Cheng, Sarat Chandra Dass. Data curation: Wan Shakira Rodzlan Hasani, Kamarul Imran Musa. Formal analysis: Wan Shakira Rodzlan Hasani. Investigation: Wan Shakira Rodzlan Hasani, Kamarul Imran Musa, Kueh Yee Cheng. Methodology: Wan Shakira Rodzlan Hasani, Kamarul Imran Musa, Sarat Chandra Dass. Project administration: Wan Shakira Rodzlan Hasani. Resources: Wan Shakira Rodzlan Hasani, Kamarul Imran Musa. Software: Wan Shakira Rodzlan Hasani. Writing – original draft: Wan Shakira Rodzlan Hasani. Writing – review & editing: Wan Shakira Rodzlan Hasani, Kamarul Imran Musa, Kueh Yee Cheng, Sarat Chandra Dass. All authors read the manuscript and approved the submission. Corresponding authorCorrespondence to Kamarul Imran Musa . Ethics declarationsEthics approval and consent to participate. The study was conducted in accordance with the Declaration of Helsinki and ethical approval was obtained from the Medical Research and Ethics Committee (MREC), Ministry of Health Malaysia and the Human Research Ethics Committee of USM (USM/JEPeM/22,030,181). Mortality data was obtained with approval from the Department of Statistics Malaysia (DOSM). All data was anonymized prior to use in this study. Due to the using of DOSM database (vital registration data), the requirement for informed consent was waived. Consent for publicationNot applicable. Competing interestsAll authors declare that they have no conflicts of interest. Additional informationPublisher’s note. Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Rights and permissionsOpen Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data. Reprints and permissions About this articleCite this article. Hasani, W.S.R., Musa, K.I., Cheng, K.Y. et al. Exploring the trend of age-standardized mortality rates from cardiovascular disease in Malaysia: a joinpoint analysis (2010–2021). BMC Public Health 24 , 2519 (2024). https://doi.org/10.1186/s12889-024-19103-7 Download citation Received : 11 July 2023 Accepted : 11 June 2024 Published : 16 September 2024 DOI : https://doi.org/10.1186/s12889-024-19103-7 Share this articleAnyone you share the following link with will be able to read this content: Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative
BMC Public HealthISSN: 1471-2458
Experience in Using an Echo Meter Touch Ultrasonic Module in Studies of the Species Composition, Occurrence, and Biotopic Preferences of Bats (Chiroptera, Vespertilionidae) in Voronezh Oblast
Cite this article
134 Accesses Explore all metrics The results of surveying echolocation signals of bats, performed using an Echo Meter Touch 2 PRO ultrasonic detector, are given. The signals were recorded in the time–expansion mode and identified manually in the BatSound program. The surveys were made in June–August 2019–2020 in the northwestern part of Voronezh oblast within the Federal Voronezh State Nature Reserve. Four types of biotopes were used as model territories to identify the species composition, occurrence, and biotopic confinement: a river bank, a forest lake, the expanse of a former burnt area, and a village. A total of 2332 audio recordings of ultrasonic signals were made. After manual verification, 1615 records (69.3%) belonging to 13 bat species were identified with a high probability (located in descending order according to the number of occurrences): N. noctula > N. leisleri > P. pygmaeus > V. murinus > P. nathusii > M. dasycneme > M. daubentonii > N. lasiopterus > P. auritus > P. pipistrellus > M. brandtii > E. nilssonii . The habitat of E. nilssonii was established for the first time in the territory studied. Biotopically, near-water areas, where the greatest diversity was noted, were the most attractive for bats. However, the distribution of species here was not the same. M. brandtii , P. pygmaeus , E. nilssonii , and M. dasycneme preferred river biotopes predominantly and were almost absent above the forest lake or were indifferent to this space. M. daubentonii , V. murinus , P. nathusii , and E. serotinus gave the greatest preference to the lake territory. Burnt areas were unattractive to most species, except for N. noctula and E. serotinus . An indifferent attitude to the territory of the village or its avoidance was noted for all species. Alpha diversity increased in the following series of biotopes: burnt area–village–river bank–forest lake, over which the largest number of species was noted with greater evenness according to the index of relative occurrence. The detected differences in biotopic confinement are discussed in connection with the spatial location of biotopes. This is a preview of subscription content, log in via an institution to check access. Access this articleSubscribe and save.
Price includes VAT (Russian Federation) Instant access to the full article PDF. Rent this article via DeepDyve Institutional subscriptions  Similar content being viewed by others Description of the echolocation pulses of insectivorous bats with new records for Southwest Colombia Acoustic identification of five insectivorous bats by their echolocation calls in the Sahelian zone of Far North Cameroon Author informationAuthors and affiliations. Penza State University, 440026, Penza, Russia D. G. Smirnov Voronezh State University, 394018, Voronezh, Russia A. S. Klimov, A. D. Numerov & E. I. Trufanova You can also search for this author in PubMed Google Scholar Corresponding authorCorrespondence to D. G. Smirnov . Ethics declarationsThe authors declare that they have no conflicts of interest. This article does not contain any studies involving animals performed by any of the authors. Additional informationTranslated by A. Barkhash Rights and permissionsReprints and permissions About this articleSmirnov, D.G., Klimov, A.S., Numerov, A.D. et al. Experience in Using an Echo Meter Touch Ultrasonic Module in Studies of the Species Composition, Occurrence, and Biotopic Preferences of Bats (Chiroptera, Vespertilionidae) in Voronezh Oblast. Biol Bull Russ Acad Sci 50 , 1511–1524 (2023). https://doi.org/10.1134/S1062359023070245 Download citation Received : 20 August 2021 Revised : 22 March 2022 Accepted : 23 March 2022 Published : 23 November 2023 Issue Date : December 2023 DOI : https://doi.org/10.1134/S1062359023070245 Share this articleAnyone you share the following link with will be able to read this content: Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative
Voronezh State Medical University Russia 2024-25: Admission, Courses, Fees, Eligibility, Ranking etc. Voronezh State Medical University (VSMU), founded in 1930, is a prestigious institution in Voronezh, Russia, offering programs in medicine, dentistry, and pharmacy. The university combines theoretical knowledge with practical skills and features modern facilities, including advanced labs, a large library, and well-equipped lecture halls. With a focus on international collaboration, VSMU attracts students from around the world and offers exchange programs, creating a multicultural learning environment. Located in Voronezh, a city rich in history and culture, VSMU provides a balanced academic and cultural experience. The university is renowned for its excellence in medical education and its contributions to healthcare advancements both in Russia and globally.
In this article, we cover all the important details about Voronezh State Medical University. You will find information on the admission process, courses offered, fee structure, and eligibility criteria. We also discuss the pros and cons of studying MBBS in Russia, as well as the university’s ranking and other relevant details. [Page Index]College summary. Before we go through Voronezh State Medical University detailed information, let’s look at the College’s essential details. Wants to Study MBBS Abroad from a top Country with low tution Fees? Subscribe Now!
Affiliation and RecognitionThese are the renowned bodies who’ve given recognition to the Voronezh State Medical University.
Below is the list of faculties that Voronezh State Medical University Russia has to offer:
Courses OfferedVoronezh State Medical University offers quality medical programs under highly qualified faculty and state-of-the-art infrastructure. The College is famous for its undergraduate medical programs (MBBS). 
Why Study MBBS at Voronezh State Medical University?
Admission ProcedureIf you want to take Voronezh State Medical University Admission, you must qualify for the National Eligibility Entrance Exam (NEET) for Indian students. To get admission to Voronezh State Medical University, one should follow these steps:
Eligibility CriteriaIf you want to study MBBS at Voronezh State Medical University, check out the eligibility criteria of this university mentioned below:
Graphical Representation of Eligibility Criteria 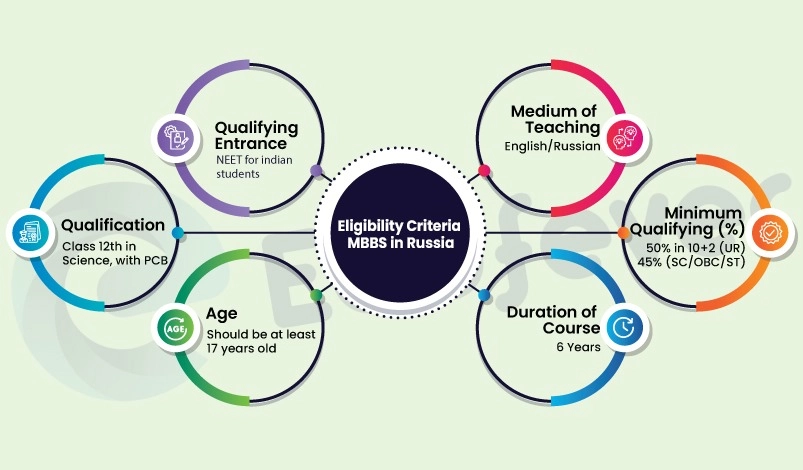 Documents RequiredBefore taking admission at Voronezh State Medical University, please do not forget to carry all these related documents.
