An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager

Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Childhood obesity: A review of current and future management options
Affiliations.
- 1 Department of Paediatric Endocrinology, Alder Hey Children's Hospital, Liverpool, UK.
- 2 Centre for Endocrinology, William Harvey Research Institute, Barts and the London School of Medicine, Queen Mary University of London, London, UK.
- 3 Department of Paediatric Dietetics, Alder Hey Children's Hospital, Liverpool, UK.
- 4 Department of Paediatric Clinical Psychology, Alder Hey Children's Hospital, Liverpool, UK.
- PMID: 34750858
- DOI: 10.1111/cen.14625
Obesity is becoming increasingly prevalent in paediatric populations worldwide. In addition to increasing prevalence, the severity of obesity is also continuing to rise. Taken together, these findings demonstrate a worrying trend and highlight one of the most significant challenges to public health. Childhood obesity affects multiple organs in the body and is associated with both significant morbidity and ultimately premature mortality. The prevalence of complications associated with obesity, including dyslipidaemia, hypertension, fatty liver disease and psychosocial complications are becoming increasingly prevalent within the paediatric populations. Treatment guidelines currently focus on intervention with lifestyle and behavioural modifications, with pharmacotherapy and surgery reserved for patients who are refractory to such treatment. Research into adult obesity has established pharmacological novel therapies, which have been approved and established in clinical practice; however, the research and implementation of such therapies in paediatric populations have been lagging behind. Despite the relative lack of widespread research in comparison to the adult population, newer therapies are being trialled, which should allow a greater availability of treatment options for childhood obesity in the future. This review summarizes the current evidence for the management of obesity in terms of medical and surgical options. Both future therapeutic agents and those which cause weight loss but have an alternative indication are also included and discussed as part of the review. The review summarizes the most recent research for each intervention and demonstrates the potential efficacy and limitations of each treatment option.
Keywords: BMI; childhood obesity; lifestyle interventions; paediatrics; pharmacotherapy.
© 2021 John Wiley & Sons Ltd.
PubMed Disclaimer
Similar articles
- The effectiveness of web-based programs on the reduction of childhood obesity in school-aged children: A systematic review. Antwi F, Fazylova N, Garcon MC, Lopez L, Rubiano R, Slyer JT. Antwi F, et al. JBI Libr Syst Rev. 2012;10(42 Suppl):1-14. doi: 10.11124/jbisrir-2012-248. JBI Libr Syst Rev. 2012. PMID: 27820152
- Treatment Options for Severe Obesity in the Pediatric Population: Current Limitations and Future Opportunities. Ryder JR, Fox CK, Kelly AS. Ryder JR, et al. Obesity (Silver Spring). 2018 Jun;26(6):951-960. doi: 10.1002/oby.22196. Epub 2018 May 7. Obesity (Silver Spring). 2018. PMID: 29732716 Review.
- The future of Cochrane Neonatal. Soll RF, Ovelman C, McGuire W. Soll RF, et al. Early Hum Dev. 2020 Nov;150:105191. doi: 10.1016/j.earlhumdev.2020.105191. Epub 2020 Sep 12. Early Hum Dev. 2020. PMID: 33036834
- Real-World Strategies to Treat Hypertension Associated with Pediatric Obesity. Binka E, Brady TM. Binka E, et al. Curr Hypertens Rep. 2019 Feb 12;21(2):18. doi: 10.1007/s11906-019-0922-2. Curr Hypertens Rep. 2019. PMID: 30747290 Free PMC article. Review.
- Screening and Interventions for Childhood Overweight [Internet]. Whitlock EP, Williams SB, Gold R, Smith P, Shipman S. Whitlock EP, et al. Rockville (MD): Agency for Healthcare Research and Quality (US); 2005 Jul. Rockville (MD): Agency for Healthcare Research and Quality (US); 2005 Jul. PMID: 20722132 Free Books & Documents. Review.
- Is oxidative stress - antioxidants imbalance the physiopathogenic core in pediatric obesity? Lupu A, Fotea S, Jechel E, Starcea IM, Ioniuc I, Knieling A, Salaru DL, Sasaran MO, Cirstea O, Revenco N, Mihai CM, Lupu VV, Nedelcu AH. Lupu A, et al. Front Immunol. 2024 Aug 8;15:1394869. doi: 10.3389/fimmu.2024.1394869. eCollection 2024. Front Immunol. 2024. PMID: 39176098 Free PMC article. Review.
- The Prevention of Childhood Obesity Is a Priority: The Preliminary Results of the "EpPOI: Education to Prevent Childhood Obesity" Project. Porri D, Luppino G, Morabito LA, La Rosa E, Pepe G, Corica D, Valenzise M, Messina MF, Zirilli G, Li Pomi A, Alibrandi A, Di Mauro D, Aversa T, Wasniewska MG. Porri D, et al. Nutrients. 2024 Aug 2;16(15):2538. doi: 10.3390/nu16152538. Nutrients. 2024. PMID: 39125417 Free PMC article.
- Comparative Efficacy and Safety of Glucagon-like Peptide-1 Receptor Agonists in Children and Adolescents with Obesity or Overweight: A Systematic Review and Network Meta-Analysis. Liu L, Shi H, Shi Y, Wang A, Guo N, Tao H, Nahata MC. Liu L, et al. Pharmaceuticals (Basel). 2024 Jun 24;17(7):828. doi: 10.3390/ph17070828. Pharmaceuticals (Basel). 2024. PMID: 39065679 Free PMC article. Review.
- Analysis of Prescription Trends for Narcotic Appetite Suppressants: Utilizing the Narcotics Information Management System. Oh KS, Han E. Oh KS, et al. Yonsei Med J. 2024 Aug;65(8):480-487. doi: 10.3349/ymj.2023.0335. Yonsei Med J. 2024. PMID: 39048324 Free PMC article.
- The Impact of Excessive Fructose Intake on Adipose Tissue and the Development of Childhood Obesity. Azevedo-Martins AK, Santos MP, Abayomi J, Ferreira NJR, Evangelista FS. Azevedo-Martins AK, et al. Nutrients. 2024 Mar 25;16(7):939. doi: 10.3390/nu16070939. Nutrients. 2024. PMID: 38612973 Free PMC article. Review.
- NHS Digital. National Statistics: National Child Measurement Programme, England. 2017/18. Accessed April, 2021. https://digital.nhs.uk/data-and-information/publications/statistical/nat...
- Viner RM, Kinra S, Christie D, et al. Improving the assessment and management of obesity in UK children and adolescents: the PROMISE research programme including a RCT. Programme Grants for Applied Research, No. 8.3. 2020.
- Baker C. Briefing paper: obesity statistics. House of Commons Library. 2019;3336:1-20.
- Styne DM, Arslanian SA, Connor EL, et al. Pediatric obesity-assessment, treatment, and prevention: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2017;102(3):709-757.
- Gungor NK. Overweight and obesity in children and adolescents. J Clin Res Pediatr Endocrinol. 2014;6(3):129-143.
Publication types
- Search in MeSH
Related information
Linkout - more resources, full text sources.
- Ovid Technologies, Inc.
- Genetic Alliance
- MedlinePlus Health Information

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 18 May 2023
Child and adolescent obesity
- Natalie B. Lister ORCID: orcid.org/0000-0002-9148-8632 1 , 2 ,
- Louise A. Baur ORCID: orcid.org/0000-0002-4521-9482 1 , 3 , 4 ,
- Janine F. Felix 5 , 6 ,
- Andrew J. Hill ORCID: orcid.org/0000-0003-3192-0427 7 ,
- Claude Marcus ORCID: orcid.org/0000-0003-0890-2650 8 ,
- Thomas Reinehr ORCID: orcid.org/0000-0002-4351-1834 9 ,
- Carolyn Summerbell 10 &
- Martin Wabitsch ORCID: orcid.org/0000-0001-6795-8430 11
Nature Reviews Disease Primers volume 9 , Article number: 24 ( 2023 ) Cite this article
46k Accesses
79 Citations
250 Altmetric
Metrics details
- Paediatric research
The prevalence of child and adolescent obesity has plateaued at high levels in most high-income countries and is increasing in many low-income and middle-income countries. Obesity arises when a mix of genetic and epigenetic factors, behavioural risk patterns and broader environmental and sociocultural influences affect the two body weight regulation systems: energy homeostasis, including leptin and gastrointestinal tract signals, operating predominantly at an unconscious level, and cognitive–emotional control that is regulated by higher brain centres, operating at a conscious level. Health-related quality of life is reduced in those with obesity. Comorbidities of obesity, including type 2 diabetes mellitus, fatty liver disease and depression, are more likely in adolescents and in those with severe obesity. Treatment incorporates a respectful, stigma-free and family-based approach involving multiple components, and addresses dietary, physical activity, sedentary and sleep behaviours. In adolescents in particular, adjunctive therapies can be valuable, such as more intensive dietary therapies, pharmacotherapy and bariatric surgery. Prevention of obesity requires a whole-system approach and joined-up policy initiatives across government departments. Development and implementation of interventions to prevent paediatric obesity in children should focus on interventions that are feasible, effective and likely to reduce gaps in health inequalities.
Similar content being viewed by others

Management for children and adolescents with overweight and obesity: a recommendations mapping
Unraveling Complexity about Childhood Obesity and Nutritional Interventions: Modeling Interactions Among Psychological Factors

Pediatric weight management interventions improve prevalence of overeating behaviors
Introduction.
The prevalence of child and adolescent obesity remains high and continues to rise in low-income and middle-income countries (LMICs) at a time when these regions are also contending with under-nutrition in its various forms 1 , 2 . In addition, during the COVID-19 pandemic, children and adolescents with obesity have been more likely to have severe COVID-19 requiring hospitalization and mechanical ventilation 3 . At the same time, the pandemic was associated with rising levels of childhood obesity in many countries. These developments are concerning, considering that recognition is also growing that paediatric obesity is associated with a range of immediate and long-term negative health outcomes, a decreased quality of life 4 , 5 , an increased presentation to health services 6 and increased economic costs to individuals and society 7 .
Body weight is regulated by a range of energy homeostatic and cognitive–emotional processes and a multifactorial interplay of complex regulatory circuits 8 . Paediatric obesity arises when multiple environmental factors — covering preconception and prenatal exposures, as well as broader changes in the food and physical activity environments — disturb these regulatory processes; these influences are now widespread in most countries 9 .
The treatment of obesity includes management of obesity-associated complications, a developmentally sensitive approach, family engagement, and support for long-term behaviour changes in diet, physical activity, sedentary behaviours and sleep 10 . New evidence highlights the role, in adolescents with more severe obesity, of bariatric surgery 11 and pharmacotherapy, particularly the potential for glucagon-like peptide 1 (GLP1) receptor agonists 12 .
Obesity prevention requires a whole-system approach, with policies across all government and community sectors systematically taking health into account, avoiding harmful health impacts and decreasing inequity. Programmatic prevention interventions operating ‘downstream’ at the level of the child and family, as well as ‘upstream’ interventions at the level of the community and broader society, are required if a step change in tackling childhood obesity is to be realized 13 , 14 .
In this Primer, we provide an overview of the epidemiology, causes, pathophysiology and consequences of child and adolescent obesity. We discuss diagnostic considerations, as well as approaches to its prevention and management. Furthermore, we summarize effects of paediatric obesity on quality of life, and open research questions.
Epidemiology
Definition and prevalence.
The World Health Organization (WHO) defines obesity as “abnormal or excessive fat accumulation that presents a risk to health” 15 . Paediatric obesity is defined epidemiologically using BMI, which is adjusted for age and sex because of the physiological changes in BMI during growth 16 . Global prevalence of paediatric obesity has risen markedly over the past four decades, initially in high-income countries (HICs), but now also in many LMICs 1 .
Despite attempts to standardize the epidemiological classification, several definitions of paediatric obesity are in use; hence, care is needed when comparing prevalence rates. The 2006 WHO Child Growth Standard, for children aged 0 to 5 years, is based on longitudinal observations of multiethnic populations of children with optimal infant feeding and child-rearing conditions 17 . The 2007 WHO Growth Reference is used for the age group 5–19 years 18 , and the 2000 US Centers for Disease Control and Prevention (CDC) Growth Charts for the age group 2–20 years 19 . The WHO and CDC definitions based on BMI-for-age charts are widely used, including in clinical practice. By contrast, the International Obesity Task Force (IOTF) definition, developed from nationally representative BMI data for the age group 2–18 years from six countries, is used exclusively for epidemiological studies 20 .
For the age group 5–19 years, between 1975 and 2016, the global prevalence of obesity (BMI >2 standard deviations (SD) above the median of the WHO growth reference) increased around eightfold to 5.6% in girls and 7.8% in boys 1 . Rates have plateaued at high levels in many HICs but have accelerated in other regions, particularly in parts of Asia. For the age group 2–4 years, between 1980 and 2015, obesity prevalence (IOTF definition, equivalent to an adult BMI of ≥30 kg/m 2 ) increased from 3.9% to 7.2% in boys and from 3.7% to 6.4% in girls 21 . Obesity prevalence is highest in Polynesia and Micronesia, the Middle East and North Africa, the Caribbean and the USA (Fig. 1 ). Variations in prevalence probably reflect different background levels of obesogenic environments, or the sum total of the physical, economic, policy, social and cultural factors that promote obesity 22 . Obesogenic environments include those with decreased active transport options, a ubiquity of food marketing directed towards children, and reduced costs and increased availability of nutrient-poor, energy-dense foods. Particularly in LMICs, the growth of urbanization, new forms of technology and global trade have led to reduced physical activity at work and leisure, a shift towards Western diets, and the expansion of transnational food and beverage companies to shape local food systems 23 .
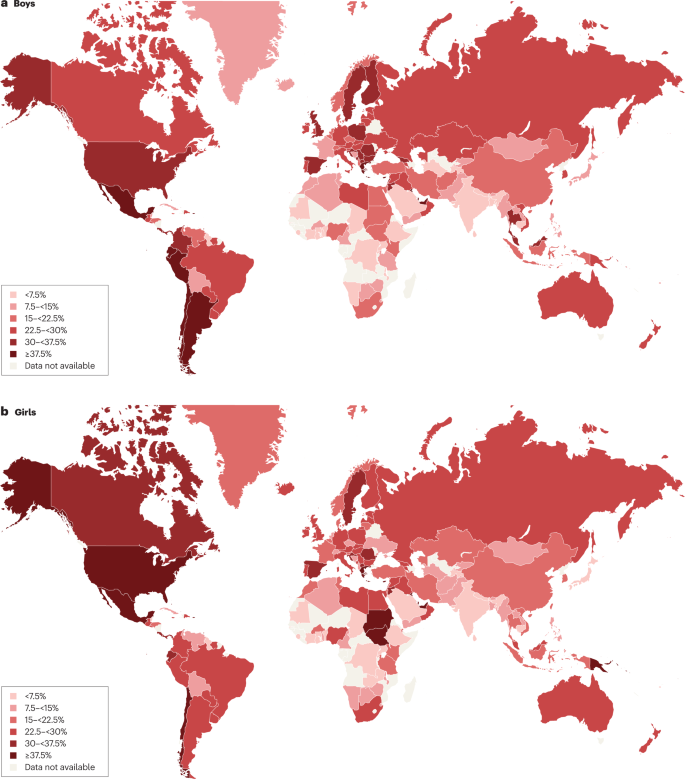
Maps showing the proportions of children and adolescents living with overweight or obesity (part a , boys; part b , girls) according to latest available data from the Global Obesity Observatory . Data might not be comparable between countries owing to differences in survey methodology.
The reasons for varying sex differences in prevalence in different countries are unclear but may relate to cultural variations in parental feeding practices for boys and girls and societal ideals of body size 24 . In 2016, obesity in the age group 5–19 years was more prevalent in girls than in boys in sub-Saharan Africa, Oceania and some middle-income countries in other regions, whereas it was more prevalent in boys than in girls in all HICs, and in East and South-East Asia 21 . Ethnic and racial differences in obesity prevalence within countries are often assumed to mirror variations in social deprivation and other social determinants of obesity. However, an independent effect of ethnicity even after adjustment for socioeconomic status has been documented in the UK, with Black and Asian boys in primary school having higher prevalence of obesity than white boys 25 .
Among individuals with obesity, very high BMI values have become more common in the past 15 years. The prevalence of severe obesity (BMI ≥120% of the 95th percentile (CDC definition), or ≥35 kg/m 2 at any age 26 , 27 ) has increased in many HICs, accounting for one-quarter to one-third of those with obesity 28 , 29 . Future health risks of paediatric obesity in adulthood are well documented. For example, in a data linkage prospective study in Israel with 2.3 million participants who had BMI measured at age 17 years, those with obesity (≥95th percentile BMI for age) had a much higher risk of death from coronary heart disease (HR 4.9, 95% CI 3.9–6.1), stroke (HR 2.6, 95% CI 1.7–4.1) and sudden death (HR 2.1, 95% CI 1.5–2.9) compared with those whose BMI fell between the 5th and 24th percentiles 30 .
Causes and risk factors
Early life is a critical period for childhood obesity development 9 , 31 , 32 , 33 . According to the Developmental Origins of Health and Disease framework, the early life environment may affect organ structure and function and influence health in later life 34 , 35 . Meta-analyses have shown that preconception and prenatal environmental exposures, including high maternal pre-pregnancy BMI and, to a lesser extent, gestational weight gain, as well as gestational diabetes and maternal smoking, are associated with childhood obesity, potentially through effects on the in utero environment 33 , 36 , 37 , 38 . Paternal obesity is also associated with childhood obesity 33 . Birthweight, reflecting fetal growth, is a proxy for in utero exposures. Both low and high birthweights are associated with later adiposity, with high birthweight linked to increased BMI and low birthweight to central obesity 33 , 39 .
Growth trajectories in early life are important determinants of later adiposity. Rapid weight gain in early childhood is associated with obesity in adolescence 32 . Also, later age and higher BMI at adiposity peak (the usual peak in BMI around 9 months of age), as well as earlier age at adiposity rebound (the lowest BMI reached between 4 and 7 years of age), are associated with increased adolescent and adult BMI 40 , 41 . Specific early life nutritional factors, including a lower protein content in formula food, are consistently associated with a lower risk of childhood obesity 42 , 43 . These also include longer breastfeeding duration, which is generally associated with a lower risk of childhood obesity 42 . However, some controversy exists, as these effects are affected by multiple sociodemographic confounding factors and their underlying mechanisms remain uncertain 44 . Some studies comparing higher and lower infant formula protein content have reported that the higher protein group have a greater risk of subsequent obesity, especially in early childhood 41 , 42 ; however, one study with a follow-up period until age 11 years found no significant difference in the risk of obesity, but an increased risk of overweight in the high protein group was still observed 42 , 43 , 45 . A high intake of sugar-sweetened beverages is associated with childhood obesity 33 , 46 .
Many other behavioural factors are associated with an increased risk of childhood obesity, including increased screen time, short sleep duration and poor sleep quality 33 , 47 , reductions in physical activity 48 and increased intake of energy-dense micronutrient-poor foods 49 . These have been influenced by multiple changes in the past few decades in the broader social, economic, political and physical environments, including the widespread marketing of food and beverages to children, the loss of walkable green spaces in many urban environments, the rise in motorized transport, rapid changes in the use of technology, and the move away from traditional foods to ultraprocessed foods.
Obesity prevalence is inextricably linked to relative social inequality, with data suggesting a shift in prevalence over time towards those living with socioeconomic disadvantage, and thus contributes to social inequalities. In HICs, being in lower social strata is associated with a higher risk of obesity, even in infants and young children 50 , whereas the opposite relationship occurs in middle-income countries 51 . In low-income countries, the relationship is variable, and the obesity burden seems to be across socioeconomic groups 52 , 53 .
Overall, many environmental, lifestyle, behavioural and social factors in early life are associated with childhood obesity. These factors cannot be seen in isolation but are part of a complex interplay of exposures that jointly contribute to increased obesity risk. In addition to multiple prenatal and postnatal environmental factors, genetic variants also have a role in the development of childhood obesity (see section Mechanisms/pathophysiology).
