Blog > 10 creative Ideas for your Title- and End-Slides in Presentations

10 creative Ideas for your Title- and End-Slides in Presentations
11.13.19 • #powerpointtips #presentation.
Of all the slides in a PowerPoint presentation, the ones that are without a doubt the most important ones are the first and the last one. It makes perfect sense – the title slide sets the general tone. Make it boring and you’ll loose your audience’s attention within the first few minutes. If you’re making it exciting and innovative on the other hand, you’re taking a big step towards giving an amazing presentation and having an engaged audience. It is very similar with the final slide. It will be the one that people are going to remember most, the one that is supposed to make people leave the room thinking ‘Wow! What a great presentation!’ A bad ending could even mess up what would otherwise be a good performance overall (just think of a good TV show with a bad ending…).
The most common mistakes for title and final slides
If you asked 100 people what belongs on your PowerPoint’s title slide, the majority would answer ‘The title, maybe a subtitle, the presenter’s name and company, the date’. That kind of title slide is alright, but you usually say all of these things in the beginning of a presentation anyway. Also, it is very likely that most of your attendees know these things – they usually signed up for it after all. So what’s the point in listing all of that information on your title slide, when you could also use it for making a stunning first impression? Not only the title slide is commonly designed in an uncreative and conventional way. Too often, you can see PowerPoint presentations ending with the ‘Any Questions?’ or even worse – the ‘Thank you for your attention’ slide. ‘Thank you for your attention’ is a set phrase that has been said so many times it can’t possibly be delivered in an authentic way anymore. Therefore, it’s better to think of something else for your grand final. Finding an unconventional ending that suits your presentation style makes you seem much more charismatic and authentic than using an empty phrase.

1. An inspiring quote
An inspiring quote on your slide is a perfect way to both start and finish your presentation. Well, it does not have to be inspiring. It could be any quote that is somehow connected to your presented topic. Just have fun looking through books and the internet to find interesting quotes that you want your audience to hear. Good pages to look at for inspiration are goodreads and brainyquotes.com .
2. A blank slide
This might seem strange to some people, but a blank slide can be really powerful if you want to have your audience’s full attention. You can use the advantage of blank slides by incorporating them at the beginning, in the end or even in between your regular slides. You can either use a blank slide of your regular template (so there will still be some design elements on it) or go all in and make the slide completely black (or white).
3. A call to action
If the goal of your presentation is to really make your audience act in some kind of way, there is no better way to start – or better yet end your presentation than with a call to action. This can be literally anything from little trivial things like “Drink enough water during the presentation so your brain stays intact!” – which will lighten up the mood – to more serious calls like “Help reducing waste by recycling whenever possible!”.
4. A question
Usually, it is the audience that asks questions after a presentation. However, you can also turn that around and ask your attendees instead. However, it’s important to ask a question that can be answered easily and individually – the best questions involve previous experiences and personal opinions (asking about facts or questions that are hard to understand can often lead to silence and no one wanting to answer).
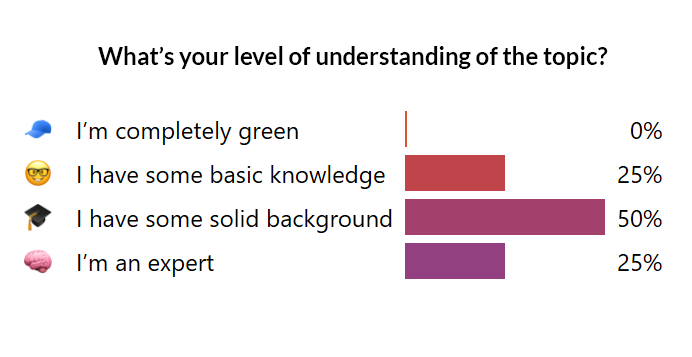
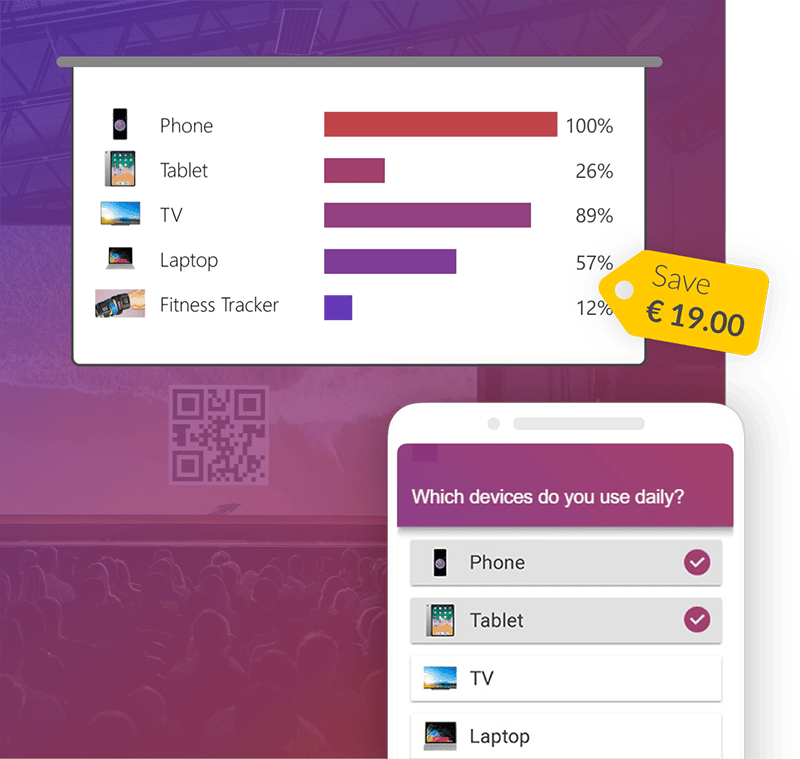
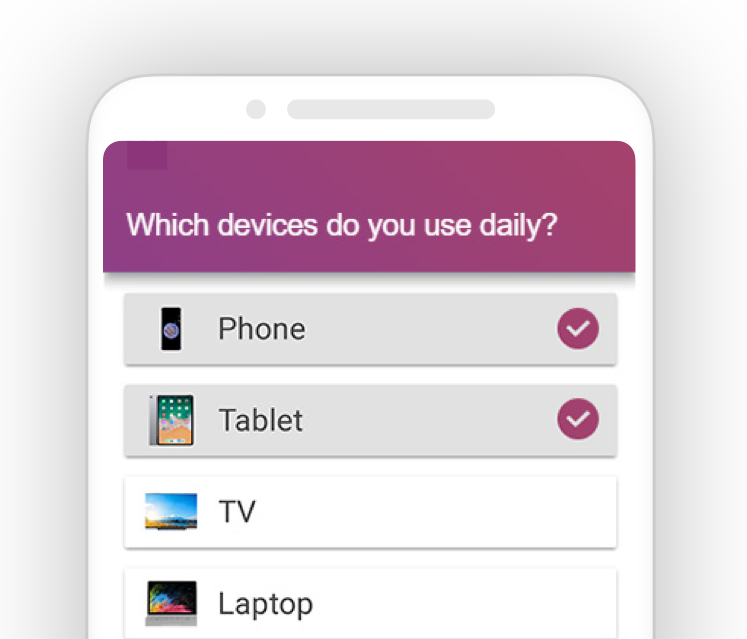
5. An interactive poll
Nothing engages the audience like a live poll. Conduct one right at the beginning to get everybody envolved, and/or wait until the end to get your audience’s opinion on something. Icebreaker polls are the perfect way to start, as they lighten the mood. You can easily create polls for free with interactive software tools such as SlideLizard .
6. A funny picture, meme, or quote
I’m pretty sure that every student nowadays has that teacher that just tries a little too hard to be cool by throwing in a meme on literally every single slide. That may be a bit too much. But just a little comedy at the beginning or in the end can make you seem very charismatic and entertaining and catch the attention of your listeners. Open (or close) with a joke, a funny picture or a quote – whichever you feel comfortable with. It is usually best if it has something to do with the topic you’re presenting.

7. An interesting fact
Catch the audience’s attention by putting an interesting fact concerning the topic on one of your slides – ideally at the beginning, but maybe also in the end (to keep up the audience’s interest even after the presentation is done).
8. The title, but with a twist
If you feel like you need to put the presentations name/topic on the front slide, but still want that little creative twist, just change the title slightly. According to what I’m proposing, rather dull presentation titles like e.g. “Marine Biology – An Introduction to Organisms in the sea” can be transformed to “Marine Biology – Diving Deep” (or something less cheesy if you prefer). Make it either funny or over-the-top spectacular and catch the audience’s attention!

9. A bold statement, opinion, or piece of information
This is probably the best way to capture your audience from the beginning on. Start with a radical, crazy opinion or statement and then get your attendees hooked by telling them that during the presentation, they will learn why you’re right. It could be anything, really, as long as it goes well with your presented topic – from the statement “Everybody has the time to read 5 books a month” to “Going to college is a waste of time” or “The human species is not the most intelligent on earth” – Take whatever crazy, unpopular theory or opinion you have, throw it out there and (very important!) explain why you’re right. You’ll have your audience’s attention for sure and might even change some of their opinions about certain things.
10. No title and end slide at all
Yes, that’s a possibility as well. If you absolutely can’t think of any creative or otherwise good way to start and end your presentation – even after reading the tips mentioned above – then simply don’t. That’s right - no title and end slide at all. You can pull that of by simply introducing yourself in the beginning, then getting right into the topic (which makes a good impression, long introductions are usually rather tedious) and when you’re at your last slide just saying a simple ‘Goodbye, thank you and feel free to ask questions’.
Related articles
About the author.

Pia Lehner-Mittermaier
Pia works in Marketing as a graphic designer and writer at SlideLizard. She uses her vivid imagination and creativity to produce good content.
Get 1 Month for free!
Do you want to make your presentations more interactive.
With SlideLizard you can engage your audience with live polls, questions and feedback . Directly within your PowerPoint Presentation. Learn more

Top blog articles More posts

6 Tips to turn your boring slides into stunning presentations
Microsoft Copilot: A Comprehensive Review of the AI tool
Get started with Live Polls, Q&A and slides
for your PowerPoint Presentations
The big SlideLizard presentation glossary
Visual communication.
If there are used images or videos for communication, it is visual communication. Visual Communication is almost used everywhere like on television, posts on social media (Instagram, Facebook), advertisement.
.ppt file extension
A .ppt file is a presentation which was made with PowerPoint, that includes different slides with texts, images and transition effects.
Virtual Event
Virtual events take place entirely online. They are very convenient as anyone may join from wherever they are via a smartphone or computer.
Recall Questions
With recall questions, you have to remember something or something has to be recalled. Example: A teacher asks his students a question so that they remember the material from the last lesson.
Be the first to know!
The latest SlideLizard news, articles, and resources, sent straight to your inbox.
- or follow us on -
We use cookies to personalize content and analyze traffic to our website. You can choose to accept only cookies that are necessary for the website to function or to also allow tracking cookies. For more information, please see our privacy policy .
Cookie Settings
Necessary cookies are required for the proper functioning of the website. These cookies ensure basic functionalities and security features of the website.
Analytical cookies are used to understand how visitors interact with the website. These cookies help provide information about the number of visitors, etc.
- Skip to primary navigation
- Skip to main content
- Skip to footer

Laura M. Foley Design
Cheat Death by PowerPoint!
How to create an effective title slide in PowerPoint
April 10, 2013 by Laura Foley 5 Comments
Presenters often overlook a valuable opportunity to connect with their audience: their title slides.
Think about it. Your title slide is up there on the screen while you wait for the audience to arrive and find their seats. It might be onscreen while you’re being introduced by your host. Your title slides can be very effective billboards for you, but only if you design them well.
The most important elements of a title slide
Since title slides are usually on display for a while before a presentation, you want to make sure that they’re doing a good job of marketing you, your topic, and your company. Always include the following elements on your title slides:
- Title of presentation, with a subtitle if the presentation’s title is unclear
- Contact information (email address, Twitter account, website, etc.)
- Company logo
Providing this information on the title slide tells the audience what they’re about to hear, who’s responsible for the presentation, and how to get in touch with you if they need to.
Simple title slides
Let’s look at a typical title slide for a corporate presentation:
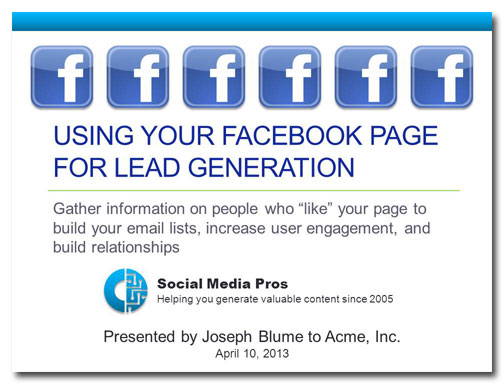
- There is too much text on the slide and it’s all competing for our attention.
- The abundance of Facebook logos distract viewers from the logo of the presenter’s company.
- That subtitle looks more like a paragraph.
- You don’t have to point out the organization to which your audience belongs. The audience already knows what company they work for.
- You also don’t have to tell them what day it is.
Here’s how I would redesign this slide while remaining true to the template:
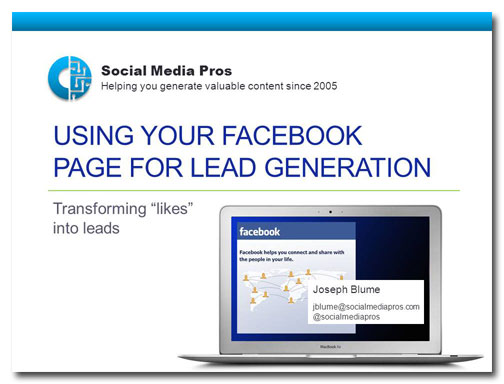
- The multiple Facebook logos have been replaced by an image that appears to be on a computer screen. Because I chose the typographic Facebook logo, it doesn’t compete with the presenter’s company logo.
- The presenter’s name appears to be a window on a computer screen, and his email address and Twitter name have been provided.
- The company logo is now on the top of the slide, giving it the most importance.
- The subtitle has been shortened from 19 words to four.
Animated title slides
Sometimes your subject matter will lend itself to a more interesting approach to your title slides. Animating a title slide can be a great way to provide contact information, to invite people to subscribe to your blog or newsletter, or to introduce opportunities for audience participation. The animation reveals information a little at a time, creating anticipation and interest.
We begin with a plain, unimaginative title slide:
Wake me when it’s over
ZZ ZZZZ ZZ ZZ ZZ … snork! Wha…what? I’m awake, I’m awake. I wasn’t sleeping!
The title and subtitle are fine, but, again, the remaining text doesn’t tell the audience something they don’t already know. And the layout is totally boring.
Now you’re talking!
Click on the video link below to see how the animations play on this title slide. I’ve sped up the animation for this demo, but if this slide were actually being used in a presentation I’d wait a couple of minutes between animations.
Presenting this information in the form of sticky notes is a good idea for this particular subject because they are used to organize thoughts and messages. They are often overused, being pasted on top of one another until their original purpose of organization is lost. Take a look at the image below, which is what the audience would see after the animations have played out.

This slide tells the audience who the presenter is, provides a personalized greeting, and includes four calls to action, including an opportunity for an audience member to win a prize. This last bit will keep people interested and engaged in the presentation, because everybody likes getting something for nothing!
What are of your ideas for creating more interesting, informative title slides?
- [email protected]
- (800) 834-7700
- Customer Portal
- Case Studies
- Training Workshops

- Food Manufacturing
- Food Distribution
- Discrete Manufacturing
- Job Shops & Made-To-Order Manufacturing
- Wholesale Distribution
- Business Central On Premise
- Business Central SaaS
- Microsoft Dynamics NAV
- Our Third Party App Partners
- BC / NAV Tune-Up
- Business Central Release Waves
- Microsoft Power Platform
- Microsoft 365 Business Plans
- Microsoft Teams
- Team's Calling Plan
- Customer Voice Surveys
- Business Central Implementations
- NAV Upgrades
- NAV Re-Implementation
- Press & News
- Upcoming Events & Webinars
- On-Demand Webinars
- Conferences
- BC Release Waves
Using Captions and Subtitles in PowerPoint
Posted By Tim Britton | Thursday, August 6, 2020
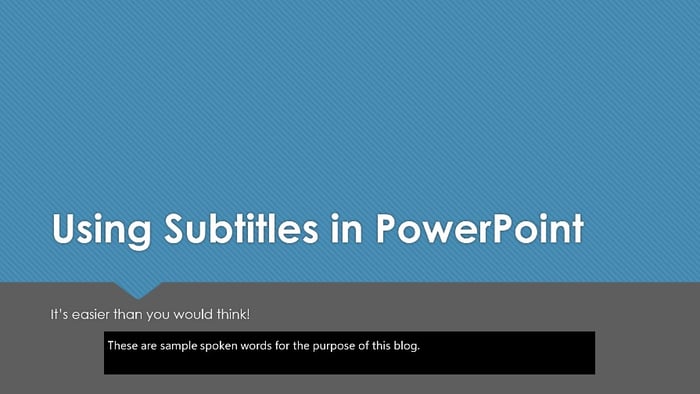
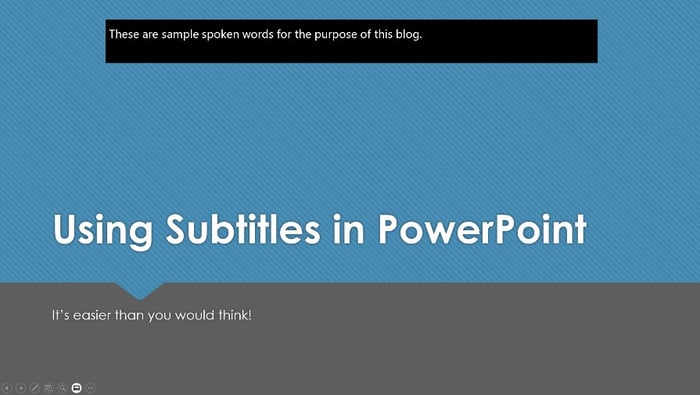
In today's blog, we are going to talk about how to use subtitles in PowerPoint. This useful feature helps ensure your audiences understand what is being said and is a great accessibility option.
To get started, open a presentation and select Slide Show from the main navigation ribbon.
At the far right, you will see a sub-menu called Captions and Subtitles . Go ahead and check the option to Always Use Subtitles, which turns on captions for your slide show. Captions and subtitles use Microsoft speech recognition services to provide you with real-time closed captioning for your presentation.
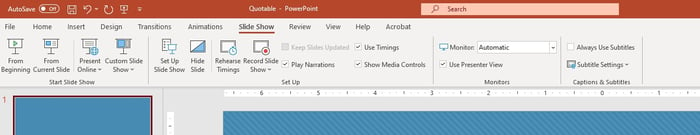
Adjusting Your Subtitles/Captions with Subtitle Settings
Under the Subtitle Settings menu, you will find a series of options to customize your subtitle experience. Let's take a closer look at each of these options in order.
- The first option you will see in your menu is the Spoken Language . You will want to choose the language that you are going to be speaking when you give the presentation. In most cases, you should not need to change this, but it's good to know the option is there in case you do.
- The second option is the Subtitle Language . This shows what language your dialogue will appear in. Microsoft Speech technology will convert your spoken words to the selected language in real-time. I have been very impressed with the overall quality of this AI. In my testing, this feature has worked accurately with every word I say.
- Continuing down the list, the next option is Microphone Settings . It is critical that you select the microphone you are going to be using as the output. Otherwise, this feature may not work as expected.
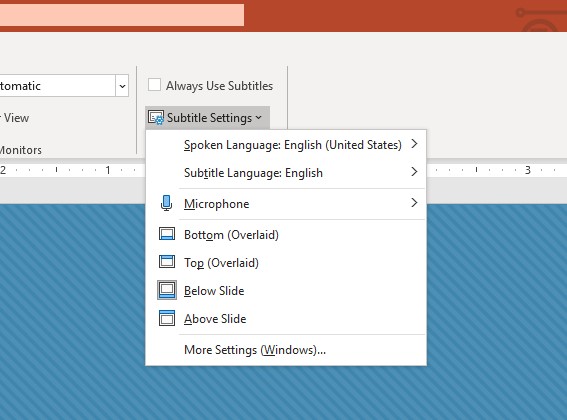
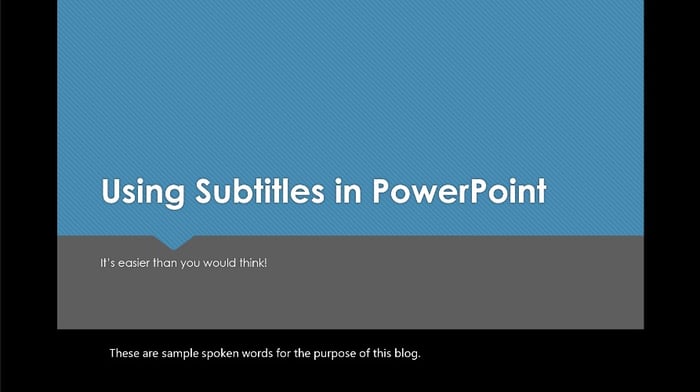
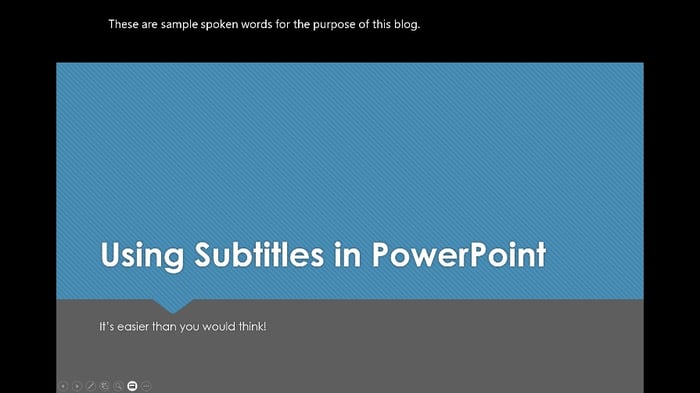
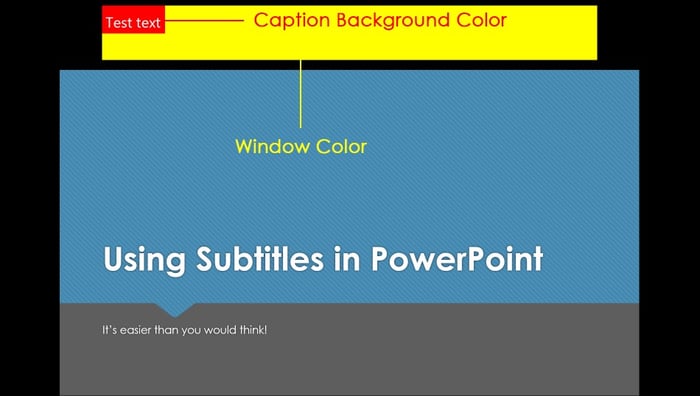
The next set of options relate specifically to the way your subtitles are formatted in the actual presentation. Below I have screenshots of how each of those captioning options looks when viewed in presentation mode.
Bottom Overlaid
Top Overlaid
Below Slide
Above Slide
More Settings for Captions/Subtitles in Windows 10
The last option in the Captions and Subtitles Menu is More Settings , which sends you to your computer’s settings to optimize the appearance of your text. I will show you what options you have in Windows 10.
The settings menu for Closed Captioning in Windows 10 is broken into 3 parts. They are:
Change Caption Font
- Change Caption Background
- Dim Window Content
Here are quick summaries of your options in all three categories
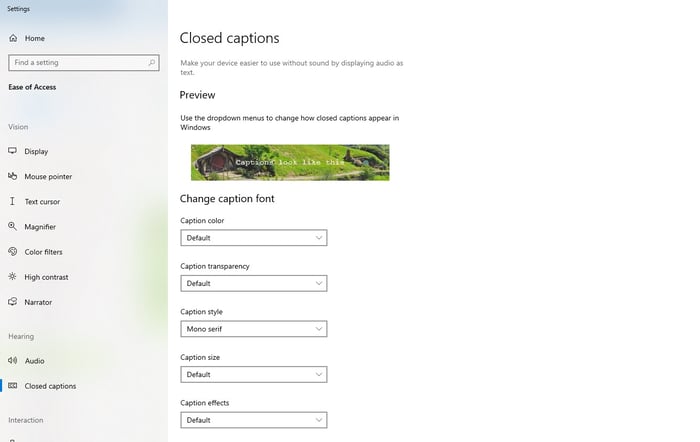
- Caption Color: Change the font color of your subtitles
- Caption Transparency: Set varying degrees of opacity to your font
- Caption Style : Change to a different font
- Caption Size: Change the overall size of the text
- Caption Effects: Some additional effects for you to choose from, most notably adding a drop shadow
Change Caption Background and Dim Window Transparency
These menus allow you to change the color and transparency of both the window and the text background for your captions.
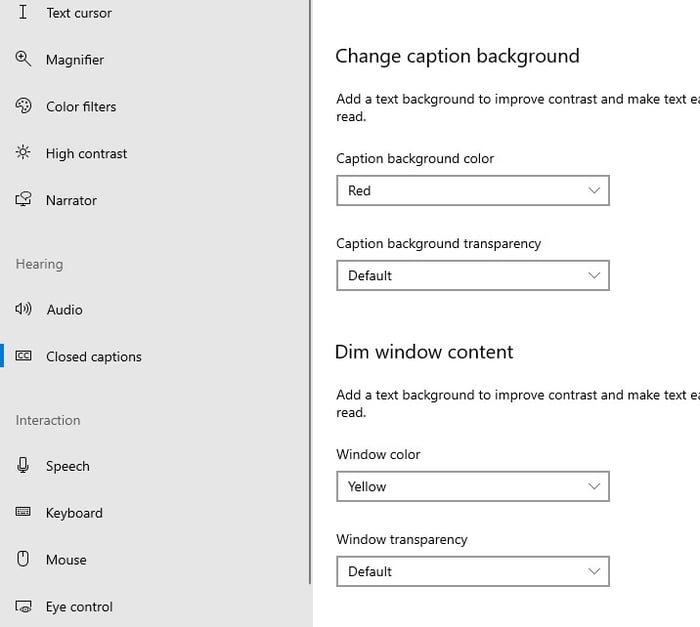
To give you a helpful visual of what that means I took a screenshot where I selected red for the caption background color and yellow for the window color.
I hope this overview has given you a good grasp of how to leverage this nifty feature when giving presentations.
If you have any questions or suggestions for another PowerPoint blog topic please feel to reach out via email [email protected] . You can also check out these other entries in my ongoing series of PowerPoint tutorials.

Related Posts

The Right Tool to Support Your Migration to The Cloud

Microsoft's New Commerce Experience (NCE) Explained

5 Reasons You Should Move to Windows 365
View All Events
Contact Info
Innovia Headquarters: 1062 Oak Forest Dr. Suite 300 Onalaska, WI 54650
Phone: 800.834.7700

Innovia is a multiple-award-winning Microsoft Dynamics NAV and Business Central consulting firm known for delivering innovative Microsoft ERP systems while providing exceptional client-focused service.

One Time Code
< Go back to Login
Forgot Password
Please enter your registered email ID. You will receive an email message with instructions on how to reset your password.

How To Create A Captivating Title Slide For A Presentation
Are you looking for a way to ditch the boring title slide and hook your audience from the start? This blog will teach you all you need to know to nail your first impression. We’ll break down the key ingredients for a captivating PowerPoint title slide, right from must-have elements to the art of titling with PowerPoint. Plus, you’ll get a step-by-step guide on how to create a title slide that will set the stage for a killer presentation.
When designing your PowerPoint presentation, there is no doubt that the most crucial slide is the one at the beginning of your presentation. A well-designed title slide can amp up your presentation game and instantly grab your audience’s attention.
What Is A Title Slide?
As the name suggests, a title slide is the first slide of a PowerPoint presentation. Usually, a title slide’s content is the presentation’s title and subtitles.
What Is The Purpose Of A Title Slide?
A title slide for a presentation has to be interesting to stand out, and one has to be very cautious while making a title slide. If you make it dull, you will lose your audience’s attention within minutes. An excellent first slide is not only a reflection of professionalism but also a great way of triggering that much-needed initial interest.
What Should Be Included In The Title Slide?
A title slide contains:
- the title of the presentation.
- a preface of a presentation, at times.
- author’s name.
- a background relevant to the topic of the presentation, at times.
- the branding of the company
How To Create A Title Slide For Presentation
Based on the device or platform you’re using PowerPoint on, you can pick from three different methods to create a presentation title slide in PowerPoint.
Method 1: Choosing A Template From The PowerPoint Library For Creating A Title Slide
Step 1: To create a title slide, open the PowerPoint presentation application and click on ‘New.’
Step 2: You will find many PowerPoint templates; double-click on the template you like and click on ‘Create.’
Step 3: The template you chose will appear. Now, the template will already have a title slide design.
Step 4: Click on the title and edit it according to your needs.
Step 5: Select the title and edit its font style, color, thickness, etc. You can customize the title, keeping in mind the background color or image of the slide.
Step 6: You can play around with the title slide’s image by cropping or adjusting it to meet your presentation style requirement.
Step 7: If you don’t like the background image, you can even delete it and adjust it according to your liking by clicking on the ‘Design’ tab and then on ‘Formate Background.’
Step 8: Tip: A plain title slide looks boring; therefore, add animations by clicking on ‘Animations’ on the file menu bar. Select the title and choose any animation.
And voila! Your title slide is ready. Make sure to play around with more tools and options to find out more features you can do to make it more attractive and presentable.
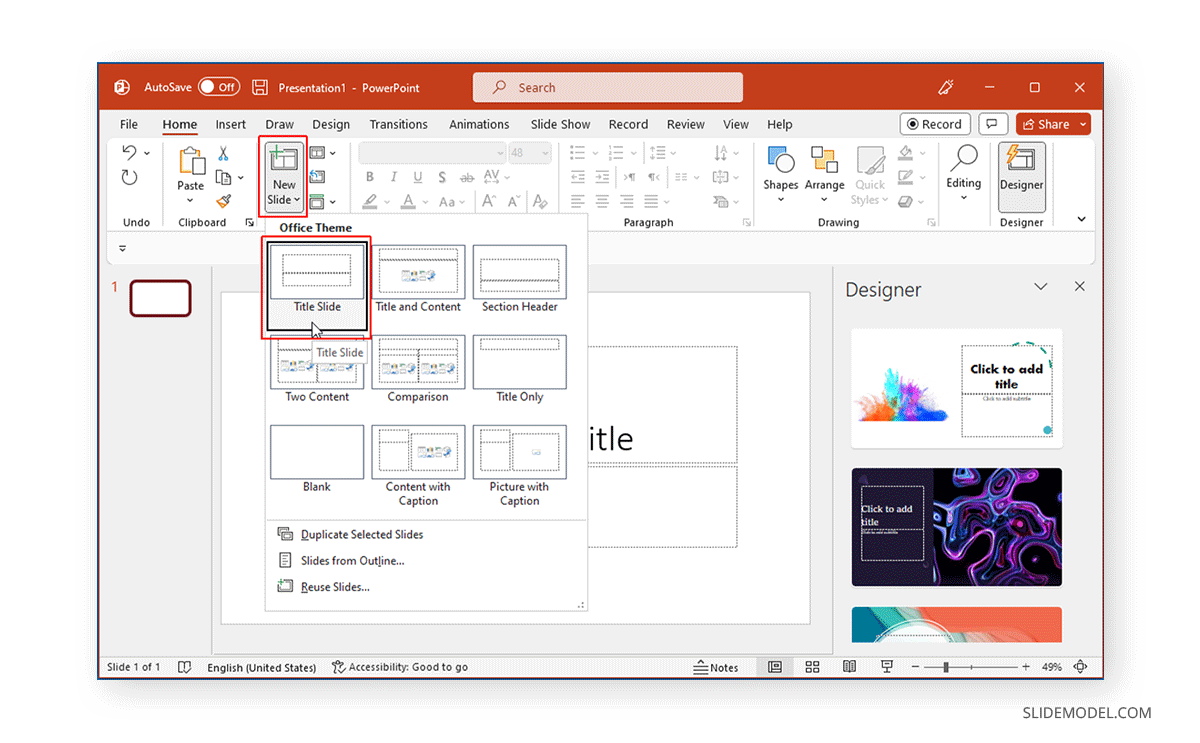
Method 2: Create A Title Slide Design Using The ‘Layout’ Option
Step 1: Open a blank presentation in your PowerPoint application and select the slide you wish to convert to a title slide.
Step 2: Click Home > Layout. Select Title Slide for a standalone title page or select Title and Content for a slide that contains a title and a full slide text box.
Step 3: Select the Click to add title text box. Enter your title for that slide.
As the previous method shows, you can similarly play around with Powerpoint animations, fonts, and colors to make it more aesthetic.
Method 3: Create A Title Slide Using Slideuplift’s PowerPoint Add-In
Slideuplift provides a plethora of templates that can assist you in making a title slide. These templates are accessible through their PowerPoint Plugin.
Follow the steps given below to make a title slide using Slideuplift PowerPoint Add-In.
Step 1: Open the slide which you want to edit.
Step 2: Go to ‘Insert,’ then click on ‘Get Add-Ins.’
Step 3: In the search bar, type ‘Slideuplift’ and click on Search.
Step 4: Click on the ‘Add’ button next to SlideUpLift, then click on ‘Continue.’
And you are done! Just type cover slides on the search console and get various PowerPoint title slides for your presentation. You can choose the one you like and make edits.
How To Title A Slide In PowerPoint
Writing a catchy title is very important. A catchy title triggers the viewers’ interest and shows that you have made some effort to make the presentation.
A title also sets the tone for a presentation; for instance, a business presentation title slide and a title slide for informal events will have a formal tone and a casual or neutral tone.
The following tips can help you write catchy presentation titles.
- Make it easy to understand.
- The title should be directly related to the presentation.
- Add an element of emotion to the title (keep it neutral during formal meetings and try to add humor if the occasion allows)
- Match other elements of the title slide, like background image, font, etc, with the title.
- Keep it concise and to the point.
Having a beautiful and functional PowerPoint title page is very important if you want to catch the attention of the viewer. A bland title page is not only boring but also shows your lack of effort, which can be a deal breaker. At the same time, keep the presentation cover page minimalistic, and only use animations and effects that add value and look interesting.
Creating the perfect title slide sure does take a lot of time and effort. We at SlideUpLift have curated a collection of PowerPoint title slides that can be used as a starting point for your presentation. These PowerPoint title slide ideas are 100% customizable and can be used on both PowerPoint and Google Slides.
It’s time to buckle up for your next presentation now that you know how to create an interesting title slide.
What Is A Good Title For A Presentation?
A good presentation title is short (under 15 words). It teases the benefit for the audience, which is what they’ll learn. Use a question, surprising fact, or statement that intrigues the audience.
How Do You Title A Presentation Slide?
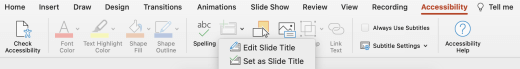
Based on which device or platform you’re using PowerPoint on, you can title a presentation slide using:
- The accessibility ribbon
- The layout option
- The outline view
Can I Add a Title To Multiple Slides At Once?
Although there isn’t a way to add the same title to multiple slides, you can use these workarounds to add a title slide to all your slides at once:
- Go to Slide > Edit theme. Add your title as word art to the theme. This way, it will show up on every slide in that presentation.
- You could also try creating your first slide and duplicating it to create the remaining slides. This way, you’ll skip typing in the title each time.
What Do You Say In The Title Slide Of A Presentation?
Your title slide PowerPoint should include a short, catchy title (benefit-focused!), your name for credibility (optional), and maybe the date/location for handouts (skip it on the slide itself).
Where Is The Layout Of The Title Slide Present In Powerpoint?
The layout of the title slide is present under the ‘home’ tab. You can change the title slide’s layout with the help of this tool.
Table Of Content
Related presentations.
Title Slides Collection

Cover Slides Colection

Animated Presentation Templates
Related posts from the same category.

15 May, 2023 | SlideUpLift
How To Add Slide Numbers To PowerPoint
Adding slide numbers to PowerPoint presentations is an important aspect of creating effective presentations. Slide numbers not only help you organize your presentation but also allow your audience to follow

16 May, 2023 | SlideUpLift
How To Move A Slide In PowerPoint
PowerPoint is an excellent presentation software that helps you create eye-catching yet informative slideshows. Whether you are making a business presentation or a school project, knowing how to move a

22 May, 2023 | SlideUpLift
How to Add a New Slide in PowerPoint
PowerPoint is a powerful tool that allows users to create engaging and dynamic slideshows for various purposes. Adding new slides to a PowerPoint presentation is a fundamental skill that is

3 May, 2024 | SlideUpLift
How To Delete A Slide In PowerPoint? [1-Minute Guide]
Whether you are giving a presentation at work, school, or to friends and family, ensuring it is polished and professional is crucial. Figuring out how to delete a slide in

How To Copy And Paste a Slide In PowerPoint
When making presentations, you can save time and effort by simply copying and pasting a slide into PowerPoint. The duplicate slide option in PowerPoint is useful to eliminate the two-step

31 May, 2023 | SlideUpLift
How to Hide And Unhide A Slide In PowerPoint
If you've ever used PowerPoint to create a presentation, you are aware that one of the reasons for its popularity is the program's extensive selection of options. There will inevitably

7 Dec, 2022 | SlideUpLift
How To Create Neumorphic PowerPoint Presentation To Dazzle Your Audience?
Neumorphic designs are a relatively recent design style that was first used in the User Interface design of gadgets in the previous decade. The perfect and straightforward design is unexpectedly

25 Jan, 2018 | SlideUpLift
PowerPoint Hack: How To Create Sections In PowerPoint And How To Zoom In PowerPoint
This PowerPoint tutorial is about How To Create Sections In PowerPoint. Imagine that you are about to begin your business presentation to a room full of clients, and you remember

26 Sep, 2022 | SlideUpLift
Learn How To Create A PowerPoint Template To Build Engaging Presentations
If you use PowerPoint often to make professional presentations, you probably have realized that PowerPoint Library doesn’t have sufficient PowerPoint templates available for all types of presentation needs. As it

26 Mar, 2024 | SlideUpLift
How To Create An Org Chart In PowerPoint?
Have you ever needed help explaining the intricacies of your company or project's structure to an investor, management, or employees? Whatever the case, creating an org chart can be a
Related Tags And Categories
Forgot Password?
Privacy Overview
Necessary cookies are absolutely essential for the website to function properly. This category only includes cookies that ensures basic functionalities and security features of the website. These cookies do not store any personal information
Any cookies that may not be particularly necessary for the website to function and is used specifically to collect user personal data via ads, other embedded contents are termed as non-necessary cookies. It is mandatory to procure user consent prior to running these cookies on your website.

- Customer stories
- Microsoft 365
Present more inclusively with Live Captions and Subtitles in PowerPoint
- The Microsoft 365 Marketing Team
- Microsoft Stream
Live presentations can be thought-provoking, inspirational, and powerful. A great presentation can inspire us to think about something in an entirely different way or bring a group together around a common idea or project. But not everyone experiences presentations in the same way. We may speak a different language from the presenter, or be a native speaker in another language, and some of us are deaf and hard of hearing. So, what if speakers could make their presentations better understood by everyone in the room? Now they can with Live Captions and Subtitles in PowerPoint .
In honor of the United Nations International Day of Persons with Disabilities , we’re announcing this new feature—powered by artificial intelligence (AI)—which provides captions and subtitles for presentations in real-time. Live Captions and Subtitles in PowerPoint supports the deaf and hard of hearing community by giving them the ability to read what is being spoken in real-time. In addition, captions and subtitles can be displayed in the same language or in a different one, allowing non-native speakers to get a translation of a presentation. At launch, Live Captions and Subtitles will support 12 spoken languages and display on-screen captions or subtitles in one of 60+ languages.
Live Captions and Subtitles in PowerPoint brings:
- The power of AI to presenters, so they can convey simple and complex information across subjects and topics.
- Speech recognition that automatically adapts based on the presented content for more accurate recognition of names and specialized terminology.
- The ability for presenters to easily customize the size, position, and appearance of subtitles. Customizations may vary by platform.
- A peace of mind with security and compliance knowing that the feature meets many industry standards for compliance certifications.
The feature joins other accessible features in Office 365, like automatic suggestions for alt-text in Word and PowerPoint , expanded availability of automatic closed captions and searchable transcripts for videos in Microsoft Stream , enhancements to the Office 365 Accessibility Checker , and more.
Here’s what one of our customers had to say:
“We are constantly looking for new ways of ensuring that the Government of Canada sets the highest possible standards as an accessible and inclusive workplace. We welcome such positive advances in technology, like this feature, that allows everyone, and notably those with disabilities, to better communicate ideas. They help break down barriers and lead to greater inclusiveness to the benefit of individuals and society as a whole.” —Yazmine Laroche, deputy minister responsible for Public Service Accessibility
Live Captions and Subtitles in PowerPoint will begin rolling out in late January 2019 and will be available for Office 365 subscribers worldwide for PowerPoint on Windows 10, PowerPoint for Mac, and PowerPoint Online.
Related Posts

From empowering frontline workers to accessibility improvements—here’s what’s new in Microsoft 365

Reduce the load on frontline workers with the right management technology

3 ways technology can help rebuild your frontline workforce

3 ways to support frontline workers in a hybrid world
Unsupported browser
This site was designed for modern browsers and tested with Internet Explorer version 10 and later.
It may not look or work correctly on your browser.
- Presentations
How to Make a Great PowerPoint Title Cover Slide Quickly (+ Video)
Want to avoid creating another boring presentation? Well-designed presentations make a great first impression. A PowerPoint title slide sets the stage for your subsequent slides!

Your PowerPoint title slide is critical for a successful slide deck.
Half the battle is building excitement with a PowerPoint title page. Invest extra time to add design polish to your cover slide PowerPoint design. Build a bold PowerPoint title slide that shows your audience that you're excited to share!
In this tutorial, I'll show you how to build a PowerPoint title page. You'll see intro slide examples that spark success. Attention is everything, and presentation title pages help you get and keep it. It's quick, easy, and key to success in 2024!
Learn How to Make Great Presentations Today: Grab our FREE eBook!
Before we take a closer look at PowerPoint cover slides, let's look at another great resource. We've got a helpful complement to this tutorial. Download our FREE eBook: The Complete Guide to Making Great Presentations . Grab it now before you read on .

How to Quickly Make Great PowerPoint Presentation Title Cover Slides (Video)
If you're making a PowerPoint title slide for your presentation, you need it to look good. Learn how to make a visually appealing PowerPoint title page quickly in the video below:

To learn even more about cover slides for PowerPoint, study the rest of the tutorial. You'll see real world examples of PowerPoint title pages. These presentation title page designs are tried-and-true options for great design.
Jump to instructions for the type of PowerPoint cover slide you're interested in:
- The Logo Slide
- The Big Question Slide
- The Introductory Slide
- The Roadmap Slide
- The Team Slide
- The Quote Slide
- The Challenge Slide
The Seven PowerPoint Cover Slides to Build
There's no limit to the directions that you can take your PowerPoint title slide. You can let your creativity run wild as you build title page in PPT designs.
But it's hard to disagree that the first slide is going to set the stage for the rest of your presentation. So, it's essential that your presentation gets off to a strong start. But what direction should you go with your presentation title page so that you grab and keep audience attention?
In this tutorial, you'll learn to build seven types of PowerPoint title slides. Here are the intro slide examples that I tend to think about when designing my PowerPoint title pages:
- The Logo Slide. Focus on the branding and brand image of your group with this PowerPoint title page! Start off by putting your logo and tagline front and center.
- The Big Question Slide. Most presentations work to inform. But it's also fun to flip the script and ask a question of your audience. It kickstarts the conversation.
- The Introductory Slide. This slide focuses on showcasing your credentials and background to establish authority.
- The Roadmap Slide. Chart the course for your presentation ahead by giving a sneak preview of the topics you'll cover.
- The Team Slide. Does your presentation focus on a group's effort? It's a great idea to start your presentation by showcasing all the minds behind the project.
- The Quote Slide. Sharing an inspirational or motivational quote is a fun way to engage your audience.
- The Challenge Slide. Many presentations strive to help solve problems. Set the stage by highlighting the big challenge immediately.
In this tutorial, we're going to build an example of each of these PowerPoint cover slides. We'll use pre-built templates to create impactful slide designs with ease. Let's dive in!
How to Make PowerPoint Title Slides
We're going to use an impressive template called the BePro PowerPoint Business template. This is one of the top PowerPoint templates for Envato Elements subscribers.
BePro has a litany of cover slide PowerPoint designs that you can use to create the perfect PowerPoint title page! It also includes several color schemes to make it easy to reuse on multiple presentation title pages.
Explore the BePro Template

Envato Elements includes over 25,000 premium PowerPoint themes! You have countless title page in PPT options. With these, you can build amazing intro slide examples of your own. Start with this collection for more great ideas:

Now, you can learn about each of the seven types of title slides:
1. The Logo Slide
The Logo Slide focuses on your brand image and showcasing the logo of your company. Branding takes center stage with this title page in PPT concept. It's ideal to use a logo slide to show your branding on the PowerPoint title page when you're building brand awareness.
A good starting point for this slide is slide design three that's built into the BePro template. It's perfect for just adding a logo and background image. In the example below, I dropped in the logo on the slide. I also took the same logo and faded it into the background image placeholder.

Make sure too that your version of the logo slide stays with the branding message. Adjust the colors of shapes and text to match the overall color scheme of your business. Presentation title pages should always fit with your overall brand style.
Building a logo slide as your title slide doesn't have to be complicated. A well-made logo slide shows your branding quickly. An alternate option for this slide is slide design 4, a simple slide with a dark color scheme. Just add your logo to that slide to create contrast.
2. The Big Question Slide
Your audience may be expecting you to impart knowledge on them. But you can flip the script by asking a question up front.
The "Big Question Slide" doesn't take much time to design. It helps you free up time that you can spend thinking about the rest of your content.
When you're writing a presentation, there should always be a goal or big idea. In the example below, I used the minimalist slide design 4 to ask a question of the audience. Over the course of the presentation, I'll answer this question for the audience.

If you aren't answering a question or sharing an idea, it might be time to re-think the content.
3. The Introductory Slide
There's nothing wrong with getting a bit personal in your presentation. Set the stage by building your authority and expertise, and the audience will trust and follow you through the presentation.
BePro has many slide designs that work well for this, but I opted for slide 25. It's a clean and straightforward slide design. It's easy to add points that explain your expertise to the audience.

As you can see above, I also added a stock photo as the background image. Envato Elements features a ton of stock images as part of the subscription. They're ideal for sourcing a stock image for your presentation.
In my example slide, I grabbed a great photo and faded it into the background. It's a great reminder that Elements is a total solution for building presentations—not just for the PowerPoint templates.
4. The Roadmap Slide
The roadmap style slide is used to tell the story of where your presentation is headed. I've sat through many presentations that seemed to wander through the agenda and would've benefitted from a roadmap slide.
When you build a roadmap, you show the audience the direction that you'll take them on over the course of the presentation.

Slide design 41 might take a bit of customization, but I do think that it's the perfect choice for showcasing your roadmap for the presentation. Just update each of the four placeholder boxes with a key section of your presentation to architect the roadmap of your big speech.
5. The Team Slide
This type of slide is the perfect intro to showcasing a project that was a total team effort. If you're going to spend your presentation sharing how you built a big app, product, or project, it's only right that you share the credit with your team.
Slide 22 in BePro is the perfect choice to build a team slide of your own. It's tailor-made to drop in images and descriptions of your team members and see it come to life.
In my example below, I put a vital member of the project team in each of the image placeholders. Giving a brief background or description of their contribution to the project is a great way to set the stage.

I think the Team Slide approach is perfect when multiple speakers are involved. Some of my favorite presentations are when several different presenters will each take a part of the presentation. If this is the style of your presentation, use a team slide that introduces everyone's role and contributions.
6. The Quote Slide
Starting off with a quote is a great way to build a PowerPoint cover slide. Share a signature quote and you can inspire and engage with your audience! Quotes provide motivation and inspiration. They can be key to helping you convey your message.
Let’s use slide #9 in the BePro template. Over on the left, you’ll see a text placeholder. Here, you can quickly keyboard in a quote to share with your audience. Optionally, up at the top, you can add a title. Using this layout as your title slide makes for a fun and inspiring opener.

As you can see, it’s easy to add a quote to your cover slide PowerPoint design. This is a good way if you’re motivating your audience to take action. Sharing the inspiring words of others helps you inspire confidence and drive your audiences to act on your message.
7. The Challenge Slide
In PowerPoint, you’re often sharing the solution to a problem. Don’t waste time - address things head-on right away! To do that, consider PPT title slide examples that outline a challenge. After all, if you’re proposing solutions, you first must define the challenge.

Above, I’ve used slide #6 to create a challenge slide. Once again, the process is quick and easy. Simply swap out the placeholder content with your own words and numbers. When you use layouts like this, there will be no confusion on the part of your audience. You can clearly show the challenge that must be accepted.
5 Quick PowerPoint Title Cover Slide Design Tips for 2024
We've looked at how to make a great PowerPoint cover slide. Soon, you can begin building amazing slides on your own.
Still need inspiration? These tips can serve as PPT title slide ideas. Let's check out five quick design tips that are sure to help you out:
Bold style is essential on your PowerPoint cover page. Remember, you've got one goal: capturing audience attention . Sharp, eye-catching design does exactly that on cover slide PowerPoint designs.

Premium templates built by creatives provide unmatched designs. They even help inspire you to do your very best work. I think of templates as a top source for PPT title slide ideas. And they're incredibly easy to customize, making you look like a PPT expert.
2. Create Your Own Layouts
PPT decks are really frameworks for your message. Inside the app, you've got the flexibility to customize every slide layout. That's never more important than on the first page of PPT presentations.
By adjusting layouts, you can show exactly what you want, where you want. It's the best way to create a memorable and unique PowerPoint cover page.
Ready to implement PPT title slide ideas of your own? Tweaking layouts helps you do just that. Learn how to customize PPT layouts with our quick tutorial:
3. Embrace Minimalism
Minimalism. It's a popular design aesthetic, and for good reason. It adds style without being overpowering or distracting. That's perfect for a PowerPoint cover page.