Fee Structure 2024-25This section shows Voronezh State Medical University MBBS fees are given below:-
Cost of Living at VoronezhThe cost of living at Voronezh city is as follows:
Ranking 2024-25According to Unirank, the Voronezh State Medical University ranking in Russia and all over the world:
Advantages of MBBS in Russia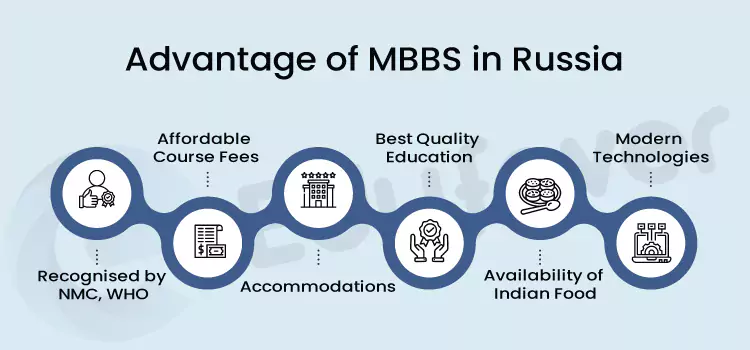 About Voronezh City
Temperature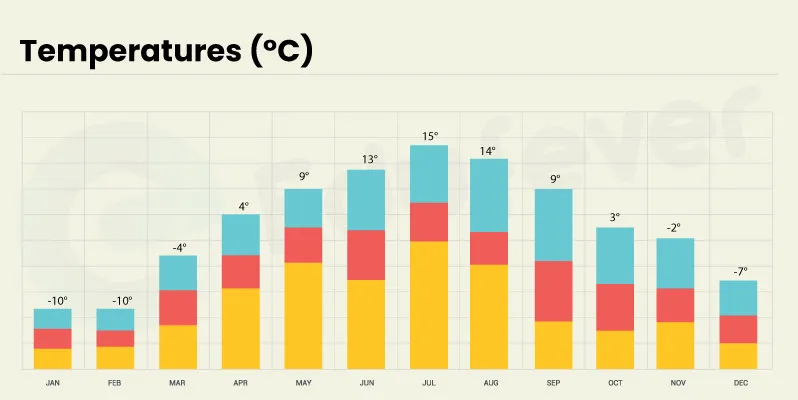 Contact DetailsVoronezh State Medical University Address: Universitetskaya Ploshchad’, 1, Voronezh, Oblast, Russia, 394036 Voronezh State Medical University Photos Frequently Asked Question(FAQs)Does this university implement modern teaching methods. Voronezh University implements modern teaching methods such as problem-based teaching, video-based classes, computer and Internet classes, and education software. Where is Voronezh State Medical University located?The address of Voronezh State Medical University is Universitetskaya Ploshchad’, 1, Voronezh, Voronezh, Oblast, Russia, 394036. What is the annual tuition fee for Indian students at Voronezh State Medical University?The annual tuition fee for Indian students at Voronezh State Medical University is $5750 (Rs.4.77 Lakhs) including hostel fees. What is the current world ranking of Voronezh State Medical University?The world ranking of Voronezh State Medical University is 4975.
You may like to read
About Manish VermaHello, I'm Manish Verma, with a year of expertise in MBBS and Ayush courses. I have detailed knowledge of various colleges' fee structures, cutoffs, and intake procedures. If you're looking for insights or assistance in pursuing MBBS or BAMS courses, feel free to comment below—I'm here to help! Leave a Comment Cancel replyNotify me via e-mail if anyone answers my comment. Abroad MBBS Update 2024 : Admission Dates, Top College, Fees, Location, Scholarship etc. Get admission to Top Overseas Universities with Affordable Fees.
The economic burden of prostate cancer in Iran: a cross-sectional cost-of-illness study
BMC Research Notes volume 17 , Article number: 268 ( 2024 ) Cite this article Metrics details This study aims to assess the economic burden of prostate cancer in Iran by analyzing direct medical costs, direct non-medical costs, and indirect costs. We conducted a cross-sectional cost-of-illness study in Khorramabad, located in western Iran, during 2023, using a prevalence-based, bottom-up approach. Data were collected from 285 prostate cancer patients using questionnaires, interviews, and patient records. Our study estimated the economic burden of prostate cancer at $744,990. Direct medical costs accounted for 63.50% of this, totaling $153,330, with therapy being the largest component. Direct non-medical costs were $62,130, and indirect costs from productivity losses were $209,760. The calculated overall cost per patient was $2,614.88. Extrapolating from the 2021 Global Burden of Disease data, which reported approximately 83,000 prostate cancer patients in Iran, the national economic burden is estimated at $217,034,040. This substantial burden highlights the need for improved insurance coverage and early detection. The findings suggest that policymakers and healthcare providers in Iran should develop standardized cost analysis methods and enhance financial protection to alleviate economic strain and improve healthcare outcomes and sustainability. Peer Review reports IntroductionProstate cancer ranks as the second most prevalent cancer among men worldwide, with approximately 1.4 million new cases diagnosed in 2020. This disease significantly contributes to the overall cancer burden in men [ 1 , 2 ]. The incidence of prostate cancer has exhibited a concerning upward trend, particularly in high-income regions such as Europe and North America. This increase can be attributed to factors such as population aging and the widespread adoption of prostate-specific antigen (PSA) screening [ 3 ]. However, mortality rates associated with prostate cancer follow a more intricate pattern. While high-income countries have witnessed a decline in mortality rates, low- and middle-income countries (LMICs) continue to grapple with higher mortality rates due to limited access to early diagnostic and treatment services [ 4 , 5 ]. In Iran, prostate cancer stands as the third most common cancer among men, with an estimated 8,937 new cases reported in 2020 [ 6 ]. Projections indicate that the prevalence of prostate cancer in Iran will escalate significantly by 2040, posing substantial challenges to the healthcare system [ 6 ]. This rise can be attributed to demographic shifts, including population aging, urbanization, and changes in lifestyle and dietary patterns. Consequently, there is an urgent need to comprehensively understand the economic impact of prostate cancer on the Iranian healthcare system [ 7 ]. The economic burden of prostate cancer encompasses both direct costs (such as diagnosis, treatment, and follow-up care) and indirect costs (including lost productivity and income) [ 8 ]. Studies conducted across various regions consistently highlight the substantial financial strain that prostate cancer imposes on healthcare systems and patients alike [ 9 ]. For instance, in the United States, the annual costs associated with managing prostate cancer were estimated at $11.85 billion in 2010, making it one of the costliest cancers to treat. Similarly, in Europe, annual healthcare costs related to prostate cancer reach €8.5 billion [ 10 ]. This study aims to fill the gap in understanding the economic burden of prostate cancer in Iran, driven by unique socio-economic and healthcare challenges. The mixed public-private healthcare system in Iran exhibits significant disparities in access to care, with high out-of-pocket expenses exacerbating the financial strain on families [ 9 ]. Rapid urbanization and lifestyle changes have led to an increased incidence of non-communicable diseases, including cancer. By analyzing direct medical costs, indirect costs, and the broader societal impact, this research provides essential insights for policymakers and healthcare providers to develop effective strategies for managing prostate cancer and mitigating its financial repercussions. Study Design and Data CollectionWe conducted a cross-sectional cost-of-illness study to assess the economic burden of prostate cancer in Khorramabad, western Iran, in 2023. Utilizing a prevalence-based, bottom-up approach from a societal perspective, we included all prostate cancer patients who visited or were hospitalized at Rahimi Hospital during the year [ 11 ]. Out of 338 identified patients, 53 were excluded due to lack of access, inaccurate diagnostic data, and mortality, leaving 285 patients for the final analysis. The study was approved by the relevant ethics committee, and informed consent was obtained from all participants. A subset of patients could not be reached or contacted despite repeated attempts, resulting in incomplete data collection. Some patients had incomplete or inaccurate diagnostic records, affecting the reliability of cost estimates. Additionally, some patients had passed away before data collection could be completed, necessitating their exclusion. This introduces potential bias, as the remaining cohort may not fully represent the broader population of prostate cancer patients in Khorramabad. The exclusion of these patients could impact the generalizability of the cost estimates. Future research with more comprehensive data collection and a larger sample size is recommended to mitigate these biases and provide a more accurate assessment of the economic burden of prostate cancer. Cost estimation approachData were collected through questionnaires, interviews, and a review of patient documents to estimate costs, categorized into three domains: direct medical costs (DMC), direct non-medical costs (DNMC), and indirect costs. Direct Medical Costs (DMC): These included diagnostic services, laboratory and pathology tests, inpatient and outpatient care, rehabilitation, medical devices, physician visits, therapies, and consultations. Costs were based on tariffs from the Ministry of Health and Medical Education (MOHME) and gathered retrospectively via patient and specialist interviews, and examination of healthcare records and financial documents. Each cost was calculated individually, considering both patient files and specialist input. Direct Non-Medical Costs (DNMC): These encompassed transportation, accommodation, and food costs. Estimates were derived from interviews with patients and their families. Indirect Costs: These were based on productivity losses from absenteeism and presenteeism, calculated using monthly income data from questionnaires and direct inquiries. This included work and daily activity absences by patients and their caregivers, with costs estimated using average salary data for 2023 from Iranian Statistics. This approach ensured comprehensive cost analysis by integrating multiple data sources and cost categories. In this study, all reported costs are annual and specific to a cohort of 285 prostate cancer patients from Rahimi Hospital in Khorramabad for the year 2023. These costs do not represent lifetime costs or the total economic burden for Iran but reflect the financial impact on this specific group. The findings are not immediately applicable to a broader national context, and future research should include multiple centers and regions for a comprehensive national estimate. Extrapolation to national costs should be done cautiously, and additional analyses are recommended. The study employed a one-way sensitivity analysis, varying the prevalence rate of prostate cancer in Iran to calculate the disease population and economic burden, assuming constant cost components per patient. To facilitate international comparisons, all costs were converted into US dollars using the exchange rate of 420,000 Iranian Rials per US dollar in 2023. The collected data underwent rigorous analysis using R software version 4.3.2. The mean age of the patients was 71.53 years, with a standard deviation of 16.18 years. Demographic characteristics are detailed in Table 1 . The highest percentage of patients fell within the 60 to 69 age group, comprising 39.64%, followed by the 70 to 79 age group at 29.82%. Among the patients, 67.36% were employed, while 18.24% were unemployed. Additionally, 88.07% of the patients were married. Regarding insurance status, 3.88% of patients had no insurance, and 4.57% had a family history of prostate cancer. The calculated costs are categorized as follows (see Table 2 A): The direct medical cost amounts to $473,100, with the bulk of this being attributed to therapy costs. The direct non-medical cost is $62,130, largely driven by accommodation costs. The indirect costs reach $209,760, primarily due to patients being absent from work and their usual daily activities. The calculated overall cost per patient was $2,614.88. Figure 1 represents the total costs across all three categories. The economic burden of prostate cancer in this study amounted to $744,990. Direct medical costs accounted for 63.50% of the total costs, indirect costs for 8.33%, and non-medical costs for 28.17%. Based on the disease stage, the economic burden was calculated as follows: $138,377 for patients in stage 1, $189,623 for patients in stage 2, $314,194 for patients in stage 3, and $102,796 for patients in stage 4. The detailed table breaking down costs by cancer stage is provided in Table 2 B. Based on the number of patients in each stage, the total cost per patient was calculated as follows: $4,463.77 for stage 1, $1,841 for stage 2, $2,513.55 for stage 3, and $3,953.65 for stage 4.  