Comorbidities and complications
Childhood obesity is associated with a wide range of short-term comorbidities (Fig. 2 ). In addition, childhood obesity tracks into adolescence and adulthood and is associated with complications across the life course 32 , 41 , 54 , 55 .
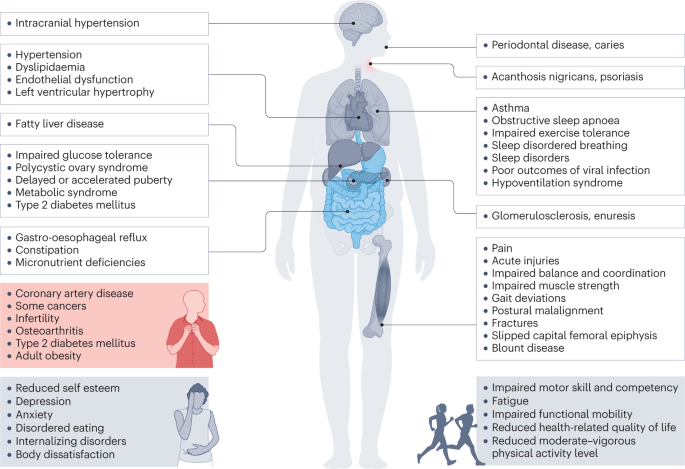
Obesity in children and adolescents can be accompanied by various other pathologies. In addition, childhood obesity is associated with complications and disorders that manifest in adulthood (red box).
Increased BMI, especially in adolescence, is linked to a higher risk of many health outcomes, including metabolic disorders, such as raised fasting glucose, impaired glucose tolerance, type 2 diabetes mellitus (T2DM), metabolic syndrome and fatty liver disease 56 , 57 , 58 , 59 . Other well-recognized obesity-associated complications include coronary heart disease, asthma, obstructive sleep apnoea syndrome (itself associated with metabolic dysfunction and inflammation) 60 , orthopaedic complications and a range of mental health outcomes including depression and low self-esteem 27 , 55 , 57 , 61 , 62 , 63 .
A 2019 systematic review showed that children and adolescents with obesity are 1.4 times more likely to have prediabetes, 1.7 times more likely to have asthma, 4.4 times more likely to have high blood pressure and 26.1 times more likely to have fatty liver disease than those with a healthy weight 64 . In 2016, it was estimated that, at a global level by 2025, childhood obesity would lead to 12 million children aged 5–17 years with glucose intolerance, 4 million with T2DM, 27 million with hypertension and 38 million with fatty liver disease 65 . These high prevalence rates have implications for both paediatric and adult health services.
Mechanisms/pathophysiology
Body weight regulation.
Body weight is regulated within narrow limits by homeostatic and cognitive–emotional processes and a multifactorial interplay of hormones and messenger substances in complex regulatory circuits (Fig. 3 ). When these regulatory circuits are disturbed, an imbalance between energy intake and expenditure leads to obesity or to poor weight gain. As weight loss is much harder to achieve than weight gain in the long term due to the regulation circuits discussed below, the development of obesity is encouraged by modern living conditions, which enable underlying predispositions for obesity to become manifest 8 , 66 .
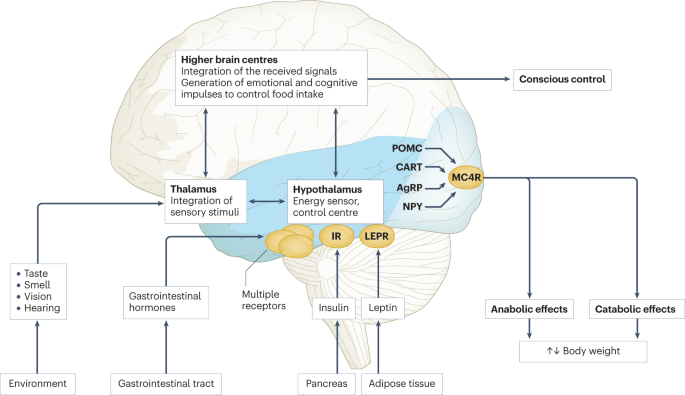
Body weight is predominantly regulated by two systems: energy homeostasis and cognitive–emotional control. Both homeostatic and non-homeostatic signals are processed in the brain, involving multiple hormone and receptor cascades 217 , 218 , 219 . This overview depicts the best-known regulatory pathways. The homeostatic system, which is mainly regulated by brain centres in the hypothalamus and brainstem, operates on an unconscious level. Both long-term signals from the energy store in adipose tissue (for example, leptin) and short-term hunger and satiety signals from the gastrointestinal tract signal the current nutrient status. During gastric distension or after the release of gastrointestinal hormones (multiple receptors are involved) and insulin, a temporary feeling of fullness is induced. The non-homeostatic or hedonic system is regulated by higher-level brain centres and operates at the conscious level. After integration in the thalamus, homeostatic signals are combined with stimuli from the environment, experiences and emotions; emotional and cognitive impulses are then induced to control food intake. Regulation of energy homeostasis in the hypothalamus involves two neuron types of the arcuate nucleus: neurons producing neuropeptide Y (NPY) and agouti-related peptide (AgRP) and neurons producing pro-opiomelanocortin (POMC). Leptin stimulates these neurons via specific leptin receptors (LEPR) inducing anabolic effects in case of decreasing leptin levels and catabolic effects in case of increasing leptin levels. Leptin inhibits the production of NPY and AgRP, whereas low leptin levels stimulate AgRP and NPY production resulting in the feeling of hunger. Leptin directly stimulates POMC production in POMC neurons. POMC is cleaved into different hormone polypeptides including α-melanocyte-stimulating hormone which in turn activates melanocortin 4 receptors (MC4R) of cells in the nucleus paraventricularis of the hypothalamus, leading to the feeling of satiety. CART, cocaine and amphetamine responsive transcript; IR, insulin receptor.
In principle, there are two main systems in the brain which regulate body weight 8 , 66 (Fig. 3 ): energy homeostasis and cognitive–emotional control. Energy homeostasis is predominantly regulated by brain centres in the hypothalamus and brainstem and operates at an unconscious level. Both long-term signals from the adipose tissue energy stores and short-term hunger and satiety signals from the gastrointestinal tract signal the current nutrient status 8 , 66 . For example, negative energy balance leading to reduced fat mass results in reduced leptin levels, a permanently reduced urge to exercise and an increased feeling of hunger. During gastric distension or after the release of gastrointestinal hormones and insulin, a temporary feeling of fullness is induced 8 , 66 . Cognitive–emotional control is regulated by higher brain centres and operates at a conscious level. Here, the homeostatic signals are combined with stimuli from the environment (sight, smell and taste of food), experiences and emotions 8 , 66 . Disorders at the level of cognitive–emotional control mechanisms include emotional eating as well as eating disorders. For example, the reward areas in the brain of people with overweight are more strongly activated by high-calorie foods than those in the brain of people with normal weight 67 . Both systems interact with each other, and the cognitive–emotional system is strongly influenced by the homeostatic control circuits.
Disturbances in the regulatory circuits of energy homeostasis can be genetically determined, can result from disease or injury to the regulatory centres involved, or can be caused by prenatal programming 8 , 66 . If the target value of body weight has been shifted, the organism tries by all means (hunger, drive) to reach the desired higher weight. These disturbed signals of the homeostatic system can have an imperative, irresistible character, so that a conscious influence on food intake is no longer effectively possible 8 , 66 . The most important disturbances of energy homeostasis are listed in Table 1 .
The leptin pathway
The peptide hormone leptin is primarily produced by fat cells. Its production depends on the amount of adipose tissue and the energy balance. A negative energy balance during fasting results in a reduction of circulating leptin levels by 50% after 24 h (ref. 68 ). In a state of weight loss, leptin production is reduced 69 . In the brain, leptin stimulates two neuron types of the arcuate nucleus in the hypothalamus via specific leptin receptors: neurons producing neuropeptide Y (NPY) and agouti-related peptide (AgRP) and neurons producing pro-opiomelanocortin (POMC). High leptin levels inhibit the production of NPY and AgRP, whereas low leptin levels stimulate AgRP and NPY production. By contrast, leptin directly stimulates POMC production in POMC neurons (Fig. 3 ). POMC is a hormone precursor that is cleaved into different hormone polypeptides by specific enzymes, such as prohormone convertase 1 (PCSK1). This releases α-melanocyte-stimulating hormone (α-MSH) which in turn activates melanocortin 4 receptors (MC4R) of cells in the nucleus paraventricularis of the hypothalamus, leading to the feeling of satiety. Rare, functionally relevant mutations in the genes for leptin and leptin receptor, POMC , PCSK1/3 or MC4R lead to extreme obesity in early childhood. These forms of obesity are potential indications for specific pharmacological treatments, for example setmelanotide 70 , 71 . MC4R mutations are the most common cause of monogenic obesity, as heterozygous mutations can be symptomatic depending on the functional impairment and with variable penetrance and expression. Other genes have been identified, in which rare heterozygous pathological variants are also associated with early onset obesity (Table 1 ).
Pathological changes in adipose tissue
Adipose tissue can be classified into two types, white and brown adipose tissue. White adipose tissue comprises unilocular fat cells and brown adipose tissue contains multilocular fat cells, which are rich in mitochondria 72 . A third type of adipocyte, beige adipocytes, within the white adipose tissue are induced by prolonged exposure to cold or adrenergic signalling, and show a brown adipocyte-like morphology 72 . White adipose tissue has a large potential to change its volume to store energy and meet the metabolic demands of the body. The storage capacity and metabolic function of adipose tissue depend on the anatomical location of the adipose tissue depot. Predominant enlargement of white adipose tissue in the visceral, intra-abdominal area (central obesity) is associated with insulin resistance and an increased risk of metabolic disease development before puberty. Accumulation of adipose tissue in the hips and flanks has no adverse effect and may be protective against metabolic syndrome. In those with obesity, adipose tissue is characterized by an increased number of adipocytes (hyperplasia), which originate from tissue-resident mesenchymal stem cells, and by enlarged adipocytes (hypertrophy) 73 . Adipocytes with a very large diameter reach the limit of the maximal oxygen diffusion distance, resulting in hypoxia, the development of an inflammatory expression profile (characterized by, for example, leptin, TNF and IL-6) and adipocyte necrosis, triggering the recruitment of leukocytes. Resident macrophages switch from the anti-inflammatory M2 phenotype to a pro-inflammatory M1 phenotype, which is associated with insulin resistance, further promoting local sterile inflammation and the development of fibrotic adipose tissue. This process limits the expandability of the adipose tissue for further storage of triglycerides. In the patient, the increase in fat mass in obesity is associated with insulin resistance and systemic low-grade inflammation characterized by elevated serum levels of C-reactive protein and pro-inflammatory cytokines. The limitation of adipose tissue expandability results in storage of triglycerides in other organs, such as the liver, muscle and pancreas 74 .
Genetics and epigenetics in the general population
Twin studies have found heritability estimates for BMI of up to 70% 75 , 76 . In contrast to rare monogenic forms of obesity, which are often caused by a single genetic defect with a large effect, the genetic background of childhood obesity in the general population is shaped by the joint effects of many common genetic variants, each of which individually makes a small contribution to the phenotype. For adult BMI, genome-wide association studies, which examine associations of millions of such variants across the genome at the same time, have identified around 1,000 genetic loci 77 . The largest genome-wide association studies in children, which include much smaller sample sizes of up to 60,000 children, have identified 25 genetic loci for childhood BMI and 18 for childhood obesity, the majority of which overlap 78 , 79 . There is also a clear overlap with genetic loci identified in adults, for example for FTO , MC4R and TMEM18 , but this overlap is not complete, some loci are specific to early life BMI, or have a relatively larger contribution in childhood 78 , 79 , 80 . These findings suggest that biological mechanisms underlying obesity in childhood are mostly similar to those in adulthood, but the relative influence of these mechanisms may differ at different phases of life.
The role of epigenetic processes in childhood and adolescent obesity has gained increasing attention. In children, several studies found associations between DNA methylation and BMI 81 , 82 , 83 , 84 , but a meta-analysis including data from >4,000 children identified only minimal associations 85 . Most studies support the hypothesis that DNA methylation changes are predominantly a consequence rather than a cause of obesity, which may explain the lower number of identified (up to 12) associations in children, in whom duration of exposure to a higher BMI is shorter than in adults, in whom associations with DNA methylation at hundreds of sites have been identified 85 , 86 , 87 . In addition to DNA methylation, some specific circulating microRNAs have been found to be associated with obesity in childhood 84 .
The field of epigenetic studies in childhood obesity is relatively young and evolving quickly. Future studies will need to focus on defining robust associations in blood as well as other tissues and on identifying cause-and-effect relationships. In addition, other omics, such as metabolomics and proteomics, are promising areas that may contribute to an improved aetiological understanding or may provide biological signatures that can be used as predictive or prognostic markers of childhood obesity and its comorbidities.
Parental obesity and childhood obesity
There is an established link between increased parental BMI and increased childhood BMI 88 , 89 . This link may be due to shared genetics, shared environment, a direct intrauterine effect of maternal BMI or a combination of these factors. In the case of shared genetics, the child inherits BMI-increasing genetic variants from one or both parents. Shared environmental factors, such as diet or lifestyle, may also contribute to an increased BMI in both parents and child. In addition, maternal obesity might create an intrauterine environment that programmes metabolic processes in the fetus, which increases the risk of childhood obesity. Some studies show larger effects of maternal than paternal BMI, indicating a potential causal intrauterine mechanism of maternal obesity, but evidence showing similar maternal and paternal effects is increasing. The data may indicate that there is only a limited direct intrauterine effect of maternal obesity on childhood obesity; rather, genetic effects inherited from the mother or father, or both, and/or shared environmental factors may contribute to childhood obesity risk 90 , 91 , 92 , 93 , 94 , 95 .
Diagnosis, screening and prevention
Diagnostic work-up.
The extent of overweight in clinical practice is estimated using BMI based on national charts 96 , 97 , 98 , 99 , 100 . Of note, the clinical classification of overweight or obesity differ depending on the BMI charts used and national recommendations; hence, local guidelines should be referred to. For example, the US CDC Growth Charts and several others use the 85th and 95th centile cut-points to denote overweight and obesity, respectively 19 . The WHO Growth Reference for children aged 5–19 years defines cut-points for overweight and obesity as a BMI-for-age greater than +1 and +2 SDs for BMI for age, respectively 18 . For children <5 years of age, overweight and obesity are defined as weight-for-height greater than +2 and +3 SDs, respectively, above the WHO Child Growth Standards median 17 . The IOTF and many countries in Europe use cut-points of 85th, 90th and 97th to define overweight, obesity and extreme obesity 26 .
BMI as an indirect measurement of body fat has some limitations; for example, pronounced muscle tissue leads to an increase in BMI, and BMI is not independent of height. In addition, people of different ethnicities may have different cut-points for obesity risk; for example, cardiometabolic risk occurs at lower BMI values in individuals with south Asian than in those with European ancestry 101 . Thus, BMI is best seen as a convenient screening tool that is supplemented by clinical assessment and investigations.
Other measures of body fat may help differentiate between fat mass and other tissues. Some of these tools are prone to low reliability, such as body impedance analyses (high day-to-day variation and dependent on level of fluid consumption) or skinfold thickness (high inter-observer variation), or are more expensive or invasive, such as MRI, CT or dual-energy X-ray absorptiometry, than simpler measures of body composition or BMI assessment.
Primary diseases rarely cause obesity in children and adolescents (<2%) 102 . However, treatable diseases should be excluded in those with obesity. A suggested diagnostic work-up is summarized in Fig. 4 . Routine measurement of thyroid-stimulating hormone (TSH) is not recommended 96 . Moderately elevated TSH levels (usually <10 IU/l) are frequently observed in obesity and are a consequence, and not a cause, of obesity 103 . In a growing child with normal height velocity, a normal BMI at the age of 2 years and normal cognitive development, no further diagnostic steps are necessary to exclude primary diseases 96 , 104 .
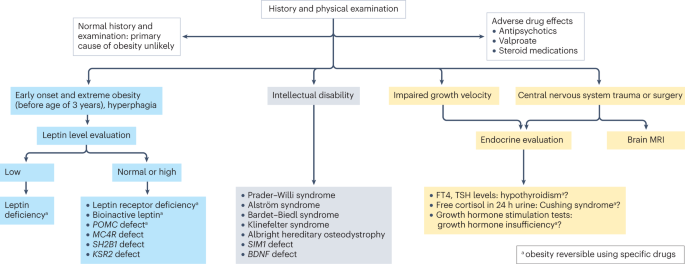
Concerning findings from a detailed medical history and physical examination will lead to further examinations. In individuals with early onset, extreme obesity (before age 3 years) and signs of hyperphagia, serum leptin level should be measured to rule out the extremely rare condition of congenital leptin deficiency. In individuals with normal or high leptin levels, genetic testing is indicated to search for monogenetic obesity. In individuals with intellectual disability, a syndromic disease may be present. Signs of impaired growth velocity or the history of central nervous system trauma or surgery will result in deeper endocrine evaluation and/or brain MRI. BDNF , brain-derived neurotropic factor; FT4, free thyroxin; KSR2 , kinase suppressor of ras 2; MC4R , melanocortin 4 receptor; POMC , pro-opiomelanocortin; SH2B1 , Src-homology 2 (SH2) B adapter protein 1; SIM1 , single-minded homologue 1; TSH, thyroid-stimulating hormone.
Clinical findings which need no further examination include pseudogynaecomastia (adipose tissue mimicking breast development; differentiated from breast tissue by ultrasonography), striae (caused by rapid weight increase) and a hidden penis in suprapubic adipose tissue (differentiated from micropenis by measurement of stretched penis length while pressing down on the suprapubic adipose tissue) 96 , 105 . Girls with obesity tend to have an earlier puberty onset (usually at around 8–9 years of age) and boys with severe obesity may have a delayed puberty onset (usually at around 13–14 years of age) 106 . Thus, if pubertal onset is slightly premature in girls or slightly delayed in boys, no further endocrine assessment is necessary.
Assessment of obesity-associated comorbidities
A waist to height ratio of >0.5 is a simple tool to identify central obesity 107 , 108 . Screening for cardiometabolic risk factors and fatty liver disease is recommended, especially in adolescents, and in those with more severe obesity or central adiposity, a strong family history of T2DM or premature heart disease, or relevant clinical symptoms, such as high blood pressure or acanthosis nigricans 96 , 97 , 98 , 99 , 109 . Investigations generally include fasting glucose levels, lipid profile, liver function and glycated haemoglobin, and might include an oral glucose tolerance test, polysomnography, and additional endocrine tests for polycystic ovary syndrome 96 , 97 , 98 , 99 .
T2DM in children and adolescents often occurs in the presence of a strong family history and may not be related to obesity severity 110 . T2DM onset usually occurs during puberty, a physiological state associated with increased insulin resistance 111 and, therefore, screening for T2DM should be considered in children and adolescents with obesity and at least one risk factor (family history of T2DM or features of metabolic syndrome) starting at pubertal onset 112 . As maturity-onset diabetes of the young (MODY) type II and type III are more frequent than T2DM in children and adolescents in many ethnicities, genetic screening for MODY may be appropriate 112 . Furthermore, type 1 diabetes mellitus (T1DM) should be excluded by measurement of autoantibodies in any individual with suspected diabetes with obesity. The differentiation of T2DM from MODY and T1DM is important as the diabetes treatment approaches differ 112 .