Try to build a cover showing only the essentials. These could be things like an image, the presentation title, a date, and your name. Be careful to avoid adding clutter: it's a quick way to lose your audience.
4. Add Kinetic Typography
You might not think of animated text. But it's actually a great way to grab attention and lock in audience focus on your title page in PPT. Thanks to PowerPoint, you can add these animations (called kinetic typography) easily.
Kinetic typography brings subtle, stylish text animation to any slide. It's ideal for the first page of PPT presentation layouts in need of a bit more energy.
Learn how to use kinetic typography in just 60 seconds here. It's yet another source of inspiration for PPT title slide ideas:
.jpg)
5. Use Industry-Specific PowerPoint Cover Slides
First impressions are key in a title page in PPT, and you'll make one with your PowerPoint cover page. So why use generic layouts if you can find something specifically suited to your needs?
My favorite PPT title slide ideas are situation specific. That means choosing PowerPoint title slides that match your purpose. Check out Pizzarena , for example. The designs are targeted at a pizza restaurant. That's far from the norm, but it will instantly resonate with your audience with eye-catching intro slide examples.

This might mean choosing a premium template built for your industry. Or, you might add your brand's colors, logos, and more. Either way, being specific and tailoring your cover slide to your needs is sure to impress.
5 Top PowerPoint Title Cover Slide Templates (For 2024 Presentations)
Premium templates from Envato Elements include stunning PowerPoint cover page designs. And remember, they're a top source for intro slide examples. Let's check out five of the very best PowerPoint templates with built-in PPT title slide examples:
1. VERA PowerPoint Template

Bold colors abound in this visually stunning PPT deck. With 55 unique slides, you're sure to find the perfect PowerPoint cover page. Also, inside is a custom icon set that's easy to work with. This title page in PowerPoint template is perfect for almost any project.
2. STYLE - Multipurpose PowerPoint Template V50

Style: it's in the name of this template, and for good reason . This is a perfect example of a sleek, minimalist PowerPoint cover page. Customize it in seconds, and with 4,000 slides to choose from, your options are almost unlimited. You're sure to find outstanding options for title page in PowerPoint designs!
3. IPSUM - PowerPoint

IPSUM offers a key part of a successful PowerPoint cover page. That's creative flexibility. Over 50 layouts are built into the pack. You can use those pre-built designs as PPT title slide examples! You'll also see custom infographics, icons, and more. Each slide element is completely editable.
4. Livy PowerPoint

Searching for a timeless, retro inspired PPT cover page? Livy has you covered. With 50 slides and resizable graphics, it's easy to adapt to your project needs. The included gallery slide makes for a perfect mosaic cover layout. It's yet another great example with PowerPoint title slide examples.
5. Conference PowerPoint Presentation Template

Last but not least is Conference, a modern PowerPoint cover page deck. Choose between multiple color themes and quickly add in your content. Plus, slides are pre-animated, saving you precious time as you build a title page in PowerPoint! Each slide is in full HD, helping them look great on large screens.
More Top PowerPoint Templates
PowerPoint templates give you a tremendous advantage when creating a presentation. Many of them even give you pre-built title page in PowerPoint designs. You've already seen options for PowerPoint cover pages in this tutorial, but these just scratch the surface.
Check out more of the top templates below. Many of these templates give you even more options for PowerPoint title slide examples:

Learn More About How to Use PowerPoint
PowerPoint is a fantastic app because it's easy to learn. But it also has many advanced features that you can use to build beautiful slides. The title slide designs and the template we used to build them are a great example of how easy it can be.
Still want to learn more about PowerPoint? One of the best resources for learning the app is our article, Ultimate Guide to the Best PPT . That guide and the tutorials below will help you build competence and present confidently.
.jpg)

The Top Source for the Best PowerPoint Cover Slide Templates (With Unlimited Downloads)
As we've shown, the title page of your PowerPoint presentation sets the tone. But you need to make sure that the rest of your presentation looks good too.
The best way to build a presentation is to use pre-built templates from Envato Elements. Elements has a massive library of PowerPoint presentation designs you can use. Each template has starter slides that you can just drop your own content into! The PowerPoint cover slides we feature are the fastest way to design.
Find PowerPoint Templates

The best part of Elements? It's an all-you-can-download creative buffet. With a single subscription, you've got access to all that Elements offers. It includes thousands of PowerPoint designs plus millions of total creative assets. That includes:
- stock photos
- so much more!

With Elements, finding the perfect assets is easier than ever. Use the tool to find PowerPoint title slide examples, and so much more with a bit of AI-assisted help. Elements now includes a powerful AI search tool ! With it, you can simply describe your own project needs.
With this prompt, Elements will deliver a curated list of assets from the vast library! It's an amazing way to save time and find the perfect content for your title page in PowerPoint. Join Elements and try it today!
Make Great Presentations ( Free PDF eBook Download )
We also have the perfect complement to this PowerPoint tutorial. It walks you through the complete presentation process. Learn how to write your presentation, design it like a pro, and prepare it to present powerfully.

Download our new eBook: The Complete Guide to Making Great Presentations . It's available for free with a subscription to the Tuts+ Business Newsletter.
Start Using PowerPoint Cover Pages Today
In this tutorial, you saw some of the best options for PowerPoint cover pages inside of premium templates. These files set the tone with the help of the first page of PPT presentations, presented perfectly. Choose one of these templates and get started now.
When you use these PPT title slide examples, you’re sure to wow your audience. You’ll kick off every presentation with a strong start! You’ll capture attention and keep everyone engaged. Try it today!
Editorial Note: This tutorial was originally published in August of 2019. It's been revised to make it current, accurate, and up to date by our staff—with special help from Andrew Childress .

Home Blog PowerPoint Tutorials How to Add Title Slides in PowerPoint
How to Add Title Slides in PowerPoint
Before you can begin showcasing your work or open up a topic for discussion before your audience, you can start with the title slide! Since a title slide template is the first impression of your slide deck , it is essential that you pay special attention to it.
What is a Title Slide?
A title slide contains the slide title, introduces the topic, and often includes other relevant details, such as the name of the presenter and the organization they are representing. The title slide is an important part of the presentation and is often good for marketing your ideas beforehand using creatively crafted layouts.
Slide Vs. Title Slide Layout
A title slide contains the title in a presentation deck. The layout of such a slide can contain a title, subtitle, and other relevant information. The title slide also often includes particular branding, such as the company’s logo or/and tagline.
Slide layout refers to not only the cover or title slide and other types. The layouts used in a presentation can differ according to the needs of the presentation. For example, other than the title slide, a presentation might have a picture layout, chart layout, dashboard layout, etc. The title slide will be the introductory slide of the presentation containing the presentation title .
How to Add Titles to Slides in Microsoft PowerPoint
If you’re making a presentation from scratch rather than using a PowerPoint template , you will notice that a title slide is added by default when you start a new PowerPoint presentation. You can also add it via Home -> New Slide .
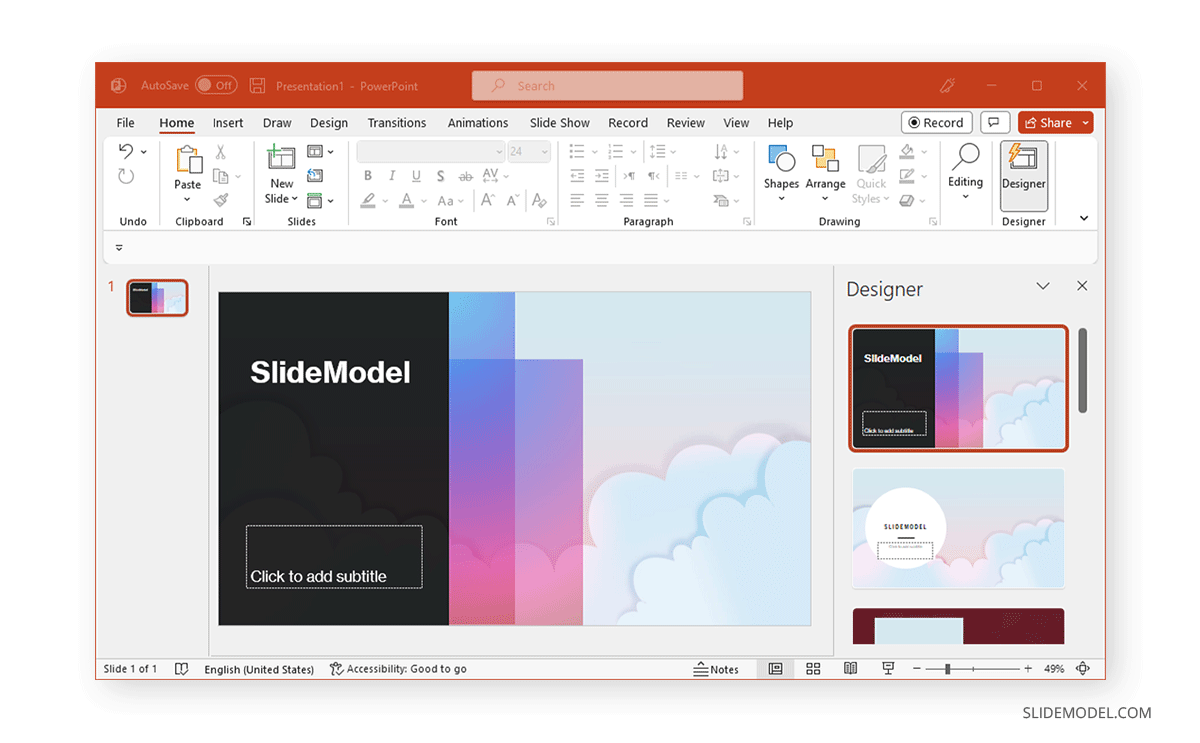
When making a title slide, you can also seek help from PowerPoint Designer, which provides suggestions based on the content of your slide, such as the text and layout of the slide you are using. To view suggestions regarding adding a slide title, click Designer from the Home tab and click on a design from the right sidebar to change your PowerPoint design.
How to Create an Effective Title Slide?
Merely adding a slide title isn’t enough to create a title slide that can help get the message across to the audience at the very start of the presentation. Below are some examples of title slides in PowerPoint that can help you design effective title slides. You might also be interested in our article about how to start a presentation .
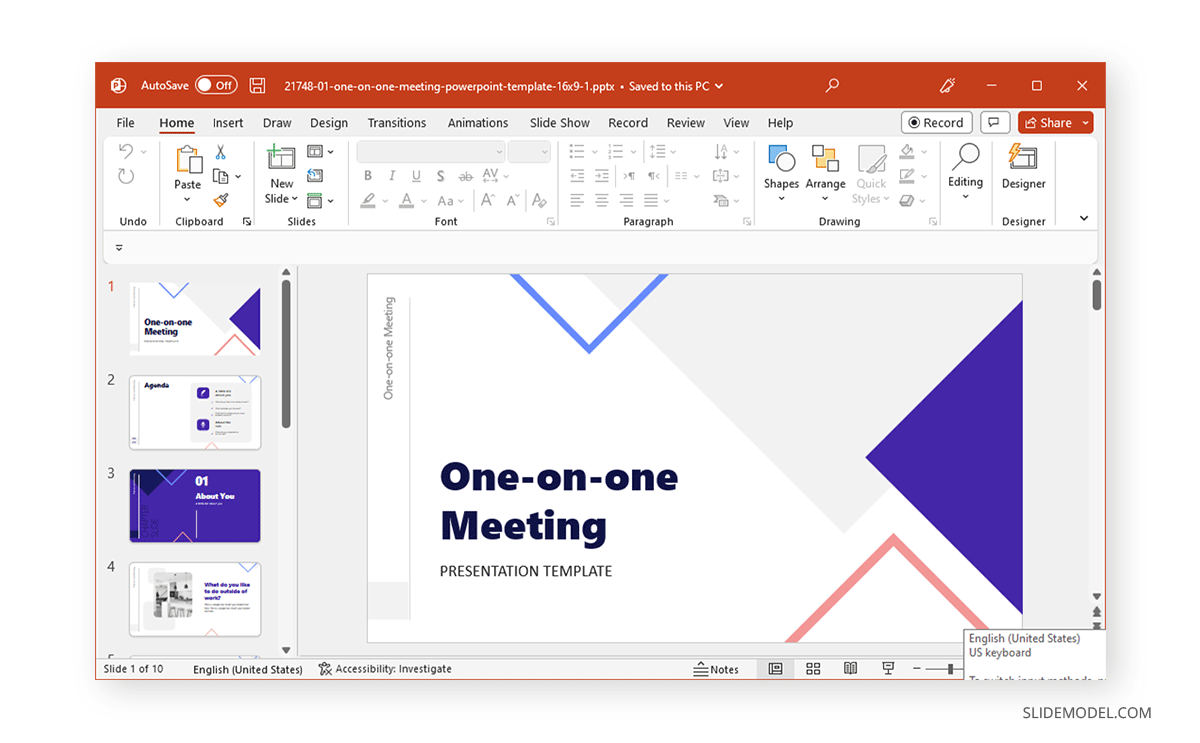
Title Slide that Provides Basic Information
The most common method for making a title slide is to use text that can easily explain the presentation context. If you are making a presentation for an interactive discussion, this can be mentioned in the title slide. Similarly, a slide deck to guide discussion for a one-on-one meeting can mention the context of the meeting.
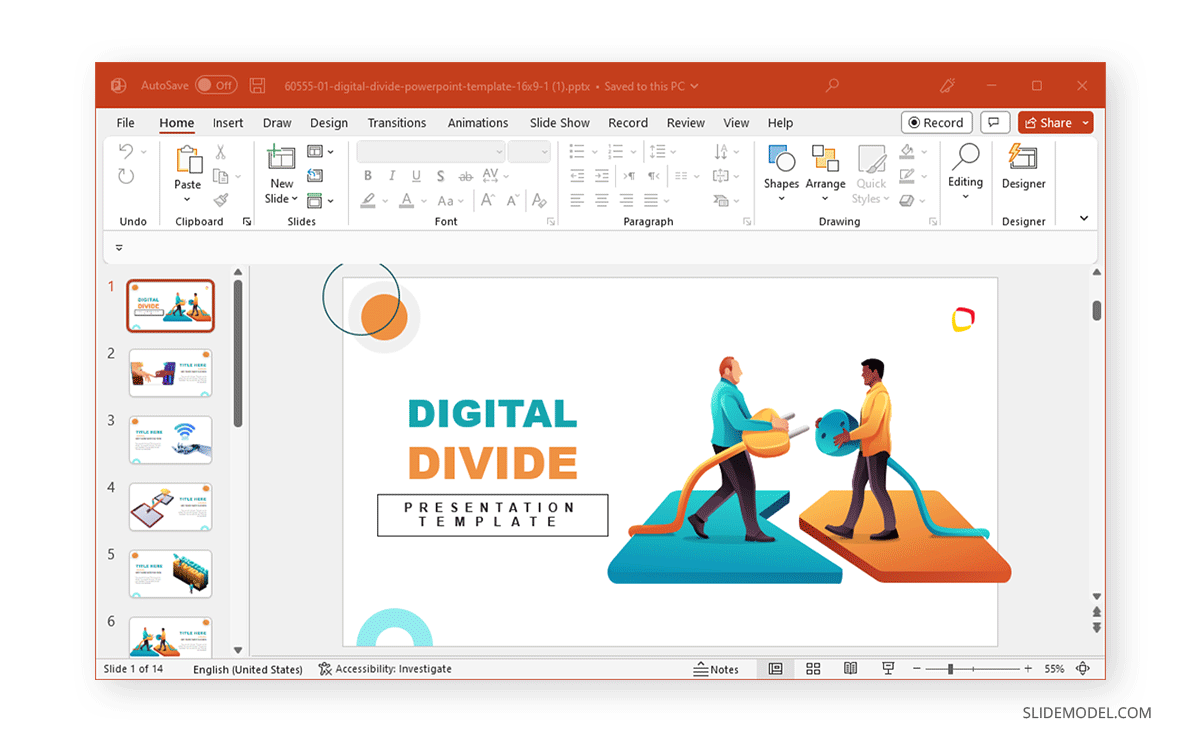
Title Slide that Visually Represents the Topic
A title slide can visually represent the topic. For example, the title slide shown below clearly elaborates on the topic under discussion, i.e., the digital divide. Such a title slide can help effectively deliver a message visually, even before the presenter elaborates on the topic.
Title Slide that Invokes Curiosity
Sometimes, making an ambiguous title slide is best to cause curiosity. This technique is often used to keep the audience interested and guess the presentation’s context. The technique can also be useful when aiming to persuade an audience during a presentation.
Related: See our article about the Zeigarnik Effect for presentations.
Zooming Title Slide
Zooming slides have been the hallmark of presentation platforms like Prezi. Some PowerPoint templates also come with a similar effect for title slides that can effectively add extensive information within the title slide to elaborate various details using a zooming UI. In such a case, the screen zooms to the area you click in slideshow mode to help you elaborate on the information before moving on to the next bit of detail.
Quiz Title Slide
If you run a quiz competition using PowerPoint or need to start your presentation with a burning question, using a quick title slide might be a good idea! Using quiz PowerPoint templates like the one below you can create a multiple-choice question as your title slide using quiz PowerPoint templates like the one below.
Final Words
A title slide is more important than many people might think. While many presenters skip through it in a rush, a title slide can be a good starting point to set the tone for the discussion ahead. Spending time making a title slide that can convey a message to the audience or cause curiosity can help make the presentation all the more interesting—enabling the presenter to positively influence the audience’s mood at the very start of the presentation.
Like this article? Please share
Design, Presentation Tips Filed under PowerPoint Tutorials
Related Articles
Filed under Google Slides Tutorials • August 6th, 2024
How to Use Google Slides Strikethrough Text
Customize your presentation slides by using Google Slides strikethrough and add a factor of humor, emphasize, or track changes in a truly visual method.
Filed under Presentation Ideas • July 17th, 2024
How to Convert a Text Document into a Presentation with AI
One of the biggest challenges for presenters is to summarize content from lengthy reports, academic papers, or any other kind of written media in an informative and concise way. Rather than losing countless hours going over and over the same text, we can speed up the process thanks to the virtues of artificial intelligence. In […]

Filed under Google Slides Tutorials • July 16th, 2024
How to Make a Google Slides Presentation Look Good
Polish your presentation slides with these 10 tips by design professionals. Learn how to make Google Slides look good now!
Leave a Reply

How to easily make an AWESOME first slide in PowerPoint?
By: Author Shrot Katewa

A good first impression can have a lasting impact. Thus, having a good design for your first slide is important. We’ve seen that people often simply put the title of the presentation as a first slide. I personally dislike this the most. It just shows that the person creating the presentation was simply not interested in it (even though that may not necessarily be true).
Thus, knowing how to create a good first slide is as important if not more as knowing how to create the rest of the presentation. The best part is – you can easily create an awesome first slide for your presentation in minutes in a few quick and easy steps. Obviously, if you have the time at hand, you can easily spend an hour or two making that perfect first slide! In this post, we take a look at how to easily create a first slide with a few examples of actual designs that we have created for our clients.
1. What is the first slide of a PPT presentation called?
The first slide of a presentation is called a “Title slide” or a “Cover slide” . This slide often contains the title of the presentation and hence the name title slide. It is also often referred to as the “Opening slide” of the presentation. The title slide is often the slide that is displayed on the screen before you start your presentation. Thus, it is important to have a title slide that not only looks good but also shares relevant information about your presentation.
2. What content should be included on the first slide of the PPT presentation?
A title slide or the cover slide does not need too much content. The purpose of the title slide is really to give an indication of what the presentation is all about. Thus, an ideal title slide should contain nothing more than –
- Presentation title
- Date of the presentation
- Presenter’s name and designation
It is not necessary to have all the above three pieces of information on a cover slide. Do keep in mind that not all cover slides are the same and what content is displayed on the cover slide can be organisation specific. An organisation may have a preference or a fixed structure for the content that needs to be put on a cover slide. This may vary from the above structure.
3. How to easily design a beautiful first slide in minutes?
As I mentioned earlier, having a good first slide can have a lasting positive impact on your audience. Thus, it is important to create a good design for your first slide. There are several ways you can design the cover slide. Let’s look at some of the easiest ways you can create a beautiful cover slide –
Method 1 – Using PowerPoint’s “Design Ideas” functionality (for beginners)
I must admit, PowerPoint’s “Design Ideas” functionality has great potential. In fact, we at OwlScape were planning on creating a similar plugin for PowerPoint users before Microsoft introduced this feature. This functionality is not just great for beginners, but also at least a must try for intermediate level users too. Designers from OwlScape also at least check out the functionality every once in a while especially when we hit a creative bloq.
It is really easy to work with. In just a couple of clicks and a few minutes, you can make your title slide look completely different –
To do this, all you need to do is put some text on your cover slide and use the “Design Ideas” functionality of PowerPoint. For example, you can write the title and subtitle of your presentation.
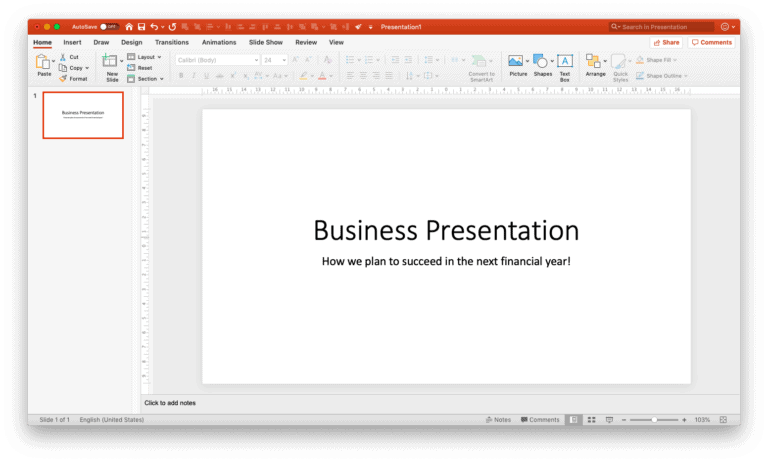
Next, click on the “Design” tab on your Menu bar. On the ribbon under the design tab, look for “Design Ideas” feature. It is normally on the far right of the screen on the ribbon. Click on it, and wait for a bit.
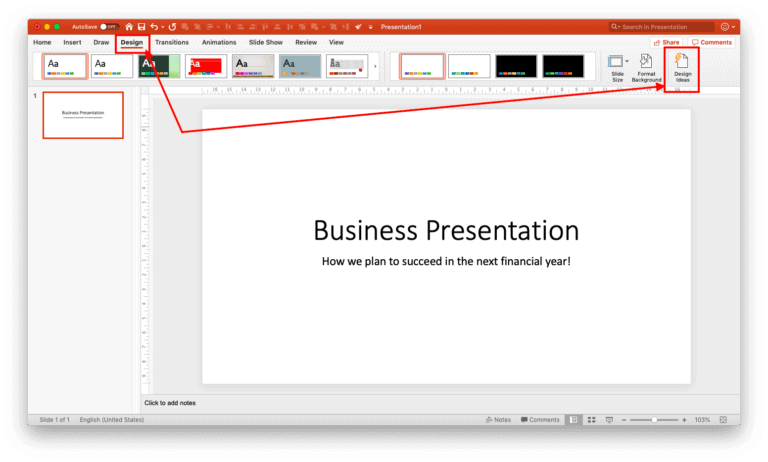
In a few seconds, PowerPoint will automatically throw a few ways in which you can design your title slide. You can choose the design you like, and repeat the process to get more results.
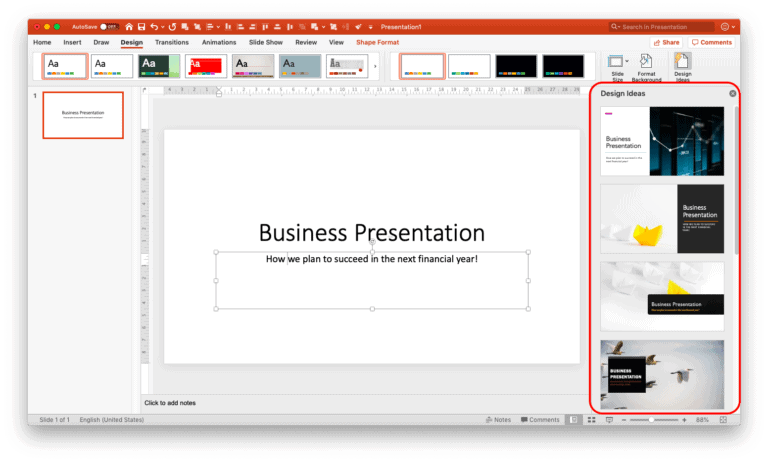
If you are unable to see any design ideas or you get an error, you could close the error result by clicking on the close button marked with “X” next to Design Ideas. Then, try clicking in any of the text box on the slide and click on “Design Ideas” again. A few attempts will surely give you some interesting results.
There are a few drawbacks though. These are as follows –
- The results are not consistent . If you happen to delete the slide and try to recreate using the exact same process, the result may be different. This can be both good and bad 🙂
- Editing the design of the suggested slide may not be easy for beginners – when you need to make some changes to the chosen design option, it doesn’t happen directly. You will need to work with the master slides in order to make the design changes. This may seem daunting especially if you are a beginner.
- Sometimes, it just doesn’t work – Even though you may have created a slide using the same content before, sometimes when you try to recreate using the same content, it may simply fail to showcase any ideas. In such an event, we would advise you to click on the text box or an image on your slide and try again by clicking on the Design Ideas option.
- Available for Office 2016 onwards – If you are a PowerPoint user using an older version of Microsoft Office, you may not be able to easily access this functionality. Having the latest PowerPoint version can be of great help!
One thing to note is that the “Design Ideas” option can be used not just for the cover slide, but also for other slides. However, I would advise resisting the temptation of using it for every single slide. 🙂
Method 2 – Using shapes to create an interesting cover slide (for intermediate users)
One other way of having an interesting cover slide is by using the shapes in PowerPoint. Let’s look at the following example –
If you look at the above example carefully, you’ll notice that we’ve only added a shape to the already existing title and the subtitle in the “After” slide. Simply adding a shape, a logo and aligning the text can alter the look of the slide drastically.
There are many ways you can add a shape to the slide. My favourite method is to add a horizontal or a vertical “Trapezoid/ trapezium” (a quadrilateral shape with one pair of parallel sides). A trapezoid shape allows me to have enough space to write the title of the slide and some more content.
To create this shape, you can follow the below steps –
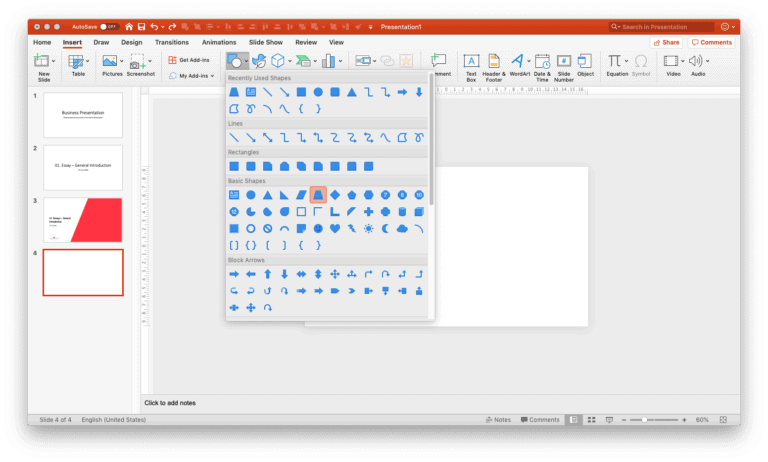
On the menu bar, click on “Insert” and then click on “Shapes”. Under the basic shapes option, select the trapezium shape. Next, create the shape on your slide.
Make sure that the size of the trapezium is good enough to cover about ⅔ parts of the slide. Also ensure that the parallel sides of the trapezium touch the top and bottom part of the slide. Now all you need to do is add the title and subtitle, along with the logo to create your cover slide.
Similarly, you can also use the trapezium vertically. You can also use various types of shapes on your cover slide. The possibilities are literally endless!
Method 3 – Using shapes with images to create an awesome cover slide! (for advanced users)
If you are still not satisfied with your cover slide, there are several other ways you can make it look even more impressive. The easiest way to take it to the next level is to use images in combination with the shapes.
Let’s look at a few examples –
Combination cover slide design example – 1

In the above design, a shape has been created in the background using a freeform tool. Next, two appropriate images have been identified and put in front of the shape. All this has been kept predominantly to the right side of the slide allowing space to write the title, subtitle and the other relevant information on the left.
Combination cover slide design example – 2

In this example, we’ve used one corner of curved rectangle shape to create an interesting design. Two copies of the same shape have been considered. The one below is filled with a colour and tilted at a slight angle. The one above has an image inserted in the shape.
Combination cover slide design example – 3
In the above example, a combination of several shapes and images are used to create a visually pleasing design. Obviously, this may not be something that a beginner can create right of the bat. But the reason we put this design as an example is because barring the design skills (knowing what shape to include and where), creating this slide is not as advanced as you might think. This slide has been created by only using shapes and image elements along with the logo and text. The purpose of using this as an example was to showcase the endless possibilities on how a seemingly complex cover slide can be made by merely using basic shapes and images.
4. How to find images for the first slide of your presentation?
Whether you are using a combination of images and shapes or simply using an image on your title slide, it is important to identify a good image that resembles the topic of your presentation. Consider the following example –

If you’ve been following along, I’m sure you would have noticed by now that the above title slide has been created using a combination of images and shapes. Again, the design can be easily created using shapes and image elements. However, part of the reason that makes this slide look good and relevant to the presentation is the choice of image. Since the presentation is for a corporate organisation, choosing an image that resembles a corporate environment would be relevant.
Take a moment to scroll up and notice the other cover slide examples that I shared above.
The cover slide example 1 was designed for a presentation on education. Thus, choosing an image that represents education effectively communicates to the audience that the presentation is something to do with education even without the word “education” in the title or the subtitle or anywhere on the slide (Don’t resist, go ahead and have a look at the slide again! 🙂 )
Likewise, example 3 uses a mobile device in the title slide giving an indication that the product being talked about in the presentation is likely going to be an app.
Thus, choosing an appropriate image is important as it subtly communicates the message to the audience.
Finding the images for your presentation can take some time. You can use Google to see a few references on what type of images can be used. Avoid the temptation of using Google images directly on your presentation as this can violate copyright laws. We wrote a detailed post on where to find and how to use images for your presentation (link – https://owlscape.in/can-i-use-google-images-for-my-presentation/ ). Be sure to check it out!
I’m sure by now you’ve noticed a few different ways you can create a good title slide for your presentation. I hope this post helps you to think out of the box while creating the title slide of your next presentation. I also hope that going forward you will surely give enough focus on creating an impressive first slide even if you only have a few minutes.
If you’re struggling while creating your next title slide or your presentation, simply drop us an email on [email protected]

Title a slide
There are multiple ways to add titles to your slides in PowerPoint. Use the Layout option to create a standalone title slide or to add a title to a slide that contains other text. You can also use the Outline view or the Accessibility ribbon to create and update the titles of your slides.
Select a heading below to open it and see the detailed instructions.
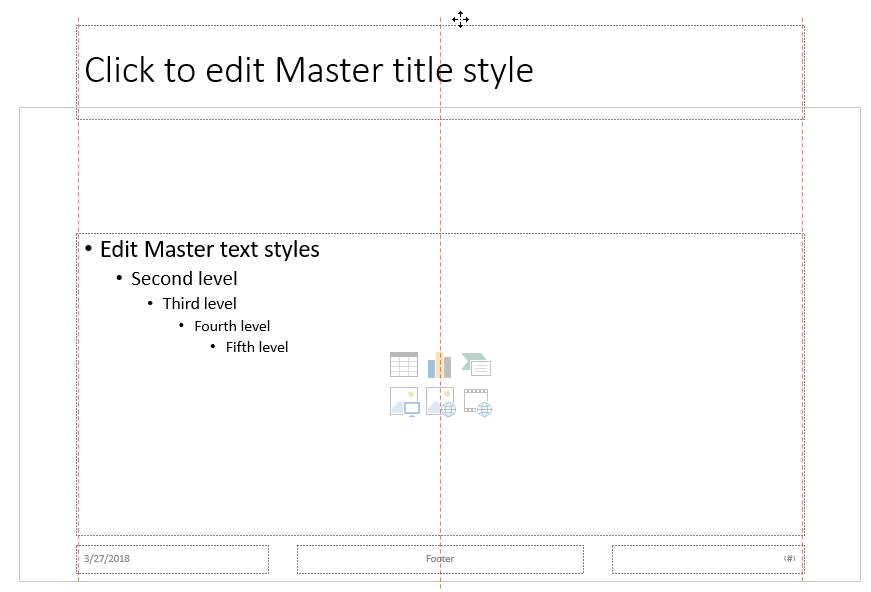
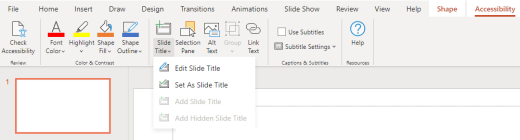
Use the Accessibility ribbon to title a slide
You can use the Accessibility ribbon to add or edit slide titles and to make sure your slides are accessible to everyone.
Select Review > Check Accessibility . The Accessibility ribbon is displayed, and the Accessibility pane opens to the right of the selected slide.
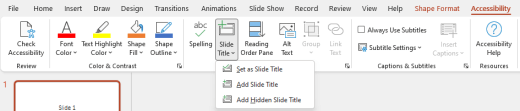
Select one of the following options:
Note: The available options depend on whether a title placeholder exists or not, and what type of element is selected on the slide.
To move the cursor to the title placeholder, select Edit Slide Title .
To add a title placeholder to the slide and move the cursor to the placeholder, select Add Slide Title .
To add an off-slide title placeholder and move the cursor to the placeholder, select Add Hidden Slide Title . Because the title is positioned off-slide, it will be invisible during a slide show, but the title is available to help users navigate or select the slide.
If there is no title placeholder on the slide, to let the Accessibility Checker select the text box or shape that seems most like a title, select Set as Slide Title . This makes the selected object your slide title. If there is another text box or shape you want to use as the title, select the object, and then choose this option. Only objects with text that aren't in groups can be made into a title.
Selecting the Slide Title button without expanding the dropdown menu does the following:
If an object that can be set as the title is selected on the slide, that object is set as the slide title ( Set as Slide Title ).
If there is a title, but no object is selected, the cursor moves to the title placeholder ( Edit Slide Title ).
If there is no title and no object is selected, a title placeholder is added and the cursor moves to the placeholder ( Add Slide Title ).
Type or edit the slide title.
Tip: To review your presentation for missing or duplicate slide titles, run the Accessibility Checker, and then check the Accessibility pane to find them.
Use the Layout option to title a slide
You can name or rename a slide by using a slide layout that has a title placeholder .
Select the slide whose layout you will change so that it can have a title.
Click Home > Layout .

Select Title Slide for a standalone title page or select Title and Content for a slide that contains a title and a full slide text box. Many other layout options include titles, too. Pick the one that’s best suited for your presentation.
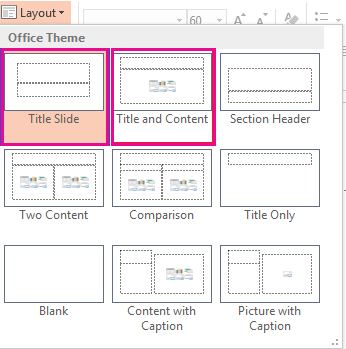
Select the Click to add title text box. Enter your title for that slide.

Use Outline view to title a slide
You can also create a slide title in Outline view. This view also shows the titles for any other slides in your presentation.
Click View > Outline View .
A slide without a title will have no text to the right of the slide number.
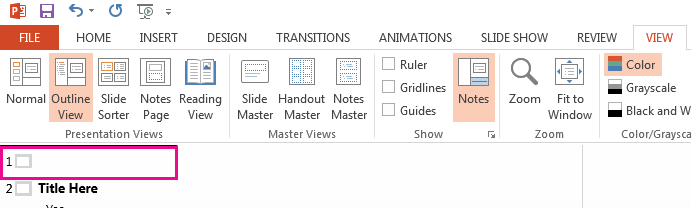
If your slide already has a title, it appears next to the slide number.
Click to the right of the slide number.
Type your new title here, or update an existing slide title. Your text will appear on the slide as you enter it.
Tip: You can use Outline view as your notes when you give a presentation.
Put a title on a slide, but make the title invisible
You can position a title off the slide. That way, the slide has a title for accessibility or sorting reasons, but you save space on the slide for other content.
On the View tab, select Zoom and then lower the zoom percentage to about 50% so that the margins outside the slide are visible.
Type a title in the Title placeholder box.

Drag the Title placeholder upward or downward and then drop it outside the slide boundary.

You can confirm that the title will be invisible during a slide show by selecting Slide Show > From Current Slide .
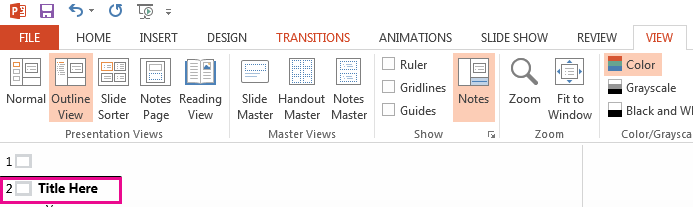
Systematically hide slide titles
If you want all or many of your slide titles to be hidden, use Slide Master view to achieve it. Duplicate the slide layout for which you want to have hidden titles. Then on the duplicate layout, move the title placeholder off-slide. Then apply the new layout to the appropriate slides.
For example:
On the View tab of the ribbon, in the Master Views group, select Slide Master .
In the slide thumbnail pane on the left side of the PowerPoint window, right-click a slide layout (such as Title and Content Layout ) that you want to alter and choose Duplicate Layout .
Select the duplicated layout.
Select the title placeholder, drag it upward, and drop it outside the boundary of the visible slide.
If PowerPoint doesn't allow you to drag the placeholder that far, use View > Zoom to make the slide surface area appear smaller so that there is adequate room to move the placeholder fully off-slide.
Close Master view and return to Normal view.
Select a slide whose title you want to hide. Right-click it, and apply the "hidden-title" slide layout that you just created.
The title moves to an off-slide position, but it still exists. You can see the title of the slide by switching to Outline view.
Put the same title on every slide
If you want the same title on every slide, you may be thinking of what PowerPoint calls a footer . For instructions on putting footers on your slides, see Insert or change footers in PowerPoint slides .
Why slide titles are important
Having slide titles is valuable for:
Accessibility A visually impaired person that uses a screen reader relies on the slide titles to know which slide is which.
Helping various PowerPoint features work correctly Design Ideas, Apply Layout, and Reset Slide work better on slides that have titles. Insert Hyperlink, Insert Zoom, and custom shows all refer to slides by their titles.
PowerPoint expert Geetesh Bajaj has an article on his site about Hiding Slide Titles in PowerPoint .
You can name or rename a slide by using a slide layout that has a title placeholder
Tip: You can use Outline view as your notes when you give a presentation.
In the slide thumbnail pane on the left side of the PowerPoint window, right-click a slide layout (such as Title and Content Layout ) that you want to alter, and choose Duplicate Layout .
If there is no title placeholder on the slide, to let the Accessibility Checker select the text box or shape that seems most like a title, select Set as Slide Title . This makes the selected object your slide title. If there is another text box or shape you want to use as the title, select that object, and then choose Set as Slide Title . Only objects with text that aren't in groups can be made into a title.
If there is no title placeholder on the slide, to let the Accessibility Checker select the text box or shape that seems most like a title, select Set As Slide Title . This makes the selected object your slide title. If there is another text box or shape you want to use as the title, select that object, and then choose Set As Slide Title . Only objects with text that aren't in groups can be made into a title.
If an object that can be set as the title is selected on the slide, that object is set as the slide title ( Set As Slide Title ).

You can confirm that the title will be invisible during a slide show by selecting Slide Show > From Current Slide .

Need more help?
Want more options.
Explore subscription benefits, browse training courses, learn how to secure your device, and more.

Microsoft 365 subscription benefits

Microsoft 365 training

Microsoft security

Accessibility center
Communities help you ask and answer questions, give feedback, and hear from experts with rich knowledge.

Ask the Microsoft Community

Microsoft Tech Community

Windows Insiders
Microsoft 365 Insiders
Was this information helpful?
Thank you for your feedback.
Byte Bite Bit
What is a Subtitle in PowerPoint: Key Uses and Best Practices
Picture this: You’re in the middle of an engaging PowerPoint presentation, and you want to ensure everyone understands your speech perfectly. That’s where subtitles come into play. Subtitles in PowerPoint are real-time captions that appear on your slides, translating your spoken words into text. This can be a game-changer for making your presentations more accessible and engaging.

Using subtitles in PowerPoint can enhance your presentation by reaching a wider audience, including non-native speakers and people with hearing impairments. By integrating this feature, you can break language barriers and make your talk more inclusive. I remember a time when I used this feature during an international conference. It was a hit, ensuring that all attendees, regardless of their native language, could follow along seamlessly.
Think of subtitles as your silent assistant, working behind the scenes to ensure clarity and comprehension. It’s like having a universal translator right there on your slide. This tool not only makes your presentations more understandable but also demonstrates your commitment to accessibility and inclusivity. So, ready to make your next PowerPoint presentation a standout? Let’s explore how you can set up and use this fantastic feature.
- 1.1 Enabling Subtitles in PowerPoint
- 1.2 Customizing Caption Appearance
- 1.3 Setting Up Microphone and Audio Options
- 2.1 Utilizing Real-Time Translation and Captioning
- 2.2 Leveraging Accessibility Options
- 3 Technical Requirements and Setup
- 4.1 Designing Presentations for All Audiences
- 4.2 Managing Subtitles During Live Events
Mastering PowerPoint Subtitles and Captions
Setting up subtitles and captions in PowerPoint enhances accessibility and inclusivity. Here’s how to enable, customize, and manage audio options effectively.
Enabling Subtitles in PowerPoint
To enable subtitles in PowerPoint, open your presentation and navigate to the “Slide Show” tab. On the right side of the ribbon, click on “Subtitle Settings” . From the dropdown list, select both the spoken language and subtitle language.
Ensure you have the latest version of PowerPoint as this feature is available with Microsoft 365, PowerPoint for the web, and other recent versions. Toggle subtitles during your presentation by using the “Toggle Subtitles” button or by pressing J on your keyboard. This quick setup can make a world of difference in making your presentation accessible.
Customizing Caption Appearance
Customizing the appearance of your captions can greatly improve readability. You can adjust the font, size, color, and background of your subtitles by going to the Slide Show Settings . Click on “Subtitle Settings” and select “Subtitle Options” .
Experiment with various combinations to find the most visually appealing and readable format. Aim for high contrast between text and background to ensure clarity. You can choose different positions for subtitles on your slides, such as the top or bottom of the screen. This customization will help cater to diverse viewing needs, making your presentation more engaging and user-friendly.
Setting Up Microphone and Audio Options
To ensure accurate real-time captioning, setting up your microphone and audio options is crucial. In PowerPoint, go to the File tab and select Options . Under Audio Settings , choose your preferred microphone.
Ensure that the microphone is properly connected and functioning. You might want to test your setup with a few practice runs to check the clarity of the captions generated. Make sure you speak at a moderate pace and articulate words clearly. Implementing these steps will enhance the accuracy of captions, making your presentations more professional and inclusive.
Advanced Features for PowerPoint Presentations
In PowerPoint, leveraging advanced features such as real-time translation and enhanced accessibility options can significantly enhance both audience engagement and the inclusivity of your presentations.
Utilizing Real-Time Translation and Captioning
One outstanding feature in PowerPoint is real-time translation and captioning, available in Microsoft 365 versions. This allows presenters to transcribe spoken words automatically and translate them into subtitles on the screen.
Real-time translation: Helps break language barriers by providing instantaneous translations in over 60 languages. Simply enabling the “Always Use Subtitles” option can make your presentations more globally accessible.
For instance, spoken English can be immediately translated into Spanish, French, or any other supported language. You can toggle subtitle settings directly from the Slide Show tab. This not only transcribes spoken language but also provides accurate translations, bridging the communication gap and making your message clear to a wider audience. Plus, the automatic transcription is a game-changer for including participants who may have hearing impairments or prefer reading.
Leveraging Accessibility Options
PowerPoint’s accessibility options ensure that your presentations are inclusive for all audiences. These features include captioning options, keyboard shortcuts, and compatibility with screen readers.
Using live captions can make your slideshow accessible to those with hearing difficulties. Additionally, setting up subtitles through the “Slide Show” tab enhances inclusivity by displaying the spoken language as written text.
| Automatically transcribes spoken words into captions. | |
| Allows customization of spoken and subtitle languages. |
Whether you’re presenting on Windows or Mac, these accessibility features are designed to create a more inclusive environment. Enabling these options is straightforward and can be done by checking the “Always Use Subtitles” box, ensuring your presentation not only reaches a broader audience but also meets diverse accessibility needs.
Technical Requirements and Setup
To get started with subtitles in PowerPoint, you’ll need a few technical basics. First, ensure you have an internet connection . This is crucial if you plan to use online features like automatic translations or updates.
| Office 365 or PowerPoint 2019 and newer | |
| Windows 10 or newer | |
| Built-in or external |
Open your PowerPoint presentation and head to the Slide Show tab. Click on Subtitle Settings . From here, you can configure your subtitles by selecting the spoken language and the subtitle language.
To enable subtitles automatically every time you present, check the box next to Always Use Subtitles . It’s like having a trusty assistant, ensuring your audience captures every word you say.
You can even toggle subtitles during your presentation with shortcut key J . This flexibility allows you to turn subtitles on or off as needed.
Make sure your microphone settings are properly configured. If your mic isn’t picking up your voice accurately, you might end up with strange and funny subtitles!
I love how easy it is to navigate these settings. PowerPoint has certainly made it user-friendly.
Best Practices for Effective Presentations
Creating an accessible and engaging presentation requires careful design and management. From thoughtful layouts to real-time subtitle adjustments, each detail enhances the audience’s understanding and engagement.
Designing Presentations for All Audiences
When designing PowerPoint presentations, I always prioritize inclusivity. Using high-contrast colors ensures readability for everyone, including those with visual impairments. Large, clear fonts are essential; they help people in the back of the room—and those with visual challenges—read with ease.
To cater to diverse audiences, I use multilingual support. This is particularly helpful when dealing with language barriers. I often embed subtitles in multiple languages by leveraging PowerPoint’s subtitle settings. Consistent use of bullet points and visuals also clarifies key points without cluttering the slides.
Managing Subtitles During Live Events
Subtitles in PowerPoint are invaluable during live events. They make the presentation more accessible and inclusive. I usually toggle subtitles on using the handy shortcut key ‘J’. This feature is fantastic for live captions.
Positioning is critical. I sometimes relocate subtitles during a presentation to ensure they don’t cover important content. Adjusting the settings in Presenter View allows me to manage this on the fly. Real-time captions help bridge the gap for those who are hard of hearing or when audio quality is poor.
| **Settings** | **Shortcut Key** | **Benefit** |
| Subtitle Position | N/A | Avoids covering vital content |
| Toggle Subtitles | J | Quick on/off control |
Related posts:
- How to Embed a YouTube Video in PowerPoint: Step-by-Step Guide
- How to Do a Voice Over on PowerPoint: Easy Steps for Professionals
- How to Make an Org Chart in PowerPoint: A Step-by-Step Guide
- How to Embed Excel into PowerPoint: Simplify Data Visualization
- How Is a Chart from Microsoft Excel Added to a PowerPoint Presentation? Step-by-Step Guide
- How to Present PowerPoint in Teams: A Step-by-Step Guide for Professionals
- How to Create a Multilevel List in PowerPoint: Step-by-Step Guide
- PowerPoint Cannot Insert a Video from the Selected File: Solutions and Workarounds
- How to Make a Picture Black and White in PowerPoint: Quick Guide
- How to Remove Page Numbers in PowerPoint: Step-by-Step Guide for All Versions
- How to Make a Quiz in PowerPoint: Step-by-Step Tech Guide
- How to Star a Slide in PowerPoint: A Step-by-Step Guide
Leave a Comment Cancel reply
Save my name, email, and website in this browser for the next time I comment.
Critical PowerPoint Shortcuts – Claim Your FREE Training Module and Get Your Time Back!

PowerPoint title slide explained (it’s not what you think it is)
- PowerPoint Tutorials
- November 29, 2023
What is a title slide in PowerPoint, and is it the same thing that you think it is? This is a tricky topic if you are an analyst, associate, or keeper of your team’s PowerPoint presentation, when it comes to managing the headers and footers in your presentation.
That’s because the Header and Footer dialog box (pictured below), has the following option that will throw you for a loop.
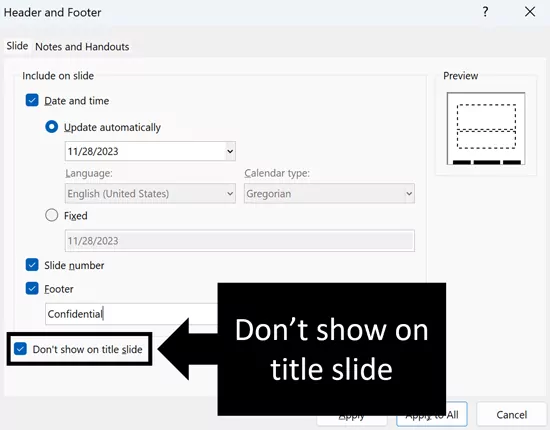
If you don’t understand what PowerPoint considers as the title slide of your presentation, it is easy to accidentally mess up the headers and footers in your presentation, creating an embarrassing disaster that you will be stuck trying to troubleshoot and fix.
This can be the same issue you find in your client decks, so it’s good to know how to fix this.
Table of Contents
What is a title slide.
A title slide in PowerPoint (as humans think of it as) is either the slide that is named “title slide” in your presentation, or the slide that looks like a title slide. Common elements include a large title, a subtitle, some kind of graphical element, etc.