Costs of prostate cancer by category. The plot shows that direct medical costs constitute 63.50% of the total costs, non-medical costs make up 28.17%, and indirect costs account for 8.33% Based on the sensitivity analysis, the range of costs is as follows: direct medical costs are between $425,790 and $520,410; direct non-medical costs range from $55,917 to $68,343; indirect costs vary from $188,784 to $230,736; and total costs are calculated to be between $670,491 and $819,489. Detailed costs for sensitivity analysis are provided in supplementary file 1. To estimate the national economic burden of prostate cancer in Iran, we extrapolated our data using prevalence statistics from the 2021 Global Burden of Disease (GBD) ( https://vizhub.healthdata.org/gbd-results/ ), which reported approximately 83,000 prostate cancer patients in the country. With a calculated cost per patient of $2,614.88, the estimated total economic burden for prostate cancer in Iran amounts to $217,034,040. The aggregate direct medical costs in our investigation amounted to $473,100, predominantly influenced by the costs of therapy. Similar studies in other in other countries and studies conducted in Iran, direct medical costs had the largest share of the economic burden of prostate cancer [ 6 , 7 , 9 ]. This discrepancy can be ascribed to variations in methodologies, treatment patterns, and cost conversion practices. Our study discovered that indirect costs, primarily due to patients’ absence from work, totaled $209,760, representing 28.17% of the total costs. This is in line with the findings from the US study by Gustavsen et al., where productivity losses were a significant component of the economic burden, although they observed that high-risk patients incurred greater costs over time due to disease progression [ 11 ]. Although patients with metastatic disease incur significant medical costs, the higher number of patients with localized disease (approximately 91% compared to those with metastatic disease) results in a greater overall share of costs for patients with localized disease. This finding is consistent with studies conducted in Iran and other countries [ 6 , 7 , 12 , 13 ]. Given that many of the services received at different stages, such as radiotherapy, hormone therapy, and chemotherapy, are expensive; this can explain why these patients incur the highest costs. This finding is consistent with studies conducted in other countries [ 13 , 14 , 15 , 16 ]. More severe stages of the disease can be very expensive for patients. Due to the higher costs and financial pressure on families, patients often reported having to use their savings, rely on family members, or borrow money to pay for their medical expenses [ 7 , 17 ]. The substantial costs associated with prostate cancer, particularly in terms of direct medical expenses, highlight the necessity for financial support for patients. The findings from Eswatini by Ngcamphalala et al., [ 18 ] indicate that advanced cancer stages significantly augment healthcare costs, a trend also observed in our study. This suggests that early detection and treatment are pivotal in managing overall costs and enhancing patient outcomes. This study highlights significant variation in stage-specific costs of prostate cancer treatment, with the highest cost per patient in stage 1 at $4,463.77 and the lowest in stage 2 at $1,841. These differences emphasize the importance of early detection and tailored treatment strategies [ 16 ]. The higher cost in stage 1 likely reflects intensive initial treatments, while stage 2’s lower cost suggests a more stable management period [ 10 ]. The estimated national economic burden of prostate cancer in Iran is approximately $217 million, underlining the need for effective public health initiatives. However, this estimate should be interpreted cautiously due to potential generalizability issues, as regional data may not fully represent the entire country. Our study provides a comprehensive analysis of the economic burden of prostate cancer in Iran, highlighting critical areas for policy intervention and patient support. By refining cost classification methodologies, enhancing the generalizability of our findings, and ensuring clear and detailed reporting, our research aims to offer more reliable insights into the financial challenges faced by patients and the healthcare system. Addressing gaps in insurance coverage, emphasizing early detection and treatment, and improving healthcare infrastructure are essential strategies to alleviate the economic impact of prostate cancer on individuals and society. These findings can inform policymakers and healthcare providers in making evidence-based decisions to improve patient outcomes and financial protection. LimitationsOur study exhibits several limitations that warrant consideration. These include the potential for misreporting of costs and income, as well as the restricted generalizability of our findings due to the metropolitan focus of our patient cohort. Similar to the observations made by Alinezhad et al., [ 6 ] the bottom-up approach employed in our study, while valuable for obtaining direct patient information, may inadvertently lead to a higher likelihood of missing values. To address these limitations, future research endeavors should strive to incorporate a more diverse patient population and explore the utilization of top-down approaches to gather more comprehensive data. Since the data were collected from a single center, Rahimi Hospital, in one city, the results may not be representative of the entire country. The socioeconomic, demographic, and healthcare infrastructure variations across different regions of Iran could influence the economic burden of prostate cancer in ways that our study does not capture. To enhance the generalizability of future research, it is recommended that similar studies be conducted in multiple centers across diverse regions of Iran. This would provide a more comprehensive understanding of the economic burden of prostate cancer nationwide. Despite these limitations, we believe our study contributes valuable preliminary data that can serve as a foundation for broader analyses. Reporting the estimated economic burden for Iran as a whole, even with the acknowledged limitations, can still be beneficial for a wider audience, providing a useful starting point for policymakers and healthcare planners. while the national burden estimate offers valuable context, it should be interpreted with caution. The extrapolation is based on regional data that may not fully represent the entire Iranian population. Therefore, the estimated national burden might not be entirely accurate due to potential generalizability issues. Data availabilityNo datasets were generated or analysed during the current study. AbbreviationsLow- and middle-income countries Direct Medical Costs Ministry of Health and Medical Education Direct Non-Medical Costs Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A. Global Cancer statistics 2020: GLOBOCAN estimates of incidence and Mortality Worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49. Article PubMed Google Scholar Wang L, Lu B, He M, Wang Y, Wang Z, Du L. Prostate Cancer incidence and mortality: global status and temporal trends in 89 countries from 2000 to 2019. Front Public Health. 2022;10:811044. Article PubMed PubMed Central Google Scholar Teoh JYC, Hirai HW, Ho JMW, Chan FCH, Tsoi KKF, Ng CF. Global incidence of prostate cancer in developing and developed countries with changing age structures. PLoS ONE. 2019;14(10):e0221775. Article CAS PubMed PubMed Central Google Scholar Zhou CK, Check DP, Lortet-Tieulent J, Laversanne M, Jemal A, Ferlay J, et al. Prostate cancer incidence in 43 populations worldwide: an analysis of time trends overall and by age group. Int J Cancer. 2016;138(6):1388–400. Article CAS PubMed Google Scholar Culp MB, Soerjomataram I, Efstathiou JA, Bray F, Jemal A. Recent global patterns in prostate Cancer incidence and mortality rates. Eur Urol. 2020;77(1):38–52. Alinezhad F, Khalili F, Zare H, Lu C, Mahmoudi Z, Yousefi M. Financial burden of prostate cancer in the Iranian population: a cost of illness and financial risk protection analysis. Cost Eff Resour Alloc. 2023;21(1):84. Mojahedian MM, Toroski M, Keshavarz K, Aghili M, Zeyghami S, Nikfar S. Estimating the cost of illness of prostate Cancer in Iran. Clin Ther. 2019;41(1):50–8. Rasouli MA, Moradi G, Zareie B, Sofimajidpour H, Tozandehjani S, Zafari H, et al. Overall survival and prognostic factors prostate cancer in Kurdistan Province-Iran: a population-based study (2011–2018). BMC Cancer. 2021;21(1):1314. Farabi H, Moradi N, Ahmadzadeh A, Aghamir SMK, Mohammadi A, Rezapour A. A cost-benefit analysis of mass prostate cancer screening. Cost Eff Resour Alloc. 2024;22(1):37. Cantarero-Prieto D, Lera J, Lanza-Leon P, Barreda-Gutierrez M, Guillem-Porta V, Castelo-Branco L, et al. The Economic Burden of localized prostate Cancer and insights derived from cost-effectiveness studies of the different treatments. Cancers (Basel). 