Several comorbidities of obesity should be considered if specific symptoms occur 96 , 109 . For polycystic ovary syndrome in hirsute adolescent girls with oligomenorrhoea or amenorrhoea, moderately increased testosterone levels and decreased sex hormone binding globulin levels are typical laboratory findings 113 . Obstructive sleep apnoea can occur in those with more severe obesity and who snore, have daytime somnolence or witnessed apnoeas. Diagnosis is made by polysomnography 114 . Minor orthopaedic disorders, such as flat feet and genu valgum, are frequent in children and adolescents with obesity and may cause pain. Major orthopaedic complications include slipped capital femoral epiphyses (acute and chronic), which manifest with hip and knee pain in young adolescents and are characterized by reduced range of hip rotation and waddling gait; and Blount disease (tibia vara), typically occurring in children aged 2–5 years 105 , 115 . In addition, children and adolescents with extreme obesity frequently have increased dyspnoea and decreased exercise capacity. A heightened demand for ventilation, elevated work of breathing, respiratory muscle inefficiency and diminished respiratory compliance are caused by increased truncal fat mass. This may result in a decreased functional residual capacity and expiratory reserve volume, ventilation to perfusion ratio abnormalities and hypoxaemia, especially when supine. However, conventional respiratory function tests are only mildly affected by obesity except in extreme cases 116 . Furthermore, gallstones should be suspected in the context of abdominal pain after rapid weight loss, which can be readily diagnosed via abdominal ultrasonography 105 . Finally, pseudotumor cerebri may present with chronic headache, and depression may present with flat affect, chronic fatigue and sleep problems 105 .
Obesity in adolescents can also be associated with disordered eating, eating disorders and other psychological disorders 117 , 118 . If suspected, assessment by a mental health professional is recommended.
A comprehensive approach
The 2016 report of the WHO Commission on Ending Childhood Obesity stated that progress in tackling childhood obesity has been slow and inconsistent, with obesity prevention requiring a whole-of-government approach in which policies across all sectors systematically take health into account, avoiding harmful health impacts and, therefore, improving population health and health equity 13 , 119 . The focus in developing and implementing interventions to prevent obesity in children should be on interventions that are feasible, effective and likely to reduce health inequalities 14 . Importantly, the voices of children and adolescents living with social disadvantage and those from minority groups must be heard if such interventions are to be effective and reduce inequalities 120 .
Figure 5 presents a system for the prevention of childhood obesity within different domains of the socioecological model 121 and highlights opportunities for interventions. These domains can be described on a continuum, from (most downstream) individual and interpersonal (including parents, peers and wider family) through to organizational (including health care and schools), community (including food, activity and environment), society (including media and finally cultural norms) and (most upstream) public policy (from local to national level). Interventions to prevent childhood obesity can be classified on the Nuffield intervention ladder 122 . This framework was proposed by the Nuffield Council on Bioethics in 2007 (ref. 122 ) and distributes interventions on the ladder steps depending on the degree of agency required by the individual to make the behavioural changes that are the aim of the intervention. The bottom step of the ladder includes interventions that provide information, which requires the highest agency and relies on a child, adolescent and/or family choosing (and their ability to choose) to act on that information and change behaviour. The next steps of the ladder are interventions that enable choice, guide choice through changing the default policy, guide choice through incentives, guide choice through disincentives, or restrict choice. On the top-most step of the ladder (lowest agency required) are interventions that eliminate choice.
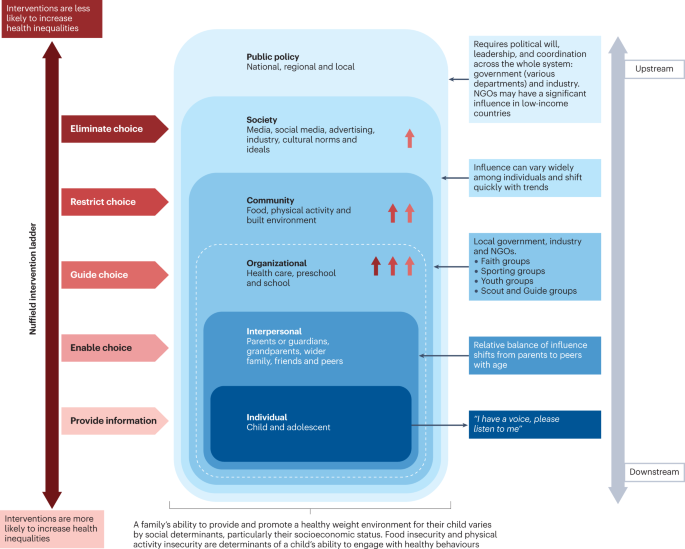
This schematic integrates interventions that were included in a Cochrane review 127 of 153 randomized controlled trials of interventions to prevent obesity in children and are high on the Nuffield intervention ladder 122 . The Nuffield intervention ladder distributes interventions depending on the degree of agency required for the behavioural changes that are the aim of the intervention. The socioecological model 121 comprises different domains (or levels) from the individual up to public policy. Interventions targeting the individual and interpersonal domains can be described as downstream interventions, and interventions within public policy can be described as the highest level of upstream interventions. Within each of these domains, arrow symbols with colours corresponding to the Nuffield intervention ladder category are used to show interventions that were both included in the Cochrane review 127 and that guide, restrict or eliminate choice as defined by the Nuffield intervention ladder 122 . Upstream interventions, and interventions on the top steps of the Nuffield ladder, are more likely to reduce inequalities. NGO, non-governmental organization.
Downstream and high-agency interventions (on the bottom steps of the Nuffield ladder) are more likely to result in intervention-generated inequalities 123 . This has been elegantly described and evidenced, with examples from the obesity prevention literature 124 , 125 . A particularly strong example is a systematic review of 38 interventions to promote healthy eating that showed that food price (an upstream and low-agency intervention) seemed to decrease inequalities, all interventions that combined taxes and subsidies consistently decreased inequalities, and downstream high-agency interventions, especially dietary counselling, seemed to increase inequalities 126 .
Effectiveness of prevention interventions
A 2019 Cochrane review of interventions to prevent obesity in children 127 included 153 randomized controlled trials (RCTs), mainly in HICs (12% were from middle-income countries). Of these RCTs, 56% tested interventions in children aged 6–12 years, 24% in children aged 0–5 years, and 20% in adolescents aged 13–18 years. The review showed that diet-only interventions to prevent obesity in children were generally ineffective across all ages. Interventions combining diet and physical activity resulted in modest benefits in children aged 0–12 years but not in adolescents. However, physical activity-only interventions to prevent obesity were effective in school-age children (aged 5–18 years). Whether the interventions were likely to work equitably in all children was investigated in 13 RCTs. These RCTs did not indicate that the strategies increased inequalities, although most of the 13 RCTs included relatively homogeneous groups of children from disadvantaged backgrounds.
The potential for negative unintended consequences of obesity prevention interventions has received much attention 128 . The Cochrane review 127 investigated whether children were harmed by any of the strategies; for example, by having injuries, losing too much weight or developing damaging views about themselves and their weight. Of the few RCTs that did monitor these outcomes, none found any harms in participants.
Intervention levels
Most interventions (58%) of RCTs in the Cochrane review aimed to change individual lifestyle factors via education-based approaches (that is, simply provide information) 129 . In relation to the socioecological model, only 11 RCTs were set in the food and physical activity environment domain, and child care, preschools and schools were the most common targets for interventions. Of note, no RCTs were conducted in a faith-based setting 130 . Table 2 highlights examples of upstream interventions that involve more than simply providing information and their classification on the Nuffield intervention ladder.
Different settings for interventions to prevent childhood obesity, including preschools and schools, primary health care, community settings and national policy, offer different opportunities for reach and effectiveness, and a reduction in inequalities.
Preschools and schools are key settings for public policy interventions for childhood obesity prevention, and mandatory and voluntary food standards and guidance on physical education are in place in many countries. Individual schools are tasked with translating and implementing these standards and guidance for their local context. Successful implementation of a whole-school approach, such as that used in the WHO Nutrition-Friendly Schools Initiative 131 , is a key factor in the effectiveness of interventions. Careful consideration should be given to how school culture can, and needs to, be shifted by working with schools to tailor the approach and manage possible staff capacity issues, and by building relationships within and outside the school gates to enhance sustainability 132 , 133 .
Primary health care offers opportunities for guidance for obesity prevention, especially from early childhood to puberty. Parent-targeted interventions conducted by clinicians in health-care or community settings have the strongest level of evidence for their effectiveness in reducing BMI z -score at age 2 years 134 . These interventions include group programmes, clinic nurse consultations, mobile phone text support or nurse home visiting, and focusing on healthy infant feeding, healthy childhood feeding behaviours and screen time.
A prospective individual participant data meta-analysis of four RCTs involving 2,196 mother–baby dyads, and involving nurse home visiting or group programmes, resulted in a small but significant reduction in BMI in infants in the intervention groups compared with control infants at age 18–24 months 134 . Improvements were also seen in television viewing time, breastfeeding duration and feeding practices. Interventions were more effective in settings with limited provision of maternal and child health services in the community. However, effectiveness diminished by age 5 years without further intervention, highlighting the need for ongoing interventions at each life stage 135 . Evidence exists that short-duration interventions targeting sleep in very early childhood may be more effective than nutrition-targeted interventions in influencing child BMI at age 5 years 136 .
Primary care clinicians can provide anticipatory guidance, as a form of primary prevention, to older children, adolescents and their families, aiming to support healthy weight and weight-related behaviours. Clinical guidelines recommend that clinicians monitor growth regularly, and provide guidance on healthy eating patterns, physical activity, sedentary behaviours and sleep patterns 97 , 100 . Very few paediatric trials have investigated whether this opportunistic screening and advice is effective in obesity prevention 100 . A 2021 review of registered RCTs for the prevention of obesity in infancy found 29 trials 137 , of which most were delivered, or were planned to be delivered, in community health-care settings, such as nurse-led clinics. At the time of publication, 11 trials had reported child weight-related outcomes, two of which showed a small but significant beneficial effect on BMI at age 2 years, and one found significant improvements in the prevalence of obesity but not BMI. Many of the trials showed improvements in practices, such as breastfeeding and screen time.
At the community level, local public policy should be mindful of the geography of the area (such as urban or rural) and population demographics. Adolescents usually have more freedom in food and beverage choices made outside the home than younger children. In addition, physical activity levels usually decline and sedentary behaviours rise during adolescence, particularly in girls 138 , 139 . These behavioural changes offer both opportunities and barriers for those developing community interventions. On a national societal level, public policies for interventions to prevent obesity in children include the control of advertising of foods and beverages high in fat, sugar and/or salt in some countries. Industry and the media, including social media, can have a considerable influence on the food and physical activity behaviours of children 13 , 119 .
Public policy may target interventions at all domains from the individual to the societal level. The main focus of interventions in most national public policies relies on the ability of individuals to make the behavioural changes that are the aim of the intervention (high-agency interventions) at the individual level (downstream interventions). An equal focus on low-agency and upstream interventions is required if a step change in tackling childhood obesity is to be realized 140 , 141 .
COVID-19 and obesity
Early indications in several countries show rising levels of childhood obesity, and an increase in inequalities in childhood obesity during the COVID-19 pandemic 142 . The substantial disruptions in nutrition and lifestyle habits of children during and since the pandemic include social isolation and addiction to screens 143 . Under-nutrition is expected to worsen in poor countries, but obesity rates could increase in middle-income countries and HICs, especially among vulnerable groups, widening the gap in health and social inequalities 143 . Public health approaches at national, regional and local levels should include strategies that not only prevent obesity and under-nutrition, but also reduce health inequalities.
In summary, although most trials of obesity prevention have occurred at the level of the individual, the immediate family, school or community, effective prevention of obesity will require greater investment in upstream, low-agency interventions.
Treatment goals
Treatment should be centred on the individual and stigma-free (Box 1 ) and may aim for a reduction in overweight and improvement in associated comorbidities and health behaviours. Clinical considerations when determining a treatment approach should include age, severity of overweight and the presence of associated complications 144 , 145 .
Box 1 Strategies for minimizing weight stigma in health care 220 , 221 , 222
Minimizing weight bias in the education of health-care professionals
Improved education of health professionals:
pay attention to the implicit and explicit communication of social norms
include coverage of the broader determinants of obesity
include discussion of harms caused by social and cultural norms and messages concerning body weight
provide opportunities to practise non-stigmatizing care throughout education
Provide causal information focusing on the genetic and/or socioenvironmental determinants of weight.
Provide empathy-invoking interventions, emphasizing size acceptance, respect and human dignity.
Provide a weight-inclusive approach, by emphasizing that all individuals, regardless of size, have the right to equal health care.
Addressing health facility infrastructure and processes
Provide appropriately sized chairs, blood pressure cuffs, weight scales, beds, toilets, showers and gowns.
Use non-stigmatizing language in signage, descriptions of clinical services and other documentation.
Providing clinical leadership and using appropriate language within health-care settings
Senior clinicians and managers should role-model supportive and non-biased behaviours towards people with obesity and indicate that they do not tolerate weight-based discrimination in any form.
Staff should identify the language that individuals prefer in referring to obesity.
Use person-first language, for example a ‘person with obesity’ rather than ‘an obese person’.
Treatment guidelines
Clinical guidelines advise that first-line management incorporates a family-based multicomponent approach that addresses dietary, physical activity, sedentary and sleep behaviours 97 , 99 , 109 , 146 . This approach is foundational, with adjunctive therapies, especially pharmacotherapy and bariatric surgery, indicated under specific circumstances, usually in adolescents with more severe obesity 144 , 145 . Guideline recommendations vary greatly among countries and are influenced by current evidence, and functionality and resourcing of local health systems. Hence, availability and feasibility of therapies differs internationally. In usual clinical practice, interventions may have poorer outcomes than is observed in original studies or anticipated in evidence-based guidelines 147 because implementation of guidelines is more challenging in resource-constrained environments 148 . In addition, clinical trials are less likely to include patients with specialized needs, such as children from culturally diverse populations, those living with social disadvantage, children with complex health problems, and those with severe obesity 149 , 150 .
Behavioural interventions
There are marked differences in individual responses to behavioural interventions, and overall weight change outcomes are often modest. In children aged 6–11 years, a 2017 Cochrane review 150 found that mean BMI z -scores were reduced in those involved in behaviour-changing interventions compared with those receiving usual care or no treatment by only 0.06 units (37 trials; 4,019 participants; low-quality evidence) at the latest follow-up (median 10 months after the end of active intervention). In adolescents aged 12–17 years, another 2017 Cochrane review 149 found that multicomponent behavioural interventions resulted in a mean reduction in weight of 3.67 kg (20 trials; 1,993 participants) and reduction in BMI of 1.18 kg/m 2 (28 trials; 2,774 participants). These effects were maintained at the 24-month follow-up. A 2012 systematic review found significant improvements in LDL cholesterol triglycerides and blood pressure up to 1 year from baseline following lifestyle interventions in children and adolescents 151 .
Family-based behavioural interventions are recommended in national level clinical practice guidelines 97 , 100 , 146 , 152 . They are an important element of intensive health behaviour and lifestyle treatments (IHBLTs) 109 . Family-based approaches use behavioural techniques, such as goal setting, parental monitoring or modelling, taught in family sessions or in individual sessions separately to children and care givers, depending on the child’s developmental level. The priority is to encourage the whole family to engage in healthier behaviours that result in dietary improvement, greater physical activity, and less sedentariness. This includes making changes to the family food environment and requires parental monitoring.
Family-based interventions differ in philosophy and implementation from those based on family systems theory and therapy 153 . All are intensive interventions that require multiple contact hours (26 or more) with trained specialists delivered over an extended period of time (6–12 months) 10 . Changing family lifestyle habits is challenging and expensive, and the therapeutic expertise is not widely available. Moving interventions to primary care settings, delivered by trained health coaches, and supplemented by remote contact (for example by phone), will improve access and equity 154 .
Very few interventions use single psychological approaches. Most effective IHBLTs are multicomponent and intensive (many sessions), and include face-to-face contact. There has been interest in motivational interviewing as an approach to delivery 155 . As client-centred counselling, this places the young person at the centre of their behaviour change. Fundamental to motivational interviewing is the practitioner partnership that helps the young person and/or parents to explore ambivalence to change, consolidate commitment to change, and develop a plan based on their own insights and expertise. Evidence reviews generally support the view that motivational interviewing reduces BMI. Longer interventions (>4 months), those that assess and report on intervention fidelity, and those that target both diet and physical activity are most effective 155 , 156 .
More intensive dietary interventions
Some individuals benefit from more intensive interventions 98 , 144 , 157 , 158 , which include very low-energy diets, very low-carbohydrate diets and intermittent energy restriction 159 . These interventions usually aim for weight loss and are only recommended for adolescents who have reached their final height. These diets are not recommended for long periods of time due to challenges in achieving nutritional adequacy 158 , 160 , and lack of long-term safety data 158 , 161 . However, intensive dietary interventions may be considered when conventional treatment is unsuccessful, or when adolescents with comorbidities or severe obesity require rapid or substantial weight loss 98 . A 2019 systematic review of very low-energy diets in children and adolescents found a mean reduction in body weight of −5.3 kg (seven studies) at the latest follow‐up, ranging from 5 to 14.5 months from baseline 161 .
Pharmacological treatment
Until the early 2020s the only drug approved in many jurisdictions for the treatment of obesity in adolescents was orlistat, a gastrointestinal lipase inhibitor resulting in reduced uptake of lipids and, thereby, a reduced total energy intake 162 . However, the modest effect on weight in combination with gastrointestinal adverse effects limit its usefulness overall 163 .
A new generation of drugs has been developed for the treatment of both T2DM and obesity. These drugs are based on gastrointestinal peptides with effects both locally and in the central nervous system. GLP1 is an incretin that reduces appetite and slows gastric motility. The GLP1 receptor agonist liraglutide is approved for the treatment of obesity in those aged 12 years and older both in the USA and Europe 164 , 165 . Liraglutide, delivered subcutaneously daily at a higher dose than used for T2DM resulted in a 5% better BMI reduction than placebo after 12 months 166 . A 2022 trial of semaglutide, another GLP1 receptor agonist, delivered subcutaneously weekly in adolescents demonstrated 16% weight loss after 68 weeks of treatment, with modest adverse events and a low drop-out rate 12 . Tirzepatide, an agonist of both GLP1 and glucose-dependent insulinotropic polypeptide (GIP), is approved by the FDA for the treatment of T2DM in adults 167 . Subcutaneous tirzepatide weekly in adults with obesity resulted in ~20% weight loss over 72 weeks 168 . Of note, GIP alone increases appetite, but the complex receptor–agonist interaction results in downregulation of the GIP receptors 169 , illustrating why slightly modified agonists exert different effects. A study of the use of tirzepatide in adolescents with T2DM has been initiated but results are not expected before 2027 (ref. 170 ). No trials of tirzepatide are currently underway in adolescents with obesity but without T2DM.
Hypothalamic obesity is difficult to treat. Setmelanotide is a MC4R agonist that reduces weight and improves quality of life in most people with LEPR and POMC mutations 71 . In trials of setmelanotide, 8 of 10 participants with POMC deficiency and 5 of 11 with LEPR deficiency had weight loss of at least 10% at ~1 year. The mean percentage change in most hunger score from baseline was −27.1% and −43.7% in those with POMC deficiency and leptin receptor deficiency, respectively 71 .
In the near future, effective new drugs with, hopefully, an acceptable safety profile will be available that will change the way we treat and set goals for paediatric obesity treatment 171 .
Bariatric surgery
Bariatric surgery is the most potent treatment for obesity in adolescents with severe obesity. The types of surgery most frequently used are sleeve gastrectomy and gastric bypass, both of which reduce appetite 172 . Mechanisms of action are complex, involving changes in gastrointestinal hormones, neural signalling, bile acid metabolism and gut microbiota 173 . Sleeve gastrectomy is a more straightforward procedure and the need for vitamin supplementation is lower than with gastric bypass. However, long-term weight loss may be greater after gastric bypass surgery 174 .
Prospective long-term studies demonstrate beneficial effects of both sleeve gastrectomy and gastric bypass on weight loss and comorbidities in adolescents with severe obesity 175 , 176 . In a 5-year follow-up period, in 161 participants in the US TEEN-LABS study who underwent gastric bypass, mean BMI declined from 50 to 37 kg/m 2 (ref. 11 ). In a Swedish prospective study in 81 adolescents who underwent gastric bypass, the mean decrease in BMI at 5 years was 13.1 kg/m 2 (baseline BMI 45.5 kg/m 2 ) compared with a BMI increase of 3.1 kg/m 2 in the control group 176 . Both studies showed marked inter-individual variations. Negative adverse effects, including gastrointestinal problems, vitamin deficits and reduction in lean body mass, are similar in adults and adolescents. Most surgical complications following bariatric surgery in the paediatric population are minor, occurring in the early postoperative time frame, but 8% of patients may have major perioperative complications 177 . Up to one-quarter of patients may require subsequent related procedures within 5 years 109 . However, many adolescents with severe obesity also have social and psychological problems, highlighting the need for routine and long-term monitoring 109 , 178 .