This is where you type the title and subtitle of your presentation, add your name, your presentation topic, the date and time, or whatever other elements you want to display on the first slide of your presentation. Typically, this is the slide you put up first to let your audience know they are attending the correct meeting.
Unfortunately, this is not how PowerPoint defines it. Read the next section to see why your instincts might lead you astray.
What PowerPoint considers your title slide
The title slide in PowerPoint (as PowerPoint thinks of it as) is simply the first slide layout of your presentation. This is true whether it is named “title slide” or whether it looks like a title slide. PowerPoint is just a program. So, whatever the first slide layout is in your presentation is, is what PowerPoint defines your title slide as.
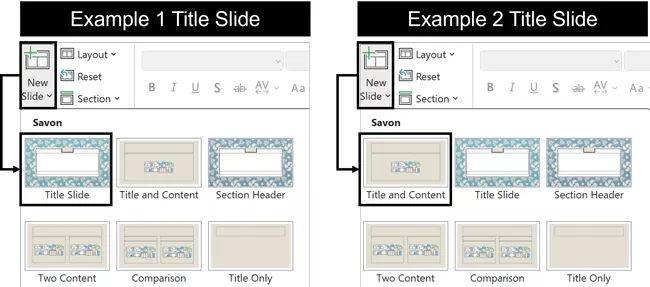
Notice in the picture above, that there is a different slide in the first position of otherwise the same exact PowerPoint template. In both cases, the first slide is what PowerPoint uses as the title slide when determining where to place your headers and footers.
The problem with example 2 in the picture above, is that if you select “don’t’ show on title slide” in the Header and Footer dialog box, then none of your slide numbers, date and time, and/or your footers will display on the Title and Content layout in your presentation. I guarantee this is not what you want.
Arranging a layout so it becomes your title slide
If the wrong slide is in the first position of your PowerPoint presentation, you will need to navigate to the Slide Master view to fix it. In short, all you need to do is move your actual title slide into the first position on your slide master, so that both you and PowerPoint are on the same page.
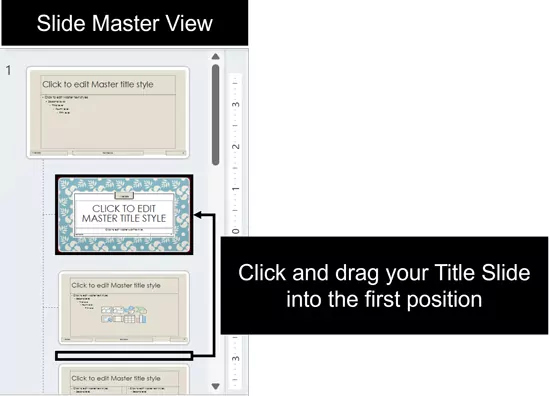
To rearrange a slide to be your title slide in PowerPoint, simply:
- Click the View tab
- Select Slide Master View
- Click and drag your desired Title Slide into the first position
By dragging your preferred slide into the first position on your Slide Master, automatically designates it as the Title Slide in PowerPoint. That means you won’t have any header or footer issues moving forward.
NOTE: For help adding and troubleshooting slide numbers in PowerPoint (which can be tricky), see our guide on adding slide numbers to PowerPoint .
Title slide examples
If you are looking for inspiration for your own presentations, below are three different examples from the default PowerPoint templates that come with the Microsoft Office Suite. All these templates include color variations too, giving you a variety of options to work with.
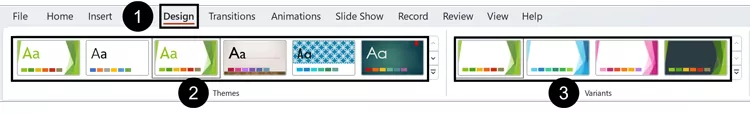
To find these default PowerPoint templates (or themes) and their color variations, simply:
- Click the Design tab
- Select a Theme
- Choose a Variant of that theme
The variant options represent different color combinations and/or design elements of the base theme you chose, giving you a different look and feel for your title slide, divider slides, and the other content container slides in your presentation.
PowerPoint Template Help: If you don’t want to use the default PowerPoint templates, you can buy a professional PowerPoint template online ( see my guide here ). Alternatively, if you are willing to invest the time, you can create your own PowerPoint template from scratch ( see my guide here ).
1. Integral template
The integral template focuses on a blue and white design element at the top, with the title and subtitle of your presentation at the bottom of the slide. That said, you can add any other elements you like. This template also includes seven other color options including green, red, yellow, solid colors etc.
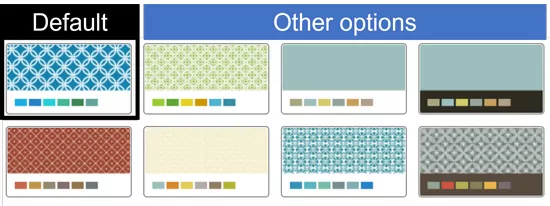
2. Circuit Template
The Circuit PowerPoint template includes a blue gradient background, with some circuit like design elements on the left side. The left side of your title slide is a great place to add your own company branding, or elements from your industry. This template includes three variations, including green, red, and black.

3. Vapor Trail Template

The Vapor Trail PowerPoint template is a bit more artsy than the other two. This includes wavey colored lines, giving it a more modern and artistic look and feel. Like the other templates, the default title slide only includes a title and subtitle, but you can add any other elements you need for your own presentation. The Vapor Trail template also includes three additional colors: green, pink, and orange.
You now know more about what a title slide is than most professionals (even those that have been using PowerPoint for years). This is a nuance of PowerPoint that specifically relates back to getting your headers and footers to properly display throughout your PowerPoint presentation. So, if you are an investment banking analyst, associate, or that is constantly updating large decks, this is something you will want to properly nail dwon.
If you enjoyed this article and want to learn more about our PowerPoint training seminars, courses, and other useful Powerpoint tutorials that will get you to Happy Hour, visit us here .
🔒 Unlock the PowerPoint Shortcuts Trusted by Industry Leaders KKR, American Express, HSBC, and More!
Join over 114,880 professionals from diverse fields including consulting, investment banking, advertising, marketing, sales, and business development who have supercharged their PowerPoint game with our proven methods.
✅ Customize compelling presentations effortlessly.
✅ Master time-saving techniques for faster deck creation.
✅ Boost your career prospects with top-notch PowerPoint skills.
Get FREE access to the Critical PowerPoint Shortcuts module of our premium training course by entering your name and email below.
DISCLAIMER: PC Users Only!
We respect your privacy and will keep your info safe and confidential.
About The Author
Popular Tutorials
- How to Strikethrough Text (l̶i̶k̶e̶ ̶t̶h̶i̶s̶) in Word, Excel & PowerPoint
- How to Make Animated Fireworks in PowerPoint (Step-by-Step)
- Strikethrough Shortcut (l̶i̶k̶e̶ ̶t̶h̶i̶s̶) for Word, Excel & PowerPoint
- How to Create a Flash Card Memory Game in PowerPoint (Like Jeopardy)
- Keyboard Shortcuts Not Working: Solved
PowerPoint Tutorial Categories
- Strategies & Opinions
- Shortcuts & Hacks
- Presentation Design
- Pictures, Icons, Videos, Etc.
- New Features
- Miscellaneous
- Charts & Data Viz
We help busy professionals save hours and gain peace of mind, with corporate workshops, self-paced courses and tutorials for PowerPoint and Word.
Work With Us
- Corporate Training
- Presentation & Template Design
- Courses & Downloads
- PowerPoint Articles
- Word Articles
- Productivity Resources
Find a Tutorial
- Free Training
- For Businesses
We help busy office workers save hours and gain peace of mind, with tips, training and tutorials for Microsoft PowerPoint and Word.
Master Critical PowerPoint Shortcuts – Secure Your FREE Training Module and Save Valuable Time!
⌛ Master time-saving expert techniques.
🔥 Create powerful presentations.
🚀 Propel your career to new heights.
We value your privacy – we keep your info safe.
Discover PowerPoint Hacks Loved by Industry Giants - KKR, AmEx, HSBC!
Over 114,880 professionals in finance, marketing and sales have revolutionized their PPT skills with our proven methods.
Gain FREE access to a full module of our premium PowerPoint training program – Get started today!
We hate spam too and promise to keep your information safe.
You are currently viewing a placeholder content from Facebook . To access the actual content, click the button below. Please note that doing so will share data with third-party providers.
- Presentation Design
- Report Design & Content Research
- Motion Graphics
- Interactive Design
- Design with AI

7 PowerPoint Title Slide Examples to Start Your Presentation Right

PresentationPanda.com is now proudly owned by INK PPT . We aim to enrich and expand upon the valuable content previously provided by PresentationPanda.com . This blog will deliver even deeper insights, comprehensive guides, and innovative strategies to elevate your presentations to new heights.
TL;DR: Your PowerPoint title slides are the gateway to your presentation, setting the stage and making the first impression on your audience. It's essential to design these slides meticulously to capture attention right from the start. A well-crafted title slide not only piques interest but also conveys professionalism and sets the tone for the content that follows. By investing time and creativity into your cover slides, you can significantly enhance the overall impact of your presentation, ensuring your audience is engaged from the very beginning.
In this guide, we showcase seven exemplary PowerPoint cover slides that exemplify outstanding design, ranging from minimalistic to highly professional. These examples provide a wealth of inspiration, demonstrating how different styles can be effectively utilized to make a powerful first impression. Whether you prefer clean and simple designs or more elaborate and polished ones, these slides offer valuable ideas for creating a compelling visual entrance to your presentation. By emulating these techniques, you can elevate your presentation game and ensure that your message is delivered with maximum impact.
Your PowerPoint title slide (i.e., cover slide) is arguably one of the most important slides in your deck and one that you should spend extra time making PERFECT. Think about it: Your title slide sets the stage for your entire presentation. We all make instant judgments that either give us hope or lower expectations. Think of your title slide as the all-important first introduction. It’s a taste of things to come for the rest of your presentation. An exceptional title slide gives your audience hope that the presentation will be exceptional. Conversely, a poorly designed or low-quality title slide conveys a lack of attention to detail.
Your audience will mostly assume that if you rushed your cover, you rushed your entire presentation. Therefore, before you get up on stage to present, take the time to make sure your cover slide rocks. If you have no idea where to begin creating a dynamic title slide, don’t worry. I have got you covered!
There are many ways to go about creating your title slide. To give you a little slide inspiration, here are some PowerPoint title slides examples that look great.
Let’s begin!
1. the minimal – a smart looking title slide design starts with simplicity.

Triangle Presentation Template – available for download here
Einstein once said, “simplicity is the ultimate sophistication,” and that is certainly true when it comes to title slides. This title slide is proof that less truly is more. A simple image married to some minimal text, with a bit of “design flair,” is really all you need to have a title slide that stands out.
Why this PowerPoint title slide example works:
- Simple and modern design
- Plenty of whitespace allows the title to shine
- Cool black and white style
- Three different font sizes create a nice visual hierarchy
- Easily directs audience eyes to flow from top to bottom
2. The Professional – A Sleek and Simple Layout That Lets Your Title and Image Equally Shine

Influencer Presentation Template – available for download here
Here’s an example of a title slide that works with pretty much every presentation. It’s sleek and has a professional design that will surely make you stand out and close the deal.
- Clean, bold, and professional look
- Plenty of whitespace allows the title and logo to shine
- Cool transparent shape overlay
- Three different font sizes create a visual hierarchy
- Great font combination
- Consistent color scheme
3. The 3 Triangles – Geometric Shapes Filled with Consistent Images Makes for a Clean Looking Slide

Modern Presentation Template – available for download here
Here’s an example of a title slide that has a unique way of showing off key images that represent what your presentation is about. As long as you keep your images looking consistent, this style will easily start your presentation off with a bang.
- Creative and simple geometric design – sharp edges
- Three attractive images that have a consistent look and feel (nature-themed)
- Good contrast of color images on a white background
- Three different image sizes create harmony (power of three)
- Good font combination
4. The Backdrop – A Transparent Overlay Over a Single Background Image Always Looks Good

Startup X Presentation Template – available for download here
Filling up your entire title page with a single background image can work wonders. Just make sure that any text that you overlay on top of the image can easily be read. If you have a busy image with limited whitespace (like the one seen above), you can simply add whitespace to the image by overlaying a semi-transparent shape. Just make sure the color of the transparent shape has plenty of contrast from the background image.
- Background image takes up the entire slide
- Cool semi-transparent shape overlay
- Plenty of whitespace allows both the title and logo to shine
- Good contrast of transparent shape over color image
5. The Designer – This Futuristic Title Slide Proves Photos Are Not Necessary
Report Presentation Template – available for download here
Using a bit of creativity with shapes and layout, you can create a title slide that looks great without using any images. Pulling off a title slide like this will surely make it look like you had your presentation created by a professional designer .
- Cool modern design – futuristic look and feel
- Bold black and white design
- Good contrast of white text over black shape
- Plenty of whitespace around the title text
6. The Profile – A Smartly Designed Collage of Consistent Photos
Company Profile Presentation Template – available for download here
Similar to the third title slide example, a great way to show what your presentation is about is to use a collage of images within a cool-looking layout (like the example above). Just make sure that your images look consistent in terms of style, color, composition, etc.
- Four consistent images show multiple aspects of the business or presentation
- Energetic color scheme
- Plenty of whitespace around the title
7. The Client – A Subtle Title Slide Look That Shows Off Your Clients Nicely

Elevator Pitch Presentation Template – available for download here
If your presentation is for a client or series of clients, you may need to add their logos to the title slide. If that is the case, make sure there is plenty of space for those logos to breathe. Also, if the logos that you are inserting happen to all be different colours (and each one is individually screaming for attention), consider either placing them all behind a transparent shape overlay or changing the colour of all the logos to match the rest of your colour scheme on the slide (as seen above).
- Cool semi-transparent shape overlay makes the title text easy to read
- Plenty of whitespace allows the title and client logos to stand out
- Client logos match the rest of the colour scheme on the slide
Spend extra time making sure your PowerPoint title slides look awesome. Remember, the PowerPoint title slides you design set the tone for your entire presentation. That’s why you need to make sure extra attention gets put into creating this slide. You’ve likely spent a lot of time working on your presentation. So, why give someone the opportunity to dismiss it in the first three seconds? You owe it to yourself to get the cover slide nailed down properly.
The best way to come up with an exciting new cover slide for your presentation is by getting presentation inspiration from others. We hope that some of the PowerPoint cover template slides shown in this post have provided a bit of creative spark to get you thinking.
Here’s my question for you: What’s your favorite way of creating awesome-looking presentation cover slides? Sound off in the comments below. I read each and every one.
Also, if you found this post on PowerPoint cover slides helpful, please share it with your friends using the share buttons to the left.
Looking for more helpful tips for creating presentation cover slides ? Here are a few suggested articles you will likely get a kick out of:
- 10 PowerPoint Cover Slide Examples That Will Energize Any Room
- Awesome SlideShare Cover Slides That Will Inspire Your Next Presentation
- 10 Professional PowerPoint Templates That Will Cut Your Design Time in Half
- Why are PowerPoint title slides important? PowerPoint title slides are crucial because they set the stage for your entire presentation, making the first impression on your audience.
- How can I create impactful presentation cover slides? To create impactful presentation cover slides , focus on simplicity, use high-quality images, and ensure a good balance of text and whitespace.
- What are some design tips for title slide design? Some design tips for title slide design include using contrasting colors, maintaining a clean layout, and incorporating visually appealing fonts.
- Where can I find inspiration for my presentation cover slides? You can find presentation inspiration by looking at examples of well-designed slides, such as those featured in this blog, and by exploring online resources like SlideShare.
- How does a good title slide impact a presentation? A good title slide creates a strong first impression, sets the tone for the presentation, and engages the audience from the start, making your presentation more effective.
Ready to elevate your presentation design? Use these examples of PowerPoint title slides to inspire your next presentation cover slides . Share this blog with friends and colleagues who could benefit from fresh presentation inspiration and start creating presentations that wow your audience today!
Want more blogs, Check out these additional blogs you may find interesting:
5 Clever Ways to Present Data Effectively in PowerPoint (With Awesome Examples)
Mastering Clip Art Remixing: A Step-by-Step Guide to Custom Icons in PowerPoint
Discover how we can create magic in your communication
%20(1).jpg)
Blog Categories
About the author.

Nikita - Unleashing Creative Magic
I'm an ardent creative explorer. With every stroke of my digital brush, I bring your ideas to life. Books are my cherished companions, sparking the exceptional ideas that I love to infuse into our team's projects.
Read The latest Related Blog

8 Essential Design Principles for Impactful Presentations: Enhance Your Brand's Message

Mastering Executive Presentations: 9 Essential Tips for Impressing Senior Management

Top 8 Sources for PowerPoint Presentation Inspiration | Enhance Your Designs
Experience excellence with your presentations..
%20(1).png)
CHICAGO AUGUST 29-30 PUBLIC SPEAKING CLASS IS ALMOST FULL! RESERVE YOUR SPOT NOW

- Public Speaking Classes
- Corporate Presentation Training
- Online Public Speaking Course
- Northeast Region
- Midwest Region
- Southeast Region
- Central Region
- Western Region
- Presentation Skills
- 101 Public Speaking Tips
- Fear of Public Speaking
Catchy Presentation Titles Are the Start of a Great Presentation
A Catchy Presentation Title is Important for Audience Satisfaction
Think about the last time you went to a conference that has multiple breakout sessions going at the same time. If you are like most people, you first scanned the list of titles. Almost instantly, you eliminated a few based solely on the topic or title. The titles that you looked at created an impression of the speech. Once you narrowed down your choices, only then do you move on to the description, etc. In that instant where you were scanning the titles, though, you probably had this inner monologue going. “Hhhmmmm… Nope. Not worth my time. Nope. Sounds boring. Nope. That one is unrelated to anything of interest to me. Aaahhh… That one might be okay.”
One of the real, closely-held, public speaking secrets is that every audience member has this inner monologue . This inner monologue occurs before every single meeting and every single presentation that we attend. In most cases, just as when we looked at the breakout session list, the answer we receive is, “Nope. This seems like a waste of my time.”
Examples of Presentation Titles that Make People Yawn
Here are a few titles that tell the audience that your presentation will be a snoozefest.
- Quarterly Financial Report
- Software Update
- Project Report
- Goals for 20__ [Fill in Your Own Year]
- Why We Need to Make Changes in Our Internal Processes
It is our job as the presentation designer (or deliverer) to make people want to pay attention to us. If you start with a great title, you are more likely to accomplish this task.
Presentation Title Generator
Follow this step-by-step approach, and your audience will want to hear you speak.
Create a One-Sentence Statement of What Your Topic is About.
- We Exceeded Our Corporate Goals and Increased Profit Last Quarter.
- The New Software Update Closed a Few Security Risks for Our Customers.
- The ABC Building Project is Behind Schedule.
- This Year, We Will Increase Revenue by $200,000 by Focusing on Repeat Business.
- Department Heads Need to Communicate Team Activities Better.
Just by forcing yourself to make your title into a complete sentence, you will narrow the topic down dramatically. If you look at the difference between the first list and the second, the second is more interesting already.
Identify Why the Audience Would Care About this Topic?
- Your Quarterly Bonus Has Increased.
- Your Customers are Less Likely to Experience a Data Breach.
- If We Adjust Our Plan, We Can Get Back on Schedule without Incurring Overruns.
- Your Commissions Will Also Increase.
- You Can Reduce Your Overall Department Costs.
Although we like to think that department heads care deeply about company revenue and profit, in reality, most of us are pretty self-centered. However, the department heads care very deeply about their bonuses. Outside of the tech folks, no one really cares about website security. However, if a company has a data breach, the entire company will have new challenges to deal with.
Combine the Sentence in Step #1 With the Benefit in Step #2.
Now that you have the two pieces, just put them together. When you do, you will create a series of catchy presentation titles .
- We Exceeded Our Corporate Goals and Increased Profit Last Quarter, So Your Quarterly Bonus Has Also Increased.
- Your Customers are Less Likely to Experience a Data Breach Because We Closed a Few Security Risks in the Recent Update.
- If We Adjust the Project Plan on the ABC Building, We Can Get Back on Schedule without Incurring Overruns.
- This Year, We Will Increase Revenue by $200,000 (And Commissions by $25,000) by Focusing on Repeat Business.
- If We as Department Heads Can Communicate Our Team’s Activities Better, We Should Be Able to Reduce Department Cost Significantly.
Maybe these presentation titles aren’t perfect, but you have to admit, they are dramatically better, now.
Compare the Two Titles
Originally, we had, “Quarterly Financial Report.” We ended up with, We Exceeded Our Corporate Goals and Increased Profit Last Quarter, So Your Quarterly Bonus Has Also Increased.” Which would you rather sit through? Guess what? Your audience thinks the same way. So, if you want to catch the attention of your audience right away, realize that catch presentation titles can help.
By the way, once you have a great title, the post called How to Design a Presentation Quickly is a good second step. In addition, we have a free Online Speech Creator that walks you through the entire process step-by-step. Also, make sure to visit our 101 public speaking tips blog post.

Podcasts , presentation skills | presentation skills
View More Posts By Category: Free Public Speaking Tips | leadership tips | Online Courses | Past Fearless Presentations ® Classes | Podcasts | presentation skills | Uncategorized
How-To Geek
How to add titles to slides in microsoft powerpoint.

Your changes have been saved
Email is sent
Email has already been sent
Please verify your email address.
You’ve reached your account maximum for followed topics.
How Sega Preserves Its Classic Arcade Games Better Than Anyone
Consider these 6 things before installing smart security cameras, the 7 battery questions people always ask me, quick links, find slides with missing titles in powerpoint, add slide titles using outline view, use a title slide layout, how to hide the title on a slide.
You may not think much about using slide titles for your presentations. But for accessibility and the use of other features, slide titles are important. Here, we'll show you how to add titles to slides in Microsoft PowerPoint.
For those using screen readers, slide titles are essential. And if you use features like custom slide shows or hyperlinks to slides in your presentation, slide titles are necessary elements. We'll show you how to quickly find slides that are missing titles and a few different ways to add titles to those slides.
Rather than reviewing each slide to visually spot the missing titles, you can use PowerPoint's built-in Accessibility Checker to find them fast.
Related: How to Add Alternative Text to an Object in PowerPoint
Open your presentation, go to the Review tab, and click "Check Accessibility" in the Accessibility section of the ribbon.

You'll see the Accessibility panel open on the right with Errors, Warnings, and Tips. Expand Errors and you'll see an item labeled Missing Slide Title with the number of slides in need of titles. If you don't see this error, then you don't have any missing titles.
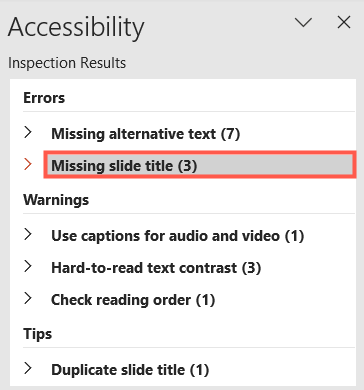
Immediately Add Slide Titles
If you expand the Missing Slide Title label, you'll see the exact slide numbers that are missing titles.
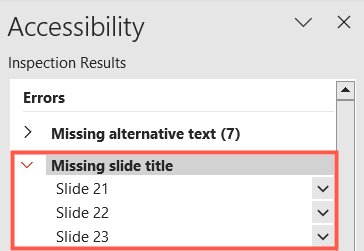
You can then immediately add a title by doing one of the following:
- Click a slide number and it will display highlighted in the panel on the left side. Click next to the number and add a title.
- Click the drop-down arrow to the right of the slide and select "Add Slide Title."
- Select the slide, use the Slide Title drop-down arrow on the Accessibility tab, and choose "Add Slide Title."
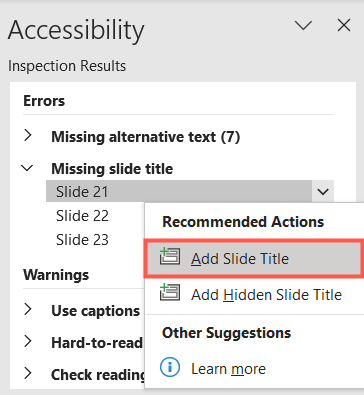
Outline view is what you'll see on the left side of PowerPoint if you use the first method above to find missing slide titles. But you can also jump right to it to see which slides need titles if you like.
Go to the View tab and click "Outline View" in the Presentation Views section of the ribbon.
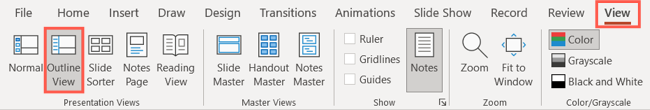
You'll then see this view appear on the left with each slide number. The title of a slide is the text that appears in bold. If you're missing a title, simply type it next to the small square for that slide.
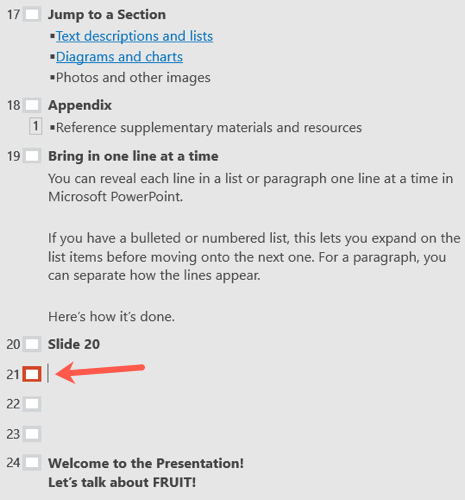
One way to avoid missing slide titles is to use a layout that includes a title. While not always convenient for the type of slide you need, it's still an option.
To add a slide with a title, click the New Slide drop-down arrow on either the Home or Insert tab. You'll see those layouts with a title such as Title and Content or Title Only. Choose one of these and use the title text box included on the slide.
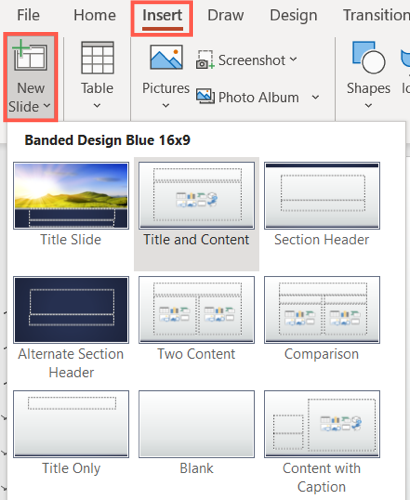
You can also change the layout of a current slide if it fits in with your presentation. Select the slide and go to the Home tab. Click the Layout drop-down arrow and choose a title slide like above. This changes the current layout to one with a title.
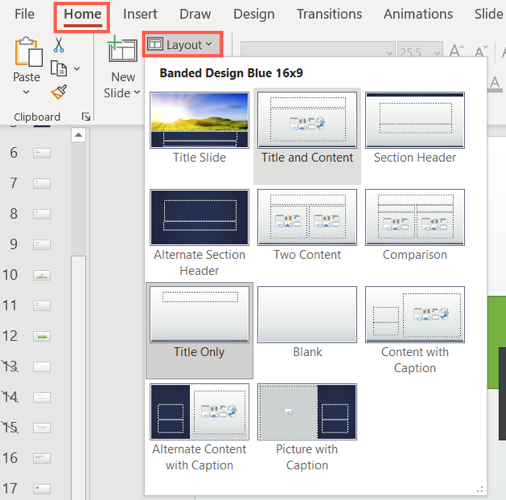
One disadvantage to adding titles to slides or using a title layout is that the title actually appears on the slide. Again, this may not be something you want, especially if the slide only contains a video or image.
Related: How to Add a Video to a Microsoft PowerPoint Presentation
A way around showing the title on the slide is to simply hide it, and there are two easy ways to do this.
Add a Hidden Title
Display the Accessibility tab by going to Review > Check Accessibility. In the Screen Reader section of the ribbon, click the Slide Title drop-down arrow and pick "Add Hidden Slide Title."
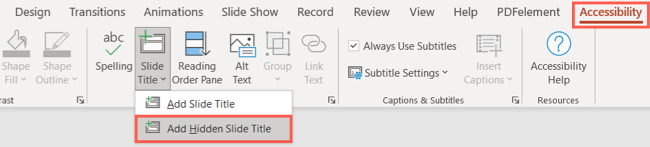
You'll see the text box for the title display directly above the slide. Simply add your title to it and leave the box where it is.
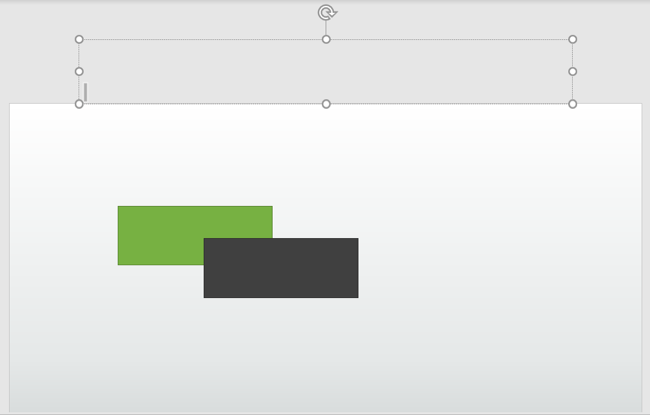
Move the Title Off the Slide
Another way to hide the title is to select the text box containing the title on your slide. When your cursor changes to a four-sided arrow, use it to drag the box off of the slide. You can move it above, below, or to one of the sides.
When you preview or practice your slideshow after using one of the above methods, you shouldn't see the title on the slide. However, the title is still technically there and available for screen readers and specific PowerPoint features.
Related: How to Practice Your Presentations with PowerPoint's Presenter Coach
Be respectful of those joining your presentation using a screen reader or prepare for other features that PowerPoint has to offer by including slide titles.
- Microsoft Office
- Microsoft PowerPoint
- Environment
- Science & Technology
- Business & Industry
- Health & Public Welfare
- Topics (CFR Indexing Terms)
- Public Inspection
- Presidential Documents
- Document Search
- Advanced Document Search
- Public Inspection Search
- Reader Aids Home
- Office of the Federal Register Announcements
- Using FederalRegister.Gov
- Understanding the Federal Register
- Recent Site Updates
- Federal Register & CFR Statistics
- Videos & Tutorials
- Developer Resources
- Government Policy and OFR Procedures
- Congressional Review
- My Clipboard
- My Comments
- My Subscriptions
- Sign In / Sign Up
- Site Feedback
- Search the Federal Register
This site displays a prototype of a “Web 2.0” version of the daily Federal Register. It is not an official legal edition of the Federal Register, and does not replace the official print version or the official electronic version on GPO’s govinfo.gov.
The documents posted on this site are XML renditions of published Federal Register documents. Each document posted on the site includes a link to the corresponding official PDF file on govinfo.gov. This prototype edition of the daily Federal Register on FederalRegister.gov will remain an unofficial informational resource until the Administrative Committee of the Federal Register (ACFR) issues a regulation granting it official legal status. For complete information about, and access to, our official publications and services, go to About the Federal Register on NARA's archives.gov.
The OFR/GPO partnership is committed to presenting accurate and reliable regulatory information on FederalRegister.gov with the objective of establishing the XML-based Federal Register as an ACFR-sanctioned publication in the future. While every effort has been made to ensure that the material on FederalRegister.gov is accurately displayed, consistent with the official SGML-based PDF version on govinfo.gov, those relying on it for legal research should verify their results against an official edition of the Federal Register. Until the ACFR grants it official status, the XML rendition of the daily Federal Register on FederalRegister.gov does not provide legal notice to the public or judicial notice to the courts.
Design Updates: As part of our ongoing effort to make FederalRegister.gov more accessible and easier to use we've enlarged the space available to the document content and moved all document related data into the utility bar on the left of the document. Read more in our feature announcement .
Medicare Program; Inpatient Rehabilitation Facility Prospective Payment System for Federal Fiscal Year 2025 and Updates to the IRF Quality Reporting Program
A Rule by the Centers for Medicare & Medicaid Services on 08/06/2024
This document has been published in the Federal Register . Use the PDF linked in the document sidebar for the official electronic format.
- Document Details Published Content - Document Details Agencies Department of Health and Human Services Centers for Medicare & Medicaid Services Agency/Docket Number CMS-1804-F CFR 42 CFR 412 Document Citation 89 FR 64276 Document Number 2024-16911 Document Type Rule Pages 64276-64340 (65 pages) Publication Date 08/06/2024 RIN 0938-AV31 Published Content - Document Details
- View printed version (PDF)
- Document Dates Published Content - Document Dates Effective Date 10/01/2024 Dates Text This final action is effective on October 1, 2024. Published Content - Document Dates
This table of contents is a navigational tool, processed from the headings within the legal text of Federal Register documents. This repetition of headings to form internal navigation links has no substantive legal effect.
FOR FURTHER INFORMATION CONTACT:
I. executive summary, b. summary of major provisions, c. summary of impact, ii. background, a. statutory basis and scope for irf pps provisions, b. provisions of the affordable care act and the medicare access and chip reauthorization act of 2015 (macra) affecting the irf pps in fy 2012 and beyond, c. operational overview of the current irf pps, iii. summary of provisions of the final rule, iv. analysis of and responses to public comments, a. general comments on the fy 2025 irf pps proposed rule, v. updates to the case-mix group (cmg) relative weights and average length of stay (alos) values for fy 2025, vi. fy 2025 irf pps payment update, a. background, b. fy 2025 market basket update and productivity adjustment, 1. fy 2025 market basket update, 2. fy 2025 productivity adjustment, c. labor-related share for fy 2025, d. wage adjustment for fy 2025, 1. background, 2. core-based statistical areas (cbsas) for the fy 2025 irf wage index, a. urban counties becoming rural, b. rural counties becoming urban, c. urban counties moving to a different urban cbsa, d. change to county-equivalents in the state of connecticut, 3. transition policy for fy 2025 wage index changes, 4. irf budget-neutral wage adjustment factor methodology, g. description of the irf standard payment conversion factor and payment rates for fy 2025, h. example of the methodology for adjusting the prospective payment rates, vii. update to payments for high-cost outliers under the irf pps for fy 2025, a. update to the outlier threshold amount for fy 2025, b. update to the irf cost-to-charge ratio (ccr) ceiling and urban/rural averages for fy 2025, viii. inpatient rehabilitation facility (irf) quality reporting program (qrp), a. background and statutory authority, b. general considerations used for the selection of measures for the irf qrp, 1. quality measures currently adopted for the irf qrp, c. collection of four new items as standardized patient assessment data elements and modification of one item collected as a standardized patient assessment data element beginning with the fy 2028 irf qrp, 1. definition of standardized patient assessment data, 2. social determinants of health collected as standardized patient assessment data elements, 3. collection of four new items as standardized patient assessment data elements beginning with the fy 2028 irf qrp, (a) living situation, (c) utilities, 4. interested party input, (a) comments on the living situation assessment item, (b) comments on the food assessment items, (c) comments on the utilities assessment item, 5. modification of the transportation item beginning with the fy 2028 irf qrp, d. irf qrp quality measure concepts under consideration for future years—request for information (rfi), 1. vaccination composite, 2. pain management, 3. depression, 4. other suggestions for future measure concepts, e. future irf star rating system: request for information (rfi), 1. specific criteria to use in measure selection, 2. presentation of irf star ratings information, 3. other comments received about an irf star ratings system, f. form, manner, and timing of data submission under the irf qrp, 2. reporting schedule for the proposed new standardized patient assessment data elements and the modified transportation data element beginning with the fy 2028 irf qrp, 3. removal of the admission class item from the irf-pai beginning october 1, 2026., (a) background, (b) removal of item, g. policies regarding public display of measure data for the irf qrp, ix. collection of information requirements, a. requirements for updates related to the irf qrp beginning with the fy 2028 irf qrp, x. regulatory impact analysis, a. statement of need, b. overall impact, c. anticipated effects, 1. effects on irfs, 2. detailed economic analysis, 3. description of table 17, 4. impact of the update to the outlier threshold amount, 5. impact of the wage index, labor-related share, and wage index cap, 6. impact of the updated cbsa delineations, 7. impact of the phase-out of the rural adjustment for irfs transitioning from rural to urban designations, 8. impact of the update to the cmg relative weights and alos values, 9. effects of requirements for the irf qrp beginning with the fy 2028 irf qrp, d. alternatives considered, e. regulatory review costs, f. accounting statement and table, g. conclusion.
This feature is not available for this document.
FederalRegister.gov retrieves relevant information about this document from Regulations.gov to provide users with additional context. This information is not part of the official Federal Register document.
Medicare Program: Inpatient Rehabilitation Facility Prospective Payment System for Federal Fiscal Year 2025 and Updates to the Inpatient Rehabilitation Facility Quality Reporting Program (CMS-1804-P)
- Sharing Enhanced Content - Sharing Shorter Document URL https://www.federalregister.gov/d/2024-16911 Email Email this document to a friend Enhanced Content - Sharing
- Print this document
Document page views are updated periodically throughout the day and are cumulative counts for this document. Counts are subject to sampling, reprocessing and revision (up or down) throughout the day.
This document is also available in the following formats:
More information and documentation can be found in our developer tools pages .
This PDF is the current document as it appeared on Public Inspection on 07/31/2024 at 4:15 pm.
It was viewed 0 times while on Public Inspection.
If you are using public inspection listings for legal research, you should verify the contents of the documents against a final, official edition of the Federal Register. Only official editions of the Federal Register provide legal notice of publication to the public and judicial notice to the courts under 44 U.S.C. 1503 & 1507 . Learn more here .
Document headings vary by document type but may contain the following:
- the agency or agencies that issued and signed a document
- the number of the CFR title and the number of each part the document amends, proposes to amend, or is directly related to
- the agency docket number / agency internal file number
- the RIN which identifies each regulatory action listed in the Unified Agenda of Federal Regulatory and Deregulatory Actions
See the Document Drafting Handbook for more details.
Department of Health and Human Services
Centers for medicare & medicaid services.
- 42 CFR Part 412
- [CMS-1804-F]
- RIN 0938-AV31
Centers for Medicare & Medicaid Services (CMS), Department of Health and Human Services (HHS).
Final action.
This final action updates the prospective payment rates for inpatient rehabilitation facilities (IRFs) for Federal fiscal year (FY) 2025. As required by statute, this final action includes the classification and weighting factors for the IRF prospective payment system's case-mix groups and a description of the methodologies and data used in computing the prospective payment rates for FY 2025. We are updating the Office of Management and Budget (OMB) market area delineations for the IRF prospective payment system (PPS) wage index and applying a 3-year phase-out of the rural adjustment. This rule also includes updates for the IRF Quality Reporting Program (QRP).
This final action is effective on October 1, 2024.
Applicability dates: The updated IRF prospective payment rates are applicable for IRF discharges occurring on or after October 1, 2024, and on or before September 30, 2025 (FY 2025).
Patricia Taft, (410)-786-4561, for general information.
Kim Schwartz, (410) 786-2571, for information about the IRF payment policies, payment rates and coverage policies.
Ariel Cress, (410) 786-8571, for information about the IRF quality reporting program.
This final rule updates the prospective payment rates for IRFs for FY 2025 (that is, for discharges occurring on or after October 1, 2024, and on or before September 30, 2025) as required under section 1886(j)(3)(C) of the Social Security Act (the Act). As required by section 1886(j)(5) of the Act, this final rule includes the classification and weighting factors for the IRF PPS's case-mix groups (CMGs), a description of the methodologies and data used in computing the prospective payment rates for FY 2025, and revised OMB core-based statistical area delineations from the July 21, 2023, OMB Bulletin (No. 23-01) for the IRF PPS wage index.
For the IRF QRP, this rule finalizes the collection of four new items as standardized patient assessment data elements and the modification of one item collected as a standardized patient assessment data element, in the IRF-Patient Assessment Instrument (IRF-PAI) beginning with the FY 2028 IRF QRP. This final rule also finalizes a proposal with modification to remove one assessment item from the IRF-PAI. In addition, this final rule provides a summary of the information received on our Request for Information on quality measure concepts for the IRF QRP in future years and an IRF star rating system.
In this final rule, we use the methods described in the FY 2024 IRF PPS final rule ( 88 FR 50956 ) to update the prospective payment rates for FY 2025 using updated FY 2023 IRF claims and the most recent available IRF cost report data, which is FY 2022 IRF cost report data. We also use the revised OMB market area delineations from the July 21, 2023, OMB Bulletin (No. 23-01) for the IRF PPS wage index, and apply a 3-year phase-out of the rural adjustment for those IRFs changing from rural to urban.
For the IRF QRP, we are finalizing four new items as standardized patient assessment data elements that IRFs must collect and submit using the IRF-PAI beginning with the FY 2028 IRF QRP: one item for Living Situation, two items for Food, and one item for Utilities. We are also finalizing our proposal to modify the current Transportation item beginning with the FY 2028 IRF QRP. Additionally, we are finalizing with modification our proposal to remove Item 14. Admission Class from the IRF-PAI. Finally, in the proposed rule, we sought input from interested parties on future IRF QRP quality measure concepts and an IRF star rating system and are providing a summary of the comment we received.
TABLE 1—Cost and Benefit
Section 1886(j) of the Act provides for the implementation of a per-discharge PPS for inpatient rehabilitation hospitals and inpatient rehabilitation units of a hospital (collectively, hereinafter referred to as IRFs). Payments under the IRF PPS encompass inpatient operating and capital costs of furnishing covered rehabilitation services (that is, routine, ancillary, and capital costs), but not direct graduate medical education costs, costs of approved nursing and allied health education activities, bad debts, and other services or items outside the scope of the IRF PPS. A complete discussion of the IRF PPS provisions appears in the original FY 2002 IRF PPS final rule ( 66 FR 41316 ) and the FY 2006 IRF PPS final rule ( 70 FR 47880 ) and we provided a general description of the IRF PPS for FYs 2007 through 2019 in the FY 2020 IRF PPS final rule ( 84 FR 39055 through 39057 ). A general description of the IRF PPS for FYs 2020 through 2024, along with detailed background information for various other aspects of the IRF PPS, is now available on the CMS website at https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/InpatientRehabFacPPS .
Under the IRF PPS from FY 2002 through FY 2005, the prospective payment rates were computed across 100 distinct CMGs, as described in the FY 2002 IRF PPS final rule ( 66 FR 41316 ). We constructed 95 CMGs using rehabilitation impairment categories (RICs), functional status (both motor and cognitive), and age (in some cases, cognitive status and age may not be a factor in defining a CMG). In addition, we constructed five special CMGs to account for very short stays and for patients who expire in the IRF.
For each of the CMGs, we developed relative weighting factors to account for a patient's clinical characteristics and expected resource needs. Thus, the weighting factors accounted for the relative difference in resource use across all CMGs. Within each CMG, we created tiers based on the estimated effects that certain comorbidities would have on resource use.
We established the Federal PPS rates using a standardized payment conversion factor (formerly referred to as the budget-neutral conversion factor). For a detailed discussion of the budget-neutral conversion factor, please refer to our FY 2004 IRF PPS final rule ( 68 FR 45684 through 45685 ). In the FY 2006 IRF PPS final rule ( 70 FR 47880 ), we discussed in detail the methodology for determining the standard payment conversion factor.
We applied the relative weighting factors to the standard payment conversion factor to compute the unadjusted prospective payment rates under the IRF PPS from FYs 2002 through 2005. Within the structure of the payment system, we then made adjustments to account for interrupted stays, transfers, short stays, and deaths. Finally, we applied the applicable adjustments to account for geographic variations in wages (wage index), the percentage of low-income patients, location in a rural area (if applicable), and outlier payments (if applicable) to the IRFs' unadjusted prospective payment rates.
For cost reporting periods that began on or after January 1, 2002, and before October 1, 2002, we determined the final prospective payment amounts using the transition methodology prescribed in section 1886(j)(1) of the Act. Under this provision, IRFs transitioning into the PPS were paid a blend of the Federal IRF PPS rate and the payment that the IRFs would have received had the IRF PPS not been implemented. This provision also allowed IRFs to elect to bypass this blended payment and immediately be paid 100 percent of the Federal IRF PPS rate. The transition methodology expired as of cost reporting periods beginning on or after October 1, 2002 (FY 2003), and payments for all IRFs now consist of 100 percent of the Federal IRF PPS rate.
Section 1886(j) of the Act confers broad statutory authority upon the Secretary to propose refinements to the IRF PPS. In the FY 2006 IRF PPS final rule ( 70 FR 47880 ) and in correcting amendments to the FY 2006 IRF PPS final rule ( 70 FR 57166 ), we are finalizing a number of refinements to the IRF PPS case-mix classification system (the CMGs and the corresponding relative weights) and the case-level and facility-level adjustments. These refinements included the adoption of the Office of Management and Budget's (OMB's) Core-Based Statistical Area market definitions; modifications to the CMGs, tier comorbidities; and CMG relative weights, implementation of a new teaching status adjustment for IRFs; rebasing and revising the market basket used to update IRF payments, and updates to the rural, low-income percentage (LIP), and high-cost outlier adjustments. Beginning with the FY 2006 IRF PPS final rule ( 70 FR 47908 through 47917 ), the market basket used to update IRF payments was a market basket reflecting the operating and capital cost structures for freestanding IRFs, freestanding inpatient psychiatric facilities (IPFs), and long-term care hospitals (LTCHs). Any reference to the FY 2006 IRF PPS final rule in this final rule also includes the provisions effective in the correcting amendments. For a detailed discussion of the final key policy changes for FY 2006, please refer to the FY 2006 IRF PPS final rule.
In response to COVID-19 Public Health Emergency (PHE), we published two interim final rules with comment period affecting IRF payment and conditions for participation. The interim final rule with comment period (IFC) entitled “Medicare and Medicaid Programs; Policy and Regulatory Revisions in Response to the COVID-19 Public Health Emergency,” published on April 6, 2020 ( 85 FR 19230 ) (hereinafter referred to as the April 6, 2020 IFC), included certain changes to the IRF PPS medical supervision requirements at 42 CFR 412.622(a)(3)(iv) and 412.29(e) during the PHE for COVID-19. In addition, in the April 6, 2020 IFC, we removed the post-admission physician evaluation requirement at § 412.622(a)(4)(ii) for all IRFs during the PHE for COVID-19. In the FY 2021 IRF PPS final rule, to ease documentation and administrative burden, we permanently removed the post-admission physician evaluation documentation requirement at § 412.622(a)(4)(ii) beginning in FY 2021.
A second IFC, entitled “Medicare and Medicaid Programs, Basic Health Program, and Exchanges; Additional Policy and Regulatory Revisions in Response to the COVID-19 Public Health Emergency and Delay of Certain Reporting Requirements for the Skilled Nursing Facility Quality Reporting Program,” was published on May 8, 2020 ( 85 FR 27550 ) (hereinafter referred to as the May 8, 2020 IFC). Among other changes, the May 8, 2020 IFC included a waiver of the “3-hour rule” at § 412.622(a)(3)(ii) to reflect the waiver required by section 3711(a) of the Coronavirus Aid, Relief, and Economic Security Act (CARES Act) ( Pub. L. 116-136 , enacted on March 27, 2020). In the May 8, 2020 IFC, we also modified certain IRF coverage and classification requirements for freestanding IRF hospitals to relieve acute care hospital capacity concerns in States (or regions, as applicable) experiencing a surge during the PHE for COVID-19. In addition to the policies adopted in our IFCs, we responded to the PHE with numerous blanket waivers [ 1 ] and other flexibilities, [ 2 ] some of which are applicable to the IRF PPS. CMS finalized these policies in the Calendar Year 2023 Hospital Outpatient Prospective Payment and Ambulatory Surgical Center Payment Systems final rule with comment period ( 87 FR 71748 ). Subsequently, on May 11, 2023, the U.S. Department of Health and Human Services (“HHS”) declared the expiration of the COVID-19 public health emergency. (See https://www.hhs.gov/about/news/2023/02/09/fact-sheet-covid-19-public-health-emergency-transition-roadmap.html . ) As a result, the “3-hour rule” waiver at § 412.622(a)(3)(ii), and other IRF flexibilities were terminated.
The regulatory history previously included in each rule or notice issued under the IRF PPS, including a general description of the IRF PPS for FYs 2007 through 2024, is available on the CMS website at https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/InpatientRehabFacPPS .
The Patient Protection and Affordable Care Act ( Pub. L. 111-148 ) was enacted on March 23, 2010. The Health Care and Education Reconciliation Act of 2010 ( Pub. L. 111-152 ), which amended and revised several provisions of the Patient Protection and Affordable Care Act, was enacted on March 30, 2010. In this final rule, we refer to the two statutes collectively as the “Affordable Care Act” or “ACA”.
The ACA included several provisions that affect the IRF PPS in FYs 2012 and beyond. In addition to what was previously discussed, section 3401(d) of the ACA also added section 1886(j)(3)(C)(ii)(I) of the Act (providing for a “productivity adjustment” for FY 2012 and each subsequent FY). The productivity adjustment for FY 2025 is discussed in section V.D. of this final rule. Section 1886(j)(3)(C)(ii)(II) of the Act provides that the application of the productivity adjustment to the market basket update may result in an update that is less than 0.0 for a FY and in payment rates for a FY being less than such payment rates for the preceding FY.
Section 3004(b) of the ACA and section 411(b) of the MACRA ( Pub. L. 114-10 , enacted on April 16, 2015) also addressed the IRF PPS. Section 3004(b) of ACA reassigned the previously designated section 1886(j)(7) of the Act to section 1886(j)(8) of the Act and inserted a new section 1886(j)(7) of the Act, which contains requirements for the Secretary to establish a QRP for IRFs. Under that program, data must be submitted in a form and manner and at a time specified by the Secretary. Beginning in FY 2014, section 1886(j)(7)(A)(i) of the Act requires the application of a 2-percentage point reduction to the market basket increase factor otherwise applicable to an IRF (after application of paragraphs (C)(iii) and (D) of section 1886(j)(3) of the Act) for a FY if the IRF does not comply with the requirements of the IRF QRP for that FY. Application of the 2-percentage point reduction may result in an update that is less than 0.0 for a FY and in payment rates for a FY being lower than payment rates for the preceding FY. Reporting-based reductions to the market basket increase factor are not cumulative; they only apply for the FY involved. Section 411(b) of the MACRA amended section 1886(j)(3)(C) of the Act by adding paragraph (iii), which required us to apply for FY 2018, after the application of section 1886(j)(3)(C)(ii) of the Act, an increase factor of 1.0 percent to update the IRF prospective payment rates.
As described in the FY 2002 IRF PPS final rule ( 66 FR 41316 ), upon the admission and discharge of a Medicare Part A fee-for-service (FFS) patient, the IRF is required to complete the appropriate sections of a Patient Assessment Instrument (PAI), designated as the IRF-PAI. In addition, beginning with IRF discharges occurring on or after October 1, 2009, the IRF is also required to complete the appropriate sections of the IRF-PAI upon the admission and discharge of each Medicare Advantage (MA) patient, as described in the FY 2010 IRF PPS final rule ( 74 FR 39762 ) and the FY 2010 IRF PPS correction notice ( 74 FR 50712 ). All required data must be electronically encoded into the IRF-PAI software product. Generally, the software product includes patient classification programming called the Grouper software. The Grouper software uses specific IRF-PAI data elements to classify (or group) patients into distinct CMGs and account for the existence of any relevant comorbidities.
The Grouper software produces a five-character CMG number. The first character is an alphabetic character that indicates the comorbidity tier. The last four characters are numeric characters that represent the distinct CMG number. A free download of the Grouper software is available on the CMS website at https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/InpatientRehabFacPPS/Software.html . The Grouper software is also embedded in the internet Quality Improvement and Evaluation System (iQIES) User tool available in iQIES at https://www.cms.gov/medicare/quality-safety-oversight-general-information/iqies .
Once a Medicare Part A FFS patient is discharged, the IRF submits a Medicare claim as a Health Insurance Portability and Accountability Act of 1996 (HIPAA) ( Pub. L. 104-191 , enacted on August 21, 1996) compliant electronic claim or, if the Administrative Simplification Compliance Act of 2002 (ASCA) ( Pub. L. 107-105 , enacted on December 27, 2002) permits, a paper claim (a UB-04 or a CMS-1450 as appropriate) using the five-character CMG number and sends it to the appropriate Medicare Administrative Contractor (MAC). In addition, once a MA patient is discharged, in accordance with the Medicare Claims Processing Manual, chapter 3, section 20.3 (Pub. 100-04), hospitals (including IRFs) must submit to their MAC an informational-only bill (type of bill (TOB) 111) that includes Condition Code 04. This will ensure that the MA days are included in the hospital's Supplemental Security Income (SSI) ratio (used in calculating the IRF LIP adjustment) for FY 2007 and beyond. Claims submitted to Medicare must comply with both ASCA and HIPAA.
Section 3 of the ASCA amended section 1862(a) of the Act by adding paragraph (22), which requires the Medicare program, subject to section 1862(h) of the Act, to deny payment under Part A or Part B for any expenses for items or services for which a claim is submitted other than in an electronic form specified by the Secretary. Section 1862(h) of the Act, in turn, provides that the Secretary shall waive such denial in situations in which there is no method available for the submission of claims in an electronic form or the entity submitting the claim is a small provider. In addition, the Secretary also has the authority to waive such denial in such unusual cases as the Secretary finds appropriate. For more information, see the “Medicare Program; Electronic Submission of Medicare Claims” final rule ( 70 FR 71008 ). Our instructions for the limited number of Medicare claims submitted on paper are available at https://www.cms.gov/manuals/downloads/clm104c25.pdf .
Section 3 of the ASCA operates in the context of the administrative simplification provisions of HIPAA, which include, among others, the requirements for transaction standards and code sets codified in 45 CFR part 160 and part 162, subparts A and I through R (generally known as the Transactions Rule). The Transactions Rule requires covered entities, including covered healthcare providers, to conduct covered electronic transactions according to the applicable transaction standards. (See the CMS program claim memoranda at https://www.cms.gov/ElectronicBillingEDITrans/ and listed in the addenda to the Medicare Intermediary Manual, Part 3, section 3600.)
The MAC processes the claim through its software system. This software system includes pricing programming called the “Pricer” software. The Pricer software uses the CMG number, along with other specific claim data elements and provider-specific data, to adjust the IRF's prospective payment for interrupted stays, transfers, short stays, and deaths, and then applies the applicable adjustments to account for the IRF's wage index, percentage of low-income patients, rural location, and outlier payments. For discharges occurring on or after October 1, 2005, the IRF PPS payment also reflects the teaching status adjustment that became effective as of FY 2006, as discussed in the FY 2006 IRF PPS final rule ( 70 FR 47880 ).
In this FY 2025 IRF PPS final rule, we are finalizing our proposal to update the IRF PPS for FY 2025 and the IRF QRP for FY 2028.
The finalized policy changes and updates to the IRF prospective payment rates for FY 2025 will be as follows:
- Update the CMG relative weights and average length of stay values for FY 2025, in a budget neutral manner, as discussed in section IV.
- Update the IRF PPS payment rates for FY 2025 by the market basket increase factor, based upon the most current data available, with a productivity adjustment required by section 1886(j)(3)(C)(ii)(I) of the Act, as described in section V.
- Update the FY 2025 IRF PPS payment rates by the FY 2025 wage index, describe the adoption of the revised OMB market area delineations, the phase-out of the rural adjustment for those IRFs changing from rural to urban, and the labor related share in a budget-neutral manner, as discussed in section V.
- Describe the calculation of the IRF standard payment conversion factor for FY 2025, as discussed in section V.
- Update the outlier threshold amount for FY 2025, as discussed in section VI.
- Update the cost-to-charge ratio (CCR) ceiling and urban/rural average CCRs for FY 2025, as discussed in section VI.
The finalized policy changes and updates to the IRF QRP for FY 2028 will be as follows:
- Adoption of four items as standardized patient assessment data elements and modification of one item currently collected as a standardized patient assessment data element in the IRF-PAI.
- Remove Item 14. Admission Class item from the IRF-PAI.
- Summarize comments received on the request for information on IRF QRP quality measure and concepts.
- Summarize comments received on the request for information on an IRF QRP star rating system.
We received 44 timely responses from the public, many of which contained multiple comments on the FY 2025 IRF PPS proposed rule ( 89 FR 22246 ). We received comments from various trade associations, inpatient rehabilitation facilities, individual physicians, therapists, clinicians, health care industry organizations, and health care consulting firms. The following sections, arranged by subject area, include a summary of the public comments that we received, and our responses.
In addition to the comments we received on specific proposals contained within the proposed rule (which we address later in this final rule), commenters also submitted more general observations on the IRF PPS and IRF care generally.
Comment: We received several comments that were outside the scope of the FY 2025 IRF PPS proposed rule. Specifically, we received comments regarding updates to the facility-level adjustments (for example, teaching, LIP, and rural); the removal of physician-centric language from regulatory text; the inclusion of recreational therapy in the IRF intensity of therapy requirement; the consequences of increased Medicare Advantage participation for IRFs and Medicare Advantage (MA) payment adjustments; disclosures of ownership and additional disclosable parties' information in the skilled nursing facility setting; and applicability of the IPPS low wage index policy for the IRF PPS wage index.
Response: We thank the commenters for bringing these issues to our attention, and we will take these comments into consideration for potential policy refinements or direct the comments to the appropriate subject matter experts.
As specified in § 412.620(b)(1), we calculate a relative weight for each CMG that is proportional to the resources needed for an average inpatient rehabilitation case in that CMG. For example, cases in a CMG with a relative weight of 2, on average, will cost twice as much as cases in a CMG with a relative weight of 1. Relative weights account for the variance in cost per discharge due to the variance in resource utilization among the payment groups, and their use helps to ensure that IRF PPS payments support beneficiary access to care, as well as provider efficiency.
In this final rule, we update the CMG relative weights and ALOS values for FY2025. Typically, we use the most recent available data to update the CMG relative weights and ALOS values. For FY 2025, we are using the FY 2023 IRF claims and FY 2022 IRF cost report data. These data are the most current and complete data available at this time. Currently, only a small portion of the FY 2023 IRF cost report data is available for analysis, but the majority of the FY 2023 IRF claims data are available for analysis.
In the FY 2025 IRF PPS proposed rule, we proposed that if more recent data became available after the publication of the proposed rule and before the publication of the final rule, we would use such data to determine the FY 2025 CMG relative weights and ALOS values in this final rule.
We proposed to apply these data using the same methodologies that we have used to update the CMG relative weights and ALOS values each FY since we implemented an update to the methodology. The detailed cost to charge ratio (CCR) data from the cost reports of IRF provider units of primary acute care hospitals is used for this methodology, instead of CCR data from the associated primary care hospitals, to calculate IRFs' average costs per case, as discussed in the FY 2009 IRF PPS final rule ( 73 FR 46372 ). In calculating the CMG relative weights, we use a hospital-specific relative value method to estimate operating (routine and ancillary services) and capital costs of IRFs. The process to calculate the CMG relative weights for this final rule is as follows:
Step 1. We estimate the effects that comorbidities have on costs.
Step 2. We adjust the cost of each Medicare discharge (case) to reflect the effects found in Step 1.
Step 3. We use the adjusted costs from Step 2 to calculate CMG relative weights, using the hospital-specific relative value method.
Step 4. We normalize the FY 2025 CMG relative weights using a normalization factor that results in the average CMG relative weights in FY 2025 being the same as the average CMG relative weights in the FY 2024 IRF PPS final rule ( 88 FR 50956 ).
Consistent with the methodology that we have used to update the IRF classification system in each instance in the past, we are updating the CMG relative weights for FY 2025 in such a way that total estimated aggregate payments to IRFs for FY 2025 are the same with or without the changes (that is, in a budget-neutral manner) by applying a budget neutrality factor to the standard payment amount. To calculate the appropriate budget neutrality factor for use in updating the FY 2025 CMG relative weights, we use the following steps:
Step 1. Calculate the estimated total amount of IRF PPS payments for FY 2025 (with no changes to the CMG relative weights).
Step 2. Calculate the estimated total amount of IRF PPS payments for FY 2025 by applying the changes to the CMG relative weights (as discussed in this final rule).
Step 3. Divide the amount calculated in Step 1 by the amount calculated in Step 2 to determine the budget neutrality factor of 0.9976 that would maintain the same total estimated aggregate payments in FY 2025 with and without the changes to the final CMG relative weights.
Step 4. Apply the budget neutrality factor from Step 3 to the FY 2025 IRF PPS standard payment amount after the application of the budget-neutral wage adjustment factor.
In section V. of this final rule, we discuss the use of the existing methodology to calculate the standard payment conversion factor for FY 2025.
In Table 2, “Relative Weights and Average Length of Stay Values for Case Mix Groups,” we present the CMGs, the comorbidity tiers, the corresponding relative weights, and the ALOS values for each CMG and tier for FY 2025. The ALOS for each CMG is used to determine when an IRF discharge meets the definition of a short stay transfer, which results in a per diem case level adjustment.