2022;14(17):4088. Gustavsen G, Gullet L, Cole D, Lewine N, Bishoff JT. Economic burden of illness associated with localized prostate cancer in the United States. Future Oncol. 2020;16(1):4265–77. Ong SC, Lim SG, Li SC. How big is the financial burden of hepatitis B to society? A cost-of-illness study of hepatitis B infection in Singapore. J Viral Hepat. 2009;16(1):53–63. Yong C, Onukwugha E, Mullins CD. Clinical and economic burden of bone metastasis and skeletal-related events in prostate cancer. Curr Opin Oncol. 2014;26(3):274–83. Hanly P, Timmons A, Walsh PM, Sharp L. Breast and prostate cancer productivity costs: a comparison of the human capital approach and the friction cost approach. Value Health. 2012;15(3):429–36. Molinier L, Bauvin E, Combescure C, Castelli C, Rebillard X, Soulié M, et al. Methodological considerations in cost of prostate cancer studies: a systematic review. Value Health. 2008;11(5):878–85. Fourcade RO, Benedict A, Black LK, Stokes ME, Alcaraz A, Castro R. Treatment costs of prostate cancer in the first year after diagnosis: a short-term cost of illness study for France, Germany, Italy, Spain and the UK. BJU Int. 2010;105(1):49–56. Stokes ME, Black L, Benedict A, Roehrborn CG, Albertsen P. Long-term medical-care costs related to prostate cancer: estimates from linked SEER-Medicare data. Prostate Cancer Prostatic Dis. 2010;13(3):278–84. Ngcamphalala C, Östensson E, Ginindza TG. The economic burden of prostate cancer in Eswatini. BMC Health Serv Res. 2022;22(1):483. Download references AcknowledgementsNot applicable. Author informationAuthors and affiliations. Health Management and Economics Research Center, School of Health Management and Information Sciences, Iran University of Medical Sciences, Tehran, Iran Banafshe Darvishi Teli & Aziz Rezapour Social Determinants of Health Research Center, Lorestan University of Medical Sciences, Khorramabad, Iran Meysam Behzadifar & Masoud Behzadifar Hospital Management Research Center, Health Management Research Institute, Iran University of Medical Sciences, Tehran, Iran Samad Azari English Language Department, School of Health Management and Information Sciences, Iran University of Medical Sciences, Tehran, Iran Seyed Jafar Ehsanzadeh You can also search for this author in PubMed Google Scholar ContributionsConceptualization: BDT, MaB, AR. Data curation: MeB, BDT, SA, And SJE. Formal analysis: MaB, AR, SA. Investigation: BDT, SJE, Methodology: MaB, BDT, Project administration: MeB, AR, SA. Supervision: MaB, AR. Validation: BDT, MaB. Writing – original draft: MaB, SA, BDT. Writing – review & editing: SJE, MaB, AR, BDT. The author(s) read and approved the final manuscript. Corresponding authorCorrespondence to Masoud Behzadifar . Ethics declarationsEthics approval and consent to participate. The study was approved by Ethics Committee of the Iran University of Medical Sciences (IR.IUMS.REC.1402.698). All participants provided written informed consent to participate in this study. Consent for publicationCompeting interests. The authors declare no competing interests. Additional informationPublisher’s note. Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Electronic supplementary materialBelow is the link to the electronic supplementary material. Supplementary Material 1: file 1. The sensitivity analysis.Rights and permissions. Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ . Reprints and permissions About this articleCite this article. Darvishi Teli, B., Rezapour, A., Behzadifar, M. et al. The economic burden of prostate cancer in Iran: a cross-sectional cost-of-illness study. BMC Res Notes 17 , 268 (2024). https://doi.org/10.1186/s13104-024-06913-6 Download citation Received : 26 May 2024 Accepted : 23 August 2024 Published : 17 September 2024 DOI : https://doi.org/10.1186/s13104-024-06913-6 Share this articleAnyone you share the following link with will be able to read this content: Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative
BMC Research NotesISSN: 1756-0500
10 Day Weather - Voronezh, RUS
Response is increased using postal rather than electronic questionnaires – new results from an updated Cochrane Systematic Review
BMC Medical Research Methodology volume 24 , Article number: 209 ( 2024 ) Cite this article 3 Altmetric Metrics details A decade ago paper questionnaires were more common in epidemiology than those administered online, but increasing Internet access may have changed this. Researchers planning to use a self-administered questionnaire should know whether response rates to questionnaires administered electronically differ to those of questionnaires administered by post. We analysed trials included in a recently updated Cochrane Review to answer this question. We exported data of randomised controlled trials included in three comparisons in the Cochrane Review that had evaluated hypotheses relevant to our research objective and imported them into Stata for a series of meta-analyses not conducted in the Cochrane review. We pooled odds ratios for response using random effects meta-analyses. We explored causes of heterogeneity among study results using subgroups. We assessed evidence for reporting bias using Harbord’s modified test for small-study effects. Twenty-seven trials (66,118 participants) evaluated the effect on response of an electronic questionnaire compared with postal. Results were heterogeneous (I-squared = 98%). There was evidence for biased (greater) effect estimates in studies at high risk of bias; A synthesis of studies at low risk of bias indicates that response was increased (OR = 1.43; 95% CI 1.08–1.89) using postal questionnaires. Ten trials (39,523 participants) evaluated the effect of providing a choice of mode (postal or electronic) compared to an electronic questionnaire only. Response was increased with a choice of mode (OR = 1.63; 95% CI 1.18–2.26). Eight trials (20,909 participants) evaluated the effect of a choice of mode (electronic or postal) compared to a postal questionnaire only. There was no evidence for an effect on response of a choice of mode compared with postal only (OR = 0.94; 95% CI 0.86–1.02). ConclusionsPostal questionnaires should be used in preference to, or offered in addition to, electronic modes. Peer Review reports IntroductionWhen collecting information from large, geographically dispersed populations, a self-administered questionnaire is usually the only financially viable option [ 1 ]. Non-responses to questionnaires reduce effective sample sizes, reducing study power, and may introduce bias in study results [ 2 ]. The Cochrane Methodology Review of methods to increase response to self-administered questionnaires has provided a much-used scientific evidence base for effective data collection by questionnaire since the publication of the first version of the review in 2003 which focused on postal questionnaires [ 3 ]. A decade ago paper-and-pencil administration of questionnaires in epidemiological studies was twenty times more common than electronic administration [ 4 ], but increased Internet access and decreasing volumes of mailed letters suggests that electronic administration has gained favour [ 5 , 6 , 7 ]. Researchers planning to collect data from participants using a self-administered questionnaire need to know how will the proportion of participants responding to a questionnaire administered electronically compare with one administered by post? We conducted further analyses of the trials included in the recently updated Cochrane Review [ 8 ] to answer this question. To assess whether response rates to questionnaires administered electronically differ to those of questionnaires administered by post. Data sources/measurementWe exported data of randomised controlled trials included in the updated Cochrane Review [ 8 ] from RevMan and imported them into Stata for a series of meta-analyses not conducted in the Cochrane review. ComparisonsWe focused on data from trials included in three comparisons in the Cochrane Review that had evaluated hypotheses relevant to our research objective: Postal vs. electronic questionnaire (Cochrane Comparison 81). Electronic questionnaire only vs. choice (postal or electronic) (Cochrane Comparison 84). Choice (electronic or postal) vs. postal questionnaire only (Cochrane Comparison 82). These comparisons assess: response to questionnaires administered by post compared with questionnaires administered electronically, response to a questionnaire administered electronically compared with response when including a postal response option, and response when including an electronic response option compared with response to a questionnaire administered by post only, respectively. Outcome measuresThe data obtained from each trial included the numbers of participants randomised to each arm of the trial with the numbers of completed, or partially completed questionnaires returned after all mailings (for trials including a postal questionnaire), and the numbers of participants randomised to each arm of the trial with the numbers of participants submitting the completed, or partially completed online questionnaires after all contacts (electronic questionnaire). Other variablesAdditional data were also extracted on the: Year of publication of the study. Risk of bias in each included study (a judgment - high, low, or unclear); we assessed the overall risk of bias in each study using the Cochrane Collaboration’s tool [ 9 ]. Effect measures and synthesisFor each of the three comparisons (2.1.1 above), we pooled the odds ratios for response in each included study in a random effects meta-analysis (to allow for heterogeneity of effect estimates between studies) using the metan command in Stata [ 10 ]. This command also produced a forest plot (a visual display of the results of the individual studies and syntheses) for each comparison. We quantified any heterogeneity using the I 2 statistic that describes the percentage of the variability in effect estimates that is due to heterogeneity [ 11 ]. Subgroup analysesWe explored possible causes of heterogeneity among study results by conducting subgroup analyses according to two study-level factors: Year of study publication, and risk of bias in studies. We used a statistical test of homogeneity of the pooled effects in subgroups to assess evidence for subgroup differences. The statistical test of homogeneity used is Cochran’s