Recommendations for bariatric surgery in adolescents differ considerably among countries, with information on long-term outcomes emerging rapidly. In many countries, bariatric surgery is recommended only from Tanner pubertal stage 3–4 and beyond, and only in children with severe obesity and cardiometabolic comorbidities 177 . The 2023 American Academy of Pediatrics clinical practice guidelines recommend that bariatric surgery be considered in adolescents ≥13 years of age with a BMI of ≥35 kg/m 2 or 120% of the 95th percentile for age and sex, whichever is lower, as well as clinically significant disease, such as T2DM, non-alcoholic fatty liver disease, major orthopaedic complications, obstructive sleep apnoea, the presence of cardiometabolic risk, or depressed quality of life 109 . For those with a BMI of ≥40 kg/m 2 or 140% of the 95th percentile for age and sex, bariatric surgery is indicated regardless of the presence of comorbidities. Potential contraindications to surgery include correctable causes of obesity, pregnancy and ongoing substance use disorder. The guidelines comment that further evaluation, undertaken by multidisciplinary centres that offer bariatric surgery for adolescents, should determine the capacity of the patient and family to understand the risks and benefits of surgery and to adhere to the required lifestyle changes before and after surgery.
Long-term weight outcomes
Few paediatric studies have investigated long-term weight maintenance after the initial, more intensive, weight loss phase. A 2018 systematic review of 11 studies in children and adolescents showed that a diverse range of maintenance interventions, including support via face-to-face psychobehavioural therapies, individual physician consultations, or adjunctive therapeutic contact via newsletters, mobile phone text or e-mail, led to stabilization of BMI z -score compared with control participants, who had increases in BMI z -score 179 . Interventions that are web-based or use mobile devices may be particularly useful in young people 180 .
One concern is weight regain which occurs after bariatric surgery in general 181 but may be more prevalent in adolescents 176 . For example, in a Swedish prospective study, after 5 years, 25–30% of participants fulfilled the definitions of low surgical treatment effectiveness, which was associated with poorer metabolic outcomes 176 . As with adults, prevention of weight regain for most at-risk individuals might be possible with the combination of lifestyle support and pharmacological treatment 182 . Further weight maintenance strategies and long-term outcomes are discussed in the 2023 American Academy of Pediatrics clinical practice guidelines 109 . The appropriate role and timing of other therapies for long-term weight loss maintenance, such as anti-obesity medications, more intensive dietary interventions and bariatric surgery, are areas for future research.
In summary, management of obesity in childhood and adolescence requires intensive interventions. Emerging pharmacological therapies demonstrate greater short-term effectiveness than behavioural interventions; however, long-term outcomes at ≥2 years remain an important area for future research.
Quality of life
Weight bias describes the negative attitudes to, beliefs about and behaviour towards people with obesity 183 . It can lead to stigma causing exclusion, and discrimination in work, school and health care, and contributes to the inequities common in people with obesity 184 . Weight bias also affects social engagement and psychological well-being of children.
Children and adolescents with obesity score lower overall on health-related quality of life (HRQoL) 4 , 5 . In measures that assess domains of functioning, most score lower in physical functioning, physical/general health and psychosocial areas, such as appearance, and social acceptance and functioning. HRQoL is lowest in treatment-seeking children and in those with more extreme obesity 185 . Weight loss interventions generally increase HRQoL independent of the extent of weight loss 186 , especially in the domains most affected. However, changes in weight and HRQoL are often not strongly correlated. This may reflect a lag in the physical and/or psychosocial benefit from weight change, or the extent of change that is needed to drive change in a child’s self-perception.
Similar observations apply to the literature on self-esteem. Global self-worth is reduced in children and adolescents with obesity, as is satisfaction with physical appearance, athletic competence and social acceptance 187 . Data from intensive interventions suggest the psychological benefit of weight loss may be as dependent on some feature of the treatment environment or supportive social network as the weight loss itself 188 . This may include the daily company of others with obesity, making new friendships, and experienced improvements in newly prioritized competences.
There is a bidirectional relationship between HRQoL and obesity 189 , something also accepted in the relationship with mood disorder. Obesity increases the risk of depression and vice versa, albeit over a longer period of time and which may only become apparent in adulthood 190 . Obesity also presents an increased risk of anxiety 191 .
Structured and professionally delivered weight management interventions ameliorate mood disorder symptoms 192 and improve self-esteem 193 . Regular and extended support are important components beyond losing weight. Such interventions do not increase the risk of eating disorders 194 . This is despite a recognition that binge eating disorder is present in up to 5% of adolescents with overweight or obesity 195 . They are five times more likely to have binge eating symptoms than those with average weight. Importantly, adolescents who do not have access to professionally delivered weight management may be more likely to engage in self-directed dieting, which is implicated in eating disorder development 196 .
The literature linking childhood obesity with either attention deficit hyperactivity disorder or autism spectrum disorder is complex and the relationship is uncertain. The association seems to be clearer in adults but the mechanisms and their causal directions remain unclear 109 , 197 . Young children with obesity, especially boys, are more likely to be parent-rated as having behavioural problems 198 . This may be a response to the behaviour of others rather than reflect clinical diagnoses such as attention deficit hyperactivity disorder or autism spectrum disorder. Conduct and peer relationship problems co-occur in children, regardless of their weight.
Children with obesity experience more social rejection. They receive fewer friendship nominations and more peer rejections, most pronounced in those with severe obesity 199 . This continues through adolescence and beyond. Children with obesity are more likely to report being victimized 200 . Younger children may respond by being perpetrators themselves. While it is assumed that children are victimized because of their weight, very few studies have looked at the nature or reason behind victimization. A substantial proportion of children with obesity fail to identify themselves as being fat-teased 187 . Although the stigma associated with obesity should be anticipated in children, especially in those most overweight, it would be inappropriate to see all as victims. A better understanding of children’s resilience is needed.
Many gaps remain in basic, translational and clinical research in child and adolescent obesity. The mechanisms (genetic, epigenetic, environmental and social) behind the overwhelming association between parental obesity and child and adolescent obesity are still unclear given the paradoxically weak association in BMI between adopted children and their parents in combination with the modest effect size of known genetic loci associated with obesity 201 .
Early manifestation of extreme obesity in childhood suggests a strong biological basis for disturbances of homeostatic weight regulation. Deep genotyping (including next-generation sequencing) and epigenetic analyses in these patients will reveal new genetic causes and causal pathways as a basis for the development of mechanism-based treatments. Future work aiming to understand the mechanisms underlying the development of childhood obesity should consider the complex biopsychosocial interactions and take a systems approach to understanding causal pathways leading to childhood obesity to contribute to evidence-based prevention and treatment strategies.
Long-term outcome data to better determine the risks of eating disorders are required. Although symptoms improve during obesity treatment in most adolescents, screening and monitoring for disordered eating is recommended in those presenting for treatment 202 and effective tools for use in clinical practice are required. A limited number of tools are validated to identify binge eating disorder in youth with obesity 203 but further research is needed to screen appropriately for the full spectrum of eating disorder diagnoses in obesity treatment seeking youth 203 . Recent reviews provide additional detail regarding eating disorder risk in child and adolescent obesity 117 , 202 , 204 .
Most studies of paediatric obesity treatment have been undertaken in HICs and predominantly middle-class populations. However, research is needed to determine which strategies are best suited for those in LMICs and low-resource settings, for priority population groups including indigenous peoples, migrant populations and those living with social disadvantage, and for children with neurobehavioural and psychiatric disorders. We currently have a limited understanding of how best to target treatment pathways for different levels of genetic risk, age, developmental level, obesity severity, and cardiometabolic and psychological risk. Current outcomes for behavioural interventions are relatively modest and improved treatment outcomes are needed to address the potentially severe long-term health outcomes of paediatric obesity. Studies also need to include longer follow-up periods after an intervention, record all adverse events, incorporate cost-effectiveness analyses and have improved process evaluation.
Other areas in need of research include the role of new anti-obesity medications especially in adolescents, long-term outcomes following bariatric surgery and implementation of digital support systems to optimize outcomes and reduce costs of behavioural change interventions 205 . We must also better understand and tackle the barriers to implementation of treatment in real-life clinical settings, including the role of training of health professionals. Importantly, treatment studies of all kinds must engage people with lived experience — adolescents, parents and families — to understand what outcomes and elements of treatment are most valued.
Obesity prevention is challenging because it requires a multilevel, multisectoral approach that addresses inequity, involves many stakeholders and addresses both the upstream and the downstream factors influencing obesity risk. Some evidence exists of effectiveness of prevention interventions operating at the level of the child, family and school, but the very poor progress overall in modifying obesity prevalence globally highlights many areas in need of research and evidence implementation. Studies are needed especially in LMICs, particularly in the context of the nutrition transition and the double burden of malnutrition. A focus on intergenerational research, rather than the age-based focus of current work, is also needed. Systems research approaches should be used, addressing the broader food and physical activity environments, and links to climate change 206 . In all studies, strategies are needed that enable co-production with relevant communities, long-term follow-up, process evaluation and cost-effectiveness analyses. In the next few years, research and practice priorities must include a focus on intervention strategies in the earliest phases of life, including during pregnancy. The effects of COVID-19 and cost of living crises in many countries are leading to widening health inequalities 207 and this will further challenge obesity prevention interventions. Available resourcing for prevention interventions may become further constrained, requiring innovative solutions across agendas, with clear identification of co-benefits. For example, public health interventions for other diseases, such as dental caries or depression, or other societal concerns, such as urban congestion or climate change, may also act as obesity prevention strategies. Ultimately, to implement obesity prevention, societal changes are needed in terms of urban planning, social structures and health-care access.
Future high-quality paediatric obesity research can be enabled through strategies that support data sharing, which avoids research waste and bias, and enables new research questions to be addressed. Such approaches require leadership, careful engagement of multiple research teams, and resourcing. Four national or regional level paediatric weight registries exist 208 , 209 , 210 , 211 , which are all based in North America or Europe. Such registries should be established in other countries, especially in low-resource settings, even if challenging 208 . Another data-sharing approach is through individual participant data meta-analyses of intervention trials, which can include prospectively collected data 212 and are quite distinct from systematic reviews of aggregate data. Two recent examples are the Transforming Obesity Prevention in Childhood (TOPCHILD) Collaboration, which includes early interventions to prevent obesity in the first 2 years of life 213 , and the Eating Disorders in Weight-Related Therapy (EDIT) Collaboration, which aims to identify characteristics of individuals or trials that increase or protect against eating disorder risk following obesity treatment 214 . Formal data linkage studies, especially those joining up routine administrative datasets, enable longer-term and broader outcome measures to be assessed than is possible with standard clinical or public health intervention studies.
Collaborative research will also be enhanced through the use of agreed core outcome sets, supporting data harmonization. The Edmonton Obesity Staging System – Paediatric 215 is one option for paediatric obesity treatment. A core outcome set for early intervention trials to prevent obesity in childhood (COS-EPOCH) has been recently established 216 . These efforts incorporate a balance between wanting and needing to share data and adhering to privacy protection regulations. Objective end points are ideal, including directly measured physical activity and body composition.
Collaborative efforts and a systems approach are paramount to understand, prevent and manage child and adolescent obesity. Research funding and health policies should focus on feasible, effective and equitable interventions.
NCD Risk Factor Collaboration. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet https://doi.org/10.1016/S0140-6736(17)32129-3 (2017).
Article Google Scholar
Popkin, B. M., Corvalan, C. & Grummer-Strawn, L. M. Dynamics of the double burden of malnutrition and the changing nutrition reality. Lancet 395 , 65–74 (2020).
Article PubMed Google Scholar
Kompaniyets, L. et al. Underlying medical conditions associated with severe COVID-19 illness among children. JAMA Netw. Open 4 , e2111182 (2021).
Article PubMed PubMed Central Google Scholar
Griffiths, L. J., Parsons, T. J. & Hill, A. J. Self‐esteem and quality of life in obese children and adolescents: a systematic review. Int. J. Pediatr. Obes. 5 , 282–304 (2010).
Buttitta, M., Iliescu, C., Rousseau, A. & Guerrien, A. Quality of life in overweight and obese children and adolescents: a literature review. Qual. Life Res. 23 , 1117–1139 (2014).
Hayes, A. et al. Early childhood obesity: association with healthcare expenditure in Australia. Obesity 24 , 1752–1758 (2016).
Marcus, C., Danielsson, P. & Hagman, E. Pediatric obesity – long-term consequences and effect of weight loss. J. Intern. Med. 292 , 870–891 (2022).
Berthoud, H. R., Morrison, C. D. & Münzberg, H. The obesity epidemic in the face of homeostatic body weight regulation: what went wrong and how can it be fixed? Physiol. Behav. 222 , 112959 (2020).
Article CAS PubMed PubMed Central Google Scholar
World Health Organization. Report of the commission on ending childhood obesity. WHO https://www.who.int/publications/i/item/9789241510066 (2016). This report from the WHO on approaches to childhood and adolescent obesity has six main recommendations for governments, covering food and physical activity, age-based settings and provision of weight management for those with obesity.
O’Connor, E. A. et al. Screening for obesity and intervention for weight management in children and adolescents: evidence report and systematic review for the US Preventive Services Task Force. JAMA 317 , 2427–2444 (2017).
Inge, T. H. et al. Five-year outcomes of gastric bypass in adolescents as compared with adults. N. Engl. J. Med. 380 , 2136–2145 (2019).
Weghuber, D. et al. Once-weekly semaglutide in adolescents with obesity. N. Engl. J. Med. https://doi.org/10.1056/NEJMoa2208601 (2022). To our knowledge, the first RCT of semaglutide 2.4 mg, administered weekly by subcutaneous injection, in adolescents with obesity.
World Health Organization. Report of the Commission on Ending Childhood Obesity: Implementation Plan: Executive Summary (WHO, 2017).
Hillier-Brown, F. C. et al. A systematic review of the effectiveness of individual, community and societal level interventions at reducing socioeconomic inequalities in obesity amongst children. BMC Public Health 14 , 834 (2014).
World Health Organization. Obesity. WHO https://www.who.int/health-topics/obesity#tab=tab_1 (2023).
Mei, Z. et al. Validity of body mass index compared with other body-composition screening indexes for the assessment of body fatness in children and adolescents. Am. J. Clin. Nutr. 75 , 978–985 (2002).
Article CAS PubMed Google Scholar
World Health Organization. Child growth standards. WHO https://www.who.int/tools/child-growth-standards/standards (2006).
World Health Organization. Growth reference data for 5–19 years. WHO https://www.who.int/tools/growth-reference-data-for-5to19-years (2007).
National Center for Health Statistics. CDC growth charts. Centers for Disease Control and Prevention http://www.cdc.gov/growthcharts/ (2022).
Cole, T. J., Bellizzi, M. C., Flegal, K. M. & Dietz, W. H. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ 320 , 1240 (2000).
Di Cesare, M. et al. The epidemiological burden of obesity in childhood: a worldwide epidemic requiring urgent action. BMC Med. 17 , 212 (2019).
Swinburn, B., Egger, G. & Raza, F. Dissecting obesogenic environments: the development and application of a framework for identifying and prioritizing environmental interventions for obesity. Prev. Med. 29 , 563–570 (1999).
Ford, N. D., Patel, S. A. & Narayan, K. V. Obesity in low-and middle-income countries: burden, drivers, and emerging challenges. Annu. Rev. Public Health 38 , 145–164 (2017).
Shah, B., Tombeau Cost, K., Fuller, A., Birken, C. S. & Anderson, L. N. Sex and gender differences in childhood obesity: contributing to the research agenda. BMJ Nutr. Prev. Health 3 , 387–390 (2020).
Public Health England. Research and analysis: differences in child obesity by ethnic group. GOV.UK https://www.gov.uk/government/publications/differences-in-child-obesity-by-ethnic-group/differences-in-child-obesity-by-ethnic-group#data (2019).
Cole, T. J. & Lobstein, T. Extended international (IOTF) body mass index cut‐offs for thinness, overweight and obesity. Pediatr. Obes. 7 , 284–294 (2012).
Kelly, A. S. et al. Severe obesity in children and adolescents: identification, associated health risks, and treatment approaches: a scientific statement from the American Heart Association. Circulation 128 , 1689–1712 (2013).
Garnett, S. P., Baur, L. A., Jones, A. M. & Hardy, L. L. Trends in the prevalence of morbid and severe obesity in Australian children aged 7–15 years, 1985-2012. PLoS ONE 11 , e0154879 (2016).
Spinelli, A. et al. Prevalence of severe obesity among primary school children in 21 European countries. Obes. Facts 12 , 244–258 (2019).
Twig, G. et al. Body-Mass Index in 2.3 million adolescents and cardiovascular death in adulthood. N. Engl. J. Med. 374 , 2430–2440 (2016).
González-Muniesa, P. et al. Obesity. Nat. Rev. Dis. Primers 3 , 17034 (2017).
Geserick, M. et al. Acceleration of BMI in early childhood and risk of sustained obesity. N. Engl. J. Med. 379 , 1303–1312 (2018).
Larqué, E. et al. From conception to infancy – early risk factors for childhood obesity. Nat. Rev. Endocrinol. 15 , 456–478 (2019).
Barker, D. J. Fetal origins of coronary heart disease. Br. Med. J. 311 , 171–174 (1995).
Article CAS Google Scholar
Gluckman, P. D., Hanson, M. A., Cooper, C. & Thornburg, K. L. Effect of in utero and early-life conditions on adult health and disease. N. Engl. J. Med. 359 , 61–73 (2008).
Philips, E. M. et al. Changes in parental smoking during pregnancy and risks of adverse birth outcomes and childhood overweight in Europe and North America: an individual participant data meta-analysis of 229,000 singleton births. PLoS Med. 17 , e1003182 (2020).
Voerman, E. et al. Maternal body mass index, gestational weight gain, and the risk of overweight and obesity across childhood: an individual participant data meta-analysis. PLoS Med. 16 , e1002744 (2019). Individual participant data meta-analysis of >160,000 mothers and their children on the associations of maternal BMI and gestational weight gain and childhood overweight or obesity.
McIntyre, H. D. et al. Gestational diabetes mellitus. Nat. Rev. Dis. Primers 5 , 47 (2019).
Oken, E. & Gillman, M. W. Fetal origins of obesity. Obes. Res. 11 , 496–506 (2003).
Hughes, A. R., Sherriff, A., Ness, A. R. & Reilly, J. J. Timing of adiposity rebound and adiposity in adolescence. Pediatrics 134 , e1354–e1361 (2014).
Rolland-Cachera, M. F. et al. Tracking the development of adiposity from one month of age to adulthood. Ann. Hum. Biol. 14 , 219–229 (1987).
Koletzko, B. et al. Prevention of childhood obesity: a position paper of the Global Federation of International Societies of Paediatric Gastroenterology, Hepatology and Nutrition (FISPGHAN). J. Pediatr. Gastroenterol. Nutr. 70 , 702–710 (2020).
Weber, M. et al. Lower protein content in infant formula reduces BMI and obesity risk at school age: follow-up of a randomized trial. Am. J. Clin. Nutr. 99 , 1041–1051 (2014).
Cope, M. B. & Allison, D. B. Critical review of the World Health Organization’s (WHO) 2007 report on ‘evidence of the long‐term effects of breastfeeding: systematic reviews and meta‐analysis’ with respect to obesity. Obes. Rev. 9 , 594–605 (2008).
Totzauer, M. et al. Different protein intake in the first year and its effects on adiposity rebound and obesity throughout childhood: 11 years follow‐up of a randomized controlled trial. Pediatr. Obes. 17 , e12961 (2022).
Deren, K. et al. Consumption of sugar-sweetened beverages in paediatric age: a position paper of the European academy of paediatrics and the European Childhood Obesity Group. Ann. Nutr. Metab. 74 , 296–302 (2019).