Generally, updates to the CMG relative weights result in some increases and some decreases to the CMG relative weight values. Table 2 shows how we estimate that the application of the revisions for FY 2025 would affect particular CMG relative weight values, which would affect the overall distribution of payments within CMGs and tiers. We note that, because we implement the CMG relative weight revisions in a budget-neutral manner (as previously described), total estimated aggregate payments to IRFs for FY 2025 would not be affected as a result of the proposed CMG relative weight revisions. However, the revisions would affect the distribution of payments within CMGs and tiers.
TABLE 3—Distributional Effects of the Changes to the CMG Relative Weights
As shown in Table 3, 99.2 percent of all IRF cases are in CMGs and tiers that would experience less than a 5 percent change (either increase or decrease) in the CMG relative weight value as a result of the revisions for FY 2025. The changes in the ALOS values for FY 2025, compared with the FY 2024 ALOS values, are small and do not show any particular trends in IRF length of stay patterns.
We invited public comment on our proposed updates to the CMG relative weights and ALOS values for FY 2025.
The following is a summary of the public comments received on the proposed revisions to update the CMG relative weights and ALOS values for FY 2025 and our responses:
Comment: Public comments generally supported CMS' update to the CMG relative weights and average length of stay values and encouraged CMS to use the latest available data to update these values in the final rule. However, one commenter advocated for meaningful increases to the CMG weights for cases that include the 13 conditions used to identify qualifying facilities under the 60 percent rule in order to help payment increases match the cost of care. Another commenter recommended that CMS consider using an average-cost weighting method, rather than the current hospital-specific relative value method (HSRV), for calculating the CMG relative weights, to improve the relationship between costs and payments and increase the uniformity of profitability across IRF cases.
Response: We appreciate these commenters' support for updating the relative weights and ALOS values for FY 2025. We have updated our data between the FY 2025 IRF PPS proposed and this final rule to ensure that we use the most recent available data in calculating IRF PPS payments.
The methodology that we use to update the CMG relative weights uses the most recent cost data reported by IRFs to compute relative weights that reflect the relative costliness of different IRF cases. We increase or decrease relative weights of the CMGs annually, including for those CMGs associated with the 13 conditions that qualify for the 60 percent rule, under 42 CFR 412.29(b)(2) , based only on the cost data reported to us by IRFs each year.
We believe that these data accurately reflect the severity of the IRF patient population and the associated costs of caring for these patients in the IRF setting. The CMG relative weights are updated each year based on the most recent available data for the full population of IRF Medicare fee-for-service beneficiaries. This ensures that the IRF case mix system is as reflective as possible of changes in the IRF patient populations and the associated coding practices and ensures that IRF payments appropriately reflect the relative costs of caring for all types of IRF patients.
We appreciate commenters' feedback and suggestions for refinements to current methodologies. We recognize commenters' desire for increased weights for cases that include the 13 qualifying conditions. However, the 13 qualifying conditions reflect those conditions that were treated in IRFs when IRFs were first excluded from payment under the IPPS in 1983. These conditions have been used to define IRFs as distinct from IPPS hospitals in terms of the types of patients treated and the types of services provided to these patients. They are not necessarily supposed to be more costly in the IRF to treat than other conditions, just more likely to make up the bulk of patients in the IRF setting.
Also, as stated in section V. of this final rule, the weight calculated for each CMG is proportional to the resources needed for an average case in that CMG. These weights are relative to one another, for example, cases in a CMG with a relative weight of 2, on average, will cost twice as much as cases in a CMG with a relative weight of 1. The weights are empirically derived, based entirely on the data that IRFs report to us on their claims and cost reports, and we do not believe it would be appropriate for us to manipulate these data to increase certain relative weights.
Furthermore, we did not propose any changes to the current HSRV method used to assign payment weights for FY 2025 and believe that a careful evaluation of the advantages and disadvantages of moving to an average-cost weighting method is essential, given the major distributional shifts that would be associated with such a change. The purpose of the HSRV method is, in part, to place a greater emphasis on more efficient IRF providers (that treat complex IRF patients at lower costs). Moving to an average-cost weighting method places more emphasis on high cost IRF providers, which could have higher costs because they are operating less efficiently. We will continue evaluating the effects of changing from HSRV weighting to average-cost weighting. The results of this analysis will inform future rulemaking.
After consideration of the comments we received, we are finalizing our proposal to update the CMG relative weights and ALOS values for FY 2025 using the same methodologies that we have used to update the CMG relative weights and ALOS values each FY since we implemented an update to the methodology in FY 2009, as shown in Table 2 of this final rule. These updates are effective for FY 2025, that is, for discharges occurring on or after October 1, 2024, and on or before September 30, 2025.
Section 1886(j)(3)(C) of the Act requires the Secretary to establish an increase factor that reflects changes over time in the prices of an appropriate mix of goods and services for which payment is made under the IRF PPS. According to section 1886(j)(3)(A)(i) of the Act, the increase factor shall be used to update the IRF prospective payment rates for each FY. Section 1886(j)(3)(C)(ii)(I) of the Act requires the application of the productivity adjustment described in section 1886(b)(3)(B)(xi)(II) of the Act. Thus, in this final rule, we are updating the IRF PPS payments for FY 2025 by a market basket increase factor as required by section 1886(j)(3)(C) of the Act based upon the most current data available, with a productivity adjustment as required by section 1886(j)(3)(C)(ii)(I) of the Act.
We have utilized various market baskets through the years in the IRF PPS. For a discussion of these market baskets, we refer readers to the FY 2016 IRF PPS final rule ( 80 FR 47046 ).
In FY 2016, we finalized the use of a 2012-based IRF market basket, using Medicare cost report data for both freestanding and hospital-based IRFs ( 80 FR 47049 through 47068 ). In FY 2020, we finalized a rebased and revised IRF market basket to reflect a 2016 base year. The FY 2020 IRF PPS final rule ( 84 FR 39071 through 39086 ) contains a complete discussion of the development of the 2016-based IRF market basket. Beginning with FY 2024, we finalized a rebased and revised IRF market basket to reflect a 2021 base year. The FY 2024 IRF PPS final rule ( 88 FR 50966 through 50988 ) contains a complete discussion of the development of the 2021-based IRF market basket.
For FY 2025 (that is, beginning October 1, 2024, and ending September 30, 2025), we proposed to update the IRF PPS payments by a market basket increase factor as required by section 1886(j)(3)(C) of the Act, with a productivity adjustment as required by section 1886(j)(3)(C)(ii)(I) of the Act. For FY 2025, we proposed to use the same methodology described in the FY 2024 IRF PPS final rule ( 88 FR 50982 through 50984 ).
Consistent with historical practice, we proposed to estimate the market basket update for the IRF PPS for FY 2025 based on IHS Global Inc.'s (IGI's) forecast using the most recent available data. Based on IGI's fourth quarter 2023 forecast with historical data through the third quarter of 2023, the proposed 2021-based IRF market basket increase factor for FY 2025 was projected to be 3.2 percent. We also proposed that if more recent data became available after the publication of the proposed rule and before the publication of the final rule (for example, a more recent estimate of the market basket percentage increase or productivity adjustment), we would use such data, if appropriate, to determine the FY 2025 market basket update in this final rule.
Based on IGI's second quarter 2024 forecast with historical data through the first quarter of 2024, the 2021-based IRF market basket percentage increase for FY 2025 is 3.5 percent.
According to section 1886(j)(3)(C)(i) of the Act, the Secretary shall establish an increase factor based on an appropriate percentage increase in a market basket of goods and services. Section 1886(j)(3)(C)(ii) of the Act requires that, after establishing the increase factor for a FY, the Secretary shall reduce such increase factor for FY 2012 and each subsequent FY, by the productivity adjustment described in section 1886(b)(3)(B)(xi)(II) of the Act. Section 1886(b)(3)(B)(xi)(II) of the Act sets forth the definition of this productivity adjustment. The statute defines the productivity adjustment to be equal to the 10-year moving average of changes in annual economy-wide, private nonfarm business multifactor productivity (as projected by the Secretary for the 10-year period ending with the applicable FY, year, cost reporting period, or other annual period) (the “productivity adjustment”). The U.S. Department of Labor's Bureau of Labor Statistics (BLS) publishes the official measures of productivity for the U.S. economy. We note that previously the productivity measure referenced in section 1886(b)(3)(B)(xi)(II) of the Act, was referred to by BLS as private nonfarm business multifactor productivity. Beginning with the November 18, 2021, release of productivity data, BLS replaced the term multifactor productivity (MFP) with total factor productivity (TFP). BLS noted that this is a change in terminology only and will not affect the data or methodology. As a result of this change, the productivity measure referenced in section 1886(b)(3)(B)(xi)(II) is now published by BLS as private nonfarm business total factor productivity. However, as mentioned above, the data and methods are unchanged. Please see www.bls.gov for the BLS historical published TFP data. A complete description of IGI's TFP projection methodology is available on the CMS website at https://www.cms.gov/data-research/statistics-trends-and-reports/medicare-program-rates-statistics/market-basket-research-and-information . In addition, in the FY 2022 IRF final rule ( 86 FR 42374 ), we noted that effective with FY 2022 and forward, CMS changed the name of this adjustment to refer to it as the productivity adjustment rather than the MFP adjustment.
Using IGI's fourth quarter 2023 forecast, the 10-year moving average growth of TFP for FY 2025 was projected to be 0.4 percent. In accordance with section 1886(j)(3)(C) of the Act, we proposed to base the FY 2025 market basket update, which is used to determine the applicable percentage increase for the IRF payments, on IGI's fourth quarter 2023 forecast of the 2021-based IRF market basket. We proposed to then reduce the market basket percentage increase by the estimated productivity adjustment for FY 2025 of 0.4 percentage point (the 10-year moving average growth of TFP for the period ending FY 2025 based on IGI's fourth quarter 2023 forecast). Therefore, the proposed FY 2025 IRF update was equal to 2.8 percent (3.2 percent market basket percentage increase reduced by the 0.4 percentage point productivity adjustment). Furthermore, we proposed that if more recent data became available after the publication of the proposed rule and before the publication of the final rule (for example, a more recent estimate of the market basket percentage increase and/or productivity adjustment), we would use such data, if appropriate, to determine the FY 2025 market basket percentage increase and productivity adjustment in the final rule.
Using IGI's second quarter 2024 forecast, the 10-year moving average growth of TFP for FY 2025 is projected to be 0.5 percent. Thus, in accordance with section 1886(j)(3)(C) of the Act, the FY 2025 market basket percentage increase, which is used to determine the applicable percentage increase for the IRF payments, is equal to 3.5 percent using IGI's second quarter 2024 forecast of the 2021-based IRF market basket. We then reduce this percentage increase by the estimated productivity adjustment for FY 2025 of 0.5 percentage point (the 10-year moving average growth of TFP for the period ending FY 2025 based on IGI's second quarter 2024 forecast). Therefore, the FY 2025 IRF update is equal to 3.0 percent (3.5 percent market basket percentage increase reduced by the 0.5 percentage point productivity adjustment).
CMS recognizes that the Medicare Payment Advisory Commission (MedPAC) recommends that we reduce IRF PPS payment rates by 5 percent for FY 2025. [ 3 ] As discussed, and in accordance with sections 1886(j)(3)(C) and 1886(j)(3)(D) of the Act, the Secretary proposed to update the IRF PPS payment rates for FY 2025 by the proposed productivity-adjusted IRF market basket increase factor of 2.8 percent.
Based on more recent data, the current estimate of the productivity-adjusted IRF market basket increase factor for FY 2025 is 3.0 percent. Section 1886(j)(3)(C) of the Act does not provide the Secretary with the authority to apply a different update factor to IRF PPS payment rates for FY 2025.
We invited public comment on the proposed FY 2025 market basket percentage increase and productivity adjustment. The following is a summary of the public comments received and our responses:
Comment: Several commenters agreed with the general approach of increasing the standard payment conversion factor, but many commenters stated concerns that the proposed increase is inadequate. Commenters cited that the proposed payment increase does not keep pace with the higher increases in costs faced by IRFs such as labor, drug, medical supplies, personal protective equipment, and capital investment costs. Commenters also stated other challenges that could impact costs such as staffing shortages, supply chain disruptions, rising need for cybersecurity investment, higher administrative costs due to MA and commercial plan practices, high patient volumes and rising acuity, and unprecedented high inflation.
Some commenters argued that the increased discrepancy between payment inflation and cost inflation is causing a material financial hardship on hospitals and that increases in hospital costs have dramatically decreased hospital profit margins. One commenter stated that in calendar year 2022, half of U.S. hospitals reported negative profit margins and through the first 10 months of 2023, IRF operating margins were down by 12 percent compared to 2022 and down by 25 percent compared to 2021.
Several commenters stated that labor shortages and higher than typical cost inflation are expected to continue and must be met with correspondingly higher payment rates, especially as some public health emergency resources have concluded. Other commenters stated that the proposed increase factor was too small and called on CMS to increase its proposed market basket percentage in the final rule, with some stating that this increase should be higher than the increase in FY 2024. Some commenters requested that CMS account for the effects of the true inflationary cost using the latest available data in the final rule and other commenters requested that CMS recalculate the market basket update using data that more accurately reflects the growth in input prices. In the absence of such data, some commenters urged CMS to consider an alternative approach to better align the market basket increases with the rising cost of treating patients.
Several commenters expressed concern that CMS' market basket forecast process relies on generalized hospital goods and services, which would not recognize the specialized training and experience IRFs require of their therapists, nurses, and other clinicians. The commenter also noted that IRFs typically pay higher costs for advanced rehabilitation technologies and specialized drugs that are likely not properly captured in the market basket.
Many commenters requested that CMS reexamine the current forecasting approach for determining the IRF PPS market basket update as well as the underlying construction of the market basket. Some commenters urged CMS to consider whether adjustments are necessary in its approach to annual market basket updates. Specifically, the commenters claimed that since the COVID-19 public health emergency, IGI's forecasted growth for the IRF market basket has shown a consistent trend of under-forecasting actual market basket growth. The commenters noted that while they are cognizant of the fact that forecasts will always be imperfect, in the past, they have been more balanced. However, the commenters argued that with four straight years of under-forecasts, they were concerned that there is a more systemic issue with IGI's forecasting. Therefore, the commenters stated that absent action from CMS, these missed forecasts are permanently established in the standard payment rate for IRFs and will continue to compound. In addition, the commenters claimed that these underpayments also influence other payments, including the growing Medicare Advantage patient population, as well as commercial insurer payment rates. The commenters further stated that in addition to inaccurate forecasts, the underlying market basket itself may have shortcomings that fail to properly capture growth. The commenters stated that it is confounding how hospitals, and especially labor-intensive IRFs, could have a change in the market basket that is significantly below general inflation. The commenters provided an example of one such factor may be CMS' use of the Employment Cost Index (ECI) to measure changes in labor compensation in the market basket. The commenters stated that the ECI may not be adequately capturing growth in the costs of employment and labor. However, the commenters claimed that this is just one example of a potential issue and encouraged CMS to thoroughly reexamine the market basket and its recent shortcomings to identify other potential areas for refinement. The commenters stated their support to work with CMS to assist with such an endeavor.
Response: We acknowledge and appreciate commenters' concerns regarding recent trends in inflation. We are required to update IRF PPS payments by the market basket update adjusted for productivity, as directed by section 1886(j)(3)(C) of the Act. Specifically, section 1886(j)(3)(C)(i) states that the increase factor shall be based on an appropriate percentage increase in a market basket of goods and services comprising services for which payment is made. In the FY 2024 IRF PPS final rule, we rebased the IRF market basket to reflect a 2021 base year ( 88 FR 50966 through 50982 ). We believe the increase in the 2021-based IRF market basket adequately reflects the average change in the price of goods and services hospitals purchase in order to provide IRF medical services and is technically appropriate to use as the IRF payment update factor.
The IRF market basket is a fixed-weight, Laspeyres-type index that measures the change in price over time of the same mix of goods and services purchased by IRFs in the base period. As we discussed in response to similar comments in the FY 2024 IRF PPS final rule ( 88 FR 50983 ), the IRF market basket update would reflect the prospective price pressures described by the commenters as increasing during a high inflation period but would inherently not reflect other factors that might increase the level of costs, such as the quantity of labor used. We note that cost changes (that is, the product of price and quantities) would only be reflected when a market basket is rebased, and the base year weights are updated to a more recent time period. Therefore, we believe the 2021-based IRF market basket appropriately reflects IRF cost structures.
To reflect expected price growth for each of the cost categories in the IRF market basket, we rely on impartial economic forecasts of the price proxies used in the market basket from IGI. We have consistently used the IGI economic price proxy forecasts in the market baskets used to update the IRF PPS payments since the implementation of the IRF PPS. For example, to measure price growth for IRF wages and salaries costs in the IRF market basket, since IRF-specific information is unavailable, we use the ECI for Wages and Salaries for All Civilian workers in Hospitals. As stated in the FY 2024 IRF final rule ( 88 FR 50978 ), we believe that this ECI is the best available price proxy to account for the occupational skill mix within IRFs and in the absence of an IRF-specific ECI, we believe that the highly skilled hospital workforce captured by the ECI for Wages and Salaries for All Civilian workers in Hospitals (inclusive of therapists, nurses, other clinicians, etc.) is a reasonable proxy for the compensation component of the IRF market basket.
IGI is a nationally recognized economic and financial forecasting firm with which CMS contracts to forecast the components of the market baskets. At the time of the FY 2025 IRF PPS proposed rule, based on IGI's fourth quarter 2023 forecast with historical data through the third quarter of 2023, the 2021-based IRF market basket update was forecasted to be 3.2 percent for FY 2025, reflecting forecasted compensation price growth of 3.7 percent (by comparison, compensation price growth in the IRF market basket averaged 2.8 percent from 2014 through 2023). We also note that when developing its forecast for labor prices, IHS Global Inc. considers overall labor market conditions (including rise in contract labor employment due to tight labor market conditions) as well as trends in contract labor wages, which both have an impact on wage pressures for workers employed directly by the hospital.
As is our general practice, in the FY 2025 IRF PPS proposed rule, we proposed that if more recent data became available, we would use such data, if appropriate, to derive the final FY 2025 IRF market basket update for the final rule. For this final rule, we now have an updated forecast of the price proxies underlying the market basket that incorporates more recent historical data and reflects a revised outlook regarding the U.S. economy and expected price inflation for FY 2025. Based on IGI's second quarter 2024 forecast with historical data through the first quarter of 2024, we are projecting a FY 2025 IRF market basket update of 3.5 percent (reflecting forecasted compensation price growth of 4.0 percent) and a productivity adjustment of 0.5 percentage point. Therefore, for FY 2025 a final IRF productivity-adjusted market basket update of 3.0 percent (3.5 percent less 0.5 percentage point) will be applicable, compared to the 2.8 percent market basket update that was proposed.
Furthermore, we acknowledge that while the projected IRF hospital market basket updates for FY 2021 through FY 2023 were under forecast (actual increases less forecasted increases were positive), this was largely due to unanticipated inflationary and labor market pressures as the economy emerged from the COVID-19 PHE. In addition, forecast errors have been both positive and negative. Only considering the forecast error for years when the IRF market basket update was lower than the actual market basket update does not consider the full experience and impact of forecast error.
Finally, we acknowledge the commenter's recommendation that we thoroughly reexamine the market basket to identify other potential areas for refinement. We continue to monitor any recent data on IRF cost structures, historical price growth, as well as updated forecasts of price pressures faced by IRFs. Any changes to the IRF market basket would be proposed in future rulemaking.
Comment: Many commenters expressed concern about the continued application of the productivity adjustment to IRFs. Commenters requested that CMS temporarily suspend the productivity adjustment to the IRF market basket due to recent declines in hospital productivity. One commenter urged CMS to use its “special exceptions and adjustments” authority to eliminate the productivity cut for FY 2025 and another commenter urged CMS to consider its regulatory authority to modify the productivity adjustment or make a PHE and inflation related exception in its application for the FY 2025 update. One commenter stated that due to the imbalance between the economy-wide productivity measure and IRFs, they encouraged CMS to explore all available avenues to provide additional financial relief for IRFs, working within the agency's existing authority under the statute. Other commenters respectfully requested CMS to carefully monitor the impact that these productivity adjustments will have on the rehabilitation hospital sector, provide feedback to Congress as appropriate, and reduce the productivity adjustment.
Response: Section 1886(j)(3)(C)(ii)(I) of the Act requires the application of the productivity adjustment, described in section 1886(b)(3)(xi)(II) of the Act, to the IRF PPS market basket increase factor. As required by statute, the FY 2025 productivity adjustment is derived based on the 10-year moving average growth in economy-wide productivity for the period ending FY 2025. We recognize the concerns of the commenters regarding the appropriateness of the productivity adjustment; however, we are required pursuant to section 1886(j)(3)(C)(ii)(I) of the Act to apply the specific productivity adjustment described here.
Comment: Many commenters urged CMS to explore all available options to update IRF PPS payments to ensure there are no disruptions in access to IRF services for Medicare beneficiaries. One commenter encouraged CMS to consider additional funding opportunities in the final rule either through an updated market basket or other allowable means.
One commenter requested CMS consider other methods and data sources to calculate the final rule “base” (before additional adjustments) market basket update that better reflects the rapidly increasing input prices facing IRFs. Specifically, the commenter requested that CMS consider using the average growth rate in allowable Medicare costs per risk adjusted discharge for IRF hospitals from IRF cost reports (both freestanding and sub-providers of an acute care hospital) for FY 2022 to calculate the FY 2025 final rule market basket update. The commenter stated that this growth rate will capture the increased cost of contract labor, unlike the proxy for labor cost growth currently used in the proposed market basket update. Based on their analysis, the commenter claimed that this would yield an unadjusted market basket update of 4.08 percent. The commenter stated that a net market basket update of 3.68 percent for FY 2025 better reflects the actual input price inflation hospitals anticipate facing in the coming year, rather than the 2.8 percent net market basket update proposed by CMS.
Another commenter requested that CMS apply a retrospective payment adjustment to account for the differences between the FY 2022 through 2024 market basket updates and the actual market basket. They stated that CMS is not required to use IHS Global Inc. data, or solely such data, as the basis for the IRF PPS increase factor and stated that CMS has the discretion to adjust the market basket update in order to account for any increased labor costs incurred by providers not currently reflected in a market basket data source(s). The commenter stated that CMS incorrectly dismissed the option of applying a special payment adjustment for IRFs in the FY 2023 IRF PPS Final Rule and the FY 2024 IRF PPS Final Rule. The commenter claimed that CMS' position is essentially that because the forecast was relatively accurate prior to the COVID-19 pandemic, it is acceptable to penalize IRFs with a less accurate payment update for the periods during and after the pandemic. However, the commenter claimed that the FY 2024 IRF final rule did not discuss the difference between the forecast and actual market basket update for periods after FY 2020, when the forecasted market basket update used for rate setting has consistently fallen far short of the actual market basket update.
A few commenters stated that considering this once-in-a-generation convergence of inflationary pressures and pandemic forces, they respectfully urged CMS to consider a one-time adjustment to the market basket update to account for forecast errors made during and after the PHE to ensure that the FY 2025 annual rate update is applied to a base rate that more accurately reflects the cost of IRF care and actual inflation experienced since the beginning of the pandemic. Specifically, a few commenters requested CMS adopt a one-time forecast error adjustment of 3.7 percentage point to the FY 2025 update based on the difference in the IRF PPS market basket percentage increase in FYs 2021, 2022, and 2023. Another commenter requested that CMS make a one-time 3.5 percentage points adjustment to the IRF market basket percentage increase in FY 2025 to account for the underpayments that occurred in FYs 2022 through 2024. One commenter requested an adjustment similar to the forecast error adjustments proposed in the FY 2025 SNF and IPPS Capital Input Price Index rules and requested that CMS apply this adjustment to a proposed FY 2025 IRF market basket update of 4.08 percent to result in a 7.78 percent update, prior to application of the 0.4 percent ACA productivity adjustment. The commenter claimed that nothing in Section 1886(j)(3) of the Act, that specifically precludes the use of a forecast error adjustment and that the word “prospective” is not used in Section 1886(j)(3)(C)(i) of the Act, to describe or modify the IRF “increase factor”, just that it is noted that the section requires that the factor be based on an “appropriate percentage increase.” One commenter also urged CMS to increase the market basket percentage increase when CMS determines actual market basket exceeds the forecasted market basket.
Response: As most recently discussed in the FY 2024 IRF PPS final rule, the IRF PPS market basket updates are set prospectively, which means that the market basket update relies on a mix of both historical data for part of the period for which the update is calculated and forecasted data for the remainder. For instance, the FY 2025 market basket update in this final rule reflects historical data through the first quarter of CY 2024 and forecasted data through the third quarter of CY 2025. While there is no precedent to adjust for market basket forecast error in the IRF payment update, a forecast error can be calculated by comparing the actual market basket increase for a given year less the forecasted market basket increase. Due to the uncertainty regarding future price trends, forecast errors can be both positive and negative. The cumulative forecast error since IRF PPS inception (FY 2003 to FY 2023) for the years where the payment update was not mandated by statute is 0.5 percent (cumulative forecasted increase was slightly lower than actual increase) and over the last ten years the cumulative forecast error is −0.1 percent (cumulative forecasted increase was slightly higher than actual increase). Though it is still too soon to know what the final IRF market basket forecast error is for FY 2024, so far it is 0.3 percent. Only considering the forecast error for years when the IRF market basket update was lower than the actual market basket update does not consider the full experience and impact of forecast error.
After careful consideration of public comments, we are finalizing a FY 2025 IRF productivity-adjusted market basket increase of 3.0 percent based on the most recent data available.
Section 1886(j)(6) of the Act specifies that the Secretary is to adjust the proportion (as estimated by the Secretary from time to time) of IRFs' costs that are attributable to wages and wage-related costs, of the prospective payment rates computed under section 1886(j)(3) of the Act, for area differences in wage levels by a factor (established by the Secretary) reflecting the relative hospital wage level in the geographic area of the rehabilitation facility compared to the national average wage level for such facilities. The labor-related share is determined by identifying the national average proportion of total costs that are related to, influenced by, or vary with the local labor market. We proposed to continue to classify a cost category as labor-related if the costs are labor-intensive and vary with the local labor market.
Based on our definition of the labor-related share and the cost categories in the 2021-based IRF market basket, we proposed to calculate the labor-related share for FY 2025 as the sum of the FY 2025 relative importance of Wages and Salaries, Employee Benefits, Professional Fees: Labor-Related, Administrative and Facilities Support Services, Installation, Maintenance, and Repair Services, All Other: Labor-Related Services, and a portion of the Capital-Related relative importance from the 2021-based IRF market basket. For more details regarding the methodology for determining specific cost categories for inclusion in the 2021-based IRF labor-related share, see the FY 2024 IRF PPS final rule ( 88 FR 50985 through 50988 ).
The relative importance reflects the different rates of price change for these cost categories between the base year (2021) and FY 2025. We proposed to calculate the labor-related relative importance from the IRF market basket, and it approximates the labor-related portion of the total costs after taking into account historical and projected price changes between the base year and FY 2025. The price proxies that move the different cost categories in the market basket do not necessarily change at the same rate, and the relative importance captures these changes. Based on IGI's fourth quarter 2023 forecast of the 2021-based IRF market basket, the sum of the FY 2025 relative importance for Wages and Salaries, Employee Benefits, Professional Fees: Labor-Related, Administrative and Facilities Support Services, Installation Maintenance & Repair Services, and All Other: Labor-Related Services was 70.5 percent. We proposed that the portion of Capital-Related costs that are influenced by the local labor market is 46 percent. Since the relative importance for Capital-Related costs was 8.1 percent of the 2021-based IRF market basket for FY 2025, we proposed to take 46 percent of 8.1 percent to determine the labor-related share of Capital-Related costs for FY 2025 of 3.7 percent. Therefore, we proposed a total labor-related share for FY 2025 of 74.2 percent (the sum of 70.5 percent for the proposed labor-related share of operating costs and 3.7 percent for the proposed labor-related share of Capital-Related costs). We also proposed that if more recent data became available after publication of the proposed rule and before the publication of the final rule (for example, a more recent estimate of the labor-related share), we would use such data, if appropriate, to determine the FY 2025 IRF labor-related share in the final rule.
Based on IGI's second quarter 2024 forecast for the 2021-based IRF market basket, the sum of the FY 2025 relative importance for Wages and Salaries, Employee Benefits, Professional Fees: Labor-related, Administrative and Facilities Support Services, Installation Maintenance & Repair Services, and All Other: Labor-Related Services is 70.7 percent. The portion of Capital-Related costs that is influenced by the local labor market is estimated to be 46 percent, which is the same percentage applied to the 2016-based IRF market basket ( 84 FR 39088 through 39089 ). Since the relative importance for Capital is 8.1 percent of the 2021-based IRF market basket in FY 2025, we took 46 percent of 8.1 percent to determine the labor-related share of Capital-Related costs for FY 2025 of 3.7 percent. Therefore, the total labor-related share for FY 2025 based on more recent data is 74.4 percent (the sum of 70.7 percent for the operating costs and 3.7 percent for the labor-related share of Capital-Related costs).
We invited public comment on the proposed labor-related share for FY 2025. The following is a summary of the public comments received and our responses:
Comment: One commenter appreciated that CMS only proposed to increase the labor-related share from 74.1 percent in FY 2024 to 74.2 percent in FY 2025. The commenter stated that although there is not a material increase in the wage percentage each increase to the labor-related share percentage penalizes any facility that has a wage index less than 1.0. The commenter stated that across the country, there is a growing disparity between high-wage and low-wage States that harms hospitals in many rural and underserved communities; limiting the increase in the labor-related share helps mitigate that growing disparity. However, another commenter believed that the 0.1 percentage point increase in the labor-related share update is inadequate and does not reflect the many challenges faced by health care facilities.
Response: We proposed to use the FY 2025 relative importance values for the labor-related cost categories from the 2021-based IRF market basket because it accounts for more recent data regarding price pressures and cost structure of IRFs. This methodology is consistent with the determination of the labor-related share since the implementation of the IRF PPS. As stated in the FY 2025 IRF proposed rule, we also proposed that if more recent data became available, we would use such data, if appropriate, to determine the FY 2025 labor-related share for the final rule. Based on IHS Global Inc.'s second quarter 2024 forecast with historical data through the first quarter of 2024, the FY 2025 labor-related share for the final rule is 74.4 percent.
After consideration of the public comments, we are finalizing a FY 2025 labor-related share of 74.4 percent. Table 4 shows the current estimate of the FY 2025 labor-related share and the FY 2024 final labor-related share using the 2021-based IRF market basket relative importance.
TABLE 4—FY 2025 IRF Labor-Related Share and FY 2024 IRF Labor-Related Share
Section 1886(j)(6) of the Act requires the Secretary to adjust the proportion of rehabilitation facilities' costs attributable to wages and wage-related costs (as estimated by the Secretary from time to time) by a factor (established by the Secretary) reflecting the relative hospital wage level in the geographic area of the rehabilitation facility compared to the national average wage level for those facilities. The Secretary is required to update the IRF PPS wage index on the basis of information available to the Secretary on the wages and wage-related costs to furnish rehabilitation services. Any adjustment or updates made under section 1886(j)(6) of the Act for a FY are made in a budget-neutral manner.
In the FY 2023 IRF PPS final rule ( 87 FR 47054 through 47056 ) we finalized a policy to apply a 5-percent cap on any decrease to a provider's wage index from its wage index in the prior year, regardless of the circumstances causing the decline. We amended IRF PPS regulations at § 412.624(e)(1)(ii) to reflect this permanent cap on wage index decreases. Additionally, we finalized a policy that a new IRF would be paid the wage index for the area in which it is geographically located for its first full or partial FY with no cap applied because a new IRF would not have a wage index in the prior FY. A full discussion of the adoption of this policy is found in the FY 2023 IRF PPS final rule.
For FY 2025, we maintained the policies and methodologies described in the FY 2024 IRF PPS final rule ( 88 FR 50956 ) related to the labor market area definitions and the wage index methodology for areas with wage data. Thus, we use the core based statistical areas (CBSAs) labor market area definitions and the FY 2025 pre-reclassification and pre-floor hospital wage index data. In accordance with section 1886(d)(3)(E) of the Act, the FY 2025 pre-reclassification and pre-floor hospital wage index is based on data submitted for hospital cost reporting periods beginning on or after October 1, 2020, and before October 1, 2021 (that is, FY 2021 cost report data).
The labor market designations made by the Office of Management and Budget (OMB) include some geographic areas where there are no hospitals and, thus, no hospital wage index data on which to base the calculation of the IRF PPS wage index. We continue to use the same methodology discussed in the FY 2008 IRF PPS final rule ( 72 FR 44299 ) to address those geographic areas where there are no hospitals and, thus, no hospital wage index data on which to base the calculation for the FY 2025 IRF PPS wage index. For FY 2025, the only rural area without wage index data available is in North Dakota. We have determined that the borders of 18 rural counties are local and contiguous with 8 urban counties. Therefore, under this methodology, the wage indexes for the counties of Burleigh/Morton/Oliver (CBSA 13900: 0.9020), Cass (CBSA 22020: 0.8763), Grand Forks (CBSA 24220: 0.7865), and McHenry/Renville/Ward (CBSA 33500: 0.7686) are averaged, resulting in an imputed rural wage index of 0.8334 for rural North Dakota for FY 2025. In past years for rural Puerto Rico, we did not apply this methodology due to the distinct economic circumstances there; due to the proximity of almost all of Puerto Rico's various urban and nonurban areas, this methodology would produce a wage index for rural Puerto Rico that is higher than that in half of its urban areas. However, because rural Puerto Rico now has hospital wage index data on which to base an area wage adjustment, we will not apply this policy for FY 2025. For urban areas without specific hospital wage index data, we will continue using the average wage indexes of all urban areas within the State to serve as a reasonable proxy for the wage index of that urban CBSA as proposed and finalized in FY 2006 ( 70 FR 47927 ). For FY 2025, the only urban area without wage index data available is CBSA 25980, Hinesville Fort Stewart, GA.
We invited public comment on the proposed Wage Adjustment for FY 2025. The following is a summary of the public comments received on the proposed revisions to the Wage Adjustment for FY 2025:
Comment: Several commenters suggested changes to the wage index methodology. Generally, commenters recommended that CMS use the same wage index adjustments for providers paid under the IPPS and under the IRF PPS in the same area. These recommendations were aimed at increasing parity between IPPS and IRF PPS hospitals. Most comments on this topic expressed concern over comparisons of shared labor markets. One commenter also voiced concerns that IPPS hospitals that have benefited from IPPS-specific geographic reclassification or other wage adjustments no longer put the same resources into the completion of Occupational Mix Surveys.
Several commenters specifically expressed support for the IPPS low wage index hospital policy, wherein wage index values are increased for the lowest quartile of the wage index values across all hospitals. These commenters urged CMS to develop and apply a corresponding low wage index hospital policy for IRFs. Commentors expressed concerns that the disparity in policy puts IRFs at a competitive disadvantage within shared labor markets and believed that extending the low wage index policy to IRFs would help maintain parity and ensure that low wage index and rural IRFs would have adequate resources to continue to provide access to care. Several commentors argued that this low wage index hospital policy to IRFs should be implemented without applying a budget neutrality adjustment.
Additionally, several commenters found the continued use of the pre-reclassification and pre-floor IPPS wage index unreasonable and urged CMS to revise its policy and apply the post-classification and post-floor hospital IPPS wage index to all IRFs, but especially the hospital-based distinct part units (DPUs). Like others, these commentors expressed concerns related to shared labor markets. Commenters believed that the current policy places inpatient hospital-based IRFs and other DPUs at a disadvantage in the labor markets in which they must compete with acute-care hospitals for staff. Additionally, several commenters suggested that CMS could leverage existing data to evaluate the policy change using the CMS Form 2552-96, Worksheet S-3, which captures “excluded area” salaries and wage-related costs.
Response: We appreciate the commenters' suggestion to adopt the IPPS low wage index hospital policy, post-classification and post-floor hospital IPPS wage index, and other IPPS wage index adjustments for the IRF wage index. We also acknowledge and appreciate the commenters' concerns regarding competition for labor resulting from different applicable wage index policies across different settings of care. While CMS and other interested parties have explored potential alternatives to the current wage index system in the past, no consensus has been achieved regarding how best to implement a replacement system that is evidence-based and data-driven. These concerns will be taken into consideration while we continue to explore potential wage index reforms and monitor IRF wage index policies.
As most recently discussed in the FY 2024 IRF PPS final rule ( 88 FR 50956 ), we would like to note that the IRF wage index is derived from IPPS wage data, that is, the pre-reclassification and pre-floor inpatient PPS (IPPS) wage index discussed in section D. of this final rule. Thus, to the extent that increasing wage index values under the IPPS for low wage index hospitals results in those hospitals increasing employee compensation, this increase would be reflected in the IPPS wage data that the IRF wage index is derived from and likely would result in higher wage indices for these areas under the IRF PPS. As such, any effects of this policy on the wage data of IPPS hospitals would be extended to the IRF setting, as this data would be used to establish the wage index for IRFs in the future. We note that IPPS wage index values are based on historical data and typically lag by four years.
As stated in prior years, as we do not have an IRF-specific wage index, we are unable to determine the degree, if any, to which these IPPS policies under the IRF PPS would be appropriate. However, CMS acknowledges that commenters have suggested that such data may be available in CMS Form 2552-96, Worksheet S-3 and will take this under consideration. Data pertaining to any IPPS policies that are applied to the pre-reclassification/pre-floor wage index is available in the FY 2024 IPPS proposed rule at https://www.cms.gov/medicare/medicare-fee-for-service-payment/acuteinpatientpps . The rationale for our current wage index policies was most recently published in the FY 2022 IRF PPS final rule ( 86 FR 42377 through 42378 ) and fully described in the FY 2006 IRF PPS final rule ( 70 FR 47880 , 47926 through 47928 ).
Comment: Several commenters voiced specific concerns about rising reliance on contract labor. The commenters stated that, as contract labor is generally not tied to the local economy, the local wage index is less and less reflective of the actual costs incurred by hospitals as the use of contract labor grows. Concerns about the rising use of contract labor were tied to concerns about workforce shortages, increasingly competitive labor markets, and the lack of parity between IRFs and IPPS hospitals in shared labor markets.
To address these challenges, several commentors encouraged CMS to explore how geographic differences in market wide labor costs and the increased use of contract labor impacts costs, and to make corresponding adjustments in policy.
Response: CMS acknowledges commenters' concerns that the current wage index policies may not capture or keep up with actual costs of care as well as specific concerns related to the cost of contract labor. As noted in the FY 2024 IRF PPS final rule ( 42 CFR 412 ), an analysis of Medicare cost report data for IPPS hospitals shows that contract labor hours accounted for about 4 percent of total compensation hours (reflecting employed and contract labor staff) in 2021. We will continue to monitor the trends in the increased use of contract labor.
Comment: Many commenters supported the existing 5 percent wage index cap and expressed appreciation of having a policy to cap and phase in the wage index changes that a provider can experience in a given year. However, at least one commenter remarked that, while they appreciate the cap policy, they believe that it does not do enough to correct the widening range in wage index amounts. Another commenter expressed frustration that the wage index values of the hospitals subject to the cap differ from the currently published tables and urged CMS to release wage index tables in the final rule that incorporate the cap on CBSAs that meet the 5 percent decrease criteria.
Response: We appreciate the commenters' support of the permanent cap on wage index decreases. We realize that the 5-percent cap on annual decreases in the wage index values does not entirely eliminate the effects of annual changes in the wage index, but we believe that it does substantially reduce the financial impact on IRFs of these annual changes. The wage index tables for IRF PPS are provided at the CBSA level. The 5-percent cap policy is applied at the provider level. Hence, when the 5-percent cap is applicable, each IRF should work directly with its MAC to understand how the 5-percent cap is applied. MACs have more detailed information about the location of each IRF and the applicability of the 5-percent cap to each IRFs situation, and CMS has provided careful instructions to the MACs on applying the 5-percent cap policy (see publication 100-04 Medicare Claims Processing Manual, Chapter 3).
After consideration of the comments we received, we are finalizing our proposals regarding the wage adjustment for FY 2025.
The wage index used for the IRF PPS is calculated using the pre-reclassification and pre-floor inpatient PPS (IPPS) wage index data and is assigned to the IRF on the basis of the labor market area in which the IRF is geographically located. IRF labor market areas are delineated based on the CBSAs established by the OMB. The CBSA delineations (which were implemented for the IRF PPS beginning with FY 2016) are based on revised OMB delineations issued on February 28, 2013, in OMB Bulletin No. 13-01. OMB Bulletin No. 13-01 established revised delineations for Metropolitan Statistical Areas, Micropolitan Statistical Areas, and Combined Statistical Areas in the United States and Puerto Rico based on the 2010 Census and provided guidance on the use of the delineations of these statistical areas using standards published in the June 28, 2010, Federal Register ( 75 FR 37246 through 37252 ). We refer readers to the FY 2016 IRF PPS final rule ( 80 FR 47068 through 47076 ) for a full discussion of our implementation of the OMB labor market area delineations beginning with the FY 2016 wage index.
Generally, OMB issues major revisions to statistical areas every 10 years, based on the results of the decennial census. Additionally, OMB occasionally issues updates and revisions to the statistical areas in between decennial censuses to reflect the recognition of new areas or the addition of counties to existing areas. In some instances, these updates merge formerly separate areas, transfer components of an area from one area to another or drop components from an area. On July 15, 2015, OMB issued OMB Bulletin No. 15-01, which provides minor updates to and supersedes OMB Bulletin No. 13-01 that was issued on February 28, 2013. The attachment to OMB Bulletin No. 15-01 provides detailed information on the update to statistical areas since February 28, 2013. The updates provided in OMB Bulletin No. 15-01 are based on the application of the 2010 Standards for Delineating Metropolitan and Micropolitan Statistical Areas to Census Bureau population estimates for July 1, 2012, and July 1, 2013.
In the FY 2018 IRF PPS final rule ( 82 FR 36250 through 36251 ), we adopted the updates set forth in OMB Bulletin No. 15-01 effective October 1, 2017, beginning with the FY 2018 IRF wage index. For a complete discussion of the adoption of the updates set forth in OMB Bulletin No. 15-01, we refer readers to the FY 2018 IRF PPS final rule. In the FY 2019 IRF PPS final rule ( 83 FR 38527 ), we continued to use the OMB delineations that were adopted beginning with FY 2016 to calculate the area wage indexes, with updates set forth in OMB Bulletin No. 15-01 that we adopted beginning with the FY 2018 wage index.
On August 15, 2017, OMB issued OMB Bulletin No. 17-01, which provided updates to and superseded OMB Bulletin No. 15-01 that was issued on July 15, 2015. The attachments to OMB Bulletin No. 17-01 provide detailed information on the update to statistical areas since July 15, 2015, and are based on the application of the 2010 Standards for Delineating Metropolitan and Micropolitan Statistical Areas to Census Bureau population estimates for July 1, 2014, and July 1, 2015. In the FY 2020 IRF PPS final rule ( 84 FR 39090 through 39091 ), we adopted the updates set forth in OMB Bulletin No. 17-01 effective October 1, 2019, beginning with the FY 2020 IRF wage index.
On April 10, 2018, OMB issued OMB Bulletin No. 18-03, which superseded the August 15, 2017, OMB Bulletin No. 17-01, and on September 14, 2018, OMB issued OMB Bulletin No. 18-04, which superseded the April 10, 2018 OMB Bulletin No. 18-03. These bulletins established revised delineations for Metropolitan Statistical Areas, Micropolitan Statistical Areas, and Combined Statistical Areas, and provided guidance on the use of the delineations of these statistical areas. A copy of this bulletin may be obtained at https://www.whitehouse.gov/wp-content/uploads/2018/09/Bulletin-18-04.pdf .
To this end, as discussed in the FY 2021 IRF PPS proposed ( 85 FR 22075 through 22079 ) and final ( 85 FR 48434 through 48440 ) rules, we adopted the revised OMB delineations identified in OMB Bulletin No. 18-04 (available at https://www.whitehouse.gov/wp-content/uploads/2018/09/Bulletin-18-04.pdf ) beginning October 1, 2020, including a 1-year transition for FY 2021 under which we applied a 5-percent cap on any decrease in an IRF's wage index compared to its wage index for the prior fiscal year (FY 2020). The updated OMB delineations more accurately reflect the contemporary urban and rural nature of areas across the country, and the use of such delineations allows us to determine more accurately the appropriate wage index and rate tables to apply under the IRF PPS. OMB issued further revised CBSA delineations in OMB Bulletin No. 20-01, on March 6, 2020 (available on the web at https://www.whitehouse.gov/wp-content/uploads/2020/03/Bulletin-20-01.pdf ). However, we determined that the changes in OMB Bulletin No. 20-01 do not impact the CBSA-based labor market area delineations adopted in FY 2021. Therefore, we did not propose to adopt the revised OMB delineations identified in OMB Bulletin No. 20-01 for FY 2022 through FY 2024.
On July 21, 2023, OMB issued OMB Bulletin No. 23-01 (available at https://www.whitehouse.gov/wp-content/uploads/2023/07/OMB-Bulletin-23-01.pdf ) which updates and supersedes OMB Bulletin No. 20-01 based upon the 2020 Standards for Delineating Core Based Statistical Areas (“the 2020 Standards”) published by OMB on July 16, 2021 ( 86 FR 37770 ). OMB Bulletin No. 23-01 revised CBSA delineations which are comprised of counties and equivalent entities (for example, boroughs, a city and borough, and a municipality in Alaska, planning regions in Connecticut, parishes in Louisiana, municipios in Puerto Rico, and independent cities in Maryland, Missouri, Nevada, and Virginia). For FY 2025, we proposed to adopt the revised OMB delineations identified in OMB Bulletin No. 23-01.
As previously discussed, we are implementing the new OMB statistical area delineations (based upon the 2020 decennial Census data) beginning in FY 2025 for the IRF PPS wage index. Our analysis shows that a total of 54 counties (and county equivalents) that are currently considered part of an urban CBSA would be considered located in a rural area, for IRF PPS payment beginning in FY 2025, if we adopt the new OMB delineations. Table 5 lists the 54 urban counties that will be rural now that we are finalizing our proposal to implement the new OMB delineations.