Q test, where the Q statistic is distributed as a chi-square statistic with k-1 degrees of freedom, where k is the number of subgroups. If there was evidence for subgroup differences provided by the test of homogeneity, we chose the ‘best estimate of effect’ as the estimate from the subgroup of studies with low risk of bias, or the subgroup of studies published after 2012. If there was no evidence for subgroup differences, we chose our best estimate of effect based on the synthesis of all studies. Year of study publicationFrom 2012, household access to a computer exceeded 40%: [ 5 ] As the odds ratios for response to questionnaires administered electronically may be associated with household access to a computer, we analysed trial results in two subgroups – before 2012 and after 2012, where we used the year of publication as an approximation of the year of study conduct. Risk of biasThe odds ratios for response estimated in the included studies may be associated with trial quality. [ 12 , 13 ] For this reason we analysed trial results in two subgroups – trials judged to be at low and at high risk of bias. Reporting bias assessmentWe assessed evidence for reporting bias using Harbord’s modified test for small-study effects implemented in Stata using the metabias command [ 14 ]. This test maintains better control of the false-positive rate than the test proposed by Egger at al [ 14 ]. Study characteristicsThirty-five studies [ 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 ] reported 45 independent trials included in one or more of the three comparisons (Table 1 ). The studies were conducted in the US ( n = 20), Europe ( n = 13), and Australasia ( n = 2). The studies included between 133 and 12,734 participants and were published between 2001 and 2020. Eight studies were judged to be at high risk of bias [ 16 , 19 , 33 , 34 , 42 , 43 , 45 , 46 ]. Results of synthesesComparison 1 - postal vs. electronic questionnaire. Twenty-seven trials (66,118 participants) evaluated the effect on questionnaire response of postal administration compared with electronic. [ 15 , 16 , 17 , 18 , 19 , 20 , 23 , 24 , 25 , 26 , 27 , 28 , 31 , 32 , 33 , 34 , 35 , 36 , 38 , 39 , 40 , 41 , 43 , 44 , 46 , 47 , 48 ] The odds of response were increased by over half (OR 1.76; 95% CI 1.34 to 2.32) using a postal questionnaire when compared with an electronic one (Fig. 1 ). There was considerable heterogeneity between the trial results (I-squared = 98%), but most of the studies showed response was greater with postal questionnaires than with electronic questionnaires, and the high I-squared is due to differences in the size of the benefit for postal questionnaires, rather than being due to an even spread of results between those favouring postal and those favouring electronic questionnaires.  Effect on response of mode of administration Comparison 2 - electronic questionnaire only vs. choice (postal or electronic)Ten trials (39,523 participants) evaluated the effect on questionnaire response of providing a choice of response mode (postal or electronic) compared to an electronic questionnaire only [ 20 , 21 , 27 , 29 , 30 , 35 , 37 , 40 , 42 , 45 ]. The odds of response were increased by over half when providing a choice of response mode (OR 1.63; 95% CI 1.18 to 2.26; Fig. 2 ). There was considerable heterogeneity between the trial results (I-squared = 97.1%), but again, most of the studies favoured giving people the choice of response mode rather than electronic questionnaire only, and the high I-squared is due to differences in the size of the benefit for choice, rather than being due to an even spread of results between those favouring choice and those favouring electronic only.  Effect on response of choice of response mode compared with electronic only Comparison 3 - choice (electronic or postal) vs. postal onlyEight trials (20,909 participants) evaluated the effect of providing a choice of response mode (electronic or postal) compared to postal response only [ 20 , 22 , 27 , 29 , 34 , 35 , 40 , 49 ]. There was no evidence for an effect on response of providing a choice (OR 0.94; 95% CI 0.86 to 1.02; Fig. 3 ). There was moderate heterogeneity among the trial results (I-squared = 50.9%).  Effect on response of choice of response mode compared with postal only Results of subgroup analysesTable 2 presents the results of subgroup analyses according to the two study-level factors (forest plots of these subgroup analyses are included in supplementary figures). Comparison 1 - postal vs. electronic questionnaireYear of publication. A third of studies were published before 2012 [ 15 , 16 , 17 , 23 , 24 , 33 , 35 , 40 , 47 , 48 ]. In this subgroup of studies the odds of response were 85% greater (OR 1.85; 95% CI 1.12 to 3.06) with a postal questionnaire compared with an electronic one. In the subgroup of studies published after 2012 the effect was lower (OR 1.70; 1.19 to 2.43), consistent with our concern (Sect. 2.4.1 ) that higher household access to a computer from 2012 may have improved preference for electronic questionnaires, however the statistical test of homogeneity of the pooled effects in these two subgroups was not significant ( p = 0.788), indicating no evidence from these studies for different effects by year of study (Supplementary Fig. 1 a). Seven of the trials [ 16 , 17 , 26 , 33 , 34 , 43 , 46 ] were judged to be at high risk of bias and for these trials the odds of response were more than tripled (OR 3.24; 95% CI 1.68 to 6.25) using a postal questionnaire when compared with an electronic one. There was considerable heterogeneity between the trial results (I-squared = 99%). When only the 20 trials deemed to be at low risk of bias were synthesised, the odds of response were increased by two-fifths (OR 1.43; 95% CI 1.08 to 1.89). There was also considerable heterogeneity between these trial results (I-squared = 96.8%). The statistical test of homogeneity of the pooled effects in these two subgroups ( p = 0.025) provides some evidence for greater effect estimates in studies at high risk of bias (Supplementary Fig. 1 b). Our best estimate of the effect on response of mode of administration is hence from a synthesis of the studies at low risk of bias (OR 1.43; 95% CI 1.08 to 1.89). Results overall were thus confounded by risk of bias, but this did not explain the between study heterogeneity. Year of studyHalf of studies were published before 2012 [ 35 , 40 , 42 , 45 ]. In this subgroup of studies there was no evidence for an effect on response of providing a postal response option (OR 1.22; 95% CI 0.93 to 1.61). In the subgroup of studies published after 2012 there was evidence for an effect on response of providing a postal response option (OR 2.02; 95% CI 1.30 to 3.13). The statistical test of homogeneity of the pooled effects in these two subgroups was significant ( p = 0.057), indicating some evidence from these studies for different effects by year of study (Supplementary Fig. 2 a). This apparent preference for a postal response option in studies published after 2012 was counter to our concern (Sect. 2.4.1 ) that higher household access to a computer from 2012 would improve preference for electronic questionnaires. There was considerable heterogeneity between the trial results (I-squared = 98.2%), but most of the studies favoured giving people the choice of response mode rather than electronic questionnaire only, and the high I-squared is due to differences in the size of the benefit for choice, rather than being due to an even spread of results between those favouring choice and those favouring electronic only. Two of the trials were judged to be at high risk of bias [ 42 , 45 ]. There was no evidence for an effect on response of a postal option in these studies (OR 1.08; 95% CI 0.43 to 2.71). When only the 8 trials deemed to be at low risk of bias were synthesised, there was evidence that the odds of response were increased when providing a postal response option (OR 1.77; 95% CI 1.23 to 2.55). There was considerable heterogeneity between these trial results (I-squared = 97.7%). The statistical test of homogeneity of the pooled effects in these two subgroups ( p = 0.326) provides no evidence for different effects by risk of bias (Supplementary Fig. 2 b). Our best estimate of the effect on response of providing a postal response option is hence from a synthesis of all of these studies (OR 1.63; 95% CI 1.18 to 2.26). Comparison 3 - choice (electronic or postal) vs. postal questionnaire onlyIn the subgroup of studies published before 2012 there was very weak evidence that the odds of response were lower with an electronic option (OR 0.85; 0.73 to 0.98), whereas in studies published after 2012 there was no evidence for a difference between an electronic option and postal only – perhaps due to electronic methods being more acceptable with increased computer access. The results in both subgroups were more homogeneous (I-squared = 48.5% and 7.0% respectively). The statistical test of homogeneity of the pooled effects in these two subgroups ( p = 0.04) provides some evidence for different effects by year of study (Supplementary Fig. 3 a). If we consider the most recent trials to better represent the situation today (i.e., greater access to computers than prior to 2012), then our best estimate of the effect on response of providing an electronic response option is from a synthesis of the studies published after 2012 (OR 1.01; 95% CI 0.93 to 1.08), i.e., no evidence for an effect. There was one study at high risk of bias [ 34 ]. Its results were entirely consistent with the results of the seven studies at low risk of bias (the statistical test of homogeneity of the pooled effects in these two subgroups was not significant ( p = 0.454), Supplementary Fig. 3 b). Results of assessments of evidence for reporting biasThere was no evidence for small study effects (Harbord’s modified test p = 0.148). There was no evidence for small study effects (Harbord’s modified test p = 0.841). There was no evidence for small study effects (Harbord’s modified test p = 0.139). General interpretation of the results in the context of other evidenceThis study has shown that response to a postal questionnaire is more likely than response to an electronic questionnaire. It has also shown that response is more likely when providing the option for postal response with an electronic