Felső, R., Lohner, S., Hollódy, K., Erhardt, É. & Molnár, D. Relationship between sleep duration and childhood obesity: systematic review including the potential underlying mechanisms. Nutr. Metab. Cardiovasc. Dis. 27 , 751–761 (2017).
Farooq, A. et al. Longitudinal changes in moderate‐to‐vigorous‐intensity physical activity in children and adolescents: a systematic review and meta‐analysis. Obes. Rev. 21 , e12953 (2020).
Mahumud, R. A. et al. Association of dietary intake, physical activity, and sedentary behaviours with overweight and obesity among 282,213 adolescents in 89 low and middle income to high-income countries. Int. J. Obes. 45 , 2404–2418 (2021).
Ballon, M. et al. Socioeconomic inequalities in weight, height and body mass index from birth to 5 years. Int. J. Obes. 42 , 1671–1679 (2018).
Buoncristiano, M. et al. Socioeconomic inequalities in overweight and obesity among 6- to 9-year-old children in 24 countries from the World Health Organization European region. Obes. Rev. 22 , e13213 (2021).
Jiwani, S. S. et al. The shift of obesity burden by socioeconomic status between 1998 and 2017 in Latin America and the Caribbean: a cross-sectional series study. Lancet Glob. Health 7 , e1644–e1654 (2019).
Monteiro, C. A., Conde, W. L., Lu, B. & Popkin, B. M. Obesity and inequities in health in the developing world. Int. J. Obes. 28 , 1181–1186 (2004).
Guo, S. S. & Chumlea, W. C. Tracking of body mass index in children in relation to overweight in adulthood. Am. J. Clin. Nutr. 70 , 145S–148S (1999).
Aarestrup, J. et al. Birthweight, childhood overweight, height and growth and adult cancer risks: a review of studies using the Copenhagen School Health Records Register. Int. J. Obes. 44 , 1546–1560 (2020).
Eslam, M. et al. Defining paediatric metabolic (dysfunction)-associated fatty liver disease: an international expert consensus statement. Lancet Gastroenterol. Hepatol. 6 , 864–873 (2021).
Daniels, S. R. et al. Overweight in children and adolescents: pathophysiology, consequences, prevention, and treatment. Circulation 111 , 1999–2012 (2005).
Cioana, M. et al. The prevalence of obesity among children with type 2 diabetes: a systematic review and meta-analysis. JAMA Netw. Open 5 , e2247186 (2022).
Gepstein, V. & Weiss, R. Obesity as the main risk factor for metabolic syndrome in children. Front. Endocrinol. 10 , 568 (2019).
Kuvat, N., Tanriverdi, H. & Armutcu, F. The relationship between obstructive sleep apnea syndrome and obesity: a new perspective on the pathogenesis in terms of organ crosstalk. Clin. Respir. J. 14 , 595–604 (2020).
Baker, J. L., Olsen, L. W. & Sorensen, T. I. Childhood body-mass index and the risk of coronary heart disease in adulthood. N. Engl. J. Med. 357 , 2329–2337 (2007).
Bjerregaard, L. G. et al. Change in overweight from childhood to early adulthood and risk of type 2 diabetes. N. Engl. J. Med. 378 , 1302–1312 (2018).
Kelsey, M. M., Zaepfel, A., Bjornstad, P. & Nadeau, K. J. Age-related consequences of childhood obesity. Gerontology 60 , 222–228 (2014).
Sharma, V. et al. A systematic review and meta-analysis estimating the population prevalence of comorbidities in children and adolescents aged 5 to 18 years. Obes. Rev. 20 , 1341–1349 (2019).
Lobstein, T. & Jackson-Leach, R. Planning for the worst: estimates of obesity and comorbidities in school-age children in 2025. Pediatr. Obes. 11 , 321–325 (2016).
Berthoud, H. R., Münzberg, H. & Morrison, C. D. Blaming the brain for obesity: integration of hedonic and homeostatic mechanisms. Gastroenterology 152 , 1728–1738 (2017).
Devoto, F. et al. Hungry brains: a meta-analytical review of brain activation imaging studies on food perception and appetite in obese individuals. Neurosci. Biobehav. Rev. 94 , 271–285 (2018).
Blum, W. F., Englaro, P., Attanasio, A. M., Kiess, W. & Rascher, W. Human and clinical perspectives on leptin. Proc. Nutr. Soc. 57 , 477–485 (1998).
Friedman, J. M. Leptin and the endocrine control of energy balance. Nat. Metab. 1 , 754–764 (2019).
Kühnen, P. et al. Proopiomelanocortin deficiency treated with a melanocortin-4 receptor agonist. N. Engl. J. Med. 375 , 240–246 (2016).
Clément, K. et al. Efficacy and safety of setmelanotide, an MC4R agonist, in individuals with severe obesity due to LEPR or POMC deficiency: single-arm, open-label, multicentre, phase 3 trials. Lancet Diabetes Endocrinol. 8 , 960–970 (2020).
Rosen, E. D. & Spiegelman, B. M. What we talk about when we talk about fat. Cell 156 , 20–44 (2014).
Fischer-Posovszky, P., Roos, J., Zoller, V. & Wabitsch, M. in Pediatric Obesity: Etiology, Pathogenesis and Treatment (ed. Freemark, M. S.) 81–93 (Springer, 2018).
Hammarstedt, A., Gogg, S., Hedjazifar, S., Nerstedt, A. & Smith, U. Impaired adipogenesis and dysfunctional adipose tissue in human hypertrophic obesity. Physiol. Rev. 98 , 1911–1941 (2018).
Silventoinen, K. et al. Genetic and environmental effects on body mass index from infancy to the onset of adulthood: an individual-based pooled analysis of 45 twin cohorts participating in the collaborative project of development of anthropometrical measures in twins (CODATwins) study. Am. J. Clin. Nutr. 104 , 371–379 (2016).
Silventoinen, K. et al. Differences in genetic and environmental variation in adult BMI by sex, age, time period, and region: an individual-based pooled analysis of 40 twin cohorts. Am. J. Clin. Nutr. 106 , 457–466 (2017).
Yengo, L. et al. Meta-analysis of genome-wide association studies for height and body mass index in approximately 700000 individuals of European ancestry. Hum. Mol. Genet. 27 , 3641–3649 (2018).
Vogelezang, S. et al. Novel loci for childhood body mass index and shared heritability with adult cardiometabolic traits. PLoS Genet. 16 , e1008718 (2020).
Bradfield, J. P. et al. A trans-ancestral meta-analysis of genome-wide association studies reveals loci associated with childhood obesity. Hum. Mol. Genet. 28 , 3327–3338 (2019). To our knowledge, currently the largest genome-wide association study meta-analysis on childhood obesity in >13,000 individuals with obesity and >15,500 controls.
Couto Alves, A. et al. GWAS on longitudinal growth traits reveals different genetic factors influencing infant, child, and adult BMI. Sci. Adv. 5 , eaaw3095 (2019).
Ding, X. et al. Genome-wide screen of DNA methylation identifies novel markers in childhood obesity. Gene 566 , 74–83 (2015).
Huang, R. C. et al. Genome-wide methylation analysis identifies differentially methylated CpG loci associated with severe obesity in childhood. Epigenetics 10 , 995–1005 (2015).
Rzehak, P. et al. DNA-methylation and body composition in preschool children: epigenome-wide-analysis in the European Childhood Obesity Project (CHOP)-Study. Sci. Rep. 7 , 14349 (2017).
Alfano, R. et al. Perspectives and challenges of epigenetic determinants of childhood obesity: a systematic review. Obes. Rev. 23 , e13389 (2022).
Vehmeijer, F. O. L. et al. DNA methylation and body mass index from birth to adolescence: meta-analyses of epigenome-wide association studies. Genome Med. 12 , 105 (2020). Meta-analysis of epigenome-wide association studies of childhood BMI in >4,000 children.
Richmond, R. C. et al. DNA methylation and BMI: investigating identified methylation sites at HIF3A in a causal framework. Diabetes 65 , 1231–1244 (2016).
Wahl, S. et al. Epigenome-wide association study of body mass index, and the adverse outcomes of adiposity. Nature 541 , 81–86 (2017).
Kivimäki, M. et al. Substantial intergenerational increases in body mass index are not explained by the fetal overnutrition hypothesis: the Cardiovascular Risk in Young Finns Study. Am. J. Clin. Nutr. 86 , 1509–1514 (2007).
Whitaker, R. C., Wright, J. A., Pepe, M. S., Seidel, K. D. & Dietz, W. H. Predicting obesity in young adulthood from childhood and parental obesity. N. Engl. J. Med. 337 , 869–873 (1997).
Davey Smith, G., Steer, C., Leary, S. & Ness, A. Is there an intrauterine influence on obesity? Evidence from parent child associations in the Avon Longitudinal Study of Parents and Children (ALSPAC). Arch. Dis. Child. 92 , 876–880 (2007).
Fleten, C. et al. Parent-offspring body mass index associations in the Norwegian Mother and Child Cohort Study: a family-based approach to studying the role of the intrauterine environment in childhood adiposity. Am. J. Epidemiol. 176 , 83–92 (2012).
Gaillard, R. et al. Childhood cardiometabolic outcomes of maternal obesity during pregnancy: the Generation R Study. Hypertension 63 , 683–691 (2014).
Lawlor, D. A. et al. Exploring the developmental overnutrition hypothesis using parental-offspring associations and FTO as an instrumental variable. PLoS Med. 5 , e33 (2008).
Patro, B. et al. Maternal and paternal body mass index and offspring obesity: a systematic review. Ann. Nutr. Metab. 63 , 32–41 (2013).
Sorensen, T. et al. Comparison of associations of maternal peri-pregnancy and paternal anthropometrics with child anthropometrics from birth through age 7 y assessed in the Danish National Birth Cohort. Am. J. Clin. Nutr. 104 , 389–396 (2016).
Styne, D. M. et al. Pediatric obesity – assessment, treatment, and prevention: an Endocrine Society Clinical Practice guideline. J. Clin. Endocrinol. Metab. 102 , 709–757 (2017).
National Institute for Health and Care Excellence. Obesity: identification, assessment and managenent: clinical guideline [CG189]. NICE https://www.nice.org.uk/guidance/cg189 (2022). A high quality clinical practice guideline for obesity management.
Barlow, S. E. Expert Committee Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics 120 (Suppl. 4), S164–S192 (2007).
Canadian Task Force on Preventive Health Care. Recommendations for growth monitoring, and prevention and management of overweight and obesity in children and youth in primary care. Can. Med. Assoc. J. 187 , 411–421 (2015).
US Preventive Services Task Force. Screening for obesity in children and adolescents: US Preventive Services Task Force recommendation statement. JAMA 317 , 2417–2426 (2017).
McConnell-Nzunga, J. et al. Classification of obesity varies between body mass index and direct measures of body fat in boys and girls of Asian and European ancestry. Meas. Phys. Educ. Exerc. Sci. 22 , 154–166 (2018).
Reinehr, T. et al. Definable somatic disorders in overweight children and adolescents. J. Pediatr. 150 , 618–622.e5 (2007).
Reinehr, T. Thyroid function in the nutritionally obese child and adolescent. Curr. Opin. Pediatr. 23 , 415–420 (2011).
Kohlsdorf, K. et al. Early childhood BMI trajectories in monogenic obesity due to leptin, leptin receptor, and melanocortin 4 receptor deficiency. Int. J. Obes. 42 , 1602–1609 (2018).
Armstrong, S. et al. Physical examination findings among children and adolescents with obesity: an evidence-based review. Pediatrics 137 , e20151766 (2016).
Reinehr, T. & Roth, C. L. Is there a causal relationship between obesity and puberty? Lancet Child Adolesc. Health 3 , 44–54 (2019).
Garnett, S. P., Baur, L. A. & Cowell, C. T. Waist-to-height ratio: a simple option for determining excess central adiposity in young people. Int. J. Obes. 32 , 1028–1030 (2008).
Maffeis, C., Banzato, C., Talamini, G. & Obesity Study Group of the Italian Society of Pediatric Endocrinology and Diabetology. Waist-to-height ratio, a useful index to identify high metabolic risk in overweight children. J. Pediatr. 152 , 207–213.e2 (2008).
Hampl, S. E. et al. Clinical practice guideline for the evaluation and treatment of children and adolescents with obesity. Pediatrics 151 , e2022060640 (2023). A new, comprehensive clinical practice guideline outlining current recommendations on assessment and treatment of children and adolescents with obesity.
Reinehr, T. et al. Comparison of cardiovascular risk factors between children and adolescents with classes III and IV obesity: findings from the APV cohort. Int. J. Obes. 45 , 1061–1073 (2021).
Reinehr, T. Metabolic syndrome in children and adolescents: a critical approach considering the interaction between pubertal stage and insulin resistance. Curr. Diabetes Rep. 16 , 8 (2016).
Zeitler, P. et al. ISPAD Clinical Practice Consensus Guidelines 2018: type 2 diabetes mellitus in youth. Pediatr. Diabetes 19 , 28–46 (2018).
Ibáñez, L. et al. An International Consortium update: pathophysiology, diagnosis, and treatment of polycystic ovarian syndrome in adolescence. Horm. Res. Paediatr. 88 , 371–395 (2017).
Brockmann, P. E., Schaefer, C., Poets, A., Poets, C. F. & Urschitz, M. S. Diagnosis of obstructive sleep apnea in children: a systematic review. Sleep Med. Rev. 17 , 331–340 (2013).
Taylor, E. D. et al. Orthopedic complications of overweight in children and adolescents. Pediatrics 117 , 2167–2174 (2006).
Winck, A. D. et al. Effects of obesity on lung volume and capacity in children and adolescents: a systematic review. Rev. Paul. Pediatr. 34 , 510–517 (2016).
PubMed PubMed Central Google Scholar
Jebeile, H., Lister, N., Baur, L., Garnett, S. & Paxton, S. J. Eating disorder risk in adolescents with obesity. Obes. Rev. 22 , e13173 (2021).
Quek, Y. H., Tam, W. W. S., Zhang, M. W. B. & Ho, R. C. M. Exploring the association between childhood and adolescent obesity and depression: a meta-analysis. Obes. Rev. 18 , 742–754 (2017).
World Health Organization. Consideration of the Evidence on Childhood Obesity for the Commission on Ending Childhood Obesity . Report of the Ad Hoc Working Group on Science and Evidence for Ending Childhood Obesity (WHO, 2016).
Pickett, K. et al. The Child of the North: building a fairer future after COVID-19. The Northern Health Science Alliance and N8 Research Partnership https://www.thenhsa.co.uk/app/uploads/2022/01/Child-of-the-North-Report-FINAL-1.pdf (2021).
Bronfenbrenner, U. Toward an experimental ecology of human development. Am. Psychol. 32 , 513–531 (1977).
Nuffield Council on Bioethics. Public Health: Ethical Issues (Nuffield Council on Bioethics, 2007).
Lorenc, T., Petticrew, M., Welch, V. & Tugwell, P. What types of interventions generate inequalities? Evidence from systematic reviews. J. Epidemiol. Community Health 67 , 190–193 (2013).
Adams, J., Mytton, O., White, M. & Monsivais, P. Why are some population interventions for diet and obesity more equitable and effective than others? The role of individual agency. PLoS Med. 13 , e1001990 (2016).
Backholer, K. et al. A framework for evaluating the impact of obesity prevention strategies on socioeconomic inequalities in weight. Am. J. Public Health 104 , e43–e50 (2014).
McGill, R. et al. Are interventions to promote healthy eating equally effective for all? Systematic review of socioeconomic inequalities in impact. BMC Public Health 15 , 457 (2015).
Brown, T. et al. Interventions for preventing obesity in children. Cochrane Database Syst. Rev. 7 , Cd001871 (2019). A Cochrane review involving 153 RCTs of diet and/or physical activity interventions to prevent obesity in children and adolescents, highlighting varying effectiveness of interventions in different age groups.
PubMed Google Scholar
Le, L. K.-D. et al. Prevention of high body mass index and eating disorders: a systematic review and meta-analysis. Eat. Weight Disord. 27 , 2989–3003 (2022).
Nobles, J., Summerbell, C., Brown, T., Jago, R. & Moore, T. A secondary analysis of the childhood obesity prevention Cochrane Review through a wider determinants of health lens: implications for research funders, researchers, policymakers and practitioners. Int. J. Behav. Nutr. Phys. Act. 18 , 22 (2021).
Rai, K. K., Dogra, S. A., Barber, S., Adab, P. & Summerbell, C. A scoping review and systematic mapping of health promotion interventions associated with obesity in Islamic religious settings in the UK. Obes. Rev. 20 , 1231–1261 (2019).
World Health Organization. Nutrition Action in Schools: A Review of Evidence Related to the Nutrition-Friendly Schools Initiative (WHO, 2021).
Daly-Smith, A. et al. Using a multi-stakeholder experience-based design process to co-develop the Creating Active Schools Framework. Int. J. Behav. Nutr. Phys. Act. 17 , 13 (2020).
Tibbitts, B. et al. Considerations for individual-level versus whole-school physical activity interventions: stakeholder perspectives. Int. J. Environ. Res. Public Health https://doi.org/10.3390/ijerph18147628 (2021).
Askie, L. M. et al. Interventions commenced by early infancy to prevent childhood obesity-The EPOCH Collaboration: an individual participant data prospective meta-analysis of four randomized controlled trials. Pediatr. Obes. 15 , e12618 (2020). To our knowledge, the first prospective individual participant data meta-analysis showing that interventions commencing in late pregnancy or very early childhood are associated with healthier BMI z -score at age 18–24 months.
Seidler, A. L. et al. Examining the sustainability of effects of early childhood obesity prevention interventions: follow-up of the EPOCH individual participant data prospective meta-analysis. Pediatr. Obes. 17 , e12919 (2022).
Taylor, R. W. et al. Sleep, nutrition, and physical activity interventions to prevent obesity in infancy: follow-up of the prevention of overweight in infancy (POI) randomized controlled trial at ages 3.5 and 5 y. Am. J. Clin. Nutr. 108 , 228–236 (2018).
Mihrshahi, S. et al. A review of registered randomized controlled trials for the prevention of obesity in infancy. Int. J. Environ. Res. Public Health 18 , 2444 (2021).
Farooq, M. A. et al. Timing of the decline in physical activity in childhood and adolescence: Gateshead Millennium Cohort Study. Br. J. Sports Med. 52 , 1002–1006 (2018).
van Sluijs, E. M. F. et al. Physical activity behaviours in adolescence: current evidence and opportunities for intervention. Lancet 398 , 429–442 (2021).
Griffin, N. et al. A critique of the English national policy from a social determinants of health perspective using a realist and problem representation approach: the ‘Childhood Obesity: a plan for action’ (2016, 2018, 2019). BMC Public Health 21 , 2284 (2021).
Knai, C., Lobstein, T., Petticrew, M., Rutter, H. & Savona, N. England’s childhood obesity action plan II. Br. Med. J. 362 , k3098 (2018).
World Health Organization. WHO European Regional Obesity Report 2022 (WHO, 2022).
Zemrani, B., Gehri, M., Masserey, E., Knob, C. & Pellaton, R. A hidden side of the COVID-19 pandemic in children: the double burden of undernutrition and overnutrition. Int. J. Equity Health 20 , 44 (2021).
Alman, K. L. et al. Dietetic management of obesity and severe obesity in children and adolescents: a scoping review of guidelines. Obes. Rev. https://doi.org/10.1111/obr.13132 (2020).
Pfeiffle, S. et al. Current recommendations for nutritional management of overweight and obesity in children and adolescents: a structured framework. Nutrients https://doi.org/10.3390/nu11020362 (2019).
Scottish Intercollegiate Guidelines Network. Management of obesity. A National Clinical Guideline . SIGN 115 (SIGN, 2010).
Reinehr, T. et al. Two-year follow-up in 21,784 overweight children and adolescents with lifestyle intervention. Obesity 17 , 1196–1199 (2009).