We are finalizing our proposal that the wage data for all hospitals located in the counties listed in Table 5 now be considered rural when their respective State's rural wage index value is calculated. This rural wage index value would be used under the IRF PPS.
Analysis of the new OMB delineations (based upon the 2020 decennial Census data) shows that a total of 54 counties (and county equivalents) that are currently located in rural areas would be in urban areas based on finalizing our proposal to implement the new OMB delineations. Table 6 lists the 54 rural counties that will be urban after we finalize this proposal.

We proposed and are finalizing that when calculating the area wage index, the wage data for hospitals located in these counties would be included in their new respective urban CBSAs.
In addition to rural counties becoming urban and urban counties becoming rural, several urban counties would shift from one urban CBSA to another urban CBSA after we adopt the new OMB delineations. In other cases, if we adopt the new OMB delineations, counties would shift between existing and new CBSAs, changing the constituent makeup of the CBSAs.
In one type of change, an entire CBSA would be subsumed by another CBSA. For example, CBSA 31460 (Madera, CA) currently is a single county (Madera, CA) CBSA. Madera County would be a part of CBSA 23420 (Fresno, CA) under the new OMB delineations.
In another type of change, some CBSAs have counties that would split off to become part of, or to form, entirely new labor market areas. For example, CBSA 29404 (Lake County-Kenosha County, IL-WI) currently is comprised of two counties (Lake County, IL and Kenosha County, WI). Under the new OMB delineations, Kenosha County would split off and form the new CBSA 28450 (Kenosha, WI), while Lake County would remain in CBSA 29404.
Finally, in some cases, a CBSA would lose counties to another existing CBSA if we adopt the new OMB delineations. For example, Meade County, KY, would move from CBSA 21060 (Elizabethtown-Fort Knox, KY) to CBSA 31140 (Louisville/Jefferson County, KY-IN). CBSA 21060 would still exist in the new labor market delineations with fewer constituent counties. Table 7 lists the urban counties that would move from one urban CBSA to another urban CBSA under the new OMB delineations.

If providers located in these counties move from one CBSA to another under the new OMB delineations, there may be impacts, both negative and positive, upon their specific wage index values.
In other cases, adopting the revised OMB delineations would involve a change only in CBSA name and/or number, while the CBSA continues to encompass the same constituent counties. For example, CBSA 19430 (Dayton-Kettering, OH) would experience a change to its name and become CBSA 19430 (Dayton-Kettering-Beavercreek, OH), while all of its three constituent counties would remain the same. We consider these changes (where only the CBSA name and/or number would change) to be inconsequential changes with respect to the IRF PPS wage index. Table 8 sets forth a list of such CBSAs where there would be a change in CBSA name and/or number only if we adopt the revised OMB delineations.

The June 6, 2022, Census Bureau Notice ( 87 FR 34235-34240 ), OMB Bulletin No. 23-01 replaced the 8 counties in Connecticut with 9 new “Planning Regions.” Planning regions now serve as county-equivalents within the CBSA system. We are adopting the planning regions as county equivalents for wage index purposes. We believe it is necessary to adopt this migration from counties to planning region county-equivalents in order to maintain consistency with OMB updates. We are providing the following crosswalk with the current and as finalized FIPS county and county-equivalent codes and CBSA assignments.
| FIPS | Current County | Current CBSA | FIPS | Proposed planning region area (County Equivalent) | CBSA |
|---|---|---|---|---|---|
| 9003 | Hartford | 25540 | 9110 | Capitol | 25540 |
| 9015 | Windham | 49340 | 9150 | Northeastern Connecticut | 7 |
| 9005 | Litchfield | 7 | 9160 | Northwest Hills | 7 |
| 9001 | Fairfield | 14860 | 9190 | Western Connecticut | 14860 |
| 9011 | New London | 35980 | 9180 | Southeastern Connecticut | 35980 |
| 9013 | Tolland | 25540 | 9110 | Capitol | 25540 |
| 9009 | New Haven | 35300 | 9170 | South Central Connecticut | 35300 |
| 9007 | Middlesex | 25540 | 9130 | Lower Connecticut River Valley | 25540 |
Overall, we believe that implementing the new OMB delineations would result in wage index values being more representative of the actual costs of labor in a given area. We recognize that some providers (10 percent) would have a higher wage index due to our implementation of the new labor market area delineations. However, we also recognize that more providers (16 percent) would experience decreases in wage index values as a result of our implementation of the new labor market area delineations. Our analysis for the FY 2025 final rule indicates that 16 IRFs will experience a change in either rural or urban designations. Of these, 8 facilities designated as rural in FY 2024 would be designated as urban in FY 2025. Based upon the CBSA delineations, those rural IRFs that change from rural to urban would lose the 14.9 percent rural adjustment. To mitigate the financial impacts of this loss, we proposed a transition for these facilities, as discussed further below.
CMS recognizes that IRFs in certain areas may experience reduced payments due to the adoption of the revised OMB delineations and is finalizing transition policies to mitigate negative financial impacts and provide stability to year-to-year wage index variations. In the FY 2021 final rule ( 85 FR 48434 ), CMS finalized a wage index transition policy to apply a 5-percent cap for IRFs that may experience decreases in their final wage index from the prior fiscal year. In FY 2023, the 5-percent cap policy was made permanent. This 5-percent cap on reductions policy is discussed in further detail in FY 2023 final rule at 87 FR 47054 through 47056 . It is CMS' long held opinion that revised labor market delineations should be adopted as soon as is possible to maintain the integrity of the wage index system. We believe the 5-percent cap policy will sufficiently mitigate significant disruptive financial impacts on hospitals negatively affected by the adoption of the revised OMB delineations. Besides the rural adjustment transition discussed immediately below, we do not believe any additional transition is necessary considering that the current cap on wage index decreases, which was not in place when implementing prior decennial census updates in FY 2006 and FY 2015, ensures that an IRFs wage index would not be less than 95 percent of its final wage index for the prior year.
Consistent with the transition policy adopted in FY 2006 ( 70 FR 47923 [ 4 ] through 47927 [ 5 ] ), we considered the appropriateness of applying a 3-year phase-out of the rural adjustment for IRFs located in rural counties that would become urban under the new OMB delineations, given the potentially significant payment impacts for these facilities. We continue to believe, as discussed in the FY 2006 IRF final rule ( 70 FR 47880 [ 6 ] ), that the phase-out of the rural adjustment transition period for these facilities specifically is appropriate because, as a group, we expect these IRFs would experience a steeper and more abrupt reduction in their payments compared to other IRFs. Therefore, we are finalizing a budget neutral three-year phase-out of the rural adjustment for existing FY 2024 rural IRFs that will become urban in FY 2025 and that experience a loss in payments due to changes from the new CBSA delineations. Accordingly, the incremental steps needed to reduce the impact of the loss of the FY 2024 rural adjustment of 14.9 percent will be phased out over FYs 2025, 2026, and 2027. This policy will allow rural IRFs which would be classified as urban in FY 2025 to receive two-thirds of the 2024 rural adjustment for FY 2025. For FY 2026, these IRFs will receive the full FY 2026 wage index and one-third of the FY 2024 rural adjustment. For FY 2027, these IRFs will receive the full FY 2027 wage index without a rural adjustment. We believe a three-year budget-neutral phase-out of the rural adjustment for IRFs that transition from rural to urban status under the new CBSA delineations would best accomplish the goals of mitigating the loss of the rural adjustment for existing FY 2024 rural IRFs. The purpose of the gradual phase-out of the rural adjustment for these facilities is to alleviate the significant payment implications for existing rural IRFs that may need time to adjust to the loss of their FY 2024 rural payment adjustment or that experience a reduction in payments solely because of this redesignation. As stated, this policy is specifically for rural IRFs that become urban in FY 2025 and that experience a loss in payments due to changes from the new CBSA delineations. Thus, we are not implementing a transition policy for urban facilities that become rural in FY 2025 because these IRFs will receive the full rural adjustment of 14.9 percent beginning October 1, 2024.
We invited public comment on the proposed implementation of revised labor market area delineations and on the proposed transition policy for rural IRFs that would be designated as urban under the new CBSA delineations.
The following is a summary of the public comments received on the proposed implementation of the revised labor market area delineations and the proposed transition policy:
Comment: Overall, many commenters supported the adoption of OMB's CBSA delineation revisions. Several others voiced appreciation for CMS' inclusion of a transition policy to reduce the impact of the CBSA delineation changes, without voicing any opposition to the adoption of the new delineations. However, some commenters specifically opposed the adoption of OMB's CBSA delineation revisions. The commenters stated that both OMB guidance and the Metropolitan Areas Protection and Standardization Act (MAPS) ( Public Law 117-219 ) support that, if CMS chooses to adopt new OMB delineations, CMS must fully explain why reliance on the updated CBSAs as set forth by OMB is appropriate for purposes of the FY 2025 wage index adjustments. The commenters stated that CMS has not provided any rationale or explanation for why relying on the updated CBSAs is appropriate. Rather than simply adopting the OMB CBSAs by default, the commenters stated that CMS must make a fact-specific determination of those CBSAs' suitability for Medicare reimbursement purposes, including whether it would be appropriate to use additional data to modify OMB's delineation to ensure that such changes are appropriate for purposes of defining regional labor markets for IRF workers.
Response: We appreciate the majority of commenters' support for the adoption of OMB's CBSA delineation revisions and recognize others' opposition. We do not agree with the commenters' assessment that CMS has not provided a rationale for the proposed adoption of the revised CBSA delineations for FY 2025. The MAPS Act specifically states that “this act limits the automatic application of, and directs the Office of Management and Budget (OMB) to provide information about, changes to the standards for designating a core-based statistical area (CBSA) . . .” We believe that our proposed rule meets the requirements of the MAPS Act because we have not automatically applied the revised CBSAs outlined in OMB Bulletin 23-01. Rather, as we noted in the proposed rule, we proposed the adoption of the revised CBSA delineations because we believe it is important for the IRF PPS to use, as soon as is reasonably possible, the latest available labor market area delineations to maintain a more accurate and up-to-date payment system that reflects the reality of population shifts and labor market conditions. We also believe that using the most current delineations increase the integrity of the IRF PPS wage index system by creating a more accurate representation of geographic variations in wage levels.
With respect to the suggestion that CMS consider whether it would be appropriate to use additional data to modify OMB's delineation to ensure that such changes are appropriate for purposes of defining regional labor markets for IRF workers, we do not believe that the use of such additional data is appropriate. As we have previously discussed in the FY 2016 final rule ( 80 FR 47069 ) and as we noted earlier in this final rule, we believe that the labor market area in which the IRF is geographically located is most appropriate for determining the wage adjustment. Accordingly, we do not believe it would be appropriate to use additional data to modify OMB's delineations, for the same reasons we previously stated with regard to floors or reclassifications. For example, using additional data to modify OMB's CBSA delineations would significantly increase administrative burden, both for IRFs and for CMS, associated with particular geographical areas or even individual IRFs moving from one CBSA to another, and it would significantly increase the complexity of the methodology.
Furthermore, because all CBSA delineation changes would be applied budget-neutrally under the wage index, these policies would increase the wage index for some IRFs while reducing IRF PPS payments for all other IRFs, which would be a departure from our longstanding policies that IRFs have relied on for many years. For these reasons, we continue to believe it is important for the IRF PPS to use the latest available labor market area delineations, based on the latest available CBSA delineations established by OMB as soon as is reasonably possible in order to maintain a more accurate and up-to-date payment system that reflects the reality of population shifts and labor market conditions. We further believe that using the delineations reflected in OMB Bulletin No. 23-01 would increase the integrity of the IRF PPS wage index system by creating a more accurate representation of geographic variations in wage levels. Therefore, we believe that it is appropriate to implement the new OMB delineations without delay.
Comment: Public comments generally all supported the phase-out policy for IRFs being reclassified from rural to urban CBSAs. Commenters expressed that this phase-out policy for loss of the rural adjustment is a reasonable way to ensure that no IRF faces a dramatic cut to its reimbursement as a result of the new CBSA delineation. A few commentors specifically noted that while they appreciate the existing permanent 5-percent cap policy, they do not believe that it is sufficient to mitigate the impact of the CBSA change, and therefore supported the implementation of a 3-year wage index transition period to allow for a wage index transition consistent with prior updates to the CBSA categorization.
Response: We appreciate the commenters' support for a 3-year phase-out of the rural adjustment for FY 2024 rural IRFs that will be considered urban in FY 2025 and for supporting the CBSA change in conjunction with applying the existing permanent 5-percent cap policy. We believe that the existing permanent 5-percent cap policy substantially mitigates the financial impact on IRFs of the updated CBSA market area delineations, and we believe that phasing in these new CBSA market area delineations over 3 years would be overly complex to administer and is therefore not the best approach. We will continue monitoring the effects of the wage index updates to ensure that the permanent 5-percent cap policy is adequately mitigating any substantial decreases in wage index values.
After consideration of the comments we received, we are finalizing our proposal to adopt the revised OMB delineations contained in OMB Bulletin No. 23-01 as well as our proposal to implement a budget neutral three-year phase-out of the rural adjustment for existing FY 2024 rural IRFs that will become urban in FY 2025.
The proposed wage index applicable to FY 2025 is set forth in Table A and Table B available on the CMS website at https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/InpatientRehabFacPPS/IRF-Rules-and-Related-Files.html .
To calculate the wage-adjusted facility payment for the payment rates set forth in this final rule, we multiply the unadjusted Federal payment rate for IRFs by the FY 2025 labor-related share based on the 2021-based IRF market basket relative importance (74.4 percent) to determine the labor-related portion of the standard payment amount. (A full discussion of the calculation of the labor-related share appears in section VI.E. of this final rule.) We then multiply the labor-related portion by the applicable IRF wage index. The wage index tables are available on the CMS website at https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/InpatientRehabFacPPS/IRF-Rules-and-Related-Files.html .
Adjustments or updates to the IRF wage index made under section 1886(j)(6) of the Act must be made in a budget-neutral manner. We calculate a budget-neutral wage adjustment factor as established in the FY 2004 IRF PPS final rule ( 68 FR 45689 ) and codified at § 412.624(e)(1), as described in the steps below. We use the listed steps to ensure that the FY 2025 IRF standard payment conversion factor reflects the update to the wage indexes (based on the FY 2021 hospital cost report data) and the update to the labor-related share, in a budget-neutral manner:
Step 1. Calculate the total amount of estimated IRF PPS payments using the labor-related share and the wage indexes from FY 2024 (as published in the FY 2024 IRF PPS final rule ( 88 FR 50956 )).
Step 2. Calculate the total amount of estimated IRF PPS payments using the FY 2025 wage index values (based on updated hospital wage data and considering the permanent cap on wage index decreases policy) and the FY 2025 labor-related share of 74.4 percent.
Step 3. Divide the amount calculated in Step 1 by the amount calculated in Step 2. The resulting quotient is the FY 2025 budget-neutral wage adjustment factor of 0.9924.
Step 4. Apply the budget neutrality factor from Step 3 to the FY 2025 IRF PPS standard payment amount after the application of the increase factor to determine the FY 2025 standard payment conversion factor.
We discuss the calculation of the standard payment conversion factor for FY 2025 in section VI.G. of this final rule.
We invited public comment on our proposals regarding the Wage Adjustment for FY 2025.
Comment: Several commentors specified that the wage index cap policy should be implemented without applying a budget neutrality adjustment.
Response: We do not believe that the permanent 5-percent cap policy for the IRF wage index should be applied in a non-budget-neutral manner. As a matter of fact, the statute at section 1886(j)(6) of the Act requires that adjustments for geographic variations in labor costs for a FY be made in a budget-neutral manner. We refer readers to the FY 2023 IRF PPS final rule ( 87 FR 47054 through 47056 ) for a detailed discussion on the wage index cap policy.
As a result of the public comments, we are finalizing our proposals regarding the IRF budget neutral wage adjustment factor methodology for FY 2025.
To calculate the standard payment conversion factor for FY 2025, as illustrated in Table 10, we begin by applying the finalized increase factor for FY 2025, as adjusted in accordance with sections 1886(j)(3)(C) of the Act, to the standard payment conversion factor for FY 2024 ($18,541). Applying the 3.0 productivity-adjusted market basket increase factor for FY 2025 to the standard payment conversion factor for FY 2024 of $18,541 yields a standard payment amount of $19,097. Then, we apply the budget neutrality factor for the FY 2025 wage index (taking into account the policy placing a permanent cap on decreases in the wage index), and labor-related share of 0.9924, which results in a standard payment amount of $18,592. We next apply the budget neutrality factor for the CMG relative weights of 0.9976, which results in the standard payment conversion factor of $18,907 for FY 2025.
We invited public comment on the proposed FY 2025 standard payment conversion factor.
We did not receive any comments on our proposed FY 2025 standard payment conversion factor, and therefore, we are finalizing the revisions as proposed.
| Explanation for Adjustment | Calculations |
|---|---|
| FY 2024 Standard Payment Conversion Factor | $18,541 |
| Market Basket Increase Factor for FY 2025 (3.5%), reduced by 0.5 percentage point for the productivity adjustment as required by section 1886(j)(3)(C)(ii)(I) of the Act | × 1.030 |
| Budget Neutrality Factor for the Updates to the Wage Index and Labor-Related Share | × 0.9924 |
| Budget Neutrality Factor for the Revisions to the CMG Relative Weights | × 0.9976 |
| FY 2025 Standard Payment Conversion Factor | = $18,907 |
We then apply the CMG relative weights described in section IV. of this final rule to the FY 2025 standard payment conversion factor ($18,907), to determine the unadjusted IRF prospective payment rates for FY 2025. The unadjusted prospective payment rates for FY 2025 are shown in Table 11.

Table 12 illustrates the methodology for adjusting the prospective payments (as described in section V. of this final rule). The following examples are based on two hypothetical Medicare beneficiaries, both classified into CMG 0104 (without comorbidities). The unadjusted prospective payment rate for CMG 0104 (without comorbidities) appears in Table 11.
Example: One beneficiary is in Facility A, an IRF located in rural Spencer County, Indiana, and another beneficiary is in Facility B, an IRF located in urban Harrison County, Indiana. Facility A, a rural non-teaching hospital has a Disproportionate Share Hospital (DSH) percentage of 5 percent (which would result in a LIP adjustment of 1.0156), a wage index of 0.8657, and a rural adjustment of 14.9 percent. Facility B, an urban teaching hospital, has a DSH percentage of 15 percent (which would result in a LIP adjustment of 1.0454 percent), a wage index of 0.9068, and a teaching status adjustment of 0.0784.
To calculate each IRF's labor and non-labor portion of the prospective payment, we begin by taking the FY 2025 unadjusted prospective payment rate for CMG 0104 (without comorbidities) from Table 11. Then, we multiply the labor-related share for FY 2025 (74.4 percent) described in section VI. of this final rule by the unadjusted prospective payment rate. To determine the non-labor portion of the prospective payment rate, we subtract the labor portion of the Federal payment from the unadjusted prospective payment.
To compute the wage-adjusted prospective payment, we multiply the labor portion of the Federal payment by the appropriate wage index located in the applicable wage index table. This table is available on the CMS website at https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/InpatientRehabFacPPS/IRF-Rules-and-Related-Files.html .
The resulting figure is the wage-adjusted labor amount. Next, we compute the wage-adjusted Federal payment by adding the wage-adjusted labor amount to the non-labor portion of the Federal payment.
Adjusting the wage-adjusted Federal payment by the facility-level adjustments involves several steps. First, we take the wage-adjusted prospective payment and multiply it by the appropriate rural and LIP adjustments (if applicable). Second, to determine the appropriate amount of additional payment for the teaching status adjustment (if applicable), we multiply the teaching status adjustment (0.0784, in this example) by the wage-adjusted and rural-adjusted amount (if applicable). Finally, we add the additional teaching status payments (if applicable) to the wage, rural, and LIP-adjusted prospective payment rates. Table 12 illustrates the components of the adjusted payment calculation.