questionnaire. It has further shown that providing an electronic response option with a postal questionnaire has no effect on response. Response is thus increased using postal rather than electronic questionnaires. A previous meta-analysis of 43 mixed-mode surveys from 1996 to 2006 also found paper and postal administration produced greater response than electronic administration [ 50 ]. Our result that providing an electronic response option to postal administration does not increase response is consistent with a previous meta-analysis of randomised trials that found that mailed surveys that incorporate a concurrent Web option have significantly lower response rates than those that do not [ 51 ]. We suggest two possible reasons for these results: Paper questionnaires are more accessible than electronic questionnaires . Although access to the Internet increased over the period during which the studies included in this study were conducted [ 5 , 52 ], a ‘digital divide’ [ 53 ] persists in many populations where completion of a paper questionnaire may be possible, but completion of an electronic one may not. Paper questionnaires are more personal than electronic questionnaires . Personalised materials have been shown to increase response [ 54 ]. If participants perceive a paper questionnaire with a return envelope to be more ‘personal’ than a request to go to a website to answer some questions, we should expect a higher response with paper. Strengths and limitationsThe main strengths of this study are that our results are based on syntheses of the results of 45 randomised controlled trials that span two decades, and most of which were judged to be at low risk of bias. There was, however, considerable heterogeneity between the results of the included studies. Our subgroup analyses did not identify any causes of heterogeneity among study results, but they did reveal confounding of the pooled result for postal versus electronic questionnaires. The unexplained heterogeneity means that we cannot be confident about the magnitude of the effects on response using postal rather than electronic questionnaires. However, from inspection of the forest plots we can be confident about the direction of these effects. The evidence included in this review addresses ‘unit’ non-response only (i.e., return of questionnaires). ‘Item’ response (i.e., completion of individual questions) may be greater with electronic methods, but this was not addressed in this review and requires investigation in the future. We assessed evidence for reporting bias using Harbord’s modified test for small-study effects and found no evidence for bias. This test may not be reliable given the substantial heterogeneity between the results of the included trials [ 55 ]. Due to the nature of this study (secondary analysis of a published review), there is no pre-registered protocol for the subgroup analyses provided in this study. Implications for practice, policy, and future researchThese results will help researchers and healthcare providers to improve data collection from study participants and patients, helping to maintain study power and reduce bias due to missing data in research studies. In addition to the methods already known to be effective in increasing questionnaire response [ 8 , 56 ], postal questionnaires should be used in preference to, or offered in addition to, electronic modes as this will help to increase the proportion of participants that responds. It should be noted, however, that the evidence upon which this recommendation is based is from studies published between 2001 and 2020, and this may change in the future as access to the Internet increases and more people become ‘tech-savvy’. Furthermore, we consider that the certainty of the evidence provided in this study is “Moderate”, due to the unexplained heterogeneity between the results of the included studies. Future researchEvidence on effective data collection in low- and middle-income settings is needed. Research centres such as LSHTM can embed studies within trials (SWATs) in their research in these settings to help to increase the evidence base [ 57 ]. Participation rates for epidemiologic studies have been declining [ 58 ]. Our study has presented evidence that postal questionnaires are preferable to electronic questionnaires to improve participation, but it does not tell us why . Research is still needed to advance sociological and psychological theories of participation in data collection procedures [ 59 ]. Electronic administration provides benefits for researchers over paper administration which have not been addressed by this study: A well-designed Web questionnaire can control skip patterns, check for allowable values and ranges and response consistencies, and it can include instructions and explanations about why a question is being asked [ 60 ]. These options could help to improve the completeness and quality of self-administered data collection, maintaining study power, reducing the risk of bias in study results, and saving study resources. Further research into the cost-effectiveness of electronic administration compared with postal administration in different settings will be needed to inform practice [ 61 ]. Data availabilityData extracted from included studies will be available in the forthcoming update on the Cochrane Library. Armstrong BK, White E, Saracci R. Principles of exposure measurement in Epidemiology. New York: Oxford University Press; 1992. Book Google Scholar Greenland S. Response and follow-up bias in cohort studies. Am J Epidemiol. 1977;106:184–7. Article CAS PubMed Google Scholar Edwards PJ, Roberts IG, Clarke MJ, DiGuiseppi C, Wentz R, Kwan I, Cooper R, Felix L, Pratap S. Methods to increase response rates to postal questionnaires. Cochrane Database of systematic reviews 2007, issue 2. Art No : MR000008 https://doi.org/10.1002/14651858.MR000008.pub3 van Gelder MMHJ, Reini W, Bretveld RW, Nel Roeleveld N. Web-based questionnaires: the Future in Epidemiology? Am J Epidemiol. 2010;172:1292–8. Article PubMed Google Scholar Alsop T. Share of households with a computer at home worldwide from 2005 to 2019 https://www.statista.com/statistics/748551/worldwide-households-with-computer/ [Accessed 4 May 2024]. Mazareanu E. United States Postal Service - mail volume. https://www.statista.com/statistics/320234/mail-volume-of-the-usps/#:text=United%20States%20Postal%20Service%20%2D%20mail%20volume%202004%2D2020&text=After%20reaching%20a%20peak%20of,to%20just%20129.2%20billion%20units [Accessed 4 May 2024]. BBC. What is happening to the Royal Mail? http://news.bbc.co.uk/2/hi/business/8304722.stm [Accessed 4 May 2024]. Edwards PJ, Roberts I, Clarke MJ, DiGuiseppi C, Woolf B, Perkins C. Methods to increase response to postal and electronic questionnaires. Cochrane Database Syst Rev. 2023;11(11):MR000008. https://doi.org/10.1002/14651858.MR000008.pub5 . Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA, Cochrane Bias Methods Group; Cochrane Statistical Methods Group. The Cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. https://doi.org/10.1136/bmj.d5928 . Article PubMed PubMed Central Google Scholar Harris RJ, Deeks JJ, Altman DG, Bradburn MJ, Harbord RM, Sterne JAC. Metan: fixed- and Random-effects Meta-Analysis. Stata J. 2008).;8(1):3–28. https://doi.org/10.1177/1536867X0800800102 . Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60. Schultz, et al. Empirical evidence of Bias - dimensions of Methodological Quality Associated with estimates of Treatment effects in controlled trials. JAMA. 1995;273(5):408–12. Article Google Scholar Sterne JA, Jüni P, Schulz KF, Altman DG, Bartlett C, Egger M. Statistical methods for assessing the influence of study characteristics on treatment effects in ‘meta-epidemiological’ research. Stat Med . 2002;21(11):1513-24. https://doi.org/10.1002/sim.1184 . PMID: 12111917. Harbord RM, Harris RJ, Sterne JA. Updated tests for small-study effects in meta-analyses. Stata J. 2009;9(2):197–210. Akl EA, Maroun N, Klocke RA, Montori V, Schünemann HJ. Electronic mail was not better than postal mail for surveying residents and faculty. J Clin Epidemiol. 2005;58(4):425–9. Basnov M, Kongsved SM, Bech P, Hjollund NH. Reliability of short form-36 in an Internet- and a pen-and-paper version. Inform Health Soc Care. 2009;34(1):53 – 8. doi: 10.1080/17538150902779527. PMID: 19306199. Bech M, Kristensen MB. Differential response rates in postal and web-based surveys among older respondents. Surv Res Methods. 2009;3(1):1–6. Google Scholar Beebe TJ, Jacobson RM, Jenkins SM, Lackore KA, Rutten LJF. Testing the impact of mixed-Mode designs (mail and web) and multiple contact attempts within Mode (Mail or web) on Clinician Survey Response. Health Serv Res. 2018;53(Suppl 1):3070–83. Epub 2018 Jan 22. PMID: 29355920; PMCID: PMC6056581. Bergeson SC, Gray J, Ehrmantraut LA, Laibson T, Hays RD. Comparing Web-based with Mail Survey Administration of the Consumer Assessment of Healthcare Providers and Systems (CAHPS R) Clinician and Group Survey. Primary health care: open access. 2013;3. Bjertnaes O, Iversen HH, Skrivarhaug T. A randomized comparison of three data collection models for the measurement of parent experiences with diabetes outpatient care. BMC Med Res Methodol. 2018;18(1):95. https://doi.org/10.1186/s12874-018-0557-z . PMID: 30236067; PMCID: PMC6149010. Bray I, Noble S, Robinson R, Molloy L, Tilling K. Mode of delivery affected questionnaire response rates in a birth cohort study. J Clin Epidemiol. 2017;81:64–71. Brøgger J, Nystad W, Cappelen I, Bakke P. No increase in response rate by adding a web response option to a postal population survey: a randomized trial. J Med Internet Res. 2007;9(5):e40. Clark M, Rogers M, Foster A, Dvorchak F, Saadeh F, Weaver J, et al. A randomized trial of the impact of survey design characteristics on response rates among nursing home providers. Eval Health Prof. 2011;34(4):464–86. Cobanoglu C, Moreo PJ, Warde B. A comparison of mail, fax and web-based Survey methods. Int J Market Res. 2001;43(4):1–15. Fluss E, Bond CM, Jones GT, Macfarlane GJ. The effect of an internet option and single-sided printing format to increase the response rate to a population-based study: a randomized controlled trial. BMC Med Res Methodol 2014;14. Fowler FJ Jr, Cosenza C, Cripps LA, Edgman-Levitan S, Cleary PD. The effect of administration mode on CAHPS survey response rates and results: a comparison of mail and web-based approaches. Health Serv Res. 2019;54(3):714–21. Hardigan PC, Succar CT, Fleisher JM. An analysis of response rate and economic costs between mail and web-based surveys among practicing dentists: a randomized trial. J Community Health. 