Ells, L. J. et al. Interventions for treating children and adolescents with overweight and obesity: an overview of Cochrane reviews. Int. J. Obes. 42 , 1823–1833 (2018).
Al‐Khudairy, L. et al. Diet, physical activity and behavioural interventions for the treatment of overweight or obese adolescents aged 12 to 17 years. Cochrane Database Syst. Rev. 6 , CD012691 (2017). One of three Cochrane reviews looking at lifestyle treatment of paediatric obesity, in this case in adolescents, which identified 44 completed trials, finding low quality evidence of improvements in BMI and moderate quality evidence of improvements in weight.
Mead, E. et al. Diet, physical activity and behavioural interventions for the treatment of overweight or obese children from the age of 6 to 11 years. Cochrane Database Syst. Rev. 6 , CD012651 (2017). A Cochrane Review, involving 70 RCTs, showing that multicomponent behavioural interventions can lead to small, short-term reductions in BMI and related measures in children aged 6–11 years with obesity.
Ho, M. et al. Effectiveness of lifestyle interventions in child obesity: systematic review with meta-analysis. Pediatrics 130 , e1647–e1671 (2012). To our knowledge, the first systematic review of lifestyle interventions in children and adolescents with obesity to show improvements in cardiometabolic outcomes (LDL cholesterol, triglycerides, fasting insulin and blood pressure), as well as weight.
Clinical Practice Guideline Panel. Clinical practice guideline for multicomponent behavioral treatment of obesity and overweight in children and adolescents: current state of the evidence and research needs. American Psychological Association https://www.apa.org/obesity-guideline/clinical-practice-guideline.pdf (2018).
Nowicka, P. & Flodmark, C. E. Family therapy as a model for treating childhood obesity: useful tools for clinicians. Clin. Child. Psychol. Psychiatry 16 , 129–145 (2011).
Wilfley, D. E. et al. Improving access and systems of care for evidence-based childhood obesity treatment: conference key findings and next steps. Obesity 25 , 16–29 (2017).
Amiri, P. et al. Does motivational interviewing improve the weight management process in adolescents? A systematic review and meta-analysis. Int. J. Behav. Med. 29 , 78–103 (2022).
Kao, T. A., Ling, J., Hawn, R. & Vu, C. The effects of motivational interviewing on children’s body mass index and fat distributions: a systematic review and meta-analysis. Obes. Rev. 22 , e13308 (2021).
Hassapidou, M. et al. European Association for the Study of Obesity (EASO) position statement on medical nutrition therapy for the management of overweight and obesity in children and adolescents developed in collaboration with the European Federation of the Associations of Dietitians (EFAD). Obes. Facts https://doi.org/10.1159/000527540 (2022).
Hoelscher, D. M., Kirk, S., Ritchie, L. & Cunningham-Sabo, L. Position of the Academy of Nutrition and Dietetics: interventions for the prevention and treatment of pediatric overweight and obesity. J. Acad. Nutr. Diet. 113 , 1375–1394 (2013).
Hoare, J. K., Jebeile, H., Garnett, S. P. & Lister, N. B. Novel dietary interventions for adolescents with obesity: a narrative review. Pediatr. Obes. 16 , e12798 (2021).
Lister, N. et al. Nutritional adequacy of diets for adolescents with overweight and obesity: considerations for dietetic practice. Eur. J. Clin. Nutr. 71 , 646–651 (2017).
Andela, S. et al. Efficacy of very low-energy diet programs for weight loss: a systematic review with meta-analysis of intervention studies in children and adolescents with obesity. Obes. Rev. 20 , 871–882 (2019).
Srivastava, G. & Apovian, C. M. Current pharmacotherapy for obesity. Nat. Rev. Endocrinol. 14 , 12–24 (2018).
Apperley, L. J. et al. Childhood obesity: a review of current and future management options. Clin. Endocrinol. 96 , 288–301 (2022).
European Medicines Agency. Saxenda. European Medicines Agency https://www.ema.europa.eu/en/medicines/human/EPAR/saxenda (2022).
US Food and Drug Administration. FDA approves weight management drug for patients aged 12 and older. FDA https://www.fda.gov/drugs/news-events-human-drugs/fda-approves-weight-management-drug-patients-aged-12-and-older (2021).
Kelly, A. S. et al. A randomized, controlled trial of liraglutide for adolescents with obesity. N. Engl. J. Med. 382 , 2117–2128 (2020). To our knowledge, the first RCT of liraglutide, administered daily via subcutaneous injection, in adolescents with obesity.
US Food and Drug Administration. FDA approves novel, dual-targeted treatment for type 2 iabetes. FDA https://www.fda.gov/news-events/press-announcements/fda-approves-novel-dual-targeted-treatment-type-2-diabetes (2022).
Jastreboff, A. M. et al. Tirzepatide once weekly for the treatment of obesity. N. Engl. J. Med. 387 , 205–216 (2022).
Holst, J. J. & Rosenkilde, M. M. GIP as a therapeutic target in diabetes and obesity: insight from incretin co-agonists. J. Clin. Endocrinol. Metab. https://doi.org/10.1210/clinem/dgaa327 (2020).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/study/NCT05260021 (2023).
Müller, T. D., Blüher, M., Tschöp, M. H. & DiMarchi, R. D. Anti-obesity drug discovery: advances and challenges. Nat. Rev. Drug Discov. 21 , 201–223 (2022).
Chalklin, C. G., Ryan Harper, E. G. & Beamish, A. J. Metabolic and bariatric surgery in adolescents. Curr. Obes. Rep. 10 , 61–69 (2021).
Albaugh, V. L. et al. Regulation of body weight: lessons learned from bariatric surgery. Mol. Metab. https://doi.org/10.1016/j.molmet.2022.101517 (2022).
Uhe, I. et al. Roux-en-Y gastric bypass, sleeve gastrectomy, or one-anastomosis gastric bypass? A systematic review and meta-analysis of randomized-controlled trials. Obesity 30 , 614–627 (2022).
Inge, T. H. et al. Long-term outcomes of bariatric surgery in adolescents with severe obesity (FABS-5+): a prospective follow-up analysis. Lancet Diabetes Endocrinol. 5 , 165–173 (2017).
Olbers, T. et al. Laparoscopic Roux-en-Y gastric bypass in adolescents with severe obesity (AMOS): a prospective, 5-year, Swedish nationwide study. Lancet Diabetes Endocrinol. https://doi.org/10.1016/S2213-8587(16)30424-7 (2017).
Pratt, J. S. et al. ASMBS pediatric metabolic and bariatric surgery guidelines, 2018. Surg. Obes. Relat. Dis. 14 , 882–901 (2018).
Jarvholm, K. et al. 5-year mental health and eating pattern outcomes following bariatric surgery in adolescents: a prospective cohort study. Lancet Child Adolesc. Health 4 , 210–219 (2020).
Van Der Heijden, L., Feskens, E. & Janse, A. Maintenance interventions for overweight or obesity in children: a systematic review and meta‐analysis. Obes. Rev. 19 , 798–809 (2018).
Park, J., Park, M.-J. & Seo, Y.-G. Effectiveness of information and communication technology on obesity in childhood and adolescence: systematic review and meta-analysis. J. Med. Internet Res. 23 , e29003 (2021).
Brissman, M., Beamish, A. J., Olbers, T. & Marcus, C. Prevalence of insufficient weight loss 5 years after Roux-en-Y gastric bypass: metabolic consequences and prediction estimates: a prospective registry study. BMJ Open 11 , e046407 (2021).
El Ansari, W. & Elhag, W. Weight regain and insufficient weight loss after bariatric surgery: definitions, prevalence, mechanisms, predictors, prevention and management strategies, and knowledge gaps – a scoping review. Obes. Surg. 31 , 1755–1766 (2021).
World Health Organization Regional Office for Europe. Weight Bias and Obesity Stigma: Considerations for the WHO European Region (WHO, 2017).
Puhl, R. M. & Latner, J. D. Stigma, obesity, and the health of the nation’s children. Psychol. Bull. 133 , 557–580 (2007).
Black, W. R. et al. Health-related quality of life across recent pediatric obesity classification recommendations. Children 8 , 303 (2021).
Finne, E., Reinehr, T., Schaefer, A., Winkel, K. & Kolip, P. Changes in self-reported and parent-reported health-related quality of life in overweight children and adolescents participating in an outpatient training: findings from a 12-month follow-up study. Health Qual. Life Outcomes 11 , 1 (2013).
Hill, A. J. Obesity in children and the ‘myth of psychological maladjustment’: self-esteem in the spotlight. Curr. Obes. Rep. 6 , 63–70 (2017).
McGregor, S., McKenna, J., Gately, P. & Hill, A. J. Self‐esteem outcomes over a summer camp for obese youth. Pediatr. Obes. 11 , 500–505 (2016).
Jansen, P., Mensah, F., Clifford, S., Nicholson, J. & Wake, M. Bidirectional associations between overweight and health-related quality of life from 4–11 years: longitudinal study of Australian children. Int. J. Obes. 37 , 1307–1313 (2013).
Mannan, M., Mamun, A., Doi, S. & Clavarino, A. Is there a bi-directional relationship between depression and obesity among adult men and women? Systematic review and bias-adjusted meta analysis. Asian J. Psychiatr. 21 , 51–66 (2016).
Lindberg, L., Hagman, E., Danielsson, P., Marcus, C. & Persson, M. Anxiety and depression in children and adolescents with obesity: a nationwide study in Sweden. BMC Med. 18 , 30 (2020).
Jebeile, H. et al. Association of pediatric obesity treatment, including a dietary component, with change in depression and anxiety: a systematic review and meta-analysis. JAMA Pediatr. 173 , e192841 (2019).
Gow, M. L. et al. Pediatric obesity treatment, self‐esteem, and body image: a systematic review with meta‐analysis. Pediatr. Obes. 15 , e12600 (2020).
Jebeile, H. et al. Treatment of obesity, with a dietary component, and eating disorder risk in children and adolescents: a systematic review with meta-analysis. Obes. Rev. 20 , 1287–1298 (2019). To our knowledge, the first systematic review to show that structured and professionally led weight management interventions in children and adolescents with obesity are associated with reductions in eating disorder risk and symptoms.
Kjeldbjerg, M. L. & Clausen, L. Prevalence of binge-eating disorder among children and adolescents: a systematic review and meta-analysis. Eur. Child Adolesc. Psychiatry https://doi.org/10.1007/s00787-021-01850-2 (2021).
Patton, G. C., Selzer, R., Coffey, C., Carlin, J. B. & Wolfe, R. Onset of adolescent eating disorders: population based cohort study over 3 years. BMJ 318 , 765–768 (1999).
Cortese, S. The association between ADHD and obesity: intriguing, progressively more investigated, but still puzzling. Brain Sci. 9 , 256 (2019).
Griffiths, L. J., Dezateux, C. & Hill, A. Is obesity associated with emotional and behavioural problems in children? Findings from the Millennium Cohort Study. Int. J. Pediatr. Obes. 6 , e423–e432 (2011).
Harrist, A. W. et al. The social and emotional lives of overweight, obese, and severely obese children. Child. Dev. 87 , 1564–1580 (2016).
Van Geel, M., Vedder, P. & Tanilon, J. Are overweight and obese youths more often bullied by their peers? A meta-analysis on the relation between weight status and bullying. Int. J. Obes. 38 , 1263–1267 (2014).
Albuquerque, D., Nóbrega, C., Manco, L. & Padez, C. The contribution of genetics and environment to obesity. Br. Med. Bull. 123 , 159–173 (2017).
Rancourt, D. & McCullough, M. B. Overlap in eating disorders and obesity in adolescence. Curr. Diabetes Rep. 15 , 78 (2015).
House, E. T. et al. Identifying eating disorders in adolescents and adults with overweight or obesity: a systematic review of screening questionnaires. Int. J. Eat. Disord. 55 , 1171–1193 (2022).
Lister, N. B., Baur, L. A., Paxton, S. J. & Jebeile, H. Contextualising eating disorder concerns for paediatric obesity treatment. Curr. Obes. Rep. 10 , 322–331 (2021).
Hagman, E. et al. Effect of an interactive mobile health support system and daily weight measurements for pediatric obesity treatment, a 1-year pragmatical clinical trial. Int. J. Obes. 46 , 1527–1533 (2022).
Swinburn, B. A. et al. The global syndemic of obesity, undernutrition, and climate change: The Lancet commission report. Lancet 393 , 791–846 (2019).
Whitehead, M., Taylor-Robinson, D. & Barr, B. Poverty, health, and covid-19. Br. Med. J. 372 , n376 (2021).
Morrison, K. M. et al. The CANadian Pediatric Weight Management Registry (CANPWR): lessons learned from developing and initiating a national, multi-centre study embedded in pediatric clinical practice. BMC Pediatr. 18 , 237 (2018).
Kirk, S. et al. Establishment of the pediatric obesity weight evaluation registry: a national research collaborative for identifying the optimal assessment and treatment of pediatric obesity. Child. Obes. 13 , 9–17 (2017).
Hagman, E., Danielsson, P., Lindberg, L. & Marcus, C., BORIS Steering Committee. Paediatric obesity treatment during 14 years in Sweden: lessons from the Swedish Childhood Obesity Treatment Register – BORIS. Pediatr. Obes. 15 , e12626 (2020).
Bohn, B. et al. Changing characteristics of obese children and adolescents entering pediatric lifestyle intervention programs in Germany over the last 11 years: an adiposity patients registry multicenter analysis of 65,453 children and adolescents. Obes. Facts 10 , 517–530 (2017).
Seidler, A. L. et al. A guide to prospective meta-analysis. BMJ 367 , l5342 (2019).
Hunter, K. E. et al. Transforming obesity prevention for children (TOPCHILD) collaboration: protocol for a systematic review with individual participant data meta-analysis of behavioural interventions for the prevention of early childhood obesity. BMJ Open 12 , e048166 (2022).
Lister, N. B. et al. Eating disorders in weight-related therapy (EDIT) collaboration: rationale and study design. Nutr. Res. Rev. https://doi.org/10.1017/S0954422423000045 (2023).
Hadjiyannakis, S. et al. Obesity class versus the Edmonton Obesity Staging System for Pediatrics to define health risk in childhood obesity: results from the CANPWR cross-sectional study. Lancet Child Adolesc. Health 3 , 398–407 (2019).
Brown, V. et al. Core outcome set for early intervention trials to prevent obesity in childhood (COS-EPOCH): agreement on “what” to measure. Int. J. Obes. 46 , 1867–1874 (2022). A stakeholder-informed study that identified the minimum outcomes recommended for collecting and reporting in obesity prevention trials in early childhood.
Han, J. C., Lawlor, D. A. & Kimm, S. Y. Childhood obesity. Lancet 375 , 1737–1748 (2010).
Shin, A. C., Zheng, H. & Berthoud, H. R. An expanded view of energy homeostasis: neural integration of metabolic, cognitive, and emotional drives to eat. Physiol. Behav. 97 , 572–580 (2009).
Lennerz, B., Wabitsch, M. & Eser, K. Ätiologie und genese [German]. Berufl. Rehabil. 1 , 14 (2014).
Google Scholar
Pont, S. J., Puhl, R., Cook, S. R. & Slusser, W. Stigma experienced by children and adolescents with obesity. Pediatrics 140 , e20173034 (2017).
Talumaa, B., Brown, A., Batterham, R. L. & Kalea, A. Z. Effective strategies in ending weight stigma in healthcare. Obes. Rev. 23 , e13494 (2022).
Rubino, F. et al. Joint international consensus statement for ending stigma of obesity. Nat. Med. 26 , 485–497 (2020).
Download references
Author information
Authors and affiliations.
Children’s Hospital Westmead Clinical School, Sydney Medical School, The University of Sydney, Sydney, New South Wales, Australia
Natalie B. Lister & Louise A. Baur
Institute of Endocrinology and Diabetes, The Children’s Hospital at Westmead, Sydney, New South Wales, Australia
Natalie B. Lister
Sydney School of Public Health, The University of Sydney, Sydney, New South Wales, Australia
Louise A. Baur
Weight Management Services, The Children’s Hospital at Westmead, Sydney, New South Wales, Australia
The Generation R Study Group, Erasmus MC, University Medical Center Rotterdam, Rotterdam, Netherlands
Janine F. Felix
Department of Paediatrics, Erasmus MC, University Medical Center Rotterdam, Rotterdam, Netherlands
Institute of Health Sciences, School of Medicine, University of Leeds, Leeds, UK
Andrew J. Hill
Division of Paediatrics, Department of Clinical Science Intervention and Technology, Karolinska Institutet and Karolinska University Hospital, Stockholm, Sweden
Claude Marcus
Vestische Hospital for Children and Adolescents Datteln, University of Witten/Herdecke, Datteln, Germany
Thomas Reinehr
Department of Sport and Exercise Sciences, Durham University, Durham, UK
- Carolyn Summerbell
Division of Paediatric Endocrinology and Diabetes, Department of Paediatrics and Adolescent Medicine, Ulm University Medical Centre, Ulm, Germany
Martin Wabitsch
You can also search for this author in PubMed Google Scholar
Contributions
Introduction (L.A.B., J.F.F. and N.B.L.); Epidemiology (L.A.B. and J.F.F.); Mechanisms/pathophysiology (L.A.B., J.F.F., T.R. and M.W.); Diagnosis, screening and prevention (L.A.B., N.B.L., T.R., C.S. and M.W.); Management (L.A.B., N.B.L., A.J.H., C.M. and T.R.); Quality of life (L.A.B., N.B.L. and A.J.H.); Outlook (L.A.B., N.B.L., J.F.F., A.J.H., C.M., T.R., C.S. and M.W.); Overview of the Primer (L.A.B. and N.B.L.).
Corresponding author
Correspondence to Louise A. Baur .
Ethics declarations
Competing interests.
A.J.H. reports receiving payment for consultancy advice for Slimming World (UK). L.A.B. reports receiving honoraria for speaking in forums organized by Novo Nordisk in relation to management of adolescent obesity and the ACTION-Teens study, which is sponsored by Novo Nordisk. L.A.B. is the Australian lead of the study. T.R. received funding from the German Federal Ministry of Education and Research (BMBF; 01GI1120A/B) as part of the German Competence Network Obesity (Consortium ‘Youth with Extreme Obesity’). T.R. receives payment for consultancy advice related to pharmacological treatment of obesity from Novo Nordisk and Lilly, as well as honoraria for lectures in symposia organized by Novo Nordisk, Novartis and Merck. C.M. receives payments for consultancy advice and advisory board participation from Novo Nordisk, Oriflame Wellness, DeFaire AB and Itrim AB. C.M. also receives honoraria for speaking at meetings organized by Novo Nordisk and Astra Zeneca. C.M. is a shareholder and founder of Evira AB, a company that develops and sells systems for digital support for weight loss, and receives grants from Novo Nordisk for epidemiological studies of the effects of weight loss on future heath. M.W. received funding from the German Federal Ministry of Education and Research (BMBF; 01GI1120A/B) as part of the German Competence Network Obesity (Consortium ‘Youth with Extreme Obesity’). M.W. receives payment for consultancy advice related to pharmacological treatment of obesity from Novo Nordisk, Regeneron, Boehringer Ingelheim and LG Chem, as well as honoraria for speaking in symposia organized by Novo Nordisk, Rhythm Pharmaceuticals and Infectopharm. M.W. is principal investigator in phase II and phase III studies of setmelanotide sponsored by Rhythm Pharmaceuticals. N.B.L., J.F.F. and C.S. declare no competing interests.
Peer review
Peer review information.
Nature Reviews Disease Primers thanks C. Maffeis, L. Moreno, R, Weiss and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Cite this article.
Lister, N.B., Baur, L.A., Felix, J.F. et al. Child and adolescent obesity. Nat Rev Dis Primers 9 , 24 (2023). https://doi.org/10.1038/s41572-023-00435-4
Download citation
Accepted : 12 April 2023
Published : 18 May 2023
DOI : https://doi.org/10.1038/s41572-023-00435-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Relationship between 24-h activity behavior and body fat percentage in preschool children: based on compositional data and isotemporal substitution analysis.