Thus, the adjusted payment for Facility A would be $30,649.63, and the adjusted payment for Facility B would be $30,519.74.
Section 1886(j)(4) of the Act provides the Secretary with the authority to make payments in addition to the basic IRF prospective payments for cases incurring extraordinarily high costs. A case qualifies for an outlier payment if the estimated cost of the case exceeds the adjusted outlier threshold. We calculate the adjusted outlier threshold by adding the IRF PPS payment for the case (that is, the CMG payment adjusted by all of the relevant facility-level adjustments) and the adjusted threshold amount (also adjusted by all of the relevant facility-level adjustments). Then, we calculate the estimated cost of a case by multiplying the IRF's overall Cost-to-Charge Ratio (CCR) by the Medicare allowable covered charge. If the estimated cost of the case is higher than the adjusted outlier threshold, we make an outlier payment for the case equal to 80 percent of the difference between the estimated cost of the case and the outlier threshold.
In the FY 2002 IRF PPS final rule ( 66 FR 41362 through 41363 ), we discussed our rationale for setting the outlier threshold amount for the IRF PPS so that estimated outlier payments would equal 3 percent of total estimated payments. For the FY 2002 IRF PPS final rule, we analyzed various outlier policies using 3, 4, and 5 percent of the total estimated payments, and we concluded that an outlier policy set at 3 percent of total estimated payments would optimize the extent to which we could reduce the financial risk to IRFs of caring for high cost- patients, while still providing for adequate payments for all other (non-high cost outlier) cases.
Subsequently, we updated the IRF outlier threshold amount in the FYs 2006 through 2024 IRF PPS final rules and the FY 2011 and FY 2013 notices ( 70 FR 47880 , 71 FR 48354 , 72 FR 44284 , 73 FR 46370 , 74 FR 39762 , 75 FR 42836 , 76 FR 47836 , 76 FR 59256 , 77 FR 44618 , 78 FR 47860 , 79 FR 45872 , 80 FR 47036 , 81 FR 52056 , 82 FR 36238 , 83 FR 38514 , 84 FR 39054 , 85 FR 48444 , 86 FR 42362 , 87 FR 47038 , and 88 FR 50956 respectively) to maintain estimated outlier payments at 3 percent of total estimated payments. We also stated in the FY 2009 final rule ( 73 FR 46370 at 46385) that we would continue to analyze the estimated outlier payments for subsequent years and adjust the outlier threshold amount as appropriate to maintain the 3 percent target.
To update the IRF outlier threshold amount for FY 2025, we proposed to use FY 2023 claims data and the same methodology that we used to set the initial outlier threshold amount in the FY 2002 IRF PPS final rule ( 66 FR 41362 through 41363 ), which is also the same methodology that we used to update the outlier threshold amounts for FYs 2006 through 2024. The outlier threshold is calculated by simulating aggregate payments and using an iterative process to determine a threshold that results in outlier payments being equal to 3 percent of total payments under the simulation. To determine the outlier threshold for FY 2025, we estimated the amount of FY 2025 IRF PPS aggregate and outlier payments using the most recent claims available (FY 2023) and the FY 2025 standard payment conversion factor, labor-related share, and wage indexes, incorporating any applicable budget-neutrality adjustment factors. The outlier threshold is adjusted either up or down in this simulation until the estimated outlier payments equal 3 percent of the estimated aggregate payments. Based on an analysis of the preliminary data used for the proposed rule, we estimated that IRF outlier payments as a percentage of total estimated payments would be approximately 3.2 percent in FY 2024. Therefore, we proposed to update the outlier threshold amount from $10,423 for FY 2024 to $12,158 for FY 2025 to maintain estimated outlier payments at approximately 3 percent of total estimated aggregate IRF payments for FY 2025.
We note that, as we typically do, we will update our data between the FY 2025 IRF PPS proposed and final rules to ensure that we use the most recent available data in calculating IRF PPS payments. This updated data includes a more complete set of claims for FY 2023. Based on our analysis using this updated data, we estimate that IRF outlier payments as a percentage of total estimated payments are approximately 3.2 percent in FY 2024. Therefore, we will update the outlier threshold amount from $10,423 for FY 2024 to $12,043 for FY 2025 to account for the increases in IRF PPS payments and estimated costs and to maintain estimated outlier payments at approximately 3 percent of total estimated aggregate IRF payments for FY 2025.
We invited public comment on the proposed update to the IRF outlier threshold for FY 2025. The following is a summary of the public comments received on our proposed update to the IRF outlier threshold:
Comment: Commenters were mixed in their support of the proposed high-cost outlier threshold, although more commentors supported the proposed threshold than opposed it. Those that supported the proposed threshold indicated support of CMS' policy to keep the outlier payments at 3 percent of total payments. However, these supporters also expressed concern over the lack of stability and predictability in the threshold, stating that the lack of stability makes it difficult for facilities to budget and poses challenges to IRFs that treat a large number of complex patients. One commenter expressed concern over the reduction in outlier payments during a time when increasing costs are outside of the hospital's control. Many suggested modifications to the outlier threshold methodology.
Response: We appreciate the commenters' support of the current 3 percent outlier threshold policy and recognize the commenters' concern regarding a reduction in outlier payments this year, and the commenters' desire for increased stability and predictability in the threshold from year-to-year. It has been our long-standing practice to utilize the most recent full fiscal year of data to update the prospective payment rates and determine the outlier threshold amount, as this data is generally considered to be the best overall predictor of experience in the upcoming fiscal year. Additionally, we continue to believe that maintaining the outlier pool at 3 percent of aggregate IRF payments optimizes the extent to which we can reduce financial risk to IRFs of caring for highest-cost patients, while still providing for adequate payments for all other non-outlier cases.
Although we recognize commenters' concerns about increasing IRF costs, we do not believe that it would be appropriate to address these concerns through the outlier payment policy. The outlier payment policy is designed to compensate IRFs for treating unusually high-cost patients, not for addressing overall inflationary pressures that increase the costs of caring for all IRF patients.
We will continue to examine ways of enhancing the stability and predictability of the outlier threshold from year to year. However, since 3 percent was deducted from IRF payments in the beginning of the IRF PPS to fund the outlier pool, we do not believe that it would be appropriate to deliberately pay more than 3 percent in outlier payments to IRFs in a given year, as that additional funding would increase overall payments to IRFs. Thus, we believe that any changes to the outlier threshold methodology to make it more stable and predictable would still need to maintain the integrity of the outlier pool, which is currently set at 3 percent. CMS will continue to monitor year-to-year changes in the outlier threshold and the impact of these changes on payment.
Comment: Several commenters expressed concerns that outlier payments may not be consistently targeted towards patients who require more intensive or complex services with related higher costs. Some of the commenters believed that factors other than patient complexity and case mix may be driving these payments. One commenter presented analysis to support their claim that inefficient cost structures, rather than highly complex patients, appear to be driving the distribution of overall IRF outlier payments, potentially resulting in patients at IRFs that warrant an outlier payment not receiving one. Moreover, many commenters expressed concern that outlier payments are being concentrated among an increasingly small number of providers. Several of these comments urged CMS to analyze the increasing concentration of outlier payments and make such analysis publicly accessible.
Response: We acknowledge commenters' concerns that outlier payments may be concentrated among a small subset of providers and may not be consistently targeted towards patients with intensive or complex needs. As most recently discussed in the FY 2024 IRF PPS Final Rule ( 88 FR 68494 ), our outlier policy is intended to reimburse IRFs for treating extraordinarily costly cases. Any future consideration given to imposing a limit on outlier payments or adjusting the outlier threshold to account for historical outlier reconciliation dollars would need to be carefully assessed and take into consideration the effect on access to IRF care for certain high-cost populations. We continue to believe that maintaining the outlier pool at 3 percent of aggregate IRF payments optimizes the extent to which we can reduce financial risk to IRFs caring for highest-cost patients, while still providing for adequate payments for all other non-outlier cases. We appreciate the commenters' suggestions for additional analysis on our methodology and will take them into consideration as we continue to assess our outlier threshold.
Comment: Many commenters provided suggestions to improve the high-cost outlier threshold methodology. By far the most frequent suggestion was for CMS to consider implementing a 3-year rolling average as a stabilizing factor for the outlier threshold, similar to the method used for the facility-level adjustments in the past. Commenters suggested that this methodology could reduce the annual outlier changes and provide greater predictability for the field. Several comments also suggested that CMS consider developing and implementing an outlier reconciliation policy for the IRF PPS, similar to the one used in IPPS. Other, less frequent suggestions that commenters offered were the following: establishing an outlier baseline and then increasing the outlier threshold each year by the approved market basket percentage increase, capping the overall outlier payments an IRF can receive, and reducing the overall 3 percent outlier pool.
Response: We thank the commenters for their suggestions regarding the outlier threshold. We appreciate the suggestion to modify the outlier threshold methodology to use a 3-year average; however, it has been our practice to utilize the most recent full fiscal year of data to update the prospective payment rates and determine the outlier threshold amount, as this data is generally considered to be the best overall predictor of experience in the upcoming fiscal year. Additionally, utilizing a 3-year rolling average approach would not be setting outlier payments at the 3 percent target and could potentially exceed or reduce the 3 percent outlier pool objective. We appreciate the commenters' suggestions and will take them into consideration as we continue to consider revisions to our outlier threshold methodology in future rulemaking.
As most recently discussed in the FY 2023 IRF PPS final rule ( 87 FR 47038 ), our outlier policy is intended to reimburse IRFs for treating extraordinarily costly cases. Any future consideration given to adjusting the outlier threshold to account for historical outlier reconciliation dollars or imposing a limit on outlier payments would need to be carefully assessed and take into consideration the effect on access to IRF care for certain high-cost populations. We continue to believe that maintaining the outlier pool at 3 percent of aggregate IRF payments optimizes the extent to which we can reduce financial risk to IRFs of caring for highest-cost patients, while still providing for adequate payments for all other non-outlier cases.
Additionally, we do not believe it would be appropriate to limit changes in the outlier threshold to changes in the market basket percentage as constraining adjustments to the outlier threshold may result in a threshold that generates outlier payments above or below the 3 percent target.
We appreciate the commenters' suggestions for refinements to the outlier methodology as well as the suggested areas of analysis and will take them into consideration as we continue to assess our outlier threshold methodology. We will continue to monitor our outlier policy to ensure it continues to compensate IRFs appropriately.
After consideration of the comments received and considering the most recent available data, we are finalizing the outlier threshold amount of $12,043 to maintain estimated outlier payments at approximately 3 percent of total estimated aggregate IRF payments for FY 2025.
CCRs are used to adjust charges from Medicare claims to costs and are computed annually from facility-specific data obtained from MCRs. IRF-specific CCRs are used in the development of the CMG relative weights and the calculation of outlier payments under the IRF PPS. In accordance with the methodology stated in the FY 2004 IRF PPS final rule ( 68 FR45692 through 45694 ), we proposed to apply a ceiling to IRFs' CCRs. Using the methodology described in that final rule, we proposed to update the national urban and rural CCRs for IRFs, as well as the national CCR ceiling for FY 2025, based on analysis of the most recent data available. We apply the national urban and rural CCRs to:
- New IRFs that have not yet submitted their first MCR.
- IRFs with an overall CCR that exceeds the national CCR ceiling for FY 2025, as discussed below in this section.
- Other IRFs for which accurate data to calculate an overall CCR are not available.
Specifically, for FY 2025, we proposed to estimate a national average CCR of 0.492 for rural IRFs, which we calculated by taking an average of the CCRs for all rural IRFs using their most recently submitted cost report data. Similarly, we proposed to estimate a national average CCR of 0.406 for urban IRFs, which we calculated by taking an average of the CCRs for all urban IRFs using their most recently submitted cost report data. We apply weights to both of these averages using the IRFs' estimated costs, meaning that the CCRs of IRFs with higher total costs factor more heavily into the averages than the CCRs of IRFs with lower total costs. For this final rule, we have used the most recent available cost report data (FY 2022). This includes all IRFs whose cost reporting periods begin on or after October 1, 2021, and before October 1, 2022. If, for any IRF, the FY 2022 cost report was missing or had an “as submitted” status, we used data from a previous FY's (that is, FY 2004 through FY 2021) settled cost report for that IRF. We do not use cost report data from before FY 2004 for any IRF because changes in IRF utilization since FY 2004 resulting from the 60 percent rule and IRF medical review activities suggest that these older data do not adequately reflect the current cost of care. Using updated FY 2022 cost report data for this final rule, we estimate a national average CCR of 0.485 for rural IRFs, and a national average CCR of 0.405 for urban IRFs.
In accordance with past practice, we proposed to set the national CCR ceiling at 3 standard deviations above the mean CCR. Using this method, we proposed a national CCR ceiling of 1.52 for FY 2025. This means that, if an individual IRF's CCR were to exceed this ceiling of 1.52 for FY 2025, we will replace the IRF's CCR with the appropriate national average CCR (either rural or urban, depending on the geographic location of the IRF). We calculated the national CCR ceiling by:
Step 1. Taking the national average CCR (weighted by each IRF's total costs, as previously discussed) of all IRFs for which we have sufficient cost report data (both rural and urban IRFs combined).
Step 2. Estimating the standard deviation of the national average CCR computed in Step 1.
Step 3. Multiplying the standard deviation of the national average CCR computed in Step 2 by a factor of 3 to compute a statistically significant reliable ceiling.
Step 4. Adding the result from Step 3 to the national average CCR of all IRFs for which we have sufficient cost report data, from Step 1.
We also proposed that if more recent data become available after the publication of the proposed rule and before the publication of this final rule, we would use such data to determine the FY 2025 national average rural and urban CCRs and the national CCR ceiling in the final rule. Using the FY 2022 cost report data for this final rule, we estimate a national average CCR ceiling of 1.50, using the same methodology.
We invited public comment on the proposed update to the IRF CCR ceiling and the urban/rural averages for FY 2025.
We did not receive any comments on the proposed update to the IRF CCR ceiling and the urban/rural averages for FY 2025. Consistent with the methodology outlined in the proposed rule, and using the most recent cost report data, we are finalizing a national average urban CCR at 0.405, the national average rural CCR at 0.485, and the national average CCR ceiling at 1.50 for FY 2025.
The Inpatient Rehabilitation Facility Quality Reporting Program (IRF QRP) is authorized by section 1886(j)(7) of the Act, and it applies to freestanding IRFs, as well as inpatient rehabilitation units of hospitals or Critical Access Hospitals (CAHs) paid by Medicare under the IRF PPS. Section 1886(j)(7)(A)(i) of the Act requires the Secretary to reduce by 2 percentage points the annual increase factor for discharges occurring during a FY for any IRF that does not submit data in accordance with the IRF QRP requirements set forth in subparagraphs (C) and (F) of section 1886(j)(7) of the Act. We have codified our program requirements in our regulations at § 412.634.
We proposed to require IRFs to report four new items to the IRF-Patient Assessment Instrument (PAI) and modify one item on the IRF-PAI as described in section VII.C. of the proposed rule. We also proposed to remove an item from the IRF-PAI as described in section VII.F.3 of the proposed rule. Finally, we also sought information on future measure concepts for the IRF QRP and on an IRF star rating system in sections VII.D. and VII.E. of the proposed rule, respectively.
For a detailed discussion of the considerations we use for the selection of IRF QRP quality, resource use, or other measures, we refer readers to the FY 2016 IRF PPS final rule ( 80 FR 47083 and 47084 ).
The IRF QRP currently has 18 adopted measures, which are listed in Table 13. For a discussion of the factors used to evaluate whether a measure should be removed from the IRF QRP, we refer readers to § 412.634(b)(2).
Table 13—Quality Measures Currently Adopted for the IRF QRP
We did not propose to adopt any new measures for the IRF QRP.
In the proposed rule, we proposed to require IRFs to report the following four new items [ 7 ] as standardized patient assessment data elements under the social determinants of health (SDOH) category: one item for Living Situation; two items for Food; and one item for Utilities. We also proposed to modify one of the current items collected as standardized patient assessment data under the SDOH category (the Transportation item), as described in section VII.C.5. of the proposed rule. [ 8 ]
Section 1886(j)(7)(F)(ii) of the Act requires IRFs to submit standardized patient assessment data required under section 1899B(b)(1) of the Act. Section 1899B(b)(1)(A) of the Act requires post-acute care (PAC) providers to submit standardized patient assessment data under applicable reporting provisions (which, for IRFs, is the IRF QRP) with respect to the admission and discharge of an individual (and more frequently as the Secretary deems appropriate) using a standardized patient assessment instrument. Section 1899B(a)(1)(C) of the Act requires, in part, the Secretary to modify the PAC assessment instruments in order for PAC providers, including IRFs, to submit standardized patient assessment data under the Medicare program. IRFs are currently required to report standardized patient assessment data through the patient assessment instrument, referred to as the Inpatient Rehabilitation Facility-Patient Assessment Instrument (IRF-PAI). Section 1899B(b)(1)(B) of the Act describes standardized patient assessment data as data required for at least the quality measures described in section 1899B(c)(1) of the Act and that is with respect to the following categories: (1) functional status, such as mobility and self-care at admission to a PAC provider and before discharge from a PAC provider; (2) cognitive function, such as ability to express ideas and to understand, and mental status, such as depression and dementia; (3) special services, treatments, and interventions, such as need for ventilator use, dialysis, chemotherapy, central line placement, and total parenteral nutrition; (4) medical conditions and comorbidities, such as diabetes, congestive heart failure, and pressure ulcers; (5) impairments, such as incontinence and an impaired ability to hear, see, or swallow; and (6) other categories deemed necessary and appropriate by the Secretary.
Section 1899B(b)(1)(B)(vi) of the Act authorizes the Secretary to collect standardized patient assessment data elements with respect to other categories deemed necessary and appropriate. Accordingly, we finalized the creation of the SDOH category of standardized patient assessment data elements in the FY 2020 IRF PPS final rule ( 84 FR 39149 through 39161 ), and defined SDOH as the socioeconomic, cultural, and environmental circumstances in which individuals live that impact their health. [ 9 ] According to the World Health Organization, research shows that the SDOH can be more important than health care or lifestyle choices in influencing health, accounting for between 30-55% of health outcomes. [ 10 ] This is a part of a growing body of research that highlights the importance of SDOH on health outcomes. Subsequent to the FY 2020 IRF PPS final rule, we expanded our definition of SDOH: SDOH are the conditions in the environments where people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks. [ 11 12 13 ] This update will align our definition of SDOH with the definition used by HHS agencies, including OASH, the Centers for Disease Control and Prevention (CDC), and the White House Office of Science and Technology Policy. [ 14 15 ] We currently collect seven items in this SDOH category of standardized patient assessment data elements: ethnicity, race, preferred language, interpreter services, health literacy, transportation, and social isolation ( 84 FR 39149 through 39161 ). [ 16 ]
In accordance with our authority under section 1899B(b)(1)(B)(vi) of the Act, we similarly finalized the creation of the SDOH category of standardized patient assessment data elements for Skilled Nursing Facilities (SNFs) in the FY 2020 SNF PPS final rule ( 84 FR 38805 through 38817 ), for Long-Term Care Hospitals (LTCHs) in the FY 2020 Inpatient Prospective Payment System (IPPS)/LTCH PPS final rule ( 84 FR 42577 through 42588 ), and for Home Health Agencies (HHAs) in the Calendar Year (CY) 2020 HH PPS final rule ( 84 FR 60597 through 60608 ). We also collect the same seven SDOH items in these PAC providers' respective patient/resident assessment instruments ( 84 FR 38817 , 84 FR 42590 , and 84 FR 60610 , respectively).
Access to standardized data relating to SDOH on a national level permits us to conduct periodic analyses, and to assess their appropriateness as risk adjustors or in future quality measures. Our ability to perform these analyses and to make adjustments relies on existing data collection of SDOH items from PAC settings. We adopted these SDOH items using common standards and definitions across the four PAC providers to promote interoperable exchange of longitudinal information among these PAC providers, including IRFs, and other providers. We believe this information may facilitate coordinated care, continuity in care planning, and the discharge planning process from PAC settings.
We noted in the FY 2020 IRF PPS final rule that each of the items was identified in the 2016 National Academies of Sciences, Engineering, and Medicine (NASEM) report as impacting care use, cost, and outcomes for Medicare beneficiaries ( 84 FR 39150 through 39151 ). At that time, we acknowledged that other items may also be useful to understand. The SDOH items we proposed to adopt as standardized patient assessment data elements under the SDOH category in this proposed rule were also identified in the 2016 NASEM report [ 17 ] or the 2020 NASEM report [ 18 ] as impacting care use, cost, and outcomes for Medicare beneficiaries. The items have the capacity to take into account treatment preferences and care goals of patients and their caregivers, to inform our understanding of patient complexity and SDOH that may affect care outcomes and ensure that IRFs are in a position to impact through the provision of services and supports, such as connecting patients and their caregivers with identified needs with social support programs.
Health-related social needs (HRSNs) are the resulting effects of SDOH, which are individual-level, adverse social conditions that negatively impact a person's health or health care. [ 19 ] Examples of HRSNs include lack of access to food, housing, or transportation, and have been associated with poorer health outcomes, greater use of emergency departments and hospitals, and higher health care costs. [ 20 ] Certain HRSNs can lead to unmet social needs that directly influence an individual's physical, psychosocial, and functional status. This is particularly true for food security, housing stability, utilities security, and access to transportation. [ 21 ]
We proposed to require IRFs to collect and submit four new items in the IRF-PAI as standardized patient assessment data elements under the SDOH category because these items would collect information not already captured by the current SDOH items. Specifically, we believe the ongoing identification of SDOH would have three significant benefits. First, promoting screening for SDOH could serve as evidence-based building blocks for supporting healthcare providers in actualizing their commitment to address disparities that disproportionately impact underserved communities. Second, screening for SDOH improves health equity through identifying potential social needs so the IRF may address those with the patient, their caregivers, and community partners during the discharge planning process, if indicated. [ 22 ] Third, these SDOH items could support our ongoing IRF QRP initiatives by providing data with which to stratify IRFs' performance on measures and in future quality measures.
Collection of additional SDOH items would permit us to continue developing the statistical tools necessary to maximize the value of Medicare data and improve the quality of care for all beneficiaries. For example, we recently developed and released the Health Equity Confidential Feedback Reports, which provided data to IRFs on whether differences in quality measure outcomes are present for their patients by dual-enrollment status and race and ethnicity. [ 23 ] We note that advancing health equity by addressing the health disparities that underlie the country's health system is one of our strategic pillars [ 24 ] and a Biden-Harris Administration priority. [ 25 ]
We proposed to require IRFs to collect and submit four new items as standardized patient assessment data elements under the SDOH category using the IRF-PAI: one item for Living Situation, as described in section VIII.3.(a) of this final rule; two items for Food, as described in section VIII.3.(b) of this final rule; and one item for Utilities, as described in VIII.3.(c) of this final rule.
We selected the SDOH items from the Accountable Health Communities (AHC) Health-Related Social Needs (HRSN) Screening Tool developed for the AHC Model. [ 26 ] The AHC HRSN Screening Tool is a universal, comprehensive screening for HRSNs that addresses five core domains as follows: (1) housing instability (for example, homelessness, poor housing quality), (2) food insecurity, (3) transportation difficulties, (4) utility assistance needs, and (5) interpersonal safety concerns (for example, intimate-partner violence, elder abuse, child maltreatment). [ 27 ]
We believe that requiring IRFs to report new items that are included in the AHC HRSN Screening Tool will further standardize the screening of SDOH across quality programs. For example, as outlined in the proposed rule, our proposal will align, in part, with the requirements of the Hospital Inpatient Quality Reporting (IQR) Program and the Inpatient Psychiatric Facility Quality Reporting (IPFQR) Program. As of January 2024, hospitals are required to report whether they have screened patients for the standardized SDOH categories of housing instability, food insecurity, utility difficulties, transportation needs, and interpersonal safety to meet the Hospital IQR Program requirements. [ 28 ] Additionally, beginning January 2025, IPFs will also be required to report whether they have screened patients for the same set of SDOH categories. [ 29 ] As we continue to standardize data collection across settings, we believe using common standards and definitions for new items is important to promote interoperable exchange of longitudinal information between IRFs and other providers to facilitate coordinated care, continuity in care planning, and the discharge planning process.
Below we describe each of the four proposed items in more detail.
Healthy People 2030 prioritizes economic stability as a key SDOH, of which housing stability is a component. [ 30 31 ] Lack of housing stability encompasses several challenges, such as having trouble paying rent, overcrowding, moving frequently, or spending the bulk of household income on housing. [ 32 ] These experiences may negatively affect one's physical health and access to health care. Housing instability can also lead to homelessness, which is housing deprivation in its most severe form. [ 33 ] On a single night in 2023, roughly 653,100 people, or 20 out of every 10,000 people in the United States, were experiencing homelessness. [ 34 ] Studies also found that people who are homeless have an increased risk of premature death and experience chronic disease more often than among the general population. [ 35 ]
We believe that IRFs can use information obtained from the Living Situation item during a patient's discharge planning. For example, IRFs could work in partnership with community care hubs and community-based organizations to establish new care transition workflows, including referral pathways, contracting mechanisms, data sharing strategies, and implementation training that can track HRSNs to ensure unmet needs, such as housing, are successfully addressed through closed loop referrals and follow-up. [ 36 ] IRFs could also take action to help alleviate a patient's other related costs of living, like food, by referring the patient to community-based organizations that would allow the patient's additional resources to be allocated towards housing without sacrificing other needs. [ 37 ] Finally, IRFs could use the information obtained from the Living Situation item to better coordinate with other healthcare providers, facilities, and agencies during transitions of care, so that referrals to address a patient's housing stability are not lost during vulnerable transition periods.
Due to the potential negative impacts housing instability can have on a patient's health, we proposed to adopt the Living Situation item as a new standardized patient assessment data element under the SDOH category. This proposed Living Situation item is based on the Living Situation item collected in the AHC HRSN Screening Tool, [ 38 39 ] and was adapted from the Protocol for Responding to and Assessing Patients' Assets, Risks, and Experiences (PRAPARE) tool. [ 40 ] The proposed Living Situation item asks, “What is your living situation today?” The proposed response options are: (1) I have a steady place to live; (2) I have a place to live today, but I am worried about losing it in the future; (3) I do not have a steady place to live; (7) Patient declines to respond; and (8) Patient unable to respond. A draft of the Living Situation item proposed to be adopted as a standardized patient assessment data element under the SDOH category can be found in the Downloads section of the IRF-PAI and IRF-PAI Manual web page at https://www.cms.gov/medicare/quality/inpatient-rehabilitation-facility/irf-pai-and-irf-qrp-manual .
The U.S. Department of Agriculture, Economic Research Service defines a lack of food security as a household-level economic and social condition of limited or uncertain access to adequate food. [ 41 ] Adults who are food insecure may be at an increased risk for a variety of negative health outcomes and health disparities. For example, a study found that food-insecure adults may be at an increased risk for obesity. [ 42 ] Another study found that food-insecure adults have a significantly higher probability of death from any cause or cardiovascular disease in long-term follow-up care, in comparison to adults that are food secure. [ 43 ]
While having enough food is one of many predictors for health outcomes, a diet low in nutritious foods is also a factor. [ 44 ] The United States Department of Agriculture (USDA) defines nutrition security as “consistent and equitable access to healthy, safe, affordable foods essential to optimal health and well-being.” [ 45 ] Nutrition security builds on and complements long standing efforts to advance food security. Studies have shown that older adults struggling with food insecurity consume fewer calories and nutrients and have lower overall dietary quality than those who are food secure, which can put them at nutritional risk. [ 46 ] Older adults are also at a higher risk of developing malnutrition, which is considered a state of deficit, excess, or imbalance in protein, energy, or other nutrients that adversely impacts an individual's own body form, function, and clinical outcomes. [ 47 ] Up to 50 percent of older adults are affected by or at risk for malnutrition, which is further aggravated by a lack of food security and poverty. [ 48 ] These facts highlight why the Biden-Harris Administration launched the White House Challenge to End Hunger and Build Healthy Communities. [ 49 ]
We believe that adopting items to collect and analyze information about a patient's food security at home could provide additional insight to their health complexity and help facilitate coordination with other healthcare providers, facilities, and agencies during transitions of care, so that referrals to address a patient's food security are not lost during vulnerable transition periods. For example, an IRF's dietitian or other clinically qualified nutrition professional could work with the patient and their caregiver to plan healthy, affordable food choices prior to discharge. [ 50 ] IRFs could also refer a patient that indicates lack of food security to government initiatives such as the Supplemental Nutrition Assistance Program (SNAP) and food pharmacies (programs to increase access to healthful foods by making them affordable), two initiatives that have been associated with lower health care costs and reduced hospitalization and emergency department visits. [ 51 ]
We proposed to adopt two Food items as new standardized patient assessment data elements under the SDOH Category. These proposed items are based on the Food items collected in the AHC HRSN Screening Tool and were adapted from the USDA 18-item Household Food Security Survey (HFSS). [ 52 ] The first proposed Food item states, “Within the past 12 months, you worried that your food would run out before you got money to buy more.” The second proposed Food item states, “Within the past 12 months, the food you bought just didn't last and you didn't have money to get more.” We proposed the same response options for both items: (1) Often true; (2) Sometimes true; (3) Never True; (7) Patient declines to respond; and (8) Patient unable to respond. A draft of the proposed Food items proposed to be adopted as standardized patient assessment data elements under the SDOH category can be found in the Downloads section of the IRF-PAI and IRF-PAI Manual web page at https://www.cms.gov/medicare/quality/inpatient-rehabilitation-facility/irf-pai-and-irf-qrp-manual .
A lack of energy (utility) security can be defined as an inability to adequately meet basic household energy needs. [ 53 ] According to the United States Department of Energy, one in three households in the U.S. are unable to adequately meet basic household energy needs. [ 54 ] The consequences associated with a lack of utility security are represented by three primary dimensions: economic, physical, and behavioral. Patients with low incomes are disproportionately affected by high energy costs, and they may be forced to prioritize paying for housing and food over utilities. [ 55 ] Some patients may face limited housing options and therefore are at increased risk of living in lower-quality physical conditions with malfunctioning heating and cooling systems, poor lighting, and outdated plumbing and electrical systems. [ 56 ] Patients with a lack of utility security may use negative behavioral approaches to cope, such as using stoves and space heaters for heat. [ 57 ] In addition, data from the Department of Energy's U.S. Energy Information Administration confirm that a lack of energy security disproportionately affects certain populations, such as low-income and African American households. [ 58 ] The effects of a lack of utility security include vulnerability to environmental exposures such as dampness, mold, and thermal discomfort in the home, which have a direct impact on a person's health. [ 59 ] For example, research has shown associations between a lack of energy security and respiratory conditions as well as mental health-related disparities and poor sleep quality in vulnerable populations such as the elderly, children, the socioeconomically disadvantaged, and the medically vulnerable. [ 60 ]
We believe adopting an item to collect information upon a patient's admission to an IRF about their utility security would facilitate the identification of patients who may not have utility security and who may benefit from engagement efforts. For example, IRFs may be able to use the information on utility security to help connect some patients in need to programs that can help older adults pay for their home energy (heating/cooling) costs, like the Low-Income Home Energy Assistance Program (LIHEAP). [ 61 ] IRFs may also be able to partner with community care hubs and community-based organizations to assist the patient in applying for these and other local utility assistance programs, as well as helping them navigate the enrollment process. [ 62 ]
We proposed to adopt a new item, Utilities, as a new standardized patient assessment data element under the SDOH category. This proposed item is based on the Utilities item collected in the AHC HRSN Screening Tool and was adapted from the Children's Sentinel Nutrition Assessment Program (C-SNAP) survey. [ 63 ] The proposed Utilities item asks, “In the past 12 months, has the electric, gas, oil, or water company threatened to shut off services in your home?” The proposed response options are: (1) Yes; (2) No; (3) Already shut off; (7) Patient declines to respond; and (8) Patient unable to respond. A draft of the proposed Utilities item to be adopted as a standardized patient assessment data element under the SDOH category can be found in the Downloads section of the IRF-PAI and IRF-PAI Manual web page at https://www.cms.gov/medicare/quality/inpatient-rehabilitation-facility/irf-pai-and-irf-qrp-manual .
We developed our updates to add these items after considering feedback we received in response to our Health Equity Update in the FY 2024 IRF PPS final rule. While there were commenters who urged CMS to balance reporting requirements so as not to create undue administrative burden and avoid making generalizations about differences in health and health care on certain data elements, it was also suggested CMS incentivize collection of data on SDOH such as housing stability and food security. Two commenters emphasized that any additional stratification of quality measures, including social risk factors and SDOH, would be of value to PAC providers, including IRFs. The FY 2024 IRF PPS final rule ( 88 FR 51037 through 51039 ) includes a summary of the public comments that we received in response to the Health Equity Update and our responses to those comments.
Additionally, we considered feedback we received when we proposed the creation of the SDOH category of standardized patient assessment data elements in the FY 2020 IRF PPS proposed rule ( 84 FR 17319 through 17326 ). Commenters were generally in favor of the concept of collecting SDOH items and stated that if implemented appropriately the data could be useful in identifying and addressing health care disparities, as well as refining the risk adjustment of outcome measures. One commenter specifically recommended CMS consider including data collection of housing status, since unmet housing needs can put patients at higher risk for readmission. The FY 2020 IRF PPS final rule ( 84 FR 39149 through 39161 ) includes a summary of the public comments that we received and our responses to those comments. We incorporated this input into the development of this proposal.
We solicited comment on the proposal to adopt four new items as standardized patient assessment data elements in the IRF-PAI under the SDOH category beginning with the FY 2028 IRF QRP: one Living Situation item; two Food items; and one Utilities item ( 89 FR 22279 ).
The following is a summary of the public comments received on the proposal and our responses:
Comment: Many commenters expressed support for the proposed new SDOH assessment items, viewing this as an important step towards identifying health disparities, improving health outcomes, understanding diverse patient needs, improving discharge planning and care coordination, and fostering continuous quality improvement. One of these commenters also emphasized the importance of collecting SDOH data in helping recognize areas of need and enhancing efforts to improve patient outcomes across healthcare settings, and another commenter emphasized the importance of identifying, documenting, and addressing SDOH in order to provide equitable, high-quality, holistic, patient-centered care.
Several commenters noted the importance of the proposed new SDOH assessment items in facilitating discharge planning strategies that can account for a person's housing, food, utilities, and transportation needs. Three of these commenters noted that the information obtained from these proposed new SDOH assessment items will provide data that can be used to better address identified needs with the patient, their caregivers, and community partners during the discharge planning process. These commenters also mentioned that addressing non-medical factors during patient visits can help connect patients to the resources they need and lead to successful discharges to the community or improved health outcomes. Another one of these commenters noted that the direct value to providers in the inpatient rehabilitation space is the insight into the home life and resources available to the patient once discharged. Finally, one of these commenters noted that these proposed SDOH assessment items support a culture of engaging with and advancing equity in IRFs by reflecting a proactive approach towards addressing the multifaceted determinants of health.
Response: We appreciate the support. We agree that the collection of the proposed SDOH assessment items will support IRFs that wish to understand the health disparities that affect their populations, facilitate coordinated care, foster continuity in care planning, and assist with the discharge planning process from the IRF setting.
Comment: Several commenters appreciated CMS' efforts at standardizing collection of patient assessment data elements related to SDOH by proposing to adopt the four new assessment items, Living Situation, Food, and Utilities, in the IRF-PAI. One of these commenters supported CMS' decision to align and standardize new SDOH data collection in the IRF QRP with data already being collected in other settings, such as the Hospital Inpatient Quality Reporting (IQR) Program and the Inpatient Psychiatric Facility Quality Reporting (IPFQR) Program. Another one of these commenters noted that the utilization of the AHC HRSN Screening Tool will help fill the existing gap of standardized SDOH data collection for CMS programs, which will reduce the administrative burden with collecting SDOH data. In addition, three commenters noted their support of the proposed new SDOH assessment items because they are similar to questions many IRFs already ask for discharge planning purposes, minimizing additional burden.
Response: We thank the commenter for recognizing that our proposal aligns, in part, with the requirements of the Hospital IQR Program and the IPFQR Program. As we continue to standardize data collection across settings, we believe using common standards and definitions for new assessment items is important to promote interoperable exchange of longitudinal information between IRFs and other providers. We heard from many IRFs that they are already collecting similar information and integrating it into their admission and discharge processes in order to facilitate coordinated care and continuity in care planning. We believe collecting this information in all IRFs may facilitate coordinated care, continuity in care planning, and IRFs' discharge planning process in accordance with our regulation at § 482.43(a).
Comment: Several commenters agreed with the importance of collecting SDOH assessment items through the IRF-PAI but also expressed concerns about the additional administrative burden associated with collecting the new SDOH data. Several of these commenters noted that data collection is overburdening the workforce, and one noted that it will take away resources from patient care while another commenter urged CMS to ensure the additional burden on providers provides meaningful benefit to rehab patients. One of these commenters requested additional funding for the increased costs associated with what they believe are tasks outside the normal day-to-day operations of the facilities.
Response: Although the addition of four new SDOH assessment items to the IRF-PAI will increase the burden associated with completing the IRF-PAI, we carefully considered this increased burden of collecting new assessment items against the benefits of adopting those assessment items for the IRF-PAI. Collection of additional SDOH assessment items will permit us to continue developing the statistical tools necessary to maximize the value of Medicare data and improve the quality of care for all beneficiaries. As noted in section VII.C.2 of the proposed rule ( 89 FR 22276 ) and section VIII.C.2. of this final rule, we recently developed and released the Health Equity Confidential Feedback Reports, which provided data to IRFs on whether differences in quality measure outcomes are present for their patients by dual-enrollment status and race and ethnicity. [ 64 ] In balancing the reporting burden for IRFs, we prioritized our policy objective to collect additional SDOH standardized patient assessment data elements that will inform care planning and coordination and quality improvement across care settings.
In response to the commenters who believe this policy, if finalized, would take time away from patient care, we believe the proposed assessment items (Living Situation, Food, and Utilities) are all important pieces of information to developing and administering a comprehensive plan of care in accordance with our regulation at § 412.606. A comprehensive plan of care includes the initiation of a discharge plan. Given the relatively short length of stay in IRFs, discharge planning generally begins at the time of admission and this information would inform the comprehensive plan of care. Using this information, IRFs have an opportunity to implement interventions to address these SDOH, if appropriate. For example, IRFs may determine that educating patients about transportation resources, teaching them how to use adaptive transportation if their condition now requires it, educating patients about safe choices for utilities, or begin the process of finding resources for patients is appropriate for the patient's comprehensive plan of care. Rather than taking time away from patient care, providers will be documenting information they are likely already collecting through the course of providing care to the patients.
Regarding the comment requesting additional funding for the increased costs associated with collecting data on these new assessment items, we find the comment unclear. We interpret the commenter to mean that they do not believe that current IRF PPS payments are sufficient to cover the increased burden (specifically, costs) associated with collection of this additional data for the proposed new SDOH assessment items. As discussed previously, we carefully considered the increased burden associated with collection of these four new SDOH assessment items against the benefits of adopting these items for the IRF-PAI. We believe the collection of these items is within the normal day-to-day operations of the facilities. For instance, IRFs are required by regulation at § 482.43(a) to identify, at an early stage of hospitalization, those patients who are likely to suffer adverse health consequences upon discharge in the absence of adequate discharge planning and must provide a discharge planning evaluation for those patients. The proposed new SDOH assessment items were identified in either the 2016 NASEM report [ 65 ] or the 2020 NASEM report [ 66 ] as impacting care use, cost, and outcomes for Medicare beneficiaries. We believe the proposed new SDOH assessment items have the potential to generate actionable data IRFs can use to implement effective discharge planning processes that can reduce the risk for negative outcomes such as hospital readmissions and admission to a nursing facility for long-term care. Given that IRFs must develop and implement an effective discharge planning process that ensures the discharge needs of each patient are identified, we believe IRFs are likely collecting some of this data already. Collection of these new SDOH items will provide key information to IRFs to support effective discharge planning.
Finally, we also plan to provide training resources in advance of the initial collection of the new SDOH assessment items to ensure that IRFs have the tools necessary to administer these new items and reduce the burden to IRFs having to create their own training resources. These training resources may include online learning modules, tip sheets, questions and answers documents, and recorded webinars and videos. We anticipate that we will make these materials available to IRFs in mid-2025, which will give IRFs several months prior to required collection and reporting to take advantage of the learning opportunities.
Comment: One commenter who supported the proposal to collect the new and modified SDOH assessment items also encouraged CMS to ensure the new assessment items are valid and reliable. Several commenters who did not support the proposal noted concerns with the validity and reliability of the proposed new and modified SDOH assessment items, and several of these commenters recommended further testing of these assessment items for the IRF population. In addition, one commenter noted that most hospitals in their network reported they do not use the AHC tool for screening for social services as they find the tool suboptimal for its ability to gather accurate information and get patients the services they need.
Response: We disagree that the proposed new and modified SDOH assessment items require further testing prior to collecting them on the IRF-PAI for the IRF QRP. The AHC HRSN Screening Tool is evidence-based and informed by practical experience. With input from a panel of national experts convened by our contractor, we developed the tool under the Center for Medicare and Medicaid Innovation (CMMI) by conducting a review of existing screening tools and questions focused on core and supplemental HRSN domains, including housing instability, food insecurity, transportation difficulties, utility assistance needs, and interpersonal safety concerns. [ 67 ] These domains were chosen based upon literature review and expert consensus utilizing the following criteria: (1) availability of high-quality scientific evidence linking a given HRSN to adverse health outcomes and increased healthcare utilization, including hospitalizations and associated costs; (2) ability for a given HRSN to be screened and identified in the inpatient setting prior to discharge, addressed by community-based services, and potentially improve healthcare outcomes, including reduced readmissions; and (3) evidence that a given HRSN is not systematically addressed by healthcare providers. [ 68 ] In addition to established evidence of their association with health status, risk, and outcomes, these domains were selected because they can be assessed across the broadest spectrum of individuals in a variety of settings. [ 69 70 ]
Through this process, over 50 screening tools totaling more than 200 questions were compiled. In order to refine this list, CMS' contractor consulted a technical expert panel (TEP) consisting of a diverse group of tool developers, public health and clinical researchers, clinicians, population health and health systems executives, community-based organization leaders, and Federal partners. Over the course of several meetings, this TEP met to discuss opportunities and challenges involved in screening for HRSNs; consider and pare down CMS' list of evidence-based screening questions; and recommend a short list of questions for inclusion in the final tool. The AHC HRSN Screening Tool was tested across many care delivery sites in diverse geographic locations across the United States. More than one million Medicare and Medicaid beneficiaries have been screened using the AHC HRSN Screening Tool, which was evaluated psychometrically and demonstrated evidence of both reliability and validity, including inter-rater reliability and concurrent and predictive validity. Moreover, the AHC HRSN Screening Tool can be implemented in a variety of places where individuals seek healthcare, including IRFs.
We selected these proposed assessment items for the IRF QRP from the AHC HRSN Screening Tool because we believe that collecting information on living situation, food, utilities, and transportation could have a direct and positive impact on patient care in IRFs. Specifically, collecting the information provides an opportunity for the IRF to identify patients' potential HRSNs, and if indicated, to those with the patient, their caregivers, and community partners during the discharge planning process, potentially resulting in improvements in patient outcomes.
Comment: Three of these commenters referenced CMS' second evaluation of the AHC model from 2018 through 2021. [ 71 ] These commenters interpret the Findings at a Glance to conclude that the AHC HRSN Screening Tool “did not appear to increase beneficiaries' connection to community services or HRSN resolution.”
Response: This two-page summary of the AHC Model 2018-2021 [ 72 ] describes the results of testing whether systematically identifying and connecting beneficiaries to community resources for their HRSNs improved health care utilization outcomes and reduced costs. To ensure consistency in the screening offered to beneficiaries across both an individual community's clinical delivery sites and across all the communities in the model, CMS developed a standardized HRSN screening tool. This AHC HRSN Screening Tool was used to screen Medicare and Medicaid beneficiaries for core HRSNs to determine their eligibility for inclusion in the AHC Model. If a Medicare or Medicaid beneficiary was eligible for the AHC Model, they were randomly assigned to one of two tracks: (1) Assistance; or (2) Alignment. The Assistance Track tested whether navigation assistance that connects navigation-eligible beneficiaries with community services results in increased HRSN resolution, reduced health care expenditures, and unnecessary utilization. The Alignment Track tested whether navigation assistance, combined with engaging key stakeholders in continuous quality improvement (CQI) to align community service capacity with beneficiaries' HRSNs, results in greater increases in HRSN resolution and greater reductions in health expenditures and utilization than navigation assistance alone. Regardless of assigned track, all beneficiaries received HRSN screening, community referrals, and navigation to community services. [ 73 ]
We believe the commenter inadvertently misinterpreted the findings, believing these findings were with respect to the effectiveness and scientific validity of the AHC HRSN Screening Tool itself. The findings section of this two-page summary described six key findings from the AHC Model, which examined whether the Assistance Track or the Alignment Track resulted in greater increases in HRSN resolution and greater reductions in health expenditures and utilization. Particularly, the AHC Model reduced emergency department visits among Medicaid and FFS Medicare beneficiaries in the Assistance Track, which was suggestive that navigation may help patients use the health care system more effectively. We acknowledge that navigation alone did not increase beneficiaries' connection to community services or HRSN resolution, and this was attributed to gaps between community resource availability and beneficiary needs. The AHC HRSN Screening Tool used in the AHC Model was limited to identifying Medicare and Medicaid beneficiaries with at least one core HRSN who could be eligible to participate in the AHC Model. Our review of the AHC Model did not identify any issues with the validity and scientific reliability of the AHC HRSN Screening Tool.
Finally, as part of our routine item and measure monitoring work, we continually assess the implementation of new assessment items, including the four new proposed SDOH assessment items.
Comment: Three commenters requested that CMS articulate the vision for how CMS plans to use the data collected from the proposed SDOH standardized patient assessment data elements in quality and payment programs. These commenters noted concern that CMS may use the SDOH assessment data to develop an IRF QRP measure that would hold IRFs solely accountable for social drivers of health that require resources and engagement across an entire community to address.
Response: We proposed the four new SDOH assessment items because collection of additional SDOH items would permit us to continue developing the statistical tools necessary to maximize the value of Medicare data and improve the quality of care for all beneficiaries. For example, we recently developed and released the Health Equity Confidential Feedback Reports, which provided data to IRFs on whether differences in quality measure outcomes are present for their patients by dual-enrollment status and race and ethnicity. [ 74 ] We note that advancing health equity by addressing the health disparities that underlie the country's health system is one of our strategic pillars [ 75 ] and a Biden-Harris Administration priority. [ 76 ] Furthermore, any updates to the IRF QRP measure set or payment system would be addressed through future notice-and-comment rulemaking, as necessary.
Comment: Several commenters did not agree with CMS that the proposed SDOH assessment items would produce interoperable data within the CMS quality programs because the proposed requirements for IRF are not standardized with the SDOH collection requirements in the Hospital IQR Program and IPFQR Programs. This commenter noted that the Screening for SDOH measures in the Hospital IQR and IPFQR Programs do not specify when a patient is screened (for example, at admission) and how the screening questions are asked (in other words, specific wording and responses). Instead, providers reporting these measures under the Hospital IQR and IPFQR Programs are only asked to document that a patient was screened for the following domains: housing instability, food insecurity, transportation difficulties, utility assistance needs, and interpersonal safety concerns.
Response: We disagree that the proposed collection of four new SDOH Assessment items and one modified SDOH assessment item for the IRF QRP and the requirements for the Hospital IQR and IPFQR Programs do not promote standardization and interoperability. Although hospitals and IPFs participating in these programs can use a self-selected SDOH screening tool, the Screening for SDOH and Screen Positive Rate for SDOH measures we have adopted for the Hospital IQR and IPFQR Programs address same SDOH domains that we have proposed to collect as standardized patient assessment data under the IRF QRP: housing instability, food insecurity, utility difficulties, transportation needs. We believe that this partial alignment will facilitate longitudinal data collection on the same topics across healthcare settings. As we continue to standardize data collection, we believe using common standards and definitions for new assessment items is important to promote interoperable exchange of longitudinal information between IRFs and other providers to facilitate coordinated care, continuity in care planning, and the discharge planning process. This is evidenced by our recent proposals to add these four SDOH assessment items and one modified SDOH assessment item in the SNF QRP ( 89 FR 23462 through 23468 ), LTCH QRP ( 89 FR 36345 through 36350 ), and Home Health QRP ( 89 FR 55383 through 55388 ).
Comment: One commenter recommended the inclusion of assessment items to improve the overall patient care among those with disabilities, such as: disability-status, caregiver availability, patients' independent living status, and ability to return to work.
Response: We appreciate the comments and suggestions provided by the commenters, and we agree that it is important to understand the needs of patients with disabilities. As we continue to evaluate SDOH standardized patient assessment data elements and future policy options, we will consider this feedback. We note that although we proposed to require the collection of the Living Situation, Food, and Utilities items for the IRF QRP, our proposals would not preclude IRFs from choosing to screen their patients for additional SDOH they believe are relevant to their patient population and the community they serve, including screening for disability-status, caregiver availability, patients' independent living status, and ability to return to work.
Comment: Several commenters supported the proposal to adopt the Living Situation assessment item as a standardized patient assessment data element in the IRF-PAI. One of these commenters noted that having information about a patient's living situation enables better care coordination, identifies support gaps, and allows IRFs to develop tailored care plans. Another one of these commenters noted that this information helps them to improve facility operations and develop internal quality improvement efforts and population health initiatives. Finally, another one of these commenters noted that understanding a person's living situation can ensure the appropriate provision of necessary adaptive equipment and engagement with community partners to address patients' needs.
Response: We thank the commenters for their support and agree that information on a person's living situation can be used to develop tailored care plans, assist with quality improvement efforts, and collaborate with partners such as community care hubs and community-based organizations during transitions of care.
Comment: Two commenters recommended that the Living Situation assessment item incorporate information on whether a patient's living situation is suitable for potentially new complex care needs. One of these commenters highlighted the changing nature of IRF patients' needs and noted that some patients may have been housing secure prior to their condition, but that prior living situation may no longer be suitable for their current needs. The other commenter noted that in some cases, a patient's prior living situation may no longer be appropriate for them following their injury or illness, due to requirements such as mobility equipment, ramps, and other accessible modifications.
Response: While we proposed to require the collection of the Living Situation item at admission only, the collection could potentially prompt the IRF to initiate additional conversations with their patients about their living situation needs throughout their stay. As the commenter pointed out, it is important to think about the patient's living situation in the context of their new care needs, and collecting the Living Situation assessment item at admission would be an important first step to that process. Additionally, IRFs may seek to collect any additional information that they believe may be relevant to their patient population in order to inform their care and discharge planning process.
Comment: Two commenters expressed concerns with the time frame of the response options for the proposed the Living Situation item. One of these commenters suggested that adding a look back period of one year or less to the response options would allow healthcare providers to promptly intervene and mitigate any eminent negative housing situations. This commenter was concerned that, if left open-ended, patients may respond yes, thinking about many possible scenarios that may occur in the distant future. The other commenter encouraged CMS to consider a shorter look back period for the Living Situation assessment item, as a 12-month look back could capture circumstances that are no longer accurate.
Response: We interpret the comments to be suggesting that a time frame be added to two of the Living Situation response options, specifically: (1) I have a place to live today, but I am worried about losing it in the future; and (2) I do not have a steady place to live. We want to clarify that the proposed Living Situation item frames the question as, “What is your living situation today?” The question establishes the look back period (the present) the patient should consider in responding to the item.
Comment: Three commenters expressed concerns with utilizing the proposed Living Situation assessment item as currently worded. Specifically, commenters believe that asking about patients' living situation “today” may be difficult for IRF patients who are receiving treatment for a traumatic injury or serious medical event to answer accurately.
Response: We acknowledge the complex medical conditions of most IRF patients. However, there are other patient interview assessment items that IRFs currently collect that address this concern, and we believe IRFs have experience in managing these complex scenarios successfully in order to obtain the information required. We would also like to remind the commenter that we proposed response options for patients that are unable to respond or decline to respond.
We also plan to provide training resources in advance of the initial collection of the assessment items to ensure that IRFs have the tools necessary to administer the new SDOH assessment items and reduce the burden to IRFs in creating their own training resources. These training resources may include online learning modules, tip sheets, questions and answers documents, and recorded webinars and videos, and would be available to providers as soon as technically feasible.
Comment: One commenter recommended that CMS simplify the responses for the Living Situation assessment item because they are likely to lead to confusion. This commenter suggested CMS align the responses for the Living Situation assessment item with the proposed Food assessment item that has an “Often true,” “Sometimes true,” and “Never true” response option or with the modified Transportation assessment item that has a “Yes” or “No” response. They believe this would be simpler for patients to answer and be easier on the IRF staff to collect the information.
Response: We agree that standardized patient assessment data elements should be easy to understand and have clear response options. However, we believe that including the specific distinction in the Living Situation response options is needed. Specifically, we believe that additional response options to indicate whether a patient is worried about their living situation in the future helps reduce ambiguity for patients who may only have temporary housing. For example, having a “Yes” and “No” response and eliminating an option for “I have a place to live today, but I am worried about losing it in the future” would not capture those patients that may be at risk of losing their place to live due to lost income resulting from the traumatic injury or event precipitating their admission to the IRF. Identifying these patients who are worried about losing their housing in the future may help IRFs facilitate discharge planning and make appropriate community referrals.
Comment: One commenter stated they did not support the proposal to add the proposed new Living Situation assessment item to the IRF-PAI because a patient's ability to be discharged to home is a variable IRFs use when considering whether admission to IRF is appropriate. This commenter noted that patients who do not have a location they can be discharged to are not good candidates for IRFs, and as a result, the addition of the proposed Living Situation assessment item will increase burden without providing data to drive outcomes. Two commenters also noted that CMS could collect a patient's living status through assessment items already collected in the IRF-PAI, such as Discharge Living Setting and Discharge Living With.
Response: We disagree with the commenter's suggestions that the collection of the proposed Living Situation assessment item will increase burden without providing data to drive outcomes or that patients who do not have a location they can be discharged to are not good candidates for IRFs. A comprehensive preadmission screening includes anticipated discharge destination, since this information would be important to developing the interdisciplinary plan of care. However, the decision whether a patient is or is not appropriate for IRF admission is generally based on whether the patient requires the interdisciplinary services offered by IRFs. Specifically IRF admission is based on whether: the patient requires the active and ongoing therapeutic intervention of multiple therapy disciplines, one of which must be physical or occupational therapy; the patient generally requires and can reasonably be expected to actively participate in, and benefit from, an intensive rehabilitation therapy program; the patient is sufficiently stable at the time of admission to the IRF to be able to actively participate in the intensive rehabilitation therapy program; and the patient requires physician supervision by a rehabilitation physician. [ 77 ] As with all new assessment items, we will monitor all aspects of data collection and submission under the IRF QRP, and should we identify changes in provider behavior, we will take the appropriate administrative action.
Regarding the comment that we ascertain a patient's living status through assessment items already collected in the IRF-PAI, such as item 44D. Patient's Discharge Destination/Living Setting and item 45. Discharge to Living With, we disagree with the suggestion since these items are not collected until the patient is discharged. As discussed in section VII.C.4(a) of the proposed rule, we proposed the Living Situation assessment item for collection at admission, rather than at discharge. The primary purpose of collecting this information at admission is to facilitate coordinated care, continuity in care planning, and the discharge planning process from IRF settings. As we stated in section VIII.C.2 of this final rule, according to the World Health Organization, research shows that SDOH can be more important than health care or lifestyle choices in influencing health, accounting for between 30 to 55 percent of health outcomes. [ 78 ] This is part of a growing body of research that highlights the importance of SDOH on health outcomes. We believe that having information on patients' living situation at admission will help IRFs better understand and address the broader needs of their patients. We also believe this information is essential for comprehensive patient care, potentially leading to improved health outcomes and more effective discharge planning.
Comment: We received several comments supporting the collection of the two proposed Food assessment items because of the importance of nutrition and food access to IRF patients' health outcomes, and the usefulness of this information for treatment and discharge planning. Specifically, two commenters highlighted the association between a lack of access to food and low-nutrient diets with negative health outcomes. Moreover, one of these commenters noted that information from the two proposed Food assessment items can give healthcare professionals a greater understanding of a patient's complex needs and improve coordination with other healthcare providers during transitions of care. Further, one commenter noted that the responses to the proposed Food assessment items would help providers incorporate treatment strategies that address patients' food access. Finally, another commenter acknowledged the intersection between these proposed SDOH assessment items, highlighting the important relationship between transportation and a person's ability to access food. This commenter provided the example that a person may have enough funds to purchase food, but not have access to transportation to obtain food.
Response: We agree that a person's access to food affects their health outcomes and risk for adverse events. Understanding the potential needs of patients admitted to IRF through the collection of the two proposed Food assessment items can help IRFs facilitate resources for IRF patients, if indicated, when discharged.
Comment: Two commenters were concerned that the proposed Food assessment items ask patients to rate the frequency of their food shortage using a three-point scale, which is inconsistent with other questions on the IRF-PAI such as the patient mood, behavioral symptoms, and daily preference assessment items, which use a four-point scale to determine frequency. This commenter suggested this inconsistency may lead to confusion for staff and patients.
Response: We clarify that the proposed Food assessment items include three frequency responses in addition to response options in the event the patient declines to respond or is unable to respond: (0) Often true; (1) Sometimes true; (2) Never True; (7) Patient declines to respond; and (8) Patient unable to respond. We acknowledge there are a number of patient interview assessment items on the IRF-PAI that use a four-point scale, but there are also assessment items on the IRF-PAI that do not use a four-point scale. For example, the Health Literacy (B1300) and Social Isolation (D0700) assessment items currently use a five-point scale and the Pain Interference with Therapy Activities (J0520) assessment item currently uses a five-point scale. We chose the proposed Food assessment items from the AHC HRSN Screening Tool, and it was tested and validated using a three-point response scale. Since the IRF-PAI currently includes assessment items that use varying response scales, we do not believe staff and patients will be confused. We plan to develop resources IRF staff can use to ensure patients understand the proposed assessment item questions and response options. For example, CMS developed cue cards to assist IRFs in conducting the Brief Interview for Mental Status (BIMS) in Writing, the Patient Mood Interview (PHQ-2 to 9), the Pain Assessment Interview, and the Interview for Daily and Activity Preference. [ 79 ]
Comment: Several commenters were concerned with the 12-month look back period of the proposed Food assessment items, noting that this broad look back period may capture needs that occurred in the past that have already been resolved. These commenters recommended a 3-month look back period instead, to capture true concerns that should inform IRFs' care and discharge planning.
Response: We disagree that the 12-month look back period for the proposed Food assessment items is too long and will not result in reliable responses. We believe the proposed 12-month look back is more appropriate than a shorter, 3-month look back period, because a person's Food situation may fluctuate over time. One study of Medicare Advantage beneficiaries found that approximately half of U.S. adults report one or more HRSNs over four quarters. However, at the individual level, participants had substantial fluctuations: 47.4 percent of the participants fluctuated between zero and one or more HRSNs over the four quarters, and 21.7 percent of participants fluctuated between one, two, three, or four or more HRSNs over the four quarters. [ 80 ] The researchers noted that the dynamic nature of individual-level HRSNs requires consideration by healthcare providers screening for HRSNs.
To account for potentially changing Food needs over time, we believe it is important to use a longer lookback window to comprehensively capture any Food needs a person may have had, so that IRFs may consider them in their care and discharge planning. However, as we develop coding guidance for these proposed new assessment items, we will utilize the feedback received in these comments.
Comment: One commenter recognized the importance of collecting patients' food access through a streamlined data collection process but urged CMS to combine the two proposed Food assessment items into a singular comprehensive assessment item to enhance efficiency and reduce respondent burden, while still capturing the nuanced aspects of food insecurity crucial for care planning and recourse allocation.
Response: While we appreciate the commenters' recommendation, past testing of the items found that the item sensitivity was higher when using both Food assessment items, as opposed to just one. Specifically, analyses found that an affirmative response to just one of the questions provided a sensitivity of 93 percent or 82 percent, depending on the item, whereas collecting both items, and evaluating whether there is an affirmative response to the first and/or second item yielded a sensitivity of 97 percent. [ 81 ] This means that only 3 percent of respondents who have food needs were likely to be misclassified. Therefore, we believe it is important to include both proposed Food assessment items.
Comment: One commenter urged CMS to recommend that IRFs complete the proposed Food assessment items in the IRF-PAI as soon as applicable for the patient after admission. This commenter highlighted that timely diagnoses of nutrition insecurity allows for immediate planning of future post-discharge plans. Because referrals and enrollment in public programs like the Supplemental Nutrition Assistance Program (SNAP) often have wait times that delay access to necessary interventions, they suggested CMS encourage IRFs to minimize delays in the delivery of adequate nutrition assistance and malnutrition intervention.
Response: We appreciate the commenter's input on timely collection of the proposed Food assessment items, and we note that in section VIII.C.3.(b) of this final rule, we proposed to collect these assessment items at admission only. Admission information on the IRF-PAI is collected as close to the time of admission as possible. As we develop coding guidance for the proposed new Food assessment item, we will utilize the feedback received in these comments.
Comment: One commenter supported the proposal to add a new Utilities assessment item to the IRF-PAI and highlighted that a patient's access to utilities, similar to a patient's living situation, is crucial for maintaining good health. Specifically, they pointed out that access to clean water is essential, particularly for patients who are unable to drive or have the funds to purchase bottled water. Additionally, this commenter highlighted that IRF patients are often discharged with equipment requiring constant, consistent electricity (for example, supplemental oxygen, vents, continuous positive airway pressure (CPAP), bilevel positive airway pressure (BiPAP), continuous ambulatory delivery device (CADD) pumps for Dobutamine and left ventricular assist device (LVAD)). If a patient does not have access to a reliable power source for these critical supports, they are at risk of not using the equipment as prescribed or dying.
Response: We thank the commenters for their support and agree that patients' utilities needs can affect IRF patients' health outcomes, and the collection of the proposed Utilities assessment item can equip IRFs with the information to inform care plans and discharge planning.
Comment: A few commenters were concerned with the 12-month look back period of the proposed Utilities assessment item. Two of these commenters noted that the 12-month look back period may not result in reliable responses because patients may have difficulty remembering if a relevant event, such as a utility shut-off threat, occurred within such a long period, especially for patients that may be recovering from a stroke or traumatic brain injury. Three of these commenters recommended a 3-month look back period instead, to provide more reliable, valid, timely, and actionable information as part of the transition of care. These commenters also recommended against the inclusion of all utilities (electric, gas, oil, or water) in the assessment item as well as the use of the term “threatened” in the proposed Utilities assessment item because they are concerned these all-encompassing and vague terms may lead to inconsistent, unreliable, or invalid responses.
Response: We disagree that the 12-month look back period for the proposed Utilities assessment item is too long and that it will not result in reliable responses. We believe a 12-month look back is more appropriate than a shorter, 3-month look back period, because a person's Utilities situation may fluctuate over time. One study of Medicare Advantage beneficiaries found that approximately half of U.S. adults report one or more HRSNs over four quarters. However, at the individual level, participants had substantial fluctuations: 47.4 percent of the participants fluctuated between zero and one or more over the four quarters, and 21.7 percent of participants fluctuated between one, two, three, or four or more over the four quarters. [ 82 ] The researchers noted that the dynamic nature of individual-level HRSNs requires consideration by healthcare providers screening for HRSNs. In order to account for potentially changing Utilities needs over time, we believe it is important to use a longer lookback window to comprehensively capture any Utilities needs a person may have had, so that IRFs may consider them in their care and discharge planning.
We also acknowledge that IRFs are accustomed to working with patients with very complex medical conditions, including traumatic brain injury, stroke, and others, and we are confident in their ability to collect this data in a consistent manner. There are currently several patient interview assessment items on the IRF-PAI, and IRFs are accustomed to administering these questions to impaired patients. We remind IRFs we proposed response options for the Utilities item that address when a patient declines to respond or when a patient is unable to respond.
We also believe it is important to capture utility needs across electric, gas, oil, and water services, in order to comprehensively understand patients' access to necessary utility services, especially since patients' needs for utilities may vary depending on their equipment needs at discharge. We note that while the IRF-PAI requires the collection of certain HRSNs, IRFs may screen for additional HRSNs that they believe are relevant for their patient population and the community in which they serve. For example, if it is useful to understand patients' access to a specific type of utility service, such as access to water or voltage capacity, IRFs may seek to collect any additional information they believe relevant for their patient population in order to inform their care and discharge planning process. However, as we develop coding guidance for the proposed new Utilities assessment item, we will utilize the feedback received in these comments.
After careful consideration of public comments we received, we are finalizing our proposal to adopt four new items as standardized patient assessment data elements under the SDOH category beginning with the FY 2028 IRF QRP: one Living Situation item; two Food items; and one Utilities item.
Beginning October 1, 2022, IRFs began collecting seven items adopted as standardized patient assessment data elements under the SDOH category on the IRF-PAI. [ 83 ] One of these items, Item A1250. Transportation collects data on whether a lack of transportation has kept a patient from getting to and from medical appointments, meetings, work, or from getting things they need for daily living. This item was adopted as a standardized patient assessment data element under the SDOH category in the FY 2020 IRF PPS final rule ( 84 FR 39158 and 39159 ). As we discussed in the FY 2020 IRF PPS final rule ( 84 FR 39158 ), we continue to believe that access to transportation for ongoing health care and medication access needs, particularly for those with chronic diseases, is essential to successful chronic disease management and the collection of a Transportation item would facilitate the connection to programs that can address identified needs.
As part of our routine item and measure monitoring work, we continually assess the implementation of the new SDOH items. We have identified an opportunity to improve the data collection for A1250. Transportation in the IRF-PAI by aligning it with the Transportation category collected in our other programs. [ 84 85 ] Specifically, we proposed to modify the current Transportation item in the IRF-PAI so that it aligns with a Transportation item collected on the AHC HRSN Screening Tool available to the IPFQR and Hospital IQR Programs.
A1250. Transportation collected in the IRF-PAI asks: “Has lack of transportation kept you from medical appointments, meetings, work, or from getting things needed for daily living?” The response options are: (A) Yes, it has kept me from medical appointments or from getting my medications; (B) Yes, it has kept me from non-medical meetings, appointments, work, or from getting things that I need; (C) No; (X) Patient unable to respond; and (Y) Patient declines to respond. The Transportation item collected in the AHC HRSN Screening Tool asks, “In the past 12 months, has lack of reliable transportation kept you from medical appointments, meetings, work or from getting things needed for daily living?” The two response options are: (1) Yes; and (2) No. Consistent with the AHC HRSN Screening Tool, we proposed to modify the A1250. Transportation item collected in the IRF-PAI in two ways: (1) revise the look back period for when the patient experienced lack of reliable transportation; and (2) simplify the response options.
First, the proposed modification of the Transportation item would use a defined 12-month look back period, while the current Transportation item uses a look back period of six to 12 months. We believe the distinction of a 12-month look back period would reduce ambiguity for both patients and clinicians, and therefore improve the validity of the data collected. Second, we proposed to simplify the response options. Currently, IRFs separately collect information on whether a lack of transportation has kept the patient from medical appointments or from getting medications, and whether a lack of transportation has kept the patient from non-medical meetings, appointments, work, or from getting things they need. Although transportation barriers can directly affect a person's ability to attend medical appointments and obtain medications, a lack of transportation can also affect a person's health in other ways, including accessing goods and services, obtaining adequate food and clothing, and social activities. [ 86 ] The proposed modified Transportation item would collect information on whether a lack of reliable transportation has kept the patient from medical appointments, meetings, work, or from getting things needed for daily living, rather than collecting the information separately. As discussed previously, we believe reliable transportation services are fundamental to a person's overall health, and as a result, the burden of collecting this information separately outweighs its potential benefit.
For the reasons stated previously, we proposed to modify A1250. Transportation based on the Transportation item adopted for use in the AHC HRSN Screening Tool and adapted from the PRAPARE tool. The proposed Transportation item asks, “In the past 12 months, has a lack of reliable transportation kept you from medical appointments, meetings, work or from getting things needed for daily living?” The proposed response options are: (0) Yes; (1) No; (7) Patient declines to respond; and (8) Patient unable to respond. A draft of the proposed modified Transportation item can be found in the Downloads section of the IRF-PAI and IRF-PAI Manual web page at https://www.cms.gov/medicare/quality/inpatient-rehabilitation-facility/irf-pai-and-irf-qrp-manual .
We solicited comment on the proposal to modify the current Transportation item previously adopted as a standardized patient assessment data element under the SDOH category beginning with the FY 2028 IRF QRP.
Comment: Several commenters supported the proposal to modify the Transportation assessment item. One of these commenters stated that knowing this information will allow the IRF to connect patients, particularly those who are dependent on a wheelchair or other assisted device for mobility, with reliable transportation services. Four of these commenters supported the simplified response options, noting it would make it easier for patients to answer the question and reduce the administrative burden associated with the transportation assessment item. Three of these commenters also expressed support for the new 12-month look back period because it would help clarify the question, improve patient comprehension of the proposed Transportation assessment item, and reduce provider burden. One of these commenters agreed with CMS' proposal to no longer require separate response options for difficulty with transportation to medical appointments and transportation to non-medical appointments.
Response: We thank the commenters for their support of the proposed modification of the Transportation assessment item. We agree that the proposed changes will help streamline the data collection process by simplifying the item for both patients and IRF staff collecting the data. The use of a 12-month look back period will reduce ambiguity for both patients and staff, and therefore, improve the validity of the data collected.
Comment: Several commenters did not support the proposal to modify the Transportation assessment item due to the retention of the 12-month look back period. These commenters noted that the 12-month look back period is too broad and long for effective care coordination and discharge planning, and some of these commenters recommended a three-month look back period instead. Four of these commenters also noted concerns with the response options, suggesting they may not provide reliable and valid information. These commenters explained that the responses do not collect information about the frequency of the patient's concern, the reasons why they do not have reliable transportation, and consideration for patients with a disability that requires special accommodations for transportation, such as wheelchair accessibility. Finally, one commenter highlighted their concern about the utility of continuing to collect data on the current Transportation assessment item through September 30, 2025, if finalized.
Response: We disagree that the 12-month look back period for the proposed modification to the Transportation assessment item is too long and that it will not result in reliable responses. We believe a 12-month look back is more appropriate than a shorter, 3-month look back period, because a person's Transportation needs may fluctuate over time. As we have noted in an earlier response, a study of Medicare Advantage beneficiaries found that approximately half of U.S. adults report one or more HRSNs over four quarters. However, at the individual level, participants had substantial fluctuations: 47.4 percent of the participants fluctuated between zero and one or more HRSNs over the four quarters, and 21.7 percent of participants fluctuated between one, two, three, or four or more HRSNs over the four quarters. [ 87 ] The researchers noted that the dynamic nature of individual-level HRSNs requires consideration by healthcare providers screening for HRSNs. In order to account for potentially changing Transportation needs over time, we believe it is important to use a longer look back period to comprehensively capture any Transportation needs an IRF patient may have had, so that IRFs may consider them in their care and discharge planning.
Regarding the comment stating the responses do not allow for nuanced understanding of the patient's transportation needs (the frequency of the concern, the reasons why reliable transportation is not available, or the special accommodations a person may need for transportation), we note that although the proposal would require the collection of the Transportation assessment item at admission only, the collection could potentially prompt the IRF to initiate conversations with its patients about their specific Transportation needs. Additionally, IRFs may seek to collect any additional information that they believe may be relevant to their patient population in order to inform their care and discharge planning process. However, as we develop coding guidance for this Transportation assessment item, we will utilize all the feedback received in these comments.
Regarding the comment about the utility of continuing to collect an assessment item that CMS has proposed to replace, we acknowledge the commenter's concern. Although we have proposed to change the assessment item in order to improve standardization across programs, we still believe collecting the information in the interim is necessary for care coordination and discharge planning purposes in accordance with CFR 482.43(a).
After careful consideration of public comments we received, we are finalizing our proposal to modify the current Transportation item previously adopted as a standardized patient assessment data element under the SDOH category beginning with the FY 2028 IRF QRP.
In the proposed rule, we sought input on the importance, relevance, appropriateness, and applicability of each of the concepts under consideration listed in Table 14 for future years in the IRF QRP. The FY 2024 IRF PPS proposed rule ( 88 FR 21000 through 21003 ) included a request for information (RFI) on a set of principles for selecting and prioritizing IRF QRP measures, identifying measurement gaps, and suitable measures for filling these gaps. Within the FY 2024 IRF PPS proposed rule, we also sought input on data available to develop measures, approaches for data collection, perceived challenges or barriers, and approaches for addressing identified challenges. We refer readers to the FY 2024 IRF PPS final rule ( 88 FR 51036 and 51037 ) for a summary of the public comments we received in response to the RFI.
Subsequently, our measure development contractor convened a Technical Expert Panel (TEP) on December 15, 2023, to obtain expert input on the future measure concepts that could fill the measurement gaps identified in our FY 2024 RFI. [ 88 ] The TEP discussed the alignment of PAC and Hospice measures with CMS' “Universal Foundation” of quality measures. [ 89 ]
In consideration of the feedback we have received through these activities, we solicited input on three concepts for the IRF QRP (See Table 14). One is a composite of vaccinations, [ 90 ] which could represent overall immunization status of patients such as the Adult Immunization Status (AIS) measure [ 91 ] in the Universal Foundation. A second concept on which we sought feedback is the concept of depression for the IRF QRP, which may be similar to the Clinical Screening for Depression and Follow-up measure [ 92 ] in the Universal Foundation. Finally, we sought feedback on the concept of pain management.
TABLE 14—Future Measure Concepts Under Consideration for the IRF QRP
We received public comments on this RFI. The following is a summary of the comments we received:
Comments: Several commenters supported the idea of adding a composite vaccination measure like the AIS measure into the IRF QRP. These commenters noted that a composite vaccination measure could improve vaccination rates for those vaccines recommended by the Advisory Committee on Immunization Practices (ACIP), as well as reduce administrative burden through alignment with the Universal Foundation. One of these commenters noted that immunization rates in PAC settings are suboptimal and believes a measure such as the Adult Immunization Status measure would improve immunization rates in PAC settings, including IRFs.
Some commenters, however, did not support the idea of adding a composite vaccination measure into the IRF QRP for a number of reasons. They questioned whether a composite vaccination measure for the IRF QRP would be suitable and whether it would represent the quality of care provided by IRFs, described the administrative challenges a composite vaccination measure would impose on IRFs, and noted reliability and validity concerns associated with a possible vaccination composite measure.
Most commenters suggested IRFs would have difficulty collecting information on patients' vaccination status when a patient may have received care from multiple proximal providers and thought a composite vaccination measure would be better suited for primary care clinicians who usually administer these vaccines as part of their preventative care. Several commenters noted that it may be infeasible or inappropriate for an IRF to offer vaccination for patients due to length of stay, ability to manage side effects and medical contraindications. They also noted that a patient's vaccination status is dependent on many factors outside an IRF's control, including the fact that patients can choose to decline recommended vaccines. Other commenters requested that CMS provide more information on the specific outcomes CMS expects to collect from this information. One of these commenters recommended CMS report on specific vaccination rates, since it would provide more actionable data to IRFs.
Other commenters stated they were concerned about the accuracy and reliability of a composite vaccination measure for the IRF QRP since IRF patients often experience cognitive deficits related to their illness or injury and verification of their vaccination status would be difficult. Commenters noted that vaccines are intended for certain age groups and have multiple doses and medical contraindications, raising questions around data validity. Several commenters also recommended that CMS evaluate the reliability, validity, and effectiveness of existing vaccination measures before developing a composite vaccination measure.
Comments: We received several comments supporting the pain management measure concept. One of these commenters stated this was an important concept for the IRF QRP and strongly encouraged CMS to move forward with measure development and testing. Another one of these commenters recommended that these measures reflect the full spectrum of recommended pain management interventions, including nonpharmacologic pain management.
Most commenters noted that pain management is a challenging topic to address in IRFs where patients are undergoing physical rehabilitation for extremely serious conditions or injuries and the experience of pain and discomfort is usually an unavoidable reality of this process. Several of these commenters were concerned that a pain management measure in the IRF QRP focused on an expectation of improvement may be misleading and could inadvertently lead to over prescribing of pain medication, including opioids. Other commenters opposed a patient-reported pain management measure since they believe it would be an unrealistic objective for an IRF to manage a patient's pain to their expectation. These commenters suggested CMS should instead seek feedback from interested parties on the aspects of pain management relevant to IRFs and then determine if there is sufficient information to develop a meaningful quality measure.
Several commenters also noted that we are considering this measure concept for other post-acute care settings as well, including SNF and LTCH, and they believe it would invariably lead to inappropriate comparisons in pain management across PAC settings. These commenters suggested that if CMS is looking to address whether pain is managed adequately, it should seek feedback from multiple interested parties to identify what aspects of pain management are of most interest and relevance to the IRF population, such as staff responsiveness to pain, and determine if there is sufficient available information to develop a meaningful quality measure.
Other commenters stated that a more meaningful pain measure in the IRF setting should be designed to assess whether staff are responsive to and help manage patients' pain, and that such a measure could rely on patient-reported data. These commenters noted that a patient reported outcome measure [ 93 ] (PROM) would be significantly more meaningful for quality measurement than a process measure collecting the existence of pain and could be collected directly from the patient without additional measure collection burden to an IRF. Specifically, they pointed to the standardized patient assessment data elements on the IRF-PAI, including items introduced on October 1, 2022, that collect information on the level of pain interference a patient experiences with daily activities, sleep, and participation in therapy activities in section J of the IRF-PAI. These commenters believe these quality indicators in section J of the IRF-PAI could present an opportunity to develop a quality measure with no additional data collection burden to IRFs.
Comments: Many commenters supported the concept of depression for a future IRF QRP measure, and one of these commenters noted that early identification and intervention for a patient's risk of depression can improve outcomes and quality of life, since depression can hinder a patient's progress and treatment. Two commenters supported a depression and follow-up measure, suggesting that the Patient Health Questionnaire (PHQ)-2 to -9 (PHQ-2 to -9) screening tool [ 94 ] could be utilized for the development of a measure. These commenters also suggested that, if a depression measure is developed, there should not be an exclusion for patients with a prior depression or bipolar diagnosis since all symptoms of depression should be reassessed when a person is recovering from life-altering events.
Other commenters suggested that, since IRFs are already required to conduct a screening for depression using the PHQ-2 to -9 on the IRF-PAI, this screening can be used to monitor and measure the severity of depression, an additional quality measure regarding depression screening would be redundant. One commenter suggested that a depression screening measure for IRF patients would be misguided, since there are already detailed questions asked on the IRF-PAI related to depression. They also note that most patients admitted to an IRF have experienced a life-altering event(s), such as a severe accident, an act of violence, or a major injury requiring intensive rehabilitation. These events can be extremely distressing and are often accompanied by new chronic conditions that are difficult to manage. As a result, many of these patients may have post-traumatic stress disorder, which is fundamentally different from clinical depression.
Several other commenters were concerned that a depression screening measure would result in a requirement for IRFs to have additional resources to treat depression, such as a psychiatrist or psychologist. They note that IRFs already collect information and use physician documentation to identify mental health or other behavioral health issues. These commenters stated that adding another screening requirement would not improve the quality of care, or better equip these facilities to care for rehabilitation needs, and instead was best left to behavioral health and primary care providers to address. At the same time, commenters noted that such a measure could add cost and burden to the IRF clinical team. Two of these commenters recommended CMS not implement a depression measure without first determining the availability of resources to treat depression within IRFs.
Comments: In addition to comments received on the three measure concepts of pain, depression and vaccination, we also received comments suggesting other concepts for future measures for the IRF QRP, including management of degenerative cognitive conditions, effectiveness of disposition planning and care transitions, changes in patient function, rates of follow-up care, and patients' access to appropriate treatments and medications, including access to a physical medicine and rehabilitation physician. One commenter suggested we consider measures of cognition and behavior in addition to mobility. Another commenter recommended including food and nutrition security and other social determinants of health (SDOH) as future IRF QRP quality measure concepts. Finally, one commenter recommended the Patient Active Measure (PAM®) [ 95 ] instrument be added to the IRF-PAI or required in parallel to the IRF-PAI.
Response: We thank all the commenters for responding to this RFI. We will take this feedback into consideration for future development of measures for the IRF QRP.
In the proposed rule, we sought feedback on the development of a five-star methodology for IRFs that can meaningfully distinguish between quality of care offered by IRFs. Star ratings serve an important function for patients, caregivers, and families, helping them to more quickly comprehend complex information about a health care providers' care quality and to easily assess differences among providers. This transparency serves an important educational function, while also helping to promote competition in health care markets. Informed patients and consumers are more empowered to select among health care providers, fostering continued quality improvement. We refer readers to the RFI in the proposed rule ( 89 FR 22281 ) for more information.
Specifically, we invited public comment on the following questions:
1. Are there specific criteria CMS should use to select measures for an IRF star rating system?
2. How should CMS present IRF star ratings information in a way that it is most useful to consumers?
We received several comments in response to this RFI, which are summarized below.
Comments: We received many comments in response to this RFI providing feedback on the criteria we should use for selecting measures to include in a potential IRF star ratings system. Many of these commenters stated the importance of including measures that are patient-centered, and several of these commenters also stated that the measures selected for an IRF star rating system should be representative of IRFs' emphasis on functional outcomes and treating pain. Several of these commenters, as well as other commenters, suggested that the IRF star rating system should incorporate measures of clinical relevance and effectiveness, such as prevention of adverse events or readmissions, discharge to home and weaning patients from catheters or other mechanical supports. Other commenters provided more general recommendations, such as selecting measures that allow for meaningful comparisons among IRFs in order to distinguish performance.
Several commenters strongly recommended against inclusion of the Falls with Major Injury measure because of inconsistency with clinical guidelines in the IRF. These commenters also recommended against inclusion of the Catheter-Associated Urinary Tract Infection (CAUTI) measure, stating that there is a lack of meaningful differences in IRF performance.
Comments: Commenters provided recommendations on how to engage the public in the development and presentation of IRF star ratings. Several of these commenters strongly recommended CMS engage with patients, caregivers, providers, and specialty societies to inform the development and display of the IRF star ratings system. Additionally, three commenters emphasized full transparency of the star ratings methodology. Finally, one commenter recommended that visualizations of the star ratings should be clear, concise, and accompanied with contextual information to empower consumers in making informed healthcare decisions.
Several commenters noted concerns about the variation in IRF volumes across the nation and raised concerns about reportability. Specifically, they believe there will be IRFs that would not have enough publicly reported data to report a star rating. Some of these commenters also suggested that that due to the limited number of IRF quality measures and the fact that many IRFs have low patient volumes, the ability to develop an overall star rating will be challenging.
Comments: We also received several comments about IRFs' need for feedback additional reports to support their efforts at improving patient outcomes. Most of these commenters noted that the lack of patient-level reports for claims-based measures available to IRFs presents barriers to identifying areas for improvement in care. Several of these commenters, as well as other commenters, urged CMS to provide IRFs timely access to their data submitted for the IRF QRP and especially data submitted for measures that may be included in a star rating system. Three of these commenters noted that IRFs should receive feedback reports for any claims-based measures used in a star rating system on a quarterly basis, noting that CMS currently provides this level of information to hospitals. Two of these commenters recommended shortening the time period between an IRF's data submission on measures and the publicly reporting of IRFs' performance on Care Compare.
Commenters also provided recommendations on additional aspects of care, specific measures to consider, the proposed methodology, and insights from other star ratings to help shape the development of an IRF star ratings system. A few commenters recommended factoring into the star ratings system other indicators of quality such as the presence of physical medicine and rehabilitation doctors, staffing levels, staff turnover, and using the same standards as IRF accreditation bodies, such as the Commission on Accreditation of Rehabilitation Facilities (CARF). Additionally, several commenters recommended accounting for factors that differentiate IRFs such as case mix and payer mix. Another commenter recommended assessing and addressing the appropriateness of social determinants of health in and IRF star ratings system.
Finally, several commenters shared their concerns about other CMS star rating systems. Many of these commenters urged CMS to delay the implementation of an IRF star rating system until these issues with existing star ratings systems have been resolved. Another commenter recommended CMS should apply lessons learned from the development and maintenance of the existing star ratings programs as well as allow sufficient time for the development and implementation of a star rating system.
Response: We thank all the commenters for responding to the RFI on this important CMS priority. We will take these recommendations into consideration in our future star rating development efforts.
We refer readers to the regulatory text at § 412.634(b)(1) for information regarding the current policies for reporting specified data for the IRF QRP.
As discussed in sections VII.C.3. and VII.C.5. of the proposed rule, we proposed to adopt four new items as standardized patient assessment data elements under the SDOH category (one Living Situation item, two Food items, and one Utilities item) and to modify the Transportation standardized patient assessment data element previously adopted under the SDOH category beginning with the FY 2028 IRF QRP.
We proposed that IRFs would be required to report these new items and the transportation item using the IRF-PAI beginning with patients admitted on October 1, 2026, for purposes of the FY 2028 IRF QRP. Starting in CY 2027, IRFs would be required to collect and submit data for the entire calendar year with the FY 2029 IRF QRP.
We also proposed that IRFs that collect and submit the Living Situation, Food, and Utilities items with respect to admission only would be deemed to have collected and submitted those items with respect to both admission and discharge. We proposed that IRFs would be required to collect and submit these four items at admission only (and not at discharge) because it is unlikely that the assessment of those items at admission would differ from the assessment of the same item at discharge. This would align the data collection for these proposed items with other SDOH items (that is, Race, Ethnicity, Preferred Language, and Interpreter Services) which are only collected at admission. [ 96 ] A draft of the proposed items is available in the Downloads section of the IRF-PAI and IRF-PAI Manual web page at https://www.cms.gov/medicare/quality/inpatient-rehabilitation-facility/irf-pai-and-irf-qrp-manual .
As we noted in section VIII.C.5. of this final rule, we continually assess the implementation of the new SDOH items, including A1250. Transportation, as part of our routine item and measure monitoring work. We received feedback from interested parties in response to the FY 2020 IRF PPS proposed rule ( 84 FR 39149 through 39161 ) noting their concern with the burden of collecting the Transportation item at admission and discharge. Specifically, commenters stated that a patient's access to transportation is unlikely to change between admission and discharge ( 84 FR 39159 ). We analyzed the data IRFs reported from October 1, 2022, through June 30, 2023 (Quarter 4 CY 2022 through Quarter 2 CY 2023) and found that patient responses do not significantly change from admission to discharge. [ 97 ] Specifically, the proportion of patients [ 98 ] who responded “Yes” to the Transportation item at admission versus at discharge differed by only 0.19 percentage points during this period. We find these results convincing, and therefore we proposed to require IRFs to collect and submit the proposed modified standardized patient assessment data element, Transportation, at admission only.
We invited public comment on our proposal to collect data on the following items proposed as standardized patient assessment data elements under the SDOH category at admission beginning October 1, 2026 with the FY 2028 IRF QRP: (1) Living Situation as described in section VII.C.3.(a) of the proposed rule; (2) Food as described in section VII.C.3.(b) of the proposed rule; and (3) Utilities as described in section VII.C.3.(c) of the proposed rule. We also invited comment on our proposal to collect and submit the proposed modified standardized patient assessment data element, Transportation, at admission only beginning October 1, 2026, with the FY 2028 IRF QRP as described in section VII.C.5. of the proposed rule.
We received public comments on these proposals. The following is a summary of the comments we received and our responses.
Comment: Several commenters supported the proposed collection of four new SDOH assessment items once, upon admission, noting that this could mitigate the administrative burden of data collection and reduce redundancy. One of these commenters recommended CMS change the collection requirements for all standardized patient assessment data elements in the SDOH category to admission only, because they believe that for most patients, the response is not going to change between admission and discharge.
In addition, several commenters supported the proposal to collect the modified Transportation assessment item at admission only, and one of these commenters agreed with CMS that the response to the Transportation assessment item is unlikely to change during the IRF stay. These commenters noted that removing the Transportation assessment item at discharge will reduce redundancy, improve the patient experience, and improve and align data collection.
Response: We appreciate the commenters' support in requiring the proposed SDOH assessment items at admission only. We continually assess the implementation of the new SDOH assessment items as part of our routine assessment item and measure monitoring work, and when we identify an opportunity to improve data collection, we want to implement it. In the FY 2025 IRF Proposed Rule ( 89 FR 22281 and 22282 ), we proposed to collect these new and modified assessment items at admission only because we believe it is unlikely that the assessment of these items at admission would differ from the assessment of the same items at discharge. We are mindful of provider burden and appreciate the support from several commenters who agreed that collection at admission only, rather than at both admission and discharge, would mitigate the administrative burden of data collection on these new and modified assessment items.
Comment: Two commenters suggested CMS offer flexibility for IRFs on how to collect the proposed SDOH assessment items, and not mandate the assessment items on the AHC HRSN Screening Tool. One of the commenters stated that they believed CMS' focus should be on whether the information is collected and less on the specific vendor or tool used for collection. The other commenter noted that flexibility in gathering screening information would allow IRFs to use their own methods of identifying patients' needs and the best time to collect this information.
Three commenters noted that CMS already collects many of the proposed SDOH assessment items from other health care providers, such as hospitals or other post-acute providers, prior to an IRF stay. These commenters recommended CMS allow IRF-PAI responses to be based upon data already collected in other settings of the hospital or health system when it is available prior to admission at an IRF to avoid unnecessary duplication of screenings and assessments.
Response: We interpret these commenters to be suggesting that CMS should allow IRFs to obtain information collected in previous healthcare settings, rather than requiring IRFs to obtain this information from the patient upon the patient's admission to the IRF. We appreciate that many IRFs may share electronic health record systems with referring hospitals. However, we proposed the collection of these assessment items through patient interview in an effort to increase the patient's voice in the assessment process and the IRF QRP. Obtaining information about the Living Situation, Food, Utilities, and Transportation assessment items directly from the patient, sometimes called “hearing the patient's voice,” is more reliable and accurate than obtaining it from a health care provider that previously cared for the patient for several reasons: the IRF would not know whether it was collected from the patient or from a family member or other source; the IRF would not know how the SDOH domain was defined—for example, whether utilities included electricity, gas, oil, or water or only asked about electricity; and the IRF would not be able to determine whether the potential problem had been resolved since then. Most importantly, we believe that by asking the patient these questions at admission, it may prompt further discussion with the patient about their needs and help formulate an appropriate discharge care plan.
We also want to clarify that the proposed SDOH assessment items will not require the use of a new collection tool, because the assessment items will be collected through the IRF-PAI, in the same way other standardized patient assessment data elements are collected. IRFs may use different methods to collect the information from the patient, as long as they are consistent with the coding guidance and defined lookback periods in the IRF-PAI manual. As we develop guidance for these new assessment items, we will utilize the feedback received in these comments.
Comment: Several commenters offered suggestions or recommendations for guidance related to collecting the proposed SDOH assessment items. One commenter recommended that CMS include coding logic to allow skipping the Utilities assessment item if a patient indicated that they do not have a steady place to live, since it would be inappropriate to ask about utilities if a patient has no place to live.
Response: We appreciate all the comments we received about coding these proposed new and modified SDOH assessment items, including the Utilities assessment item. We proposed that IRFs would be required to collect and submit information on the four new assessment items, in order to have complete information. We do not agree that it would be inappropriate to ask about utilities just because a patient does not have a place to live at the time of the assessment. The patient may be living in temporary housing or a shelter, and gathering this information would still be important for their discharge planning.
In response to the commenter who noted that patients may be uncomfortable sharing sensitive personal information with facility staff, we acknowledge that the proposed SDOH assessment items require the patient to be asked potentially sensitive questions. We also note that we proposed additional response options for these new and modified SDOH items for patients that decline to respond or are unable to respond. We encourage IRFs to assess all patients and select the appropriate response options for all SDOH assessment items.
Comment: Some commenters were concerned that the proposed SDOH assessment items are not applicable to certain types of patients receiving care in the IRF setting, including patients younger than 18 years old and patients requiring special accommodations. Many commenters highlighted that beginning October 1, 2024, IRFs will begin collecting IRF-PAI data on all patients regardless of payer and recommended that CMS exclude patients under 18 from these assessments because the proposed assessment items have not been validated or tailored for the pediatric and adolescent populations. One of these commenters stated the PRAPARE website Frequently Asked Questions (FAQs) stated, “Currently there is no PRAPARE version that is specifically tailored for pediatrics/adolescents. There are health centers who have modified PRAPARE to be used with their pediatric and adolescent populations, which varies based on their staffing model and engagement of family members. The National NACHC team hopes to develop a Pediatric/Adolescent version of PRAPARE in the coming years.” [ 99 ]
Response: We are uncertain what the commenter's concerns are related to collecting the items adapted from the PRAPARE tool, Living Situation and Transportation, from patients younger than 18 years old, but we interpret the commenter to be concerned that these patients would be too young to provide a response or that these patients may be too young to own a house or have a driver's license, so the questions would not be applicable to them.
In response to the potential concern that patients would be too young to provide a response, we highlight that there is growing recognition of the need for effective screening methods for HRSNs in all patient populations, including pediatrics and adolescents. Children are especially vulnerable to HRSNs, as poverty in childhood correlates to poor health outcomes. [ 100 101 102 ] Although there is no standardized protocol for screening in pediatric settings, [ 103 ] organizations like the American Academy of Pediatrics provide toolkits with suggestions for a screening protocol. Housing and transportation have been identified by hospitals and clinics [ 104 105 ] that care for pediatric and adolescent patients as an important area to screen. One hospital system began using the AHC HRSN Screening Tool, including the proposed Living Situation and Transportation item, during selected well child visits at a Federally Qualified Health Center, and found the tool was feasible to administer and identified more than a third of patients with one or more HRSNs. [ 106 ]
In response to the potential concern that the question would not be applicable to these patients because they may be too young to own a house or have a driver's license, we believe that even if a patient younger than 18 years old cannot own a house or drive themselves, they may rely on others, or they may live in shelters and use public transportation. As a result, they may still have living situation and transportation access needs that should be identified.
Finally, we interpret the second part of the comment to be recommending that CMS modify the response options to collect information about patients requiring special transportation accommodations. We note that although the proposal would require IRFs to collect the modified Transportation assessment item as described in section VIII.F.2. of this final rule, such collection could potentially prompt the IRF to initiate conversations with its patients about their potential Transportation needs, such as special accommodations a patient may need to access transportation. Additionally, IRFs may seek to collect any additional information that they believe may be relevant to their patient population in order to inform their care and discharge planning process.
Comment: Several commenters were also concerned that the proposed SDOH assessment items will be challenging for IRF patients to respond to, considering that many IRF patients have cognitive deficits as a result of a traumatic injury or are more severely ill than the average Medicare beneficiary for which the screening tool was developed. One of these commenters recommended that CMS reassess the wording and response options for the SDOH assessment items to account for these patients.
Response: We interpret the comments to be recommending that CMS reassess the wording and response options for the proposed SDOH assessment items to account for these patients with cognitive impairment. However, we believe IRFs are accustomed to working with patients with very complex medical conditions, including traumatic brain injury, stroke, and others, and we are confident in their ability to collect this data in a consistent manner. There are currently several patient interview assessment items on the IRF-PAI, and IRFs are accustomed to administering these questions to cognitively impaired patients.
We also plan to provide training resources in advance of the initial collection of the assessment items to ensure that IRFs have the tools necessary to administer the new SDOH assessment items and reduce the burden to IRFs in creating their own training resources. These training resources may include online learning modules, tip sheets, questions and answers documents, and/or recorded webinars and videos, and would be available to providers as soon as technically feasible.
After careful consideration of public comments we received, we are finalizing our proposal to require IRFs to collect and submit data on the following items adopted as standardized patient assessment data elements under the SDOH category at admission only beginning with the FY 2028 IRF QRP: (1) Living Situation as described in section VIII.C.3(a) of this final rule; (2) Food as described in section VIII.C.3(b) of this final rule; and (3) Utilities as described in section VIII.C.3(c) of this final rule. We are also finalizing our proposal to require IRFs to collect and submit the modified standardized patient assessment data element, Transportation, at admission only beginning October 1, 2026, with the FY 2028 IRF QRP as described in section VIII.C.5 and VIII.E.2. of this final rule.
In the CY 2002 PPS for IRFs final rule ( 66 FR 41324 through 41342 ), we finalized the use of the IRF-PAI, through which IRFs are now required to collect and electronically submit patient data for all Medicare Part A FFS and Medicare Part C (Medicare Advantage) patients admitted and discharged from an IRF through September 30, 2024 [ 107 ] and for all patients regardless of payer beginning October 1, 2024. [ 108 ] Item 14-Admission Class has been included on the IRF-PAI since the IRF-PAI was first implemented and is completed only at admission. The most recent version of the IRF-PAI is available for reference on the IRF-PAI and IRF QRP Manual web page at https://www.cms.gov/medicare/quality/inpatient-rehabilitation-facility/irf-pai-and-irf-qrp-manual . Item 14-Admission Class, includes the following response options: (i) Initial Rehab; (iii) Readmission; (iv) Unplanned Discharge; and (v) Continuing Rehabilitation.
We routinely review item sets for redundancies and identify opportunities to simplify data submission requirements. We proposed to remove Item 14-Admission Class entirely from the IRF-PAI, beginning October 1, 2026. We identified this item is currently not used in the calculation of quality measures already adopted in the IRF QRP. It is also not used for previously established purposes unrelated to the IRF QRP, such as payment, survey, or care planning.
We invited public comment on the proposal to remove Item 14-Admission Class from the IRF-PAI, effective October 1, 2026.
Comment: Most commenters supported the proposal to remove Item 14-Admission Class from the IRF-PAI, pointing to its lack of value to the assessment process. One of these commenters appreciated CMS' review of the IRF-PAI to identify potential items for removal. The other commenters acknowledged that the proposed removal aligns with CMS' commitment to reducing administrative burden and agreed that it would result in a reduction in administrative burden.
Response: We thank the commenters for their support of the proposed removal of Item 14-Admission Class and agree that the removal of this item will reduce administrative burden for IRFs.
Comment: Four commenters suggested that CMS perform additional analysis of the IRF-PAI and other PAC patient assessment tools to identify additional items that could be removed.
Response: As part of our routine item and measure monitoring work, we continually assess the implementation of items collected on the IRF-PAI. We will continue to look for opportunities to improve data collection using the IRF-PAI, including considering items to remove from the IRF-PAI in order to reduce administrative burden.
Comment: Three commenters expressed concerns about removing the item and its potential impact on data collection requirements. They noted that response option (4) Unplanned Discharges is used to activate a skip pattern for incomplete stays in the IRF-PAI data specifications. These commenters suggested CMS conduct an impact analysis to identify the implications of the item removal. Two commenters suggested CMS modify the item, instead of removing it, to track incomplete stays and use the item to trigger skip patterns across the IRF-PAI in cases of unplanned discharges.
Response: We acknowledge the commenters' concerns about the item's use with triggering skip patterns in the data specifications, but the data specifications currently include a means to identify incomplete stays that does not rely on Item 14-Admission Class. Therefore, this item is not necessary. Additionally, as we noted in the proposed rule and this section of this final rule, we have identified that this item is currently not used in the calculation of quality measures already adopted in the IRF QRP, nor is it used for previously established purposes unrelated to the IRF QRP, such as payment, survey, or care planning. Therefore, its removal will not have an impact in our data, such as activation of a skip pattern for incomplete stays. Additionally, we conduct regular item monitoring and carefully consider the downstream implications of removing any item from the IRF-PAI. Accordingly, prior to proposing removal of this item, we analyzed CY 2023 assessment data and confirmed less than one percent of IRF-PAI admission assessments are coded as incomplete stays using Item 14-Admission Class. CMS will continue to monitor and assess changes resulting from removal of this item to ensure there are no unintended consequences or added burden to providers.
Comment: One commenter suggested that CMS remove the item from the IRF-PAI beginning October 1, 2024, instead of the proposed October 1, 2026 date. This commenter noted that delaying the removal of the Item 14-Admission Class item until October 1, 2026 is unreasonable provided IRFs are still required to collect and submit data for the Admission Class item even though CMS is not utilizing the information.
Response: We appreciate the commenter's suggestion, but we proposed October 1, 2026, to effectuate this change. Removing an item from the IRF-PAI has downstream logistical implications, such as changes to data submission specifications, updates to the assessment instruments, revisions to the IRF-PAI guidance manual, and provider training, if necessary. For example, we finalized and published the IRF-PAI 4.2 item set that will be effective October 1, 2024, almost 12 months before the October 12, 2023, to allow providers adequate time for preparation. The IRF-PAI Manual Version 4.0 was published over 7 months before the October 1, 2024 on February 1, and the IRF data specifications V5.00.1 were published over 4 months before the October 1, 2024 on May 25, 2024. Additionally, to allow for adequate time to draft, test and implement item set changes, we typically follow a 2-year cycle of updates to the item sets. Therefore, IRFs will continue to see Item 14-Admission Class on the IRF-PAI until the next release of the IRF-PAI on October 1, 2026.
However, we acknowledge that there is no longer a need to collect this information at admission. Therefore, we are finalizing our proposal with modification to reflect that IRFs would no longer be required to collect Item 14-Admission Class at admission beginning with patients admitted on October 1, 2024. Item 14-Admission Class is not a standardized patient assessment data element and therefore its completion does not have an impact on an IRF's annual compliance determination for the IRF QRP.
After careful consideration of public comments we received, we are finalizing our proposal to remove Item 14-Admission Class from the IRF-PAI with modification. Specifically, while we are finalizing our proposal to remove Item 14-Admission Class from the IRF-PAI effective October 1, 2026 as proposed, IRFs will no longer be required to collect and submit data on this Item 14-Admission Class beginning with patients admitted on October 1, 2024.
We did not propose any new policies regarding the public display of measure data in the proposed rule. For a more detailed discussion about our policies regarding public display of IRF QRP measure data and procedures for the opportunity to review and correct data and information, we refer readers to the FY 2017 IRF PPS final rule ( 81 FR 52125 through 52131 ).
Under the Paperwork Reduction Act of 1995, we are required to provide 60-day notice in the Federal Register and solicit public comment before a collection of information requirement is submitted to the Office of Management and Budget (OMB) for review and approval. In order to fairly evaluate whether an information collection should be approved by OMB, section 3506(c)(2)(A) of the Paperwork Reduction Act of 1995 requires that we solicit comment on the following issues:
- The need for the information collection and its usefulness in carrying out the proper functions of our agency.
- The accuracy of our estimate of the information collection burden.
- The quality, utility, and clarity of the information to be collected.
- Recommendations to minimize the information collection burden on the affected public, including automated collection techniques.
This final rule refers to associated information collections that are not discussed in the regulation text contained in this document.
An IRF that does not meet the requirements of the IRF QRP for a fiscal year will receive a 2-percentage point reduction to its otherwise applicable annual increase factor for that fiscal year.
In section VII.C. of the proposed rule, we proposed to adopt four items as standardized patient assessment data elements and modify one item currently collected and submitted as a standardized patient assessment data element beginning with the FY 2028 IRF QRP. In section VII.F.3. of the proposed rule, we proposed to remove one item, Item 14-Admission Class, from the IRF-PAI.
As stated in sections VIII.C.3. and VIII.C.5. of this final rule, we proposed to adopt four items as standardized patient assessment data elements and modify one item currently collected and submitted as a standardized patient assessment data element beginning with the FY 2028 IRF QRP. The four new and modified items would be collected and submitted using the IRF-PAI. The IRF-PAI, in its current form, has been approved under OMB control number 0938-0842. [ 109 ] Four items will need to be added to the IRF-PAI at admission to allow for collection of these data, and one item would be modified. Additionally, as stated in section VIII.F.2. of this final rule, we proposed that IRFs would submit the four new items and one modified item at admission only. The net result of collecting and submitting four new items at admission, modifying the Transportation item (including the modification that this item be collected at admission only, rather than at admission and discharge is an increase of 0.9 minutes or 0.015 hour of clinical staff time at admission [(4 items × 0.005 hour) minus (1 item × 0.005 hour)]. We identified the staff type based on past IRF burden calculations, and our assumptions are based on the categories generally necessary to perform an assessment. We believe that the items would be completed equally by a Registered Nurse (RN) (50 percent of the time) and a Licensed Practical and Licensed Vocational Nurse (LPN/LVN) (50 percent of the time). However, IRFs determine the staffing resources necessary.
For the purposes of calculating the costs associated with the collection of information requirements, we obtained median hourly wages for these staff from the U.S. Bureau of Labor Statistics' (BLS) May 2022 National Occupational Employment and Wage Estimates. [ 110 ] To account for other indirect costs and fringe benefits, we doubled the hourly wage. These amounts are detailed in Table 15. We established a composite cost estimate using our adjusted wage estimates. The composite estimate of $65.31/hr was calculated by weighting each adjusted hourly wage equally (that is, 50 percent) [($78.10/hr × 0.5) + ($52.52/hr × 0.5) = $65.31].
| Occupation title | Occupation code | Median hourly wage ($/hr) | Other indirect costs and fringe benefit ($/hr) | Adjusted hourly wage ($/hr) |
|---|---|---|---|---|
| Registered Nurse (RN) | 29-1141 | $39.05 | $39.05 | $78.10 |
| Licensed Practical and Licensed Vocational Nurse (LPN/LVN) | 29-2061 | 26.26 | 26.26 | 52.52 |
We estimated that the burden and cost for IRFs for complying with requirements of the FY 2028 IRF QRP would increase under this proposal. Using FY 2023 data, we estimate a total of 571,151 admissions to and 512,677 planned discharges from 1,160 IRFs annually for an increase of 8,859.64 hours in burden for all IRFs [(571,151 × 0.02 hour) admissions−(512,677 × 0.005 hour) planned discharges]. Given 0.02 hour at $65.31 per hour to complete an average of 492 IRF-PAI admission assessments per IRF per year minus 0.005 at $65.31 per hour to complete an average of 442 IRF-PAI Planned Discharge assessments per IRF per year, we estimate the total cost will be increased by $498.81 per IRF annually, or $578,622.76 for all IRFs annually.
In section VIII.F.3. of this final rule, we proposed to remove one item, Item 14-Admission Class, from the IRF-PAI beginning October 1, 2026. We believe that the removal of Item 14-Admission Class will result in a decrease of 18 seconds (0.3 minutes or 0.005 hours) of clinical staff time at admission beginning with the FY 2028 IRF QRP. We believe the IRF-PAI item, Item 14-Admission Class, is completed equally by a Registered Nurse (RN) and a Licensed Practical and Licensed Vocational Nurse (LPN/LVN). Individual IRFs determine the staffing resources necessary.
We estimated that the burden and cost for IRFs for complying with requirements of the FY 2028 IRF QRP will decrease under this proposal in section VIII.F.3. Specifically, we believe that there will be a 2.46 hour decrease in clinical staff time to report data for each IRF-PAI completed at admission. Using data from FY 2023, we estimated 571,151 admission assessments from 1,160 IRFs annually. This equates to a decrease of 2,855.76 hours in burden at admission for all IRFs (0.005 hour × 571,151 admissions). Given 0.005 hour at $65.31 per hour to complete an average of 492 IRF-PAI admission assessments per IRF per year, we estimated the total cost will be decreased by $160.78 ($186,509.36 total decrease/1,160 IRFs) per IRF annually, or $186,509.36 for all IRFs annually, based on the proposal to remove one item from the IRF-PAI.
In summary, under OMB control number 0938-0842, the changes to the IRF QRP will result in a burden increase of $338.03 per IRF ($392,113.40/1,160 IRFs). The total cost increase related to this proposed information collection is approximately $392,113.40 and is summarized in Table 16.
| Requirement | Per IRF | All IRFs | ||
|---|---|---|---|---|
| Estimated change in annual burden hours | Estimated change in annual cost | Estimated change in annual burden hours | Estimated change in annual cost | |
| Collection of Four New Items as Standardized Patient Assessment Data Elements and Modification of One Item Collected as a Standardized Patient Assessment Data Element beginning with the FY 2028 IRF QRP | +7.64 | +$498.81 | +8,859.64 | +$578,622.76 |
| Removal of Item 14-Admission Class item effective October 1, 2026 | −2.46 | −$160.78 | −2,855.76 | −$186,509.36 |
| Change in burden for the IRF QRP associated with 0938-0842 | 5.18 | $338.03 | 6,003.88 | $392,113.40 |
We invited public comments on the proposed information collection requirements. The following is a summary of the public comments received on the proposed information collection requirements as well as our responses.
Comment: Three commenters urged CMS to update its estimate of the change in burden resulting from these new IRF QRP changes to account for the costs associated with training and education, time required to administer and reconcile patient assessments, and costs associated with software development and other required technical updates. One of these commenters specifically noted they do not believe the estimate accurately reflects the time to conduct patient interviews and reconcile information from the patient nor does it account for the costs associated with software development and other technology that will make the collection of this information easier and timelier for IRFs and other providers.
Response: We acknowledge that the net effect of our policies finalized in this final rule is an increase of $338.03 per IRF per year.
The burden estimate for the proposed SDOH items is based on past IRF burden calculations and represents the time it takes to encode the IRF-PAI. As the commenter pointed out in their example, the patient must be assessed and information gathered. After the patient assessment is completed, the IRF-PAI is coded with the information and submitted to the internet Quality Improvement and Evaluation System (iQIES), and it is these steps (after the patient assessment) that the estimated burden and cost captures. This method is consistent with past collection of information estimates. [ 111 ]
We also note that some IRFs will incur a higher cost than was estimated due to their size and volume of admissions, and some IRFs will incur a lower cost. Regarding the comments about IRFs' costs associated with training and education, time required to administer and reconcile patient assessments, and costs associated with software development and other required technical updates, CMS continually looks for opportunities to minimize burden associated with collection and submission of the IRF-PAI for information users through strategies that simplify collection and submission requirements. This includes standardizing instructions, providing a help desk, hosting a dedicated web page, communication strategies, free data specifications, and free on-demand reports. We describe each of those below and how they will potentially reduce new burden on IRFs collecting and submitting these new and modified SDOH assessment items.
First, we will standardize the collection instructions for the new and modified SDOH assessment items across all IRFs, ensuring that all instructions and notices are written in plain language, and by providing step-by-step examples for completing the IRF-PAI. Second, CMS provides a dedicated help desk to support users and respond to questions about the data collection, and IRFs can utilize this help desk when they have questions about the new and modified SDOH assessment items. Third, a dedicated IRF QRP web page houses multiple modes of tools, such as instructional videos, case studies, user manuals, and frequently asked questions. We plan to update this web page with new resources to support IRFs' understanding of the new SDOH assessment items and the modified assessment item as soon as technically feasible, and these resources will be available to all users of the IRF-PAI. Fourth, CMS utilizes a listserv to facilitate outreach to users, such as communicating timely and important new material(s), and we will use those outreach resources when providing training and information about the new and modified SDOH assessment items. Fifth, CMS creates data collection and submission specifications for IRF electronic health record (EHR) software available free of charge to all IRFs and their technology partners, and these will be updated to incorporate the new and modified SDOH assessment items. Finally, CMS provides IRFs with a free internet-based system through which users can access on-demand reports for feedback about the IRFs' compliance with collection and submission of the new and modified SDOH assessment items associated with their facility.
Comment: One commenter urged CMS to recognize that administrative requirements are already overburdening the IRF workforce and incorporating these new standardized patient assessment data elements would further decrease resources from patient care. This commenter reported that it currently takes an average of 45 minutes per patient to pull information and scores and enter them into the IRF-PAI. This commenter noted that the 45 minutes of time does not include the time it takes their staff to complete their assessments that contribute to the IRF-PAI, and completing assessments for patients with cognitive deficits takes even longer.
Response: As the commenter pointed out in their example, the patient must be assessed, and information gathered. We disagree that this policy, if finalized, will take time away from patient care. The new assessment items (Living Situation, Food, and Utilities) are all important pieces of information to developing and administering a comprehensive plan of care in accordance with § 412.606. Rather than taking time away from patient care, providers will be documenting information they are likely already collecting through the course of providing care to the patients.
After the patient assessment is completed, the IRF-PAI is coded with the information and submitted to the CMS system, and it is these steps (after the patient assessment) that the estimated burden and cost captures. As we stated in section IX.A. of this final rule, our assumptions for staff type were based on the categories generally necessary to perform an assessment, and subsequently encode it, which is consistent with past collection of information estimates. [ 112 ] While we acknowledge that some IRFs may train and utilize other personnel, our estimates are based on the categories of personnel necessary to complete the IRF-PAI.
We also note that the commenter's estimate of the time it takes its members to code the IRF-PAI (45 minutes) is consistent with the total time we report in our Paperwork Reduction Act (PRA) package (0938-0842). We estimate the next version of the IRF-PAI will take an average of 1 hour and 47 minutes per IRF-PAI assessment which includes the time to review instructions, search existing data resources, gather the data needed, and complete and review the information collection.
After considering the public comments received, and for the reasons outlined in this section of the final rule and our comment responses, we are finalizing our proposal to remove Item 14-Admission Class from the IRF-PAI with modification. Specifically, while we are finalizing our proposal to remove Item 14-Admission Class from the IRF-PAI effective October 1, 2026 as proposed, IRFs will no longer be required to collect and submit data on this Item 14-Admission Class beginning with patients admitted on October 1, 2024. We are also finalizing our proposal to collect and submit data on the following items adopted as standardized patient assessment data elements under the SDOH category at admission only beginning with October 1, 2026 IRF admissions: (1) Living Situation as described in section VIII.C.3(a) of this final rule; (2) Food as described in section VIII.C.3(b) of this final rule; and (3) Utilities as described in section VIII.C.3(c) of this final rule. We are also finalizing our proposal to collect and submit the modified standardized patient assessment data element, Transportation, at admission only beginning with October 1, 2026, IRF admissions as described in section VIII.C.5 of this final rule.
This final rule updates the IRF prospective payment rates for FY 2025 as required under section 1886(j)(3)(C) of the Act and in accordance with section 1886(j)(5) of the Act, which requires the Secretary to publish in the Federal Register on or before August 1 before each FY, the classification and weighting factors for CMGs used under the IRF PPS for such FY and a description of the methodology and data used in computing the prospective payment rates under the IRF PPS for that FY. This final rule will also implement section 1886(j)(3)(C) of the Act, which requires the Secretary to apply a productivity adjustment to the market basket percentage increase for FY 2012 and subsequent years.
Furthermore, this final rule adopts policy changes to the IRF QRP under the statutory discretion afforded to the Secretary under section 1886(j)(7) of the Act. This rule updates the IRF QRP requirements beginning with the FY 2028 IRF QRP.
We have examined the impacts of this rule as required by Executive Order 12866 on Regulatory Planning and Review (September 30, 1993), Executive Order 13563 on Improving Regulation and Regulatory Review (January 18, 2011), Executive Order 14094 on Modernizing Regulatory Review (April 6, 2023), the Regulatory Flexibility Act (RFA) (September 19, 1980, Pub. L. 96-354), section 1102(b) of the Social Security Act, section 202 of the Unfunded Mandates Reform Act of 1995 (March 22, 1995; Pub. L. 104-4 ), and Executive Order 13132 on Federalism (August 4, 1999) and the Congressional Review Act ( 5 U.S.C. 804(2) ).
Executive Orders 12866 and 13563 direct agencies to assess all costs and benefits of available regulatory alternatives and, if regulation is necessary, to select regulatory approaches that maximize net benefits (including potential economic, environmental, public health and safety effects, distributive impacts, and equity). Executive Order 14094 (Modernizing Regulatory Review) amends section 3(f)(1) of Executive Order 12866 (Regulatory Planning and Review). The amended section 3(f) of Executive Order 12866 defines a “significant regulatory action” as an action that is likely to result in a rule: (1) having an annual effect on the economy of $200 million or more in any 1 year (adjusted every 3 years by the Administrator of OMB's Office of Information and Regulatory Affairs (OIRA) for changes in gross domestic product), or adversely affect in a material way the economy, a sector of the economy, productivity, competition, jobs, the environment, public health or safety, or State, local, territorial, or Tribal governments or communities; (2) creating a serious inconsistency or otherwise interfering with an action taken or planned by another agency; (3) materially altering the budgetary impacts of entitlement grants, user fees, or loan programs or the rights and obligations of recipients thereof; or (4) raise legal or policy issues for which centralized review would meaningfully further the President's priorities or the principles set forth in the Executive order, as specifically authorized in a timely manner by the Administrator of OIRA in each case.
A regulatory impact analysis (RIA) must be prepared for major rules with significant regulatory action/s and/or with significant effects as per section 3(f)(1) ($200 million or more in any 1 year). We estimate the total impact of the policy updates described in this final rule by comparing the estimated payments in FY 2025 with those in FY 2024. This analysis results in an estimated $280 million increase for FY 2025 IRF PPS payments. Additionally, we estimated that costs associated with updating the reporting requirements under the IRF QRP result in an estimated $392,113.40 additional cost for IRFs in FY 2026 for purposes of meeting the FY 2028 IRF QRP. Based on our estimates, OMB's Office of Information and Regulatory Affairs has determined this rulemaking is significant per section 3(f)(1) as measured by the $200 million or more in any 1 year, and hence also a major rule under Subtitle E of the Small Business Regulatory Enforcement Fairness Act of 1996 (also known as the Congressional Review Act). Accordingly, we have prepared an RIA that, to the best of our ability, presents the costs and benefits of the rulemaking.
The RFA requires agencies to analyze options for regulatory relief of small entities, if a rule has a significant impact on a substantial number of small entities. For purposes of the RFA, small entities include small businesses, nonprofit organizations, and small governmental jurisdictions. Most IRFs and most other providers and suppliers are small entities, either by having revenues of $9.0 million to $47.0 million or less in any 1 year depending on industry classification, or by being nonprofit organizations that are not dominant in their markets. (For details, see the Small Business Administration's final rule that set forth size standards for health care industries, at 65 FR 69432 at https://www.sba.gov/sites/default/files/2019-08/SBA%20Table%20of%20Size%20Standards_Effective%20Aug%2019%2C%202019_Rev.pdf , effective January 1, 2017, and updated on August 19, 2019.) Because we lack data on individual hospital receipts, we cannot determine the number of small proprietary IRFs or the proportion of IRFs' revenue that is derived from Medicare payments. Therefore, we assume that all IRFs (an approximate total of 1,160 IRFs, of which approximately 50 percent are nonprofit facilities) are considered small entities and that Medicare payment constitutes the majority of their revenues. HHS generally uses a revenue impact of 3 to 5 percent as a significance threshold under the RFA. As shown in Table 17, we estimate that the net revenue impact of the final rule on all IRFs is to increase estimated payments by approximately 2.8 percent. The rates and policies proposed in this rule would not have a significant impact (not greater than 5 percent) on a substantial number of small entities. The estimated impact on small entities is shown in Table 17. MACs are not considered to be small entities. Individuals and States are not included in the definition of a small entity.
In addition, section 1102(b) of the Act requires us to prepare an RIA if a rule may have a significant impact on the operations of a substantial number of small rural hospitals. This analysis must conform to the provisions of section 604 of the RFA. For purposes of section 1102(b) of the Act, we define a small rural hospital as a hospital that is located outside of a Metropolitan Statistical Area and has fewer than 100 beds. As shown in Table 17, we estimate that the net revenue impact of this final rule on rural IRFs is to increase estimated payments by approximately 4.9 percent based on the data of the 131 rural units and 13 rural hospitals in our database of 1,160 IRFs for which data were available. We estimate an overall impact for rural IRFs in all areas between 1.4 percent and 10.7 percent. As a result, we anticipate that this final rule will not have a significant negative impact on a substantial number of small entities.
Section 202 of the Unfunded Mandates Reform Act of 1995 ( Pub. L. 104-04 , enacted March 22, 1995) (UMRA) also requires that agencies assess anticipated costs and benefits before issuing any rule whose mandates require spending in any 1 year of $100 million in 1995 dollars, updated annually for inflation. In 2024, that threshold is approximately $183 million. This final rule does not mandate any requirements for State, local, or Tribal governments, or for the private sector.
Executive Order 13132 establishes certain requirements that an agency must meet when it issues a proposed rule (and subsequent final rule) that imposes substantial direct requirement costs on State and local governments, preempts State law, or otherwise has federalism implications. As stated, this final rule will not have a substantial effect on State and local governments, preempt State law, or otherwise have a federalism implication.
This final rule updates the IRF PPS rates contained in the FY 2024 IRF PPS final rule ( 88 FR 50956 ). Specifically, this final rule updates the CMG relative weights and ALOS values, the wage index, and the outlier threshold for high-cost cases. This final rule will apply a productivity adjustment to the FY 2025 IRF market basket percentage increase in accordance with section 1886(j)(3)(C)(ii)(I) of the Act.
We estimate that the impact of the changes and updates described in this final rule will be a net estimated increase of $280 million in payments to IRFs. The impact analysis in Table 17 of this final rule represents the projected effects of the updates to IRF PPS payments for FY 2025 compared with the estimated IRF PPS payments in FY 2024. We determined the effects by estimating payments while holding all other payment variables constant. We use the best data available, but we do not attempt to predict behavioral responses to these changes, and we do not make adjustments for future changes in such variables as number of discharges or case-mix.
We note that certain events may combine to limit the scope or accuracy of our impact analysis, because such an analysis is future-oriented and, thus, susceptible to forecasting errors because of other changes in the forecasted impact time period. Some examples could be legislative changes made by the Congress to the Medicare program that would impact program funding, or changes specifically related to IRFs. Although some of these changes may not necessarily be specific to the IRF PPS, the nature of the Medicare program is such that the changes may interact, and the complexity of the interaction of these changes could make it difficult to predict accurately the full scope of the impact upon IRFs.
In updating the rates for FY 2025, we are implementing the standard annual revisions described in this final rule (for example, the update to the wage index and market basket percentage increase used to adjust the Federal rates). We are also reducing the FY 2025 IRF market basket percentage increase by a productivity adjustment in accordance with section 1886(j)(3)(C)(ii)(I) of the Act. We estimate the total increase in payments to IRFs in FY 2025, relative to FY 2024, will be approximately $280 million.
This estimate is derived from the application of the FY 2025 IRF market basket percentage increase, reduced by a productivity adjustment in accordance with section 1886(j)(3)(C)(ii)(I) of the Act, which yields an estimated increase in aggregate payments to IRFs of $300 million. However, there is an estimated $20 million decrease in aggregate payments to IRFs due to the update to the outlier threshold amount. Therefore, we estimate that these updates will result in a net increase in estimated payments of $280 million from FY 2024 to FY 2025.
The effects of the updates that impact IRF PPS payment rates are shown in Table 17. The following updates that affect the IRF PPS payment rates are discussed separately below:
- The effects of the update to the outlier threshold amount, from approximately 3.2 percent to 3.0 percent of total estimated payments for FY 2025, consistent with section 1886(j)(4) of the Act.
- The effects of the annual market basket update (using the 2021-based IRF market basket) to IRF PPS payment rates, as required by sections 1886(j)(3)(A)(i) and (j)(3)(C) of the Act, including a productivity adjustment in accordance with section 1886(j)(3)(C)(ii)(I) of the Act.
- The effects of applying the budget-neutral labor-related share and wage index adjustment, as required under section 1886(j)(6) of the Act, accounting for the permanent cap on wage index decreases when applicable.
- The effects of the budget-neutral changes to the CMG relative weights and ALOS values under the authority of section 1886(j)(2)(C)(i) of the Act.
- The total change in estimated payments based on the FY 2025 payment changes relative to the estimated FY 2024 payments.
Table 17 shows the overall impact on the 1,160 IRFs included in the analysis.
The next 12 rows of Table 17 contain IRFs categorized according to their geographic location, designation as either a freestanding hospital or a unit of a hospital, and by type of ownership; all urban, which is further divided into urban units of a hospital, urban freestanding hospitals, and by type of ownership; and all rural, which is further divided into rural units of a hospital, rural freestanding hospitals, and by type of ownership. There are 1,016 IRFs located in urban areas included in our analysis. Among these, there are 653 IRF units of hospitals located in urban areas and 363 freestanding IRF hospitals located in urban areas. There are 144 IRFs located in rural areas included in our analysis. Among these, there are 131 IRF units of hospitals located in rural areas and 13 freestanding IRF hospitals located in rural areas. There are 498 for-profit IRFs. Among these, there are 463 IRFs in urban areas and 35 IRFs in rural areas. There are 567 non-profit IRFs. Among these, there are 477 urban IRFs and 90 rural IRFs. There are 95 government-owned IRFs. Among these, there are 76 urban IRFs and 19 rural IRFs.
The remaining five parts of Table 17 show IRFs grouped by their urban or rural status before and after the application of the new CBSA delineations, by geographic location within a region, by teaching status, and by DSH patient percentage (PP). First, IRFs are categorized by their urban or rural designation before and after the updates to the OMB CBSA delineations. Second, IRFs located in urban areas are categorized for their location within a particular one of the nine Census geographic regions. Third, IRFs located in rural areas are categorized for their location within a particular one of the nine Census geographic regions. In some cases, especially for rural IRFs located in the New England, Mountain, and Pacific regions, the number of IRFs represented is small. IRFs are then grouped by teaching status, including non-teaching IRFs, IRFs with an intern and resident to average daily census (ADC) ratio less than 10 percent, IRFs with an intern and resident to ADC ratio greater than or equal to 10 percent and less than or equal to 19 percent, and IRFs with an intern and resident to ADC ratio greater than 19 percent. Finally, IRFs are grouped by DSH PP, including IRFs with zero DSH PP, IRFs with a DSH PP less than 5 percent, IRFs with a DSH PP between 5 and less than 10 percent, IRFs with a DSH PP between 10 and 20 percent, and IRFs with a DSH PP greater than 20 percent.
The estimated impacts of each policy described in this final rule to the facility categories listed are shown in the columns of Table 17. The description of each column is as follows:
- Column (1) shows the facility classification categories.
- Column (2) shows the number of IRFs in each category in our FY 2025 analysis file.
- Column (3) shows the number of cases in each category in our FY 2025 analysis file.
- Column (4) shows the estimated effect of the adjustment to the outlier threshold amount.
- Column (5a) shows the estimated effect of the FY 2025 update to the IRF labor-related share, FY 2024 CBSA delineations, and FY 2025 wage index with the 5-percent cap, in a budget-neutral manner.
- Column (5b) shows the estimated effect of the FY 2025 update to the IRF labor-related share, FY2025 CBSA delineations and FY 2025 wage index with the 5-percent cap, in a budget-neutral manner. These updates are made without applying the rural adjustment to IRFs transitioning from urban to rural status under the new CBSA delineations or reducing the rural adjustment or IRFs transitioning from rural to urban status.
- Column (5c) shows the estimated effects of the 3-year phase-out of the rural adjustment for IRFs transitioning from rural to urban status under the new CBSA delineations and the application of the standard rural adjustment for IRFs transitioning to rural status.
- Column (6) shows the estimated effect of the update to the CMG relative weights and ALOS values, in a budget-neutral manner.
- Column (7) compares our estimates of the payments per discharge, incorporating all of the policies reflected in this final rule for FY 2025 to our estimates of payments per discharge in FY 2024.
The average estimated increase for all IRFs is approximately 2.8 percent. This estimated net increase includes the effects of the IRF market basket update for FY 2025 of 3.0 percent, which is based on a IRF market basket percentage increase of 3.5 percent, less a 0.5 percentage point productivity adjustment, as required by section 1886(j)(3)(C)(ii)(I) of the Act. It also includes the approximate 0.2 percent overall decrease in estimated IRF outlier payments from the update to the outlier threshold amount. Since we are updating the IRF wage index, labor-related share and the CMG relative weights in a budget-neutral manner, we estimate there is no expected impact to total estimated IRF payments in aggregate. However, as described in more detail in each section, we estimate there will be expected impacts to the estimated distribution of payments among providers.