2012;37(2):383–94. Hardigan PC, Popovici I, Carvajal MJ. Response rate, response time, and economic costs of survey research: a randomized trial of practicing pharmacists. Res Social Administrative Pharm. 2016;12(1):141–8. Hohwu L, Lyshol H, Gissler M, Jonsson SH, Petzold M, Obel C. Web-based Versus Traditional Paper questionnaires: a mixed-Mode Survey with a nordic perspective. J Med Internet Res 2013;15(8). Iversen HH, Holmboe O, Bjertnaes O. Patient-reported experiences with general practitioners: a randomised study of mail and web-based approaches following a national survey. BMJ open. 2020;10(10):e036533. Jacob RT, Jacob B. Prenotification, incentives, and Survey Modality: an experimental test of methods to increase Survey Response Rates of School principals. J Res Educational Eff. 2012;5(4):401–18. Lagerros YT, Sandin S, Bexelius C, Litton JE, Löf M. Estimating physical activity using a cell phone questionnaire sent by means of short message service (SMS): a randomized population-based study. Eur J Epidemiol. 2012;27(7):561–6. Leece P, Bhandari M, Sprague S, Swiontkowski MF, Schemitsch EH, Tornetta P, et al. Internet versus mailed questionnaires: a randomized comparison (2). J Med Internet Res. 2004;6(3):26–33. Mauz E, Hoffmann R, Houben R, Krause L, Kamtsiuris P, Gößwald A. Population-Based Health Interview Surveys for Children and Adolescents: Methodological Study. J Med Internet Res. 2018;20(3):e64. https://doi.org/10.2196/jmir.7802 . PMID: 29506967; PMCID: PMC5859740. Mode Equivalence of Health Indicators Between Data Collection Modes and Mixed-Mode Survey Designs in. Millar MM, Dillman DA. Improving response to web and mixed-Mode surveys. Pub Opin Q. 2011;75(2):249–69. Millar MM, Elena JW, Gallicchio L, Edwards SL, Carter ME, Herget KA, Sweeney C. The feasibility of web surveys for obtaining patient-reported outcomes from cancer survivors: a randomized experiment comparing survey modes and brochure enclosures. BMC Med Res Methodol. 2019;19(1):208. Murphy CC, Craddock Lee SJ, Geiger AM, Cox JV, Ahn C, Nair R, Gerber DE, Halm EA, McCallister K, Skinner CS. A randomized trial of mail and email recruitment strategies for a physician survey on clinical trial accrual. BMC Med Res Methodol. 2020;20(1):123. Reinisch JF, Yu DC, Li WY. Getting a Valid Survey Response From 662 Plastic Surgeons in the 21st Century. Ann Plast Surg. 2016;76(1):3–5. https://doi.org/10.1097/SAP.0000000000000546 . PMID: 26418779. Sakshaug JW, Vicari B, Couper MP. Paper, e-mail, or both? Effects of contact mode on participation in a web survey of establishments. Social Sci Comput Rev. 2019;37(6):750–65. Schmuhl P, Van Duker H, Gurley KL, Webster A, Olson LM. Reaching emergency medical services providers: is one survey mode better than another? Prehospital Emerg Care. 2010;14(3):361–9. Schwartzenberger J, Presson A, Lyle A, O’Farrell A, Tyser AR. Remote Collection of patient-reported outcomes following outpatient hand surgery: a Randomized Trial of Telephone, Mail, and E-Mail. J Hand Surg. 2017;42(9):693–9. Scott A, Jeon SH, Joyce CM, Humphreys JS, Kalb G, Witt J et al. A randomised trial and economic evaluation of the effect of response mode on response rate, response bias, and item non-response in a survey of doctors. BMC Med Res Methodol 2011;11. Sebo P, Maisonneuve H, Cerutti B, Fournier JP, Senn N, Haller DM, Rates. Delays, and Completeness of General Practitioners’ Responses to a Postal Versus Web-Based Survey: A Randomized Trial. J Med Internet Res 2017;19(3). Taylor S, Ferguson C, Peng F, Schoeneich M, Picard RW. Use of In-Game rewards to Motivate Daily Self-Report Compliance: Randomized Controlled Trial. J Med Internet Res. 2019;21(1):e11683. https://doi.org/10.2196/11683 . PMID: 30609986; PMCID: PMC6682282. van den Berg MH, Overbeek A, van der Pal HJ, Versluys AB, Bresters D, van Leeuwen FE et al. Using web-based and paper-based questionnaires for Collecting Data on Fertility Issues among Female Childhood Cancer survivors: differences in response characteristics. J Med Internet Res 2011;13(3). Weaver L, Beebe TJ, Rockwood T. The impact of survey mode on the response rate in a survey of the factors that influence Minnesota physicians’ disclosure practices. BMC Med Res Methodol. 2019;19(1):73. Whitehead L. Methodological issues in internet-mediated research: a randomized comparison of internet versus mailed questionnaires. J Med Internet Res. 2011;13(4):e109. Yetter G, Capaccioli K. Differences in responses to web and paper surveys among school professionals. Behav Res Methods. 2010;42(1):266–72. Ziegenfuss JY, Beebe TJ, Rey E, Schleck C, Locke GR 3rd, Talley NJ. Internet option in a mail survey: more harm than good? Epidemiology. 2010;21(4):585–6. https://doi.org/10.1097/EDE.0b013e3181e09657 . Shih TH, Fan X. Response Rates and Mode preferences in Web-Mail mixed-Mode surveys: a Meta-analysis. Int J Internet Sci. 2007;2(1):59–82. Medway RL, Fulton J. When more gets you less - a Meta-analysis of the effect of concurrent web options on Mail Survey Response Rates. Pub Opin Q. 2012;76(4):733–46. Petrosyan A. Global internet access rate 2005–2022. https://www.statista.com/statistics/209096/share-of-internet-users-worldwide-by-market-maturity/#:text=As%20of%202022%2C%2066%20percent,access%20rate%20was%2066%20percent [Accessed 4 May 2024]. Vestberg H. How can we bring 2.6 billion people online to bridge the digital divide? World Economic Forum Annual Meeting; Jan 2024. https://www.weforum.org/agenda/2024/01/digital-divide-internet-access-online-fwa/ [Accessed 4 May 2024]. Scott P, Edwards P. Personally addressed hand-signed letters increase questionnaire response: a meta-analysis of randomised controlled trials. BMC Health Serv Res. 2006;6:111. https://doi.org/10.1186/1472-6963-6-111 . Harbord RM, Egger M, Sterne JA. A modified test for small-study effects in meta-analyses of controlled trials with binary endpoints. Stat Med. 2006;25(20):3443-57. https://doi.org/10.1002/sim.2380 . PMID: 16345038. Edwards P, Cooper R, Roberts I, Frost C. Meta-analysis of randomised trials of monetary incentives and response to mailed questionnaires. J Epidemiol Community Health. 2005;59(11):987–99. https://doi.org/10.1136/jech.2005.034397 . Treweek S, Bevan S, Bower P, Campbell M, Christie J, Clarke M, et al. Trial Forge Guidance 1: what is a study within a trial (SWAT)? Trials. 2018;19(1):139. https://doi.org/10.1186/s13063-018-2535-5 . Galea S, Tracy M. Participation rates in epidemiologic studies. Ann Epidemiol. 2007;17(9):643–53. Dillman DA. Towards survey response rate theories that no longer pass each other like strangers in the night. In: Brenner PS, editor. Understanding survey methodology - sociological theory and applications. Switzerland: Springer Nature; 2020. pp. 15–44. Chapter Google Scholar Griffin DH, Fischer DP, Morgan MT. Testing an Internet Response Option for the American Community Survey. Washington: U.S. Bureau of the Census, 2001. https://www.census.gov/library/working-papers/2001/acs/2001_Griffin_01.html [Accessed 27 October 2023]. Sinclair M, O’Toole J, Malawaraarachchi M, et al. Comparison of response rates and cost-effectiveness for a community-based survey: postal, internet and telephone modes with generic or personalised recruitment approaches. BMC Med Res Methodol. 2012;12:132. https://doi.org/10.1186/1471-2288-12-132 . Download references AcknowledgementsNot applicable. This work was supported by the NIHR Evidence Synthesis Programme [Grant NIHR133238]. Conduct of the work was entirely independent of the funder. Author informationAuthors and affiliations. Data Collection Methodology Group, Department of Population Health, Faculty of Epidemiology and Population Health, London School of Hygiene & Tropical Medicine, Keppel Street, London, WC1E 7HT, UK Phil Edwards & Chloe Perkins You can also search for this author in PubMed Google Scholar ContributionsPE independently screened the search results and the full-text reports, and extracted data from eligible studies. He assisted with data entry into RevMan 5. He exported data into Stata and he conducted the meta-analyses and other statistical analyses. He drafted the manuscript. PE is guarantor for the paper.CP ran the electronic searches, independently screened the search results and the full-text reports, and extracted data from eligible studies. CP assisted with data entry into RevMan 5, and commented on the manuscript. Corresponding authorCorrespondence to Phil Edwards . Ethics declarationsEthics approval and consent to participate, consent for publication, competing interests. The authors declare no competing interests. Additional informationPublisher’s note. Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Electronic supplementary materialBelow is the link to the electronic supplementary material. Supplementary Material 1Supplementary material 2, supplementary material 3, supplementary material 4, supplementary material 5, supplementary material 6, supplementary material 7, rights and permissions. Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . Reprints and permissions About this articleCite this article. Edwards, P., Perkins, C. Response is increased using postal rather than electronic questionnaires – new results from an updated Cochrane Systematic Review. BMC Med Res Methodol 24 , 209 (2024). https://doi.org/10.1186/s12874-024-02332-0 Download citation Received : 06 November 2023 Accepted : 06 September 2024 Published : 16 September 2024 DOI : https://doi.org/10.1186/s12874-024-02332-0 Share this articleAnyone you share the following link with will be able to read this content: Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative
BMC Medical Research MethodologyISSN: 1471-2288
 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
IMAGES
VIDEO
COMMENTS
Article processing charges (APC) Authors who publish open access in BMC Medical Research Methodology are required to pay an article processing charge (APC). The APC price will be determined from the date on which the article is accepted for publication. The current APC, subject to VAT or local taxes where applicable, is: £2190.00/$2990.00/€ ...