BMC Public Health (2024)
Young people's experiences of physical activity insecurity: a qualitative study highlighting intersectional disadvantage in the UK
- Caroline Dodd-Reynolds
- Naomi Griffin
Enough with simplifying: “eat less and move more”: at what point are we with the treatment of excess weight in paediatrics?
- Giovanni Corsello
- Sergio Bernasconi
Italian Journal of Pediatrics (2024)
Association between watching eating broadcast “Mukbang and Cookbang” and body mass index status in South Korean adolescents stratified by gender
- Sang-yeon Park
- Jeongha Eom
- Eun-Cheol Park
Nutrition Journal (2024)
The relationship between body mass index and cerebrospinal fluid pressure in children with pseudotumor cerebri
- Safiye Güneş Sağer
- Yasemin Akın
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- Funding Opportunities
Accelerating Progress to Reduce Childhood Obesity
Explore the many products nccor has created over the past decade.
Want To Know More?
Stay up to date

FEATURED TOOL
Catalogue of Surveillance Systems
Increase efficiency with access over 100 surveillance systems relevant to childhood obesity research— now featuring variables for sleep research!
Additional tools

Research articles
Featured Publication
2023 annual report, news & webinars.
E-Newsletter
August 2024
NCCOR E-newsletter
New NCCOR Research Presented at ISBNPA 2024
May 22, 2024
Obesity-Related Policy, Systems, and Environmental Research in the U.S. (OPUS)
June 4-5, 2024
Register Today! Upcoming NCCOR Workshop Examines Obesity Prevention Research, Community Engagement, and Systems Change
May 06, 2024
Celebrating a Milestone: NCCOR’s 2023 Annual Report Showcases Strategic Impact on Childhood Obesity Research
Apr 12, 2024
Sleep’s Role in Child Health: Expanding NCCOR’s Catalogue of Surveillance Systems
March 13, 2024 -
February 2024
Never miss a newsletter, we are social.
Check us out on Facebook, LinkedIn, Twitter and YouTube

The overall mission of the Duke Center for Childhood Obesity Research (DCCOR) is to advance effective and equitable obesity prevention and treatment by conducting innovative interdisciplinary research to achieve optimal health for all children.
DCCOR conducts groundbreaking research that seeks to change practice and policy to help children lead healthier lives. Three pillars form the foundation for our research:
- Causes, consequences, and correlates of childhood obesity
- Prevention of obesity and its related morbidities
- Treatment of childhood obesity across the lifespan
Across all pillars, we approach research relative to the following intersecting themes, in order to achieve optimal obesity-related health outcomes:
- Reducing stigma and bias
- Improving health equity
- Establishing policy
- Training the next generation of researchers
In support of our overarching mission, the center’s goals are to:
- Embrace innovative research strategies and support interdisciplinary collaboration by intentionally seeking out collaborators across different departments.
- Discover and deliver effective obesity prevention and treatment to populations of children across the age spectrum from pre-conception through early adulthood by identifying the physical, mental, social, and economic factors that affect parents and/or children in ways that lead to weight gain.
- Close disparities in optimal nutrition and activity that exist for children from diverse racial, ethnic, and economic diverse backgrounds by developing culturally-sensitive intervention materials and focus on reducing barriers and facilitating access to opportunities for healthy eating and activity.
- Combat stigma and bias against those affected by obesity by exploring implicit attitudes and their effects on beliefs, behaviors, and health.
- Educate learners at all levels about obesity --its causes and effects, weight stigma, and healthy lifestyles by developing a curriculum for children and/or parents that can be used in schools or other settings.
- Train future leaders in the field of child obesity research by offering training opportunities and mentorship of junior researchers.
- Engage with schools and local health partners to ensure research efforts are community-based by involving non-university and non-academic collaborators at various steps of the research process.
- Encourage the development of policies that will benefit child health and promote healthy lifestyle habits by collaborating with legislators and key decision-makers and providing them with expertise and advice.
- Publicize our research and disseminate the findings to a wide audience through rigorous scientific channels, center-created newsletters and informational resources, and social media platforms.
With the creation of the Duke Center for Childhood Obesity Research (DCCOR) in January 2017 under the leadership of Eliana Perrin, MD, MPH, the Department of Pediatrics and School of Medicine strengthened its commitment to the multidisciplinary research necessary to develop effective and efficient evidence-based behavioral interventions to prevent childhood obesity. Additional Center revenue and project funding is generated by grant awards from sources such as The Duke Endowment and the National Institutes of Health (NIH). The Center is currently co-directed by Sarah Armstrong, MD , director of the Duke Healthy Lifestyles clinical and research programs and Division Chief of General Pediatrics and Adolescent Health in the Department of Pediatrics, and Asheley Skinner, PhD , Professor of Population Health Sciences and Director of Graduate Studies for Population Health Sciences. The Center is conducting impactful, multidisciplinary research on the causes, consequences, correlates, prevention and treatment of childhood obesity.
Research Environment
DCCOR, which is an integral part of the Department of Pediatrics in the Duke University School of Medicine, is strategically positioned to conduct innovative and groundbreaking research in pediatric obesity. Duke University has a strong reputation as one of the top research institutions in the country. In 2021, the Duke School of Medicine received more than $608 million in NIH funding, ranking third in the nation. Ranking first nationally in NIH research grant funding for pediatrics clinical science departments, Duke’s Department of Pediatrics received nearly $210 million in NIH grants in 2021.
Duke University is highly supportive of research collaboration among faculty members across disciplines, departments, and schools. With the introduction of the 2006 strategic plan “Making a Difference,” Duke began to build university-wide interdisciplinary institutes, initiatives, and centers with the intention of taking novel approaches to problem-focused research. These interdisciplinary entities are supported with core funding from the Office of the Provost, sharing infrastructures that facilitate the work being accomplished by the faculty and students within them. Further evidence of Duke’s support of facilitating interdisciplinary partnerships is the School of Medicine’s interdisciplinary colloquia awards, which aim to connect faculty members from a variety departments to share knowledge and collaborate on common interests.
Duke’s expansive research infrastructure and history of supporting interdisciplinary collaborations will provide DCCOR with a strong foundation to successfully engage in innovative research, make critical advancements and discoveries, and become a leader in the field of pediatric obesity research and prevention.
- Study protocol
- Open access
- Published: 15 July 2019
A randomized controlled trial for overweight and obesity in preschoolers: the More and Less Europe study - an intervention within the STOP project
- Anna Ek ORCID: orcid.org/0000-0002-2179-8408 1 na1 ,
- Christine Delisle Nyström 2 na1 ,
- Adela Chirita-Emandi 3 , 4 ,
- Josep A. Tur 5 , 6 ,
- Karin Nordin 1 ,
- Cristina Bouzas 5 , 6 ,
- Emma Argelich 5 , 6 ,
- J. Alfredo Martínez 6 , 7 , 8 ,
- Gary Frost 9 ,
- Isabel Garcia-Perez 10 ,
- Marc Saez 11 , 12 ,
- Corina Paul 13 , 14 ,
- Marie Löf 2 , 15 &
- Paulina Nowicka 1 , 16
BMC Public Health volume 19 , Article number: 945 ( 2019 ) Cite this article
19k Accesses
21 Citations
18 Altmetric
Metrics details
Childhood overweight and obesity is a serious public health issue with an increase being observed in preschool-aged children. Treating childhood obesity is difficult and few countries use standardized treatments. Therefore, there is a need to find effective approaches that are feasible for both health care providers and families. Thus, the overall aim of this study is to assess the acceptance and effectiveness of a parent support program (the More and Less, ML) for the management of overweight and obesity followed by a mobile health (mHealth) program (the MINISTOP application) in a socially diverse population of families.
Methods/design
A two-arm, parallel design randomized controlled trial in 300 2-to 6-year-old children with overweight and obesity from Romania, Spain and Sweden ( n = 100 from each). Following baseline assessments children are randomized into the intervention or control group in a 1:1 ratio. The intervention, the ML program, consists of 10-weekly group sessions which focus on evidence-based parenting practices, followed by the previously validated MINISTOP application for 6-months to support healthy eating and physical activity behaviors. The primary outcome is change in body mass index (BMI) z-score after 9-months and secondary outcomes include: waist circumference, eating behavior (Child Eating Behavior Questionnaire), parenting behavior (Comprehensive Feeding Practices Questionnaire), physical activity (ActiGraph wGT3x-BT), dietary patterns (based on metabolic markers from urine and 24 h dietary recalls), epigenetic and gut hormones (fasting blood samples), and the overall acceptance of the overweight and obesity management in young children (semi-structured interviews). Outcomes are measured at baseline and after: 10-weeks (only BMI z-score, waist circumference), 9-months (all outcomes), 15- and 21-months (all outcomes except physical activity, dietary patterns, epigenetics and gut hormones) post-baseline.
This study will evaluate a parent support program for weight management in young children in three European countries. To boost the effect of the ML program the families will be supported by an app for 6-months. If the program is found to be effective, it has the potential to be implemented into routine care to reduce overweight and obesity in young children and the app could prove to be a viable option for sustained effects of the care provided.
Trial registration
ClinicalTrials.gov NCT03800823; 11 Jan 2019.
Peer Review reports
According to the World Health Organization childhood obesity is one of the gravest public health challenges of today’s society [ 1 ], with approximately 108 million 2- to 19-year-old children being classified as having obesity [ 2 ]. More specifically, in children less than 5 years, there has been a swift increase in childhood overweight and obesity and if these trends continue it is predicted that 70 million children will be overweight or obese by 2025 [ 3 ]. These statistics are concerning as Geserick et al. [ 4 ] found that 90% of 3 year olds with obesity still had overweight or obesity in adolescence. Furthermore, for those adolescents with overweight or obesity, the majority of weight gain happened between two and 6 years of age [ 4 ]. Thus, this demonstrates the need for evidence-based treatment programs in the pre-school years in order to attempt to rectify the increased prevalence of childhood overweight and obesity.
According to Colquitt et al. [ 5 ] for children under 6 years of age multicomponent interventions (i.e., diet, physical activity, and behavioral interventions) seem to be effective at treating overweight and obesity. However, the authors did state that evidence is limited [ 5 ]. To date, the majority of the treatment interventions for overweight and obesity use face-to-face delivery methods [ 6 ]. A recent meta-analysis by Ling et al. [ 6 ] found small effect sizes on treatment interventions for preschool-aged children for body mass index (BMI) (− 0.28 kg/m 2 , p < 0.001) using various in person delivery methods. Furthermore, the More and Less (ML) study found that at the 12-month follow-up, a 10-week group treatment program focusing on parenting practices had a greater reduction in BMI z-scores than standard treatment in health care (− 0.30 vs. -0.07, p < 0.05). An even greater reduction was observed in the intervention group who received booster sessions (a 30-min phone call every 4 to 6 weeks over a 9-month period) [ 7 ]. These results are promising; however, sustained contacts with families after treatment programs are burdensome on both health care providers and participants, which makes it difficult to scale-up. Therefore, different types of boosters need to be used in order to reduce the burden on both health care and participants.
The universal use of smartphones makes the use of mobile health (mHealth) an option for boosting the effects of treatment programs. mHealth is increasingly being used for promoting healthy habits and as treatment of many types of health conditions and diseases. In adults, two meta-analyses have found that mHealth interventions focusing on weight loss significantly decreased participants’ weight in the intervention groups compared to the control groups [ 8 , 9 ]. In children and adolescents few studies have utilized mHealth in the prevention or treatment of obesity [ 10 , 11 , 12 , 13 , 14 ] and hardly any have been conducted in the preschool-age group [ 15 , 16 ]. The Mobile-based Intervention Intended to Stop Obesity in Preschoolers (MINISTOP) trial was a mHealth obesity prevention intervention that was developed and led by Marie Löf and her team to improve 4-year-old children’s body composition, dietary, physical activity, and sedentary behaviors [ 17 , 18 ]. The MINISTOP intervention had a significant effect on a composite score composed of body composition, diet, and physical activity variables, with this effect being more evident among children with a higher fat mass index [ 18 ]. There are numerous advantages of mHealth over conventional intervention approaches such as: the programs can be delivered any time and place; are interactive; can be tailored to different groups (e.g., translated into multiple languages); and reduces burden on health care professionals and participants. These advantages further motivates the use of mHealth in families with young children with overweight and obesity.
The mechanisms that drive weight gain such as epigenetics and gut hormones are still unclear [ 19 , 20 ]. Epigenetics has received attention during the recent years for the putative involvement in transmitting obesity risk to offspring and in the heritable regulation of gene expression without altering their coding sequence [ 21 ]. The most relevant epigenetic mechanisms involved in gene activity control are histone modifications, non-coding RNAs (ncRNA) and DNA methylation [ 20 ]. Further, obesity has been associated with the epigenetic modulation of several genes. For example, a relationship has been reported between increased BMI and adiposity as well as higher DNA methylation levels at the hypoxia-inducible transcription factor 3A (HIF3A) gene [ 22 ]. Moreover, an increased methylation in the gene RXRA measured at birth has been associated with greater adiposity in later childhood [ 23 ]. Two other investigations identified a strong correlation between obesity and serum levels of micro RNA (miR)-122 and miR-519d [ 24 ] and found DNA methylation to be related to insulin resistance [ 25 ]. However, these findings need to be confirmed and further explored in young children.
Another field of interest for obesity is the gastrointestinal tract (GIT) [ 26 ]. The GIT plays an important role in acute appetite regulation through a number of mechanisms: (1) the release of hormones that play a role in appetite regulation such as anorectic hormones (Peptide YY, PYY, and glucagon-like peptide, GLP-1) and orexogenic gut hormones (e.g., ghrelin), (2) the enteric nervous system and signals through the vagus to the brain to influence appetite and (3) secondary to stimulating signals from other organs such as liver adipose. Previous research in adults has demonstrated that the infusion of the GIT anorectic hormones PYY and GLP-1 at physiological doses has profound effects to suppress appetite [ 26 ]. Also weight loss appears to lead to a suppression of PYY and GLP-1 suggesting a role in the feelings of hunger during weight reduction. However, evidence of the role of GIT hormones in overweight and obesity among young children is sparse.
A major challenge in the management of obesity in both adults and children is understanding what people eat. Most dietary assessment methodologies use methods of self-reported food intake which is a subject to large misreporting error [ 27 , 28 ]. It is therefore impossible to understand what children eat. Garcia et al. has developed a new metabolomic methodology of dietary assessment using urine, which is not subject to the same misreporting errors [ 29 ]. This method has been validated in adults. Our aim is to do this is children.
To the best of our knowledge there is no study to date that has the ambition to assess a broad array of key biological and social determinants of obesity in young children. This study protocol outlines the design of a multi-country study that incorporates both a parent support program and mHealth in an overweight and obesity intervention in 2- to 6-year-old children with overweight and obesity.
The overall aim of this study is to assess the feasibility, acceptance and effectiveness of an overweight and obesity intervention in a socially diverse population of families. The specific aims are:
To determine the effectiveness on child weight status (BMI z-score) of a 10-week parent support program delivered in groups focusing on evidence-based parenting practices (the ML program) followed by a mHealth component for 6-months (the MINISTOP application, app) for overweight and obesity in preschool-aged children.
To assess change in secondary outcomes, which are: waist circumference, child eating behavior, parental feeding practices, and physical activity.
To assess epigenetic mechanisms and physio pathological processes underlying childhood obesity including the role of gut hormones.
To assess and validate child food intake with metabolic markers in urine metabolomics.
To evaluate the feasibility of recruitment (facilitators and barriers), attrition and acceptability of the ML program, the standard treatment and the overall acceptance of overweight and obesity management according to patients and care providers.
Our central hypothesis is that the intervention (the ML program followed by the MINISTOP app for boosting) will be more effective in decreasing children’s BMI z-score (primary outcome), improving eating and feeding behaviors, and physical activity (secondary outcomes) compared to standard care. Another study hypothesis is that the intervention will produce changes in urinary metabolites, which will serve as biomarkers of the nutritional outcomes or as targets for application. We also hypothesize that the parent program and the mHealth intervention will be well accepted by families and caregivers.
Study design
ML Europe is a two-arm parallel design randomized controlled trial (RCT) comparing overweight and obesity treatments in 2-to 6-year-old children in three countries (Romania, Spain, and Sweden). Following baseline assessments, participants will be randomized into the intervention and control group in a 1:1 ratio. The intervention group receives a 10-week parent support program (the ML program) which focuses on evidence-based parenting practices [ 7 , 30 ] followed by a previously validated 6-month mHealth program (the MINISTOP app, PI: M Löf) to support healthy lifestyle changes [ 17 , 18 ]. The control group receives standard treatment as offered in the country of participation. The different interventions are described in greater detail below. Assessments will be conducted at 10 weeks, 9 months, 15 months, and 21 months post-baseline (see Fig. 1 for study outline). This study protocol follows the SPIRIT 2013 statement [ 31 , 32 ].

Flow-chart of the More and Less Europe trial design
Sample size and power calculation
Based on power calculations, 75 children are needed in each group (adjusted for drop-out) to detect a difference of 0.3 BMI z-score with 85% power at the 9-month follow-up between the intervention and control group. These calculations are based on a previous study in this age group [ 33 ]. Thus, each site aims to recruit 100 participants to ensure adequate power.
Participants, eligibility, and recruitment
In total, we aim to include 300 families ( n = 100 in Romania, Spain, and Sweden, respectively). To be included in this study: children must be between 2 and 6 years old and have overweight or obesity as classified by international cut-offs [ 34 ]; have no other underlying medical condition(s); the child has not started any treatment for overweight or obesity; and at least one parent has to have the ability to communicate in Romanian, Spanish, or Swedish depending on the country of participation. Parents who do not own a smartphone compatible with the MINISTOP app will be excluded from this study (i.e., version 10.0 or higher for iOS or version 5.0 or higher for Android).
Recruitment will follow a standardized protocol for all countries. In Romania, family physicians and pediatricians will be involved to hand out information regarding the study to families with 2- to 6-year-olds with overweight or obesity. Parents who want to learn more about the study are provided with a phone number, email address, web page and Facebook page with information of how to contact the research group. Participants will also be recruited, as self-referrals, using an official page for the study on Facebook to be shared with specialized groups.
In Spain, families with children who attend weight and height assessments at their pediatricians at primary care health centers and hospitals will be asked to participate in the study. If the parents are interested in participating, the pediatrician will schedule a visit within a maximum of 7 days to provide them with more detailed information regarding the study and for them to sign the informed consent.
Finally, in Sweden, the recruitment methods have been previously described in detail [ 7 , 30 ]. Briefly, recruitment is done primarily at primary child health care centers, where all parents of children from birth to 5 years of age are offered free, yearly check-ups. If overweight or obesity is detected the nurse provides a verbal and a short one-page explanation of the study. If the parent(s) are interested in participating the nurse sends a referral to the research group that will send out more detailed information regarding the study together with a consent letter. After 1 week, a member from the research team will contact the families to answer any questions that they have. Recruitment is also conducted at secondary health care (i.e., out-patient pediatric clinics). Additionally, self-recruitment is being done through newspaper ads as well as by placing posters on primary health care bulletin boards.
For all countries, after fully informing the families, if they still want to participate they send back the signed consent letter, which is subsequently signed by a member of the research team and a copy is sent back to the family. A time for baseline assessments is then scheduled with the research group.
Randomization and blinding
After the consent form has been signed, the participants are randomly allocated to either the intervention group (parent support program and mHealth booster) or the control group (standard care as per country) at a 1:1 ratio via a random allocation sequence list (in blocks of three). The sequence list was generated using free software environment for statistical computing and graphics R (version 3.5.1) [ 35 ]. The random allocation sequence is managed by a person who has no relationship with recruitment or treatment and opaque envelopes are used to ensure concealment. Those assessing the outcomes are blinded to the treatment allocation; however, owing to the nature of the intervention participants are not blind to their allocation.
Intervention
The more and less program.
The ML program is based on the Keeping Foster and Kin Parents Supported and Trained (KEEP) parenting program, which has been tested in multiple settings [ 36 , 37 , 38 , 39 ]. KEEP is based on Bandura’s Social Learning Theory [ 40 ] and Patterson’s Social Interaction Learning Theory [ 41 , 42 ]. The key concept of the programs is to support parents in evidence-based parenting practices, especially regarding positive reinforcement and limit setting, in order to improve parent and child communication. In ML, the improved communication lays the foundation for parents to support a healthy lifestyle for the child.