The estimated effects of the update to the outlier threshold adjustment are presented in column 4 of Table 17.
For the FY 2025 proposed rule, we used preliminary FY 2023 IRF claims data and based on that preliminary analysis, we estimated that IRF outlier payments as a percentage of total estimated IRF payments would be 3.2 percent in FY 2024. As we typically do between the proposed and final rules each year, we updated our FY 2023 IRF claims data to ensure that we are using the most recent available data in setting IRF payments. Therefore, based on an updated analysis of the most recent IRF claims data for this final rule, we estimate that IRF outlier payments as a percentage of total estimated IRF payments are 3.2 percent in FY 2024. Thus, we are adjusting the outlier threshold amount in this final rule to maintain total estimated outlier payments equal to 3 percent of total estimated payments in FY 2025.
The estimated change in total IRF payments for FY 2025, therefore, includes an approximate 0.2 percentage point decrease in payments because the estimated outlier portion of total payments is estimated to decrease from approximately 3.2 percent to 3.0 percent.
The impact of this update to the outlier threshold amount (as shown in column 4 of Table 17) is to decrease estimated overall payments to IRFs by 0.2 percentage point.
In column 5a of Table 17, we present the effects of the budget-neutral update of the wage index and labor-related share, taking into account the permanent 5-percent cap on wage index decreases when applicable, without taking into account the updated FY2025 CBSA delineations, which are presented separately in the next column. The changes to the wage index and the labor-related share are discussed together because the wage index is applied to the labor-related share portion of payments, so the changes in the two have a combined effect on payments to providers. As discussed in section VI.E. of this final rule, we are updating the FY 2025 labor-related share from 74.1 percent in FY 2024 to 74.4 percent in FY 2025.
In column 5b of Table 17, we present the effects of the revised FY2025 CBSA delineations, without applying the rural adjustment to IRFs transitioning from urban to rural status under the new CBSA delineations or reducing the rural adjustment for IRFs transitioning from rural to urban status. In aggregate, we do not estimate that these updates will affect overall estimated payments to IRFs. However, we do expect these updates to have small distributional effects. We estimate the largest decrease in payment from the update to the FY 2025 CBSA delineation and wage index and labor-related share (column 5b of Table 17) to be a 0.5 percent decrease for IRFs in the Rural Middle Atlantic region and the largest increase in payment to be a 1.4 percent increase for IRFs in the Rural South Atlantic region.
In column 5c of Table 17, we present the effects of the 3-year phase-out of the rural adjustment for IRFs transitioning from rural to urban status under the new CBSA delineations and the application of the standard rural adjustment for IRFs transitioning to rural status. Under the IRF PPS, IRFs located in rural areas receive a 14.9 percent adjustment to their payment rates to account for the higher costs incurred in treating beneficiaries in rural areas. Under the new CBSA delineations, we estimate that 8 IRFs will transition from rural to urban status for purposes of the IRF PPS wage index adjustment in FY 2025. Without the phase-out of the rural adjustment, these 8 IRFs would experience an automatic 14.9 percent decrease in payments as a result of this change from rural to urban status in FY 2025.
To mitigate the effects of this relatively large decrease in payments, we will phase-out the rural adjustment for these providers over a 3-year period, as discussed in more detail in section VI.D.3 of this final rule. Thus, these IRFs would receive two thirds of the rural adjustment in FY 2025, one third of the rural adjustment in FY 2026, and none of the rural adjustment in FY 2027, thus giving these IRFs time to adjust to the reduced payments.
Column 5c shows the effect on providers of this budget-neutral phase-out of the rural adjustment for IRFs transitioning from rural to urban status in FY 2025. Under this policy, these providers would only experience a reduction in payments of one third of the 14.9 percent rural adjustment in FY 2025. While this does not impact aggregate payments, there are small effects on the distribution of payments to IRFs. The largest decrease as a result of this policy change is a 4.1 percent decrease in payments to IRFs that transitioned from rural to urban status since they will receive only two thirds of the rural adjustment in FY 2025. We note that the decrease in payments to these providers is substantially lessened from what it otherwise would have been as a result of the phase-out of the rural adjustment for these IRFs.
In column 6 of Table 17, we present the effects of the budget-neutral update of the CMG relative weights and ALOS values. In the aggregate, we do not estimate that these updates will affect overall estimated payments of IRFs. However, we do expect these updates to have small distributional effects between −0.1 to 0.2.
In accordance with section 1886(j)(7)(A) of the Act, the Secretary must reduce by 2 percentage points the annual market basket increase factor otherwise applicable to an IRF for a fiscal year if the IRF does not comply with the requirements of the IRF QRP for that fiscal year. In section IX.A. of the final rule, we discussed the method for applying the 2-percentage points reduction to IRFs that fail to meet the IRF QRP requirements.
As discussed in sections VIII.C.3. and VIII.C.5. of this final rule, we are finalizing our proposal to collect four new items as standardized patient assessment data elements under the SDOH category and modify one item collected as a standardized patient assessment data element under the SDOH category on the IRF-PAI beginning with the FY 2028 IRF QRP. Although the increase in burden will be accounted for in a revised information collection request under OMB control number (0938-0842), we are providing impact information. We believe the items would be completed equally by a Registered Nurse (RN) (50 percent of the time) and a Licensed Practical and Vocational Nurses (LPN/LVN) (50 percent of the time). For the purposes of calculating the costs associated with the collection of information requirements, we obtained median hourly wages for these staff from the U.S. Bureau of Labor Statistics' (BLS) May 2022 National Occupational Employment and Wage Estimates. [ 113 ] To account for other indirect costs and fringe benefits, we doubled the hourly wage. These amounts are detailed in Table 18.
| Occupation title | Occupation code | Median hourly wage ($/hr) | Other indirect costs and fringe benefit ($/hr) | Adjusted hourly wage ($/hr) |
|---|---|---|---|---|
| Registered Nurse (RN) | 29-1141 | $39.05 | $39.05 | $78.10 |
| Licensed Practical and Licensed Vocational Nurse (LPN/LVN) | 29-2061 | 26.26 | 26.26 | 52.52 |
With 571,151 admissions from 1,160 IRFs annually, we estimated an annual burden increase of 8,859.64 hours [(571,151 × 0.02 hour) admissions—(512,677 × 0.005 hour) planned discharges] and an increase of $578,622.76 [8,859.64 hours × $65.31/hr)]. For each IRF, we estimate an annual burden increase of 7.64 hours (8,859.64 hours/1,160 IRFs) for an annual increase of $498.81 ($578,622.76/1,160 IRFs).
As discussed in section VII.F.3. of this final rule, we are finalizing our proposal to remove Item 14, Admission Class, from the IRF-PAI with modification. Specifically, while we are finalizing our proposal to remove Item 14—Admission Class from the IRF-PAI effective October 1, 2026 as proposed, IRFs will no longer be required to collect and submit data on this Item 14—Admission Class beginning with patients admitted on October 1, 2024. We estimate the removal of this item would result in a decrease of 0.005 hour of clinical staff time beginning with admission assessments completed on October 1, 2026. Although the decrease in burden will be accounted for in a revised information collection request under OMB control number 0938-0842, we are providing impact information. We estimate this item is completed equally by an RN (50 percent of the time) and by an LPN/LVN (50 percent of the time). For the purposes of calculating the costs associated with the collection of information requirements, we obtained median hourly wages for these staff from the U.S. Bureau of Labor Statistics' (BLS) May 2022 National Occupational Employment and Wage Estimates. [ 114 ] To account for other indirect costs and fringe benefits, we doubled the hourly wage. These amounts are detailed in Table 18. With 571,151 admissions from 1,160 IRFs annually, we estimate an annual burden decrease of 2,855.76 hours (571,151 admissions × 0.005 hour) and a decrease of $186,509.36 [2,855.76 hours × $65.31/hr)]. For each IRF we estimate an annual burden decrease of 2.46 hours (2,855.76 hours/1,160 IRFs) for an annual decrease of $160.78 ($186,509.36/1,160 IRFs).
In summary, under OMB control number 0938-0842, the changes we are finalizing to the IRF QRP would result in an estimated increase in programmatic burden for 1,160 IRFs. The total burden increase is approximately $392,113.40 for all IRFs and $338.03 per IRF and is summarized in Table 19.
| Requirement | Per IRF | All IRFs | ||
|---|---|---|---|---|
| Estimated change in annual burden hours | Estimated change in annual cost | Estimated change in annual burden hours | Estimated change in annual cost | |
| Collection of Four New Items as Standardized Patient Assessment Data Elements and Modification of One Item Collected as a Standardized Patient Assessment Data Element beginning with the FY 2028 IRF QRP | +7.64 | +$498.81 | +8,859.64 | +$578,622.76 |
| Removal of the Admission Class item effective October 1, 2026 | −2.46 | −160.78 | −2,855.76 | −186,509.36 |
| Increase in burden for the IRF QRP | 5.18 | 338.03 | 6,003.88 | 392,113.40 |
We invited public comments on the overall impact of the IRF QRP proposals for FY 2028. We received several comments on the impact of the IRF QRP proposals and responded to those comments in sections VIII.C.4, VIII.F.2, and IX.A of this final rule.
The following is a discussion of the alternatives considered for the IRF PPS updates contained in the final rule.
As noted previously, section 1886(j)(3)(C) of the Act requires the Secretary to update the IRF PPS payment rates by an increase factor that reflects changes over time in the prices of an appropriate mix of goods and services included in the covered IRF services and section 1886(j)(3)(C)(ii)(I) of the Act requires the Secretary to apply a productivity adjustment to the market basket percentage increase for FY 2025. Thus, in accordance with section 1886(j)(3)(C) of the Act, we updated the IRF prospective payments in this final rule by 3.0 percent (which equals the 3.5 percent IRF market basket percentage increase for FY 2025 reduced by a 0.5 percentage point productivity adjustment as determined under section 1886(b)(3)(B)(xi)(II) of the Act (as required by section 1886(j)(3)(C)(ii)(I) of the Act).
We considered maintaining the existing CMG relative weights and average length of stay values for FY 2025. However, in light of recently available data and our desire to ensure that the CMG relative weights and average length of stay values are as reflective as possible of recent changes in IRF utilization and case mix, we believe that it is appropriate to update the CMG relative weights and average length of stay values at this time to ensure that IRF PPS payments continue to reflect as accurately as possible the current costs of care in IRFs.
We considered maintaining the existing outlier threshold amount for FY 2025. However, analysis of updated FY 2024 data indicates that estimated outlier payments would be more than 3 percent of total estimated payments for FY 2025, unless we updated the outlier threshold amount. Consequently, we are adjusting the outlier threshold amount to maintain estimated outlier payments at 3 percent of estimated aggregate payments in FY 2025.
With regard to the proposal to collect and submit four new items as standardized patient assessment data elements under the SDOH category and modify one item collected and submitted as a standardized patient assessment data element under the SDOH category beginning with the FY 2028 IRF QRP, we believe these proposals would advance the CMS National Quality Strategy Goals of equity and engagement. We considered the alternative of delaying the proposal to collect and submit these assessment items but given the fact they would encourage meaningful collaboration among healthcare providers, caregivers, and community-based organizations to address SDOH prior to discharge from the IRF, we believe further delay is unwarranted.
With regard to the proposal to remove one item, Item 14-Admission Class, from the IRF-PAI, we routinely review the IRF-PAI for redundancies and opportunities to simplify data submission requirements. We have identified that this item is currently not used in the calculation of quality measures already adopted in the IRF QRP, payment, survey, or care planning, and therefore no alternatives were considered.
If regulations impose administrative costs on private entities, such as the time needed to read and interpret this final rule, we should estimate the cost associated with regulatory review. Due to the uncertainty involved with accurately quantifying the number of entities that will review the rule, we assume that the total number of unique commenters on the FY 2025 IRF PPS proposed rule will be the number of reviewers of this year's final rule. We acknowledge that this assumption may understate or overstate the costs of reviewing this final rule. It is possible that not all commenters reviewed the FY 2025 IRF PPS proposed rule in detail, and it is also possible that some reviewers chose not to comment on the FY 2025 proposed rule. For these reasons, we believe that the number of commenters would be a fair estimate of the number of reviewers of this final rule.
We also recognize that different types of entities are in many cases affected by mutually exclusive sections of this final rule, and therefore, for the purposes of our estimate we assume that each reviewer reads approximately 50 percent of the rule.
Using the national mean hourly wage data from the May 2023 BLS for Occupational Employment Statistics (OES) for medical and health service managers (SOC 11-9111), we estimate that the cost of reviewing this rule is $129.28 per hour, including other indirect costs and fringe benefits ( https://www.bls.gov/oes/current/oes_nat.htm ). Assuming an average reading speed, we estimate that it will take approximately 3 hours for the staff to review half of this final rule. For each reviewer of the rule, the estimated cost is $387.84 (3 hours × $129.28). Therefore, we estimate that the total cost of reviewing this regulation is $17,064.96 ($387.84 × 44 reviewers).
As required by OMB Circular A-4 (available at https://www.whitehouse.gov/wp-content/uploads/2023/11/CircularA-4.pdf ), in Table 20 we have prepared an accounting statement showing the classification of the expenditures associated with the provisions of this final rule. Table 20 provides our best estimate of the increase in Medicare payments under the IRF PPS as a result of the updates presented in this final rule based on the data for 1,160 IRFs in our database.
| Category | Transfers | |
|---|---|---|
| Change in Estimated Transfers from FY 2024 IRF PPS to FY 2025 IRF PPS | Annualized Monetized Transfers From Whom to Whom? | $280 million. Federal Government to IRF Medicare Providers. |
| Estimated Costs Associated with the FY 2028 IRF QRP | Annualized monetized cost in FY 2028 due to proposed data collection requirements | $392,113.40. |
| Estimated Costs Associated with Review Cost for FY 2025 IRF PPS | Cost associated with regulatory review cost | 17,064.96. |
Overall, the estimated payments per discharge for IRFs in FY 2025 are projected to increase by 2.8 percent, compared with the estimated payments in FY 2024, as reflected in column 7 of Table 17.
IRF payments per discharge are estimated to increase by 2.7 percent in urban areas and 4.9 percent in rural areas, compared with estimated FY 2024 payments. Payments per discharge to rehabilitation units are estimated to increase 2.1 percent in urban areas and 4.8 percent in rural areas. Payments per discharge to freestanding rehabilitation hospitals are estimated to increase 3.0 percent in urban areas and 5.2 percent in rural areas.
Overall, IRFs are estimated to experience a net increase in payments as a result of the policies in this final rule. The largest payment increase is estimated to be a 21.4 percent increase for IRFs transitioning to rural status under the new CBSA delineations, followed by a 10.7 percent increase for IRFs located in the Rural Middle Atlantic region. The analysis above, together with the remainder of this preamble, provides an RIA.
In accordance with the provisions of Executive Order 12866 , this regulation was reviewed by OMB.
Chiquita Brooks-LaSure, Administrator of the Centers for Medicare & Medicaid Services, approved this document on July 25, 2024.
Xavier Becerra,
Secretary, Department of Health and Human Services.
1. CMS, “COVID-19 Emergency Declaration Blanket Waivers for Health Care Providers,” (updated Feb. 19, 2021) (available at https://www.cms.gov/files/document/summary-covid-19-emergency-declaration-waivers.pdf ).
2. CMS, “COVID-19 Frequently Asked Questions (FAQs) on Medicare Fee-for-Service (FFS) Billing,” (updated March 5, 2021) (available at https://www.cms.gov/files/document/03092020-covid-19-faqs-508.pdf ).
3. https://www.medpac.gov/wp-content/uploads/2025/03/Mar25_MedPAC_ReportToCongress_SEC.pdf .
4. https://www.federalregister.gov/citation/70-FR-47923 .
5. https://www.federalregister.gov/citation/70-FR-47927 .
6. https://www.federalregister.gov/citation/70-FR-47880 .
7. Items may also be referred to as “data elements.”
8. As noted in section VII.C of the proposed rule and section VIII.C of this final rule, hospitals are required to report whether they have screened patients for five standardized SDOH categories: housing instability, food insecurity, utility difficulties, transportation needs, and interpersonal safety.
9. Office of the Assistant Secretary for Planning and Evaluation (ASPE). Second Report to Congress on Social Risk and Medicare's Value-Based Purchasing Programs. June 28, 2020. Available at: https://aspe.hhs.gov/reports/second-report-congress-social-risk-medicares-value-based-purchasing-programs .
10. World Health Organization. Social determinants of health. Available at: https://www.who.int/health-topics/social-determinants-of-health#tab=tab_1 .
11. Using Z Codes: The Social Determinants of Health (SDOH). Data Journey to Better Outcomes. https://www.cms.gov/files/document/zcodes-infographic.pdf .
12. Improving the Collection of Social Determinants of Health (SDOH) Data with ICD-10-CM Z Codes. https://www.cms.gov/files/document/cms-2023-omh-z-code-resource.pdf .
13. CMS.gov. Measures Management System (MMS). CMS Focus on Health Equity. Health Equity Terminology and Quality Measures. https://mmshub.cms.gov/about-quality/quality-at-CMS/goals/cms-focus-on-health-equity/health-equity-terminology .
14. Centers for Disease Control and Prevention. Social Determinants of Health (SDOH) and PLACES Data. https://www.cdc.gov/places/social-determinants-of-health-and-places-data/ .
15. “U.S. Playbook To Address Social Determinants Of Health” from the White House Office Of Science And Technology Policy (November 2023).
16. These SDOH data are also collected for purposes outlined in section 2(d)(2)(B) of the Improving Medicare Post-Acute Care Transitions Act (IMPACT Act). For a detailed discussion on SDOH data collection under section 2(d)(2)(B) of the IMPACT Act, see the FY 2020 IRF PPS final rule ( 84 FR 39149 through 39161 ).
17. Social Determinants of Health. Healthy People 2020. https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-of-health . (February 2019).
18. National Academies of Sciences, Engineering, and Medicine. 2020. Leading Health Indicators 2030: Advancing Health, Equity, and Well-Being. Washington, DC: The National Academies Press. https://doi.org/10.17226/25682 .
19. Centers for Medicare & Medicaid Services. “A Guide to Using the Accountable Health Communities Health-Related Social Needs Screening Tool: Promising Practices and Key Insights.” August 2022. Available at: https://www.cms.gov/priorities/innovation/media/document/ahcm-screeningtool-companion .
20. Berkowitz, S.A., T.P. Baggett, and S.T. Edwards, “Addressing Health-Related Social Needs: Value-Based Care or Values-Based Care?” Journal of General Internal Medicine, vol. 34, no. 9, 2019, pp. 1916-1918, https://doi.org/10.1007/s11606-019-05087-3 .
21. Hugh Alderwick and Laura M. Gottlieb, “Meanings and Misunderstandings: A Social Determinants of Health Lexicon for Health Care Systems: Milbank Quarterly,” Milbank Memorial Fund, November 18, 2019, https://www.milbank.org/quarterly/articles/meanings-and-misunderstandings-a-social-determinants-of-health-lexicon-for-health-care-systems/ .
22. American Hospital Association. (2020). Health Equity, Diversity & Inclusion Measures for Hospitals and Health System Dashboards. December 2020. Accessed: January 18, 2022. Available at: https://ifdhe.aha.org/system/files/media/file/2020/12/ifdhe_inclusion_dashboard.pdf .
23. In October 2023, we released two new annual Health Equity Confidential Feedback Reports to IRFs: The Discharge to Community (DTC) Health Equity Confidential Feedback Report and the Medicare Spending Per Beneficiary (MSPB) Health Equity Confidential Feedback Report. The PAC Health Equity Confidential Feedback Reports stratified the DTC and MSPB measures by dual-enrollment status and race/ethnicity. For more information on the Health Equity Confidential Feedback Reports, please refer to the Education and Outreach materials available on the IRF QRP Training web page at https://www.cms.gov/medicare/quality-initiatives-patient-assessment-instruments/irf-quality-reporting/irf-quality-reporting-training .
24. Brooks-LaSure, C. (2021). My First 100 Days and Where We Go from Here: A Strategic Vision for CMS. Centers for Medicare & Medicaid. Available at: https://www.cms.gov/blog/my-first-100-days-and-where-we-go-here-strategic-vision-cms .
25. The Biden-Harris Administration's strategic approach to addressing health related social needs can be found in The U.S. Playbook to Address Social Determinants of Health (SDOH) (2023): https://www.whitehouse.gov/wp-content/uploads/2023/11/SDOH-Playbook-3.pdf .
26. The AHC Model was a five-year demonstration project run by the Centers for Medicare & Medicaid Innovation between May 1, 2017 and April 30, 2023. For more information go to https://www.cms.gov/priorities/innovation/innovation-models/ahcm .
27. More information about the AHC HRSN Screening Tool is available on the website at https://innovation.cms.gov/Files/worksheets/ahcm-screeningtool.pdf .
28. Centers for Medicare & Medicaid Services, FY2023 IPPS/LTCH PPS final rule ( 87 FR 49191 through 49194).
29. Centers for Medicare & Medicaid Services, FY2024 Inpatient Psychiatric Prospective Payment System—Rate Update ( 88 FR 51107 through 51121 ).
30. https://health.gov/healthypeople/priority-areas/social-determinants-health .
31. Healthy People 2030 is a long-term, evidence-based effort led by the U.S. Department of Health and Human Services (HHS) that aims to identify nationwide health improvement priorities and improve the health of all Americans.
32. Kushel, M.B., Gupta, R., Gee, L., & Haas, J.S. (2006). Housing instability and food insecurity as barriers to health care among low-income Americans. Journal of General Internal Medicine, 21 (1), 71-77. doi: https://doi.org/10.1111/j.1525-1497.2005.00278.x .
33. Homelessness is defined as “lacking a regular nighttime residence or having a primary nighttime residence that is a temporary shelter or other place not designed for sleeping.” Crowley, S. (2003). The affordable housing crisis: Residential mobility of poor families and school mobility of poor children. Journal of Negro Education, 72 (1), 22-38. doi: https://doi.org/10.2307/3211288 .
34. The 2023 Annual Homeless Assessment Report (AHAR) to Congress. The U.S. Department of Housing and Urban Development 2023. https://www.huduser.gov/portal/sites/default/files/pdf/2023-AHAR-Part-1.pdf .
35. Baggett, T.P., Hwang, S.W., O'Connell, J.J., Porneala, B.C., Stringfellow, E.J., Orav, E.J., Singer, D.E., & Rigotti, N.A. (2013). Mortality among homeless adults in Boston: Shifts in causes of death over a 15-year period. JAMA Internal Medicine, 173(3), 189-195. doi: https://doi.org/10.1001/jamainternmed.2013.1604 . Schanzer, B., Dominguez, B., Shrout, P.E., & Caton, C.L. (2007). Homelessness, health status, and health care use. American Journal of Public Health, 97(3), 464-469. doi: https://doi.org/10.2105/ajph.2005.076190 .
36. U.S. Department of Health & Human Services (HHS), Call to Action, “Addressing Health Related Social Needs in Communities Across the Nation.” November 2023. https://aspe.hhs.gov/sites/default/files/documents/3e2f6140d0087435cc6832bf8cf32618/hhs-call-to-action-health-related-social-needs.pdf .
37. Henderson, K.A., Manian, N., Rog, D.J., Robison, E., Jorge, E., AlAbdulmunem, M. “Addressing Homelessness Among Older Adults” (Final Report). Washington, DC: Office of the Assistant Secretary for Planning and Evaluation, U.S. Department of Health and Human Services. October 26, 2023.
38. More information about the AHC HRSN Screening Tool is available on the website at https://innovation.cms.gov/Files/worksheets/ahcm-screeningtool.pdf .
39. The AHC HRSN Screening Tool Living Situation item includes two questions. In an effort to limit IRF burden, we are only proposing the first question.
40. National Association of Community Health Centers and Partners, National Association of Community Health Centers, Association of Asian Pacific Community Health Organizations, Association OPC, Institute for Alternative Futures. “PRAPARE.” 2017. https://prapare.org/the-prapare-screening-tool/ .
41. U.S. Department of Agriculture, Economic Research Service. (n.d.). Definitions of food security. Retrieved March 10, 2022, from https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-u-s/definitions-of-food-security/ .
42. Hernandez, D.C., Reesor, L.M., & Murillo, R. (2017). Food insecurity and adult overweight/obesity: Gender and race/ethnic disparities. Appetite, 117, 373-378.
43. Banerjee, S., Radak, T., Khubchandani, J., & Dunn, P. (2021). Food Insecurity and Mortality in American Adults: Results From the NHANES-Linked Mortality Study. Health promotion practice, 22(2), 204-214. https://doi.org/10.1177/1524839920945927 .
44. National Center for Health Statistics. (2022, September 6). Exercise or Physical Activity. Retrieved from Centers for Disease Control and Prevention: https://www.cdc.gov/nchs/fastats/exercise.htm .
45. Ziliak, J.P., & Gundersen, C. (2019). The State of Senior Hunger in America 2017: An Annual Report. Prepared for Feeding America. Available at https://www.feedingamerica.org/research/senior-hunger-research/senior .
46. Ziliak, J.P., & Gundersen, C. (2019). The State of Senior Hunger in America 2017: An Annual Report. Prepared for Feeding America. Available at: https://www.feedingamerica.org/research/senior-hunger-research/senior .
47. The Malnutrition Quality Collaborative. (2020). National Blueprint: Achieving Quality Malnutrition Care for Older Adults, 2020 Update. Washington, DC: Avalere Health and Defeat Malnutrition Today. Available at: https://defeatmalnutrition.today/advocacy/blueprint/ .
48. Food Research & Action Center (FRAC). “Hunger is a Health Issue for Older Adults: Food Security, Health, and the Federal Nutrition Programs.” December 2019. https://frac.org/wp-content/uploads/hunger-is-a-health-issue-for-older-adults-1.pdf .
49. The White House Challenge to End Hunger and Build Health Communities (Challenge) was a nationwide call-to-action released on March 24, 2023, to stakeholders across all of society to make commitments to advance President Biden's goal to end hunger and reduce diet-related diseases by 2030—all while reducing disparities. More information on the White House Challenge to End Hunger and Build Health Communities can be found: https://www.whitehouse.gov/briefing-room/statements-releases/2023/03/24/fact-sheet-biden-harris-administration-launches-the-white-house-challenge-to-end-hunger-and-build-healthy-communities-announces-new-public-private-sector-actions-to-continue-momentum-from-hist/ .
50. Schroeder K, Smaldone A. Food Insecurity: A Concept Analysis. Nurse Forum. 2015 Oct-Dec;50(4):274-84. doi: 10.1111/nuf.12118. Epub 2015 Jan 21. PMID: 25612146; PMCID: PMC4510041.
51. Tsega M, Lewis C, McCarthy D, Shah T, Coutts K. Review of Evidence for Health-Related Social Needs Interventions. July 2019. The Commonwealth Fund. https://www.commonwealthfund.org/sites/default/files/2019-07/COMBINED_ROI_EVIDENCE_REVIEW_7.15.19.pdf .
52. More information about the HFSS tool can be found at https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-u-s/survey-tools/ .
53. Hernández D. Understanding `energy insecurity' and why it matters to health. Soc Sci Med. 2016 Oct; 167:1-10. Doi: 10.1016/j.socscimed.2016.08.029. Epub 2016 Aug 21. PMID: 27592003; PMCID: PMC5114037.
54. US Energy Information Administration. “One in Three U.S. Households Faced Challenges in Paying Energy Bills in 2015.” 2017 Oct 13. https://www.eia.gov/consumption/residential/reports/2015/energybills/ .
55. Hernández D. “Understanding `energy insecurity' and why it matters to health.” Soc Sci Med. 2016; 167:1-10.
56. Hernández D. Understanding `energy insecurity' and why it matters to health. Soc Sci Med. 2016 Oct; 167:1-10. doi: 10.1016/j.socscimed.2016.08.029. Epub 2016 Aug 21. PMID: 27592003; PMCID: PMC5114037.
57. Hernández D. “What `Merle' Taught Me About Energy Insecurity and Health.” Health Affairs, VOL.37, NO.3: Advancing Health Equity Narrative Matters. March 2018. https://doi.org/10.1377/hlthaff.2017.1413 .
58. US Energy Information Administration. “One in Three U.S. Households Faced Challenges in Paying Energy Bills in 2015.” 2017 Oct 13. https://www.eia.gov/consumption/residential/reports/2015/energybills/ .
59. Hernández D. Understanding `energy insecurity' and why it matters to health. Soc Sci Med. 2016 Oct; 167:1-10. doi: 10.1016/j.socscimed.2016.08.029. Epub 2016 Aug 21. PMID: 27592003; PMCID: PMC5114037.
60. Hernández D, Siegel E. Energy insecurity and its ill health effects: A community perspective on the energy-health nexus in New York City. Energy Res Soc Sci. 2019 Jan; 47:78-83. doi: 10.1016/j.erss.2018.08.011. Epub 2018 Sep 8. PMID: 32280598; PMCID: PMC7147484.
61. https://www.fcc.gov/broadbandbenefit .
62. National Council on Aging (NCOA). “How to Make It Easier for Older Adults to Get Energy and Utility Assistance.” Promising Practices Clearinghouse for Professionals. Jan 13, 2022. https://www.ncoa.org/article/how-to-make-it-easier-for-older-adults-to-get-energy-and-utility-assistance .
63. This validated survey was developed as a clinical indicator of household energy security among pediatric caregivers. Cook, J.T., D.A. Frank., P.H. Casey, R. Rose-Jacobs, M.M. Black, M. Chilton, S. Ettinger de Cuba, et al. “A Brief Indicator of Household Energy Security: Associations with Food Security, Child Health, and Child Development in US Infants and Toddlers.” Pediatrics, vol. 122, no. 4, 2008, pp. e874-e875. https://doi.org/10.1542/peds.2008-0286 .
64. In October 2023, we released two new annual Health Equity Confidential Feedback Reports to IRFs: The Discharge to Community (DTC) Health Equity Confidential Feedback Report and the Medicare Spending Per Beneficiary (MSPB) Health Equity Confidential Feedback Report. The PAC Health Equity Confidential Feedback Reports stratified the DTC and MSPB measures by dual-enrollment status and race/ethnicity. For more information on the Health Equity Confidential Feedback Reports, please refer to the Education and Outreach materials available on the IRF QRP Training web page at https://www.cms.gov/medicare/quality-initiatives-patient-assessment-instruments/irf-quality-reporting/irf-quality-reporting-training .
65. National Academies of Sciences, Engineering, and Medicine. 2016. Accounting for Social Risk Factors in Medicare Payment: Identifying Social Risk Factors. Washington, DC: The National Academies Press. https://doi.org/10.17226/21858 .
66. National Academies of Sciences, Engineering, and Medicine. 2020. Leading Health Indicators 2030: Advancing Health, Equity, and Well-Being. Washington, DC: The National Academies Press. https://doi.org/10.17226/25682 .
67. https://nam.edu/standardized-screening-for-health-related-social-needs-in-clinical-settings-the-accountable-health-communities-screening-tool/ .
68. Billioux, A., Verlander, K., Anthony, S., & Alley, D. (2017). Standardized Screening for Health-Related Social Needs in Clinical Settings: The Accountable Health Communities Screening Tool. NAM Perspectives, 7(5). Available at: https://doi.org/10.31478/201705b . Accessed on June 9, 2024.
69. Billioux, A., Verlander, K., Anthony, S., & Alley, D. (2017). Standardized Screening for Health-Related Social Needs in Clinical Settings: The Accountable Health Communities Screening Tool. NAM Perspectives, 7(5). Available at: https://doi.org/10.31478/201705b . Accessed on June 9, 2024.
70. Centers for Medicare & Medicaid Services. (2021). Accountable Health Communities Model. Accountable Health Communities Model | CMS Innovation Center. Available at: https://innovation.cms.gov/innovation-models/ahcm . Accessed on February 20, 2023.
71. https://www.cms.gov/priorities/innovation/data-and-reports/2023/ahc-second-eval-rpt-fg .
72. https://www.cms.gov/priorities/innovation/data-and-reports/2023/ahc-second-eval-rpt-fg .
73. Accountable Health Communities (AHC) Model Evaluation, Second Evaluation Report. May 2023. This project was funded by the Centers for Medicare & Medicaid Services under contract no. HHSM-500-2014-000371, Task Order75FCMC18F0002. https://www.cms.gov/priorities/innovation/data-and-reports/2023/ahc-second-eval-rpt .
74. In October 2023, we released two new annual Health Equity Confidential Feedback Reports to IRFs: The Discharge to Community (DTC) Health Equity Confidential Feedback Report and the Medicare Spending Per Beneficiary (MSPB) Health Equity Confidential Feedback Report. The PAC Health Equity Confidential Feedback Reports stratified the DTC and MSPB measures by dual-enrollment status and race/ethnicity. For more information on the Health Equity Confidential Feedback Reports, please refer to the Education and Outreach materials available on the IRF QRP Training web page at https://www.cms.gov/medicare/quality-initiatives-patient-assessment-instruments/irf-quality-reporting/irf-quality-reporting-training .
75. Brooks-LaSure, C. (2021). My First 100 Days and Where We Go from Here: A Strategic Vision for CMS. Centers for Medicare & Medicaid. Available at https://www.cms.gov/blog/my-first-100-days-and-where-we-go-here-strategic-vision-cms .
76. The Biden-Harris Administration's strategic approach to addressing health related social needs can be found in The U.S. Playbook to Address Social Determinants of Health (SDOH) (2023): https://www.whitehouse.gov/wp-content/uploads/2023/11/SDOH-Playbook-3.pdf .
77. Medicare Benefit Policy Manual (100-2). Chapter 1, Section 110.2. Available at: https://www.cms.gov/regulations-and-guidance/guidance/manuals/downloads/bp102c01.pdf .
78. World Health Organization. Social determinants of health. Available at https://www.who.int/health-topics/social-determinants-of-health#tab=tab_1 .
79. These cue cards are currently available on the IRF QRP Training web page at https://www.cms.gov/medicare/quality/inpatient-rehabilitation-facility/irf-quality-reporting-training .
80. Haff, N, Choudhry, N.K., Bhatkhande, G., Li, Y., Antol, D., Renda, A., Laufffenburger, J. Frequency of Quarterly Self-reported Health-Related Social Needs Among Older Adults, 2020. JAMA Network Open. 2022;5(6):e2219645. Doi:101001/jamanetworkopen.2022.19645. Accessed June 9, 2024.
81. Gundersen C, Engelhard E, Crumbaugh A, Seligman, H.K. Brief assessment of Food insecurity Accurately Identifies High0Risk US Adults. Public Health Nutrition, 2017. Doi: 10.1017/S1368980017000180. https://childrenshealthwatch.org/wp-content/uploads/brief-assessment-of-food-insecurity-accurately- identifies-high-risk-us-adults.pdf. Accessed July 2, 2024.
82. Haff, N, Choudhry, N.K., Bhatkhande, G., Li, Y., Antol, D., Renda, A., Laufffenburger, J. Frequency of Quarterly Self-reported Health-Related Social Needs Among Older Adults, 2020. JAMA Network Open. 2022;5(6):e2219645. Doi:101001/jamanetworkopen.2022.19645. Accessed June 9, 2024.
83. The seven SDOH items are ethnicity, race, preferred language, interpreter services, health literacy, transportation, and social isolation ( 84 FR 39149 through 39161 ).
84. Centers for Medicare & Medicaid Services, FY2024 Inpatient Psychiatric Prospective Payment System—Rate Update ( 88 FR 51107 through 51121 ).
85. Centers for Medicare & Medicaid Services, FY2023 IPPS/LTCH PPS final rule ( 87 FR 49202 through 49215 ).
86. Centers for Medicare & Medicaid Services, FY2024 Inpatient Psychiatric Prospective Payment System—Rate Update ( 88 FR 51107 through 51121 ).
87. Haff, N, Choudhry, N.K., Bhatkhande, G., Li, Y., Antol, D., Renda, A., Laufffenburger, J. Frequency of Quarterly Self-reported Health-Related Social Needs Among Older Adults, 2020. JAMA Network Open. 2022;5(6):e2219645. Doi:101001/jamanetworkopen.2022.19645. Accessed June 9, 2024.
88. The Post-Acute Care (PAC) and Hospice Quality Reporting Program Cross-Setting TEP summary report will be published in early summer or as soon as technically feasible. IRFs can monitor the Partnership for Quality Measurement website at https://mmshub.cms.gov/get-involved/technical-expert-panel/updates for updates.
89. Centers for Medicare & Medicaid Services. Aligning Quality Measures Across CMS—the Universal Foundation. November 17, 2023. https://www.cms.gov/aligning-quality-measures-across-cms-universal-foundation .
90. A composite measure can summarize multiple measures through the use of one value or piece of information. More information can be found at https://www.cms.gov/medicare/quality-initiatives-patient-assessment-instruments/mms/downloads/composite-measures.pdf .
91. CMS Measures Inventory Tool. Adult immunization status measure found at https://cmit.cms.gov/cmit/#/FamilyView?familyId=26 .
92. CMS Measures Inventory Tool. Clinical Depression Screening and Follow-Up measure found at https://cmit.cms.gov/cmit/#/FamilyView?familyId=672 .
93. Patient reported outcome measures are tools used to collect patient-reported outcomes (PRO). CMS defines a PRO as any report of the status of a patient's health condition or health behavior coming directly from the patient, without interpretation of the patient's response by a clinician or anyone else. Available at: https://mmshub.cms.gov/sites/default/files/Patient-Reported-Outcome-Measures.pdf .
94. The Patient Health Questionnaire (PHQ)-2 to -9 (PHQ-2 to -9) screening tool is used as the initial screening test for depression. The items were adopted as standardized patient assessment data elements in the FY 2020 IRF PPS final rule ( 84 FR 39119 through 39121 ) and are collected on all patients admitted to an IRF.
95. The Patient Activation Measure (PAM®) is a 10- or 13-item survey that assesses an individual's knowledge, skills and confidence integral to managing one's own health and healthcare. Available at: https://www.insigniahealth.com/pam/ .
96. FY 2020 IRF PPS final rule ( 84 FR 39161 through 39162 ).
97. Due to data availability of IRF SDOH standardized patient assessment data elements, this is based on three quarters of Transportation data.
98. The analysis is limited to patients who responded to the Transportation item at both admission and discharge.
99. https://prapare.org/faq/ .
100. Feltner C WI, Berkman N, et al. Screening for Intimate Partner Violence, Elder Abuse, and Abuse of Vulnerable Adults: An Evidence Review for the U.S. Preventive Services Task Force Agency for Healthcare Research and Quality. 2018. Available at https://www.ncbi.nlm.nih.gov/books/NBK533720/ .
101. National Academy of Science EaM. A Roadmap to Reducing Child Poverty. The National Academies; 2019.
102. Wise PH. Child poverty and the promise of Human Capacity: childhood as a foundation for healthy aging. Acad Pediatr. 2016;16(suppl 3):S37-S45.
103. Boch S, Keedy H, Chavez L, et al. An integrative review of social determinants of health screenings used in primary care settings. J Health Care Poor Underserved. 2020;31:603-622.
104. Halpin, K, Colvin, JD, Clements, MA, et al. Outcomes of Health-Related Social Needs Screening in a Midwest Pediatric Diabetes Clinic Network. Diabetes. 2023; Vol. 72; Iss: Supplement 1.
105. Nerlinger, AL, Kopsombut, G. Social determinants of health screening in pediatric healthcare settings. Curr Opin Pediatr. 2023 Feb 1;35(1):14-21. Doi: 10.1097/MOP.0000000000001191.
106. Gray, T.W., Podewils, L.J., Rasulo, R.M., Weiss, R.P., Tomcho M.M. Examining the Implementation of Health-Related Social Need (HRSN) Screenings at a Pediatric Community Health Center. Journal of Primary Care & Community Health. 2023. Volume 14: 1-8. https://doi.org/10.1177/21501319231171519 .
107. In the FY 2010 IRF PPS final rule ( 74 FR 39798 through 39800 ), CMS revised the regulation text in §§ 412.604, 412.606, 412.610, 412.614, and 412.618 to require that all IRFs submit IRF-PAI data on all of their Medicare Part C patients.
108. In the FY 2023 IRF PPS final rule ( 87 FR 47073 through 47092 ), CMS revised the regulation text in §§ 412.604, 412.606, 412.610, 412.614, and 412.618 to require that all IRFs submit IRF-PAI data on each patient receiving care in an IRF, regardless of payer.
109. https://www.reginfo.gov/public/do/DownloadNOA?requestID=494186 .
110. U.S. Bureau of Labor Statistics' (BLS) May 2022 National Occupational Employment and Wage Estimates. https://www.bls.gov/oes/current/oes_nat.htm .
111. FY 2016 IRF PPS proposed rule https://www.federalregister.gov/citation/80-FR-23390 ( 80 FR 23390 ).
112. FY 2016 IRF PPS proposed rule ( 80 FR 23390 ).
113. U.S. Bureau of Labor Statistics' (BLS) May 2022 National Occupational Employment and Wage Estimates. https://www.bls.gov/oes/current/oes_nat.htm .
114. U.S. Bureau of Labor Statistics' (BLS) May 2022 National Occupational Employment and Wage Estimates. https://www.bls.gov/oes/current/oes_nat.htm .
[ FR Doc. 2024-16911 Filed 7-31-24; 4:15 pm]
BILLING CODE 4120-01-P
- Executive Orders
Reader Aids
Information.
- About This Site
- Legal Status
- Accessibility
- No Fear Act
- Continuity Information