Publish your healthcare research with BMC Medical Research Methodology, with 3.9 Impact Factor and 18 days to first decision. Focusing on manuscripts ...
An article-processing charge (APC) applies for each article accepted for publication in BMC Medical Research Methodology . For further details please see our article-processing-charge page.
Article processing charges (APC) The publication costs for BMC Methods are covered by Springer Nature until 30 November 2024. Authors whose articles are accepted for publication before that date will not pay an article processing charge - see submission guidelines.
Article processing charges. All articles published in our journals are open access and freely available online, immediately upon publication. This is made possible by an article-processing charge (APC) that covers the range of publishing services we provide. This includes provision of online tools for editors and authors, article production and ...
Find breakthrough research in BMC Medicine, an open access journal with 7.0 Impact Factor, and 6 days to first decision. Open for submissions! BMC Medicine ...
A peer-reviewed, open access journal in research methodology, review methodology & clinical trial methodology.
Scope BMC Medical Research Methodology is an open access journal publishing original peer-reviewed research articles in methodological approaches to healthcare research.
About this journal Focusing on manuscripts describing a rigorous methodological approach to healthcare research, BMC Medical Research Methodology is in the top quartile of journals publishing research on health care sciences. Peer-review is overseen by our experienced editorial board composed of active researchers who are enthusiastic about making methodology studies openly available. This ...
BMC Methods is an open-access, peer-reviewed journal that focuses on publishing lab protocols and methodology papers in the natural sciences; including biology, chemistry, physics, computational and biomedical sciences. The journal serves as a platform for researchers to disseminate experimental procedures, novel techniques, and innovative ...
We have APC data for both 2018 and 2019 for 260 BMC journals. The average APC for these journals was 1,416 GBP in 2018, 1,555 GBP in 2019, an average increase of 139 GBP or an average 9% increase. The pricing changes are more complex, however, as some BMC journals have maintained or lowered their prices.
Archive of "BMC Medical Research Methodology". - PMC An official website of the United States government Here's how you know
Publisher Policy Open Access pathways permitted by this journal's policy are listed below by article version. Click on a pathway for a more detailed view.
Publish your healthcare research with BMC Medical Research Methodology, with 3.9 Impact Factor and 18 days to first decision. Focusing on manuscripts ...
BMC Medical Research Methodology | Citations: 4,715 | Focusing on manuscripts describing a rigorous methodological approach to healthcare research, BMC Medical Research Methodology is in the top ...
Scoping review design. This study followed the Joanna Briggs Institute (JBI) methodology [] for conducting and reporting scoping reviews built on Arksey and O'Malley's framework []: (1) Define and align the objectives (2) develop and align the inclusion criteria with the objectives (3) describe the planned approach to evidence searching, selection, data extraction, and presentation of the ...
Background Portal vein tumor thrombosis (PVTT) commonly occurs in patients with primary liver cancer (PLC). Transarterial chemoembolization (TACE) is a treatment for patients with PLC and PVTT. Some studies have shown that combining TACE therapy with hepatic arterial infusion chemotherapy (HAIC) might improve the survival rate of PLC patients with PVTT. However, few studies have compared the ...
Academic dishonesty as a fundamental challenge in adherence of ethical principles in providing care to patients has caused concern to the scientific community of nurses. In addition, positive professional identity and high moral competence are important for nurses to perform multiple care roles in high quality care of patients. The purpose of the present study is of investigating academic ...
Background Projection of future cancer incidence is an important task in cancer epidemiology. The results are of interest also for biomedical research and public health policy. Age-Period-Cohort (APC) models, usually based on long-term cancer registry data (> 20 yrs), are established for such projections. In many countries (including Germany), however, nationwide long-term data are not yet ...
Introduction Cardiovascular disease (CVD) is a major health concern worldwide, particularly in low- and middle-income countries. The COVID-19 pandemic that emerged in late 2019 may have had an impact on the trend of CVD mortality. This study aimed to investigate the trend and changes in CVD mortality rates in Malaysia, using age-standardized mortality rates (ASMR) from 2010 to 2021. Methods ...
Abstract— The results of surveying echolocation signals of bats, performed using an Echo Meter Touch 2 PRO ultrasonic detector, are given. The signals were recorded in the time-expansion mode and identified manually in the BatSound program. The surveys were made in June-August 2019-2020 in the northwestern part of Voronezh oblast within the Federal Voronezh State Nature Reserve. Four ...
Voronezh State Medical University (VSMU), founded in 1930, is a prestigious institution in Voronezh, Russia, offering programs in medicine, dentistry, and pharmacy. The university combines theoretical knowledge with practical skills and features modern facilities, including advanced labs, a large library, and well-equipped lecture halls. With a focus on international collaboration, VSMU ...
Objective This study aims to assess the economic burden of prostate cancer in Iran by analyzing direct medical costs, direct non-medical costs, and indirect costs. We conducted a cross-sectional cost-of-illness study in Khorramabad, located in western Iran, during 2023, using a prevalence-based, bottom-up approach. Data were collected from 285 prostate cancer patients using questionnaires ...
Background Stepped wedge randomised trial designs involve sequential roll-out of an intervention to participants (individuals or clusters) over a number of time periods. By the end of the study, all participants will have received the intervention, although the order in which participants receive the intervention is determined at random. The design is particularly relevant where it is ...
Plan you week with the help of our 10-day weather forecasts and weekend weather predictions for Voronezh, Voronezhskaya oblast', RU
Background Experimental studies of wound healing often use survival analysis and time to event outcomes or differences in wound area at a specific time point. However, these methods do not use a potentially large number of observations made over the course of a trial and may be inefficient. A model-based approach can leverage all trial data, but there is little guidance on appropriate models ...
Satellite imagery has revealed the extensive damage caused by a fire at a Russian ammunition depot in Voronezh Oblast, reportedly triggered by a Ukrainian drone attack.
Background Systematic reviews (SRs) are time-consuming and labor-intensive to perform. With the growing number of scientific publications, the SR development process becomes even more laborious. This is problematic because timely SR evidence is essential for decision-making in evidence-based healthcare and policymaking. Numerous methods and tools that accelerate SR development have recently ...
Background and objectives Although the goal of translational research is to bring biomedical knowledge from the laboratory to clinical trial and therapeutic products for improving health, this goal has not been well achieved as often as desired because of many barriers documented in different countries. Therefore, the aim of this study was to investigate the challenges and opportunities of ...
Rationale. When collecting information from large, geographically dispersed populations, a self-administered questionnaire is usually the only financially viable option [].Non-responses to questionnaires reduce effective sample sizes, reducing study power, and may introduce bias in study results [].The Cochrane Methodology Review of methods to increase response to self-administered ...