IMAGES
VIDEO
COMMENTS
Turn the feature on or off while presenting. If you're in the middle of giving a presentation and want to turn the feature on or off, click the Toggle Subtitles button from Slide Show View or Presenter View, on the toolbar below the main slide:. In Slide Show View:. In Presenter View:. You can also toggle subtitles from the right-click menu, or with the shortcut key J.
Set Up Subtitles in PowerPoint. Open your slideshow in PowerPoint and head to the Slide Show tab to set up the subtitles. On the right side of the ribbon, click "Subtitle Settings." Use the drop-down list to select the Spoken Language, if necessary, and then the Subtitle Language from over 60 dialects. If you have more than one microphone ...
The most common mistakes for title and final slides. If you asked 100 people what belongs on your PowerPoint's title slide, the majority would answer 'The title, maybe a subtitle, the presenter's name and company, the date'. That kind of title slide is alright, but you usually say all of these things in the beginning of a presentation ...
Avoid cluttering the slide with too much text or too many design elements. Focus on the main title and, if necessary, a subtitle or tagline. White space can be your friend, making the slide more elegant and easier to read. 5. Add a Personal Touch. Adding a personal touch to your title slide can make it more engaging.
In PowerPoint, in the Normal view, open the slide that has the video that you want to add captions to. Select the video on the slide. On the Playback tab, select Insert Captions, and then select Insert Captions. In the Insert Captions dialog box, select the file or files and then click Insert. If you need to add more caption files, just repeat ...
Step 2 - Check the Subtitle Settings. Check the subtitle settings to ensure they are in line with your requirements from the Subtitle Settings drop down menu. From here, you can select the position of the spoken language, subtitle language, position of the subtitles, microphone settings, and system settings. For the purpose of this post, we ...
Since title slides are usually on display for a while before a presentation, you want to make sure that they're doing a good job of marketing you, your topic, and your company. Always include the following elements on your title slides: Title of presentation, with a subtitle if the presentation's title is unclear. Your name.
To get started, open a presentation and select Slide Show from the main navigation ribbon. At the far right, you will see a sub-menu called Captions and Subtitles. Go ahead and check the option to Always Use Subtitles, which turns on captions for your slide show. Captions and subtitles use Microsoft speech recognition services to provide you ...
Method 1: Choosing A Template From The PowerPoint Library For Creating A Title Slide. Step 1: To create a title slide, open the PowerPoint presentation application and click on 'New.'. Step 2: You will find many PowerPoint templates; double-click on the template you like and click on 'Create.'. Step 3: The template you chose will appear.
At launch, Live Captions and Subtitles will support 12 spoken languages and display on-screen captions or subtitles in one of 60+ languages. Live Captions and Subtitles in PowerPoint brings: The power of AI to presenters, so they can convey simple and complex information across subjects and topics. Speech recognition that automatically adapts ...
Presentation title pages should always fit with your overall brand style. Building a logo slide as your title slide doesn't have to be complicated. A well-made logo slide shows your branding quickly. An alternate option for this slide is slide design 4, a simple slide with a dark color scheme. Just add your logo to that slide to create contrast.
Presentation titles can also be optimized with SEO criteria if the intent is to repurpose the presentation in a web-based format. The question lies in how natural and relevant sounds, in comparison with a descriptive presentation title, as it may evoke emotions rather than direct, keyword-targeted results. 1. Surprise
The title slide is an important part of the presentation and is often good for marketing your ideas beforehand using creatively crafted layouts. Slide Vs. Title Slide Layout. A title slide contains the title in a presentation deck. The layout of such a slide can contain a title, subtitle, and other relevant information.
To create this shape, you can follow the below steps -. On the menu bar, click on "Insert" and then click on "Shapes". Under the basic shapes option, select the trapezium shape. Next, create the shape on your slide. Make sure that the size of the trapezium is good enough to cover about ⅔ parts of the slide.
Use the Layout option to create a standalone title slide or to add a title to a slide that contains other text. You can also use the Outline view or the Accessibility ribbon to create and update the titles of your slides. Select a heading below to open it and see the detailed instructions. Microsoft 365 2016-2024 macOS Web. Select a heading ...
To enable subtitles in PowerPoint, open your presentation and navigate to the "Slide Show" tab. On the right side of the ribbon, click on "Subtitle Settings". From the dropdown list, select both the spoken language and subtitle language. Ensure you have the latest version of PowerPoint as this feature is available with Microsoft 365 ...
A title slide in PowerPoint (as humans think of it as) is either the slide that is named "title slide" in your presentation, or the slide that looks like a title slide. Common elements include a large title, a subtitle, some kind of graphical element, etc. This is where you type the title and subtitle of your presentation, add your name ...
In a presentation, the slide title will be the first thing your audience sees, and if they only spend a few moments scanning your slide, make it easy for them to understand the primary point. This post provides real-world examples as well as seven practical tips for crafting action-oriented slide titles to communicate data effectively. Read ...
TL;DR: Your PowerPoint title slides are the gateway to your presentation, setting the stage and making the first impression on your audience. It's essential to design these slides meticulously to capture attention right from the start. A well-crafted title slide not only piques interest but also conveys professionalism and sets the tone for the content that follows.
Combine the Sentence in Step #1 With the Benefit in Step #2. Now that you have the two pieces, just put them together. When you do, you will create a series of catchy presentation titles. We Exceeded Our Corporate Goals and Increased Profit Last Quarter, So Your Quarterly Bonus Has Also Increased.
You can then immediately add a title by doing one of the following: Click a slide number and it will display highlighted in the panel on the left side. Click next to the number and add a title. Click the drop-down arrow to the right of the slide and select "Add Slide Title." Select the slide, use the Slide Title drop-down arrow on the ...
Create single-page webpages for portfolios, resumes, presentations, blog posts, photo galleries, and more. You can also use webpages to promote an upcoming event, advertise a special offer, or act as a weekly or monthly newsletter for business. ... Add title and subtitle to the webpage.
This final action updates the prospective payment rates for inpatient rehabilitation facilities (IRFs) for Federal fiscal year (FY) 2025. As required by statute, this final action includes the classification and weighting factors for the IRF prospective payment system's case-mix groups and a...
childhood vaccines. Subtitle 2 of title XXI of the PHS Act, 42 U.S.C. 300aa- 10 et seq., provides that those seeking compensation are to file a petition with the United States Court of Federal Claims and to serve a copy of the petition to the Secretary of HHS, who is named as the respondent in each proceeding. The Secretary has delegated