The ML program is comprised of 10 weekly sessions (1.5 h/week) and is culturally adapted for Romanian, Spanish, and Swedish families with preschool aged children with overweight or obesity. Table 1 displays the content of the ML program [ 7 , 30 ]. Beyond the evidence-based parenting practices, the program includes content regarding healthy food habits, physical activity habits, as well as techniques to help parents regulate emotional control. Each session begins with a theoretical introduction to a parenting skill, the focus of the session is then discussed and practice is done through role play and homework assignments. To facilitate the implementation of the ML program it follows a manual where the sessions are described with precise instructions to the group leaders (2 per group). The parents receive a manual which summarizes what has been discussed during each session. For parents who are unable to attend sessions, the parental manual is sent home to the family and the family is contacted by phone for a brief review of the session. To facilitate session attendance the time and location for the groups are planned to suit the parents. Child care is also provided during the sessions.
The ML group leaders received an initial 4 day training in child overweight and obesity management and in the ML program content. The training was provided by the ML program developers PN and AE. During the training the sessions of the program were thoroughly discussed and the group leaders were trained in how to deliver the program by acting as group leaders while the other participants acted as parents. The training of group leaders will continue by external supervision after each weekly session for the first group in all countries. The group leaders will be asked to watch the filmed sessions and reflect on how they delivered the program. In Sweden and in Spain, groups will be held in health care facilities and in Romania in university facilities.
The MINISTOP app
The MINISTOP app was developed and evaluated in a population based study with preschool aged children (PI: Marie Löf) and has been previously described in detail [ 17 , 18 ]. Briefly, MINISTOP comprises of an extensive program of information and push notifications built using current guidelines for a healthy diet and physical activity in pre-school aged children [ 43 ]. Over the 6-month period 12 themes will be covered (Table 1 ). A new theme is introduced bi-weekly, with parents being alerted by a push notification when this happens. Every theme is split into three parts (general information; advice; and strategies to change unwanted behavior). Through the app, parents have the ability to register their child’s consumption of sugar sweetened beverages, candy, fruits and vegetables, and physical activity and sedentary behavior. Parents then receive feedback on the registered parameters at the end of every week. Reminder messages are sent out to parents if they have not been in the app after a couple of days [ 17 ].
Two days before the tenth and final session of the ML program, parents receive an email with a username and password for the MINISTOP app as well as a text message with a link to download the app. At the final session, the ML program leaders will ensure that all parents were able to download the app and sign in. Thereafter, they will explain how the app works to the parents and answer any questions that they may have.
The weight management offered to the control group follows the standard care procedure for each country of participation. In Romania and Spain, the control group receives an evaluation of a one-day food frequency questionnaire as well as a 30-min consultation with a doctor that is a specialist in childhood nutrition, where healthy lifestyle recommendations are made. The parents also receive a hand-out which provides general recommendations for healthy food and physical activity in 2 to 6 year olds. Furthermore, in Romania the children are re-evaluated after 3 months during a 15-min consultation. In Sweden, the control group receives standard care according to the Action plan for overweight and obesity for Stockholm County [ 44 ]. Children with overweight and children with obesity younger than 4 years receive support from their child health care nurse. Children older than for 4 years with obesity are followed in an outpatient pediatric clinic with yearly visits to a pediatrician and follow-up visits to a pediatric nurse, approximately 5 visits (30 min in duration) per year [ 7 ]. The treatment centers around supporting the family in creating healthy diet and physical activity habits for the child. Children may also be referred to dieticians, psychologists or physiotherapists.
Outcome measures are collected at baseline, 10 weeks, 9 months, 15 months, and 21 months post baseline. Table 2 presents when outcome measures are assessed and the instruments used to assess child and parental behaviors are displayed in Table 3 .
Primary outcome
BMI z-score is the primary outcome measure which is the most commonly used indicator of weight change in pediatric obesity studies [ 47 ]. The children’s weight and height will be measured to the nearest 0.1 kg and 0.1 cm, respectively. A fixed stadiometer is used to assess height and weight will be measured with the children wearing only underwear. BMI is derived as weight (kg) divided by height (m) squared. BMI z-scores are then calculated using age and gender specific reference values [ 34 ].
Secondary outcomes
Waist circumference.
Waist circumference is measured at the mid-point between the lower rib and iliac crest to the nearest 0.1 cm using a non-elastic tape measurer.
Weight, height and waist circumference are measured three times and mean values are then calculated. All children are measured in a standardized manner by trained health care professionals using calibrated instruments.
Eating behavior
The children’s eating behavior is assessed using the Child Eating Behavior Questionnaire (CEBQ) [ 45 ]. It includes 35 items on eating styles comprising eight factors related to the risk of obesity. Parents rate each behavior on a five-point Likert scale (`never´, `rarely´, `sometimes´, `mostly´, and `always´ for items 1 to 13 and `disagree´, `slightly disagree´, `neutral´, `slightly agree´, and `agree´ for items 14 to 49). Mean scores for each sub-scale are calculated. This questionnaire has been found to have high internal reliability and good validity [ 45 , 48 , 49 , 50 , 51 , 52 , 53 ].
Parenting behavior
The Comprehensive Feeding Practices Questionnaire (CFPQ) is used to measure parenting behavior [ 46 ]. The CFPQ is a parent-report instrument, designed to measure feeding practices of parents of children aged 2–8 years. It contains 49 items comprising 12 factors, where parents rate each behavior on a five-point Likert scale (`never´, `rarely´, `sometimes´, `mostly´, and `always´). The CFPQ has previously been validated in Brazilian preschoolers [ 54 ].
Physical activity and sedentary behavior
The ActiGraph wGT3x-BT accelerometer (ActiGraph Corp, Pensacola, USA, www.actiGraphcorp.com ) is used to assess physical activity and sedentary behavior over seven consecutive 24 h periods. The ActiGraph will be attached the child’s non-dominant wrist and be worn at all times, except for water-based activities (e.g., showering/bathing or swimming). The recorded movements will be used to estimate time in various activity levels based on appropriate cut-points.
Metabolites of food intake
First void urinary samples will be collected from the children and will be used to assess metabolites of food intake. Two urine samples from the child will be collected by the parents at home six and 3 days before the visit to the research group. The third urine sample is collected on the morning of the visit to the research group. The urine metabolite analysis will be carried out as previously described [ 29 ]. In brief, urine samples will be measured by proton nuclear magnetic resonance ( 1 H-NMR) spectroscopy. Global urinary 1 H-NMR profiles will be used to predict the quality of the diet using the World Health Organization guidelines as a reference. Individual urinary metabolites associated with the intake of foods will be used to assess the dietary profile of the child. The Dietary Metabotype Score that embodies concentrations of urinary metabolites related to food components and adherence to diet will be developed and validated against one 24-h dietary recall with a parent. The 24-h recall will cover the day before the visit to the research group. For children attending preschool a food diary for teachers to fill out will be collected to cover the food intake not provided by the parent.
Epigenetic markers and gut hormones
Fasting blood samples are collected to assess reversibility of metabolic markers through epigenetic markers and the role of gut hormones.
Epigenetic markers
The epigenetic analysis is carried out in white blood cells, which require DNA extraction, bisulphite transformation, and analysis with Polymerase chain reactions (PCRs) or other technologies involving hypothesis driven methylation (CpGs). The unit of measurement/criteria is changes in percentage CpGs. The methodology has been explained in detail elsewhere [ 55 , 56 ]. Methylation levels will be analyzed following standardized epigenetic methods after bisulphite conversion as described previously [ 55 , 56 ] in hypothesis- driven specific CpGs.
Gut hormones
PYY concentrations will be measured using an in-house radioimmunoassay (RIA). The assays are highly sensitive and do not cross-react with other gut hormones. Separation of the antibody-antigen complexes from the free antigen is achieved by secondary antibody. The reported intra- and inter-assay variation is 5.8 and 9.8% respectively.
GLP-1 concentrations will be measured using an in-house RIA. This assay is highly specific and sensitive with the antibody cross reacting with 100% of all amidated forms of GLP-1. The assay does not cross react with glycine extended forms (GLP1–37 and GLP9–37) or any other gut hormones. The lowest level of GLP-1 that can be detected by this assay is 7.5 pmol/l. Separation of the antibody-antigen complexes from the free antigen is achieved by charcoal adsorption. The reported in-house intra- and inter-assay variation is 5.4 and 11.5% respectively.
Feasibility, attrition, and acceptability
Using semi-structured interviews, the facilitators and barriers of recruitment as well as attrition to the intervention (first 10 weeks, i.e., the ML parent program) and feasibility and acceptability of the MINISTOP app and of the standard care offered are assessed. Both parents and healthcare professionals are interviewed by trained research staff. During the interviews a set of questions are asked to all participants follow-up questions are however based on individual responses. The questions have been tested in pilot interviews with both parents and health care professionals. The interviews are recorded and fully transcribed. Interviews will be conducted before and after the intervention.
Sociodemographic data
At baseline parents are asked to fill out a background questionnaire for the child and themselves. Questions for the parent include: health status, sociodemographic factors and social support. For the child, questions include: country of birth, health status, family structure and lifestyle related questions such as food and screen time behaviors.
Adverse events
Adverse events will be monitored, reported and handled appropriately. The risks imposed by this research project are deemed to be low, i.e., the burden of the experiments for the research subjects is limited. It is important to note that blood samples collected in the study are optional and not a criteria for participation. However, blood samples are taken by experienced nurses and a pain reducing cream is used to reduce any discomfort. Urinary samples are none invasive and thus cause no risk to the participants. In addition, the investigators have extensive experience conducting behavioral weight control studies, and active efforts will be taken by the research staff to ensure the participating families’ safety. Other adverse events may include psychosocial burden that parents may experience when made aware about their child’s weight status and the sense of guilt that may arise. To handle that, already in the first session of the ML program causes and consequences are reviewed in a non-judgmental way. Also, potential impact on the child’s self-esteem and the way to talk about body weight and obesity with children, if necessary, are addressed.
Data management
All collected data will be handled as approved by the ethical boards to protect confidentiality. Data is de-identified and entered manually into a database by research staff at the participating site where the data originated from. An identical database is used at each site. To ensure data quality and validity the researchers follow standard operation procedure protocols when entering data. The entered data will be double checked by the person entering the data and random checks will be performed regularly to ensure data validity. The database will be password protected and access is restricted to researchers with passwords. Original data forms will be stored in a secure place at each study site.
Statistical analysis
Intention-to-treat analysis using generalized linear mixed models with repeated measures will be used to examine the effects of the intervention on primary (aim 1) and secondary outcomes (aim 2) for the total study population (i.e., all three sites). The link function for the primary outcome (BMI z-score) will be the identity and the Gaussian family (equivalent to a linear regression). In secondary outcomes we will use a Gaussian identity and family link function for waist circumference, physical activity and sedentary behavior, and a logarithmic link and Poisson family function (equivalent to a Poisson regression) for child eating behavior and parental feeding practices. A random effect for country will be used to account for the clustered study design. In the models, we will control for relevant covariates such as sex, age, parental weight status, education level, income and foreign background. Random intercept and a random slope for time will be included in the model to control those non-observed confounders specific to each child that could be constant or vary in time, respectively. Furthermore, interactions between variables will be estimated. If missing values in the outcomes (primary and secondary) are more than 10%, these will be imputed through a two-part model (also known as a model for semi continuous data). In this model, we would simultaneously estimate the probability of not being missing (first part) and the outcome (second part), using a mixed generalized linear model, in which we would include, as explanatory variables: age, sex, parental weight status, foreign background, educational level, and the random effects which are aforementioned.
Statistical tests and analyses of the interaction of phenotypical outcomes with epigenetics will include Manhattan plots, volcano plots, principal component analysis (PCA)/cluster, heatmaps, partial least square-discriminant analysis (PLS-DA), correlations and association studies, linear regression models, receiver operating characteristic (ROC) curves and these will be implemented as appropriate.
The means and medians for the gut hormone values before and after the intervention will be compared, using Student’s t test and Mann-Whitney U test, respectively. The differences will be adjusted in a generalized linear mixed model, with an identity link and Gaussian family, including the confounders, both observed and unobserved, indicated above.
For the validation of child food intake with metabolic markers in urine, the urinary dietary model will be derived using previously described methodology [ 29 ]. Comparison between the study groups will be carried out using PCA and Monte Carlo cross-validated partial least square-discriminant analysis (MCCV-PLS-DA) methodology. The relationship between dietary biomarkers and the dietary metabolite profile will be carried out using a generalized linear mixed model, with an identity link and Gaussian family, including, again, the confounders.
The semi-structured interviews with parents and health care professional will be fully transcribed verbatim and analyzed using thematic analysis [ 57 ].
For our analyses we will use R [ 35 ], STATA version 12.1 (StataCorp 2011, College Station, TX, USA) and SPSS Statistics (IBM, Armonk, NY, USA).
Ethics approval
This trial was approved by: the Ethics Committee of Scientific Research in University of Medicine and Pharmacy “Victor Babes”, Timisoara, Romania, October 31st, 2018 (25/31.10.2018), the Balearic Islands Ethics Committee, Mallorca, Spain, February 13th, 2019 (IB 3814/18 PI), and the Research Ethics Committee, Stockholm, Sweden, December 11th, 2018 (2018/2082–31/1). Written informed consent is obtained from all parents/caregivers. The ethics committees approved the consent procedure.
Trial status
In Sweden and Romania recruitment began in January 2019 and Spain began to recruit in February 2019. Recruitment is expected to last until 2020.
The ML Europe trial will assess the impact of parent support group sessions (the ML program) followed by a mHealth program (the MINISTOP app) to treat overweight and obesity in 2- to 6-year-old children from three European countries. Globally, there has been very few overweight and obesity treatment interventions targeted to pre-school aged children [ 6 ] and to date no intervention has coupled face-to-face delivery with mHealth to boost the effect of the intervention.
In this trial we aim to recruit a representative sample of the study population in each participating country. In Sweden this will be done by inviting all primary and secondary health care centers in Stockholm County to participate in recruitment, with a similar process being done in Spain (all primary health care centers and hospitals in Mallorca were invited to participate). However, the ability to get a representative sample of the study population in Romania might be more difficult as recruitment relies on families contacting the research team themselves through contacts with physicians and pediatricians and Facebook announcements. Therefore, certain parts of the population may be missed, e.g., those not likely to contact the research team and those who do not use Facebook.
Additionally, there are a few other factors that should be considered with regards to recruitment, which have the possibility to influence the representativeness of the overall sample. Firstly, the participating families need to be able to understand, speak, and read Romanian, Spanish, or Swedish sufficiently well (depending on the country of participation) in order to participate. Secondly, families with low socioeconomic status and parents with a lower educational background have been found to be less likely to participate in research [ 58 , 59 ]. The inability to speak the language the intervention is being conducted in coupled with the possibility of low participation rates in families with low socioeconomic status is of concern. This is due to the fact that children of migrant parents and those of low socioeconomic status are more likely to have overweight or obesity [ 60 , 61 ]. Furthermore, families will only be included if they own a smartphone compatible with the MINISTOP app, which could affect recruitment of low socioeconomic families; however, we believe this risk to be quite small as smartphones are so commonly used in most populations. Finally, we foresee that recruitment for this study will be a challenge as was found in the ML trial [ 7 ]. In the ML trial parents decided not to participate for various reasons, with the most common being parents’ work schedules or family situation [ 7 ]. When recruiting for ML Europe we used our experiences from previous clinical RCTs to ensure that recruitment and patient participation are organized in the most feasible way, e.g., time, date and place for the parent groups will be adjusted to suit as many families as possible. We anticipate the recruitment to be influenced by target population size which varies between the countries (330,000 in Timisoara, 860,000 in Mallorca and 2.3 million in Stockholm County). Also, we are aware that the prevalence of overweight and obesity among children differs in each site. While recent national data are yet to be published, in Romania, a study including 6-year-old children found the prevalence for overweight and obesity to be 19% [ 62 ]. In Spain, the prevalence of overweight and obesity was 21% in 3 to 5-year-old children [ 63 ]. In the Stockholm County, the prevalence of overweight and obesity among 4-year-old children is on average 11% ranging from 4% in the more affluent areas to over 15% in less affluent areas [ 64 ]. Thus, although the prevalence and obesity seems to be lowest in the Swedish site the larger population may compensate this challenge. It remains to be elucidated what the largest barrier in the recruitment process will be: not sufficiently large targeted population or low prevalence of overweight and obesity.
The randomized controlled design and multi-site recruitment (i.e., Timisoara, Romania; Mallorca, Spain; and Stockholm, Sweden) are strengths of this study. Furthermore, the fairly large sample size ( n = 300) will allow us to assess the intervention’s effectiveness in samples within and across three very different European countries. With regards to the intervention, both components are based on behavior change theories (i.e., Bandura’s Social Learning Theory [ 40 ] and Patterson’s Social Interaction Learning Theory [ 41 , 42 ] for the ML program and Social Cognitive Theory [ 65 ] for the MINISTOP program). Furthermore, the combination of group sessions followed by a previously evaluated mHealth app is a further strength, as it will allow for the reiteration of the material taught during the group sessions to be explained in different ways with different examples. This is important as the booster group in the ML study had a mean change in BMI z-score from baseline which was significantly larger in comparison to standard treatment and the group without boosters (− 0.54, p < 0.001; − 0.11, p = 0.551; and − 0.04 for the booster, without boosters, and standard treatment groups, respectively) [ 7 ]. In today’s society, telephone based booster sessions after an intervention such as ML is difficult to sustain due to parents’ busy schedules. Therefore, a mHealth solution such as MINISTOP to booster the effect of treatment may be a more feasible approach as it allows parents to work through the material at their own pace, when they have time. Finally, this study is limited by the fact that there is no standard overweight and obesity treatment across Europe. Therefore, the control group will receive different treatment depending on the country of participation, which could influence the results. However, standard treatment as per country is the best possible control as it would be considered unethical to withhold treatment for a condition if a treatment exists [ 66 ].
The use of objective assessments for anthropometrics and body composition, physical activity and sedentary behavior, food intake, as well as epigenetic and metabolic markers is a further strength of this study. Additionally, the use of qualitative methods, i.e., semi-structured interviews with health care professionals and parents from all sites will allow us to assess the feasibility of this new overweight and obesity management intervention in three European countries.
In conclusion, in the majority of countries, there is no standard management of overweight and obesity in the pre-school years. As overweight and obesity in this age may track into adolescence and adulthood, causing psychological and physical consequences, families should receive support as early as possible. Feasible and effective approaches for families with pre-school aged children are yet to be developed. If the ML Europe intervention is found to be effective, it has the potential to be implemented into routine care for overweight and obesity across Europe.
Availability of data and materials
Not applicable.
Abbreviations
proton nuclear magnetic resonance
Application
Body mass index
Child eating behaviour questionnaire
Comprehensive feeding practices questionnaire
Deoxyribonucleic acid
Gastrointestinal tract
Glucagon-like peptide
Hypoxia-inducible transcription factor 3A
Keeping foster and kin parents supported and trained
Monte Carlo cross-validated partial least square-discriminant analysis
Mobile health
Mobile-based intervention intended to stop obesity in preschoolers
Micro Ribonucleic acid
More and Less
Non-coding Ribonucleic acid
Principal component analysis
Polymerase chain reaction
Partial least square-discriminant analysis
Randomized controlled trial
Radioimmunoassay
receiver operating characteristic curves
World Health Organization. The Commision on ending childhood obesity. https://www.who.int/end-childhood-obesity/publications/echo-plan-executive-summary/en/ . Accessed 20 Feb 2019.
Collaborators GBDO, Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, et al. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017;377(1):13–27.
Article Google Scholar
World Health Organization. Facts and figures on childhood obesity. http://www.who.int/end-childhood-obesity/facts/en/ . Accessed 20 Feb 2019.
Geserick M, Vogel M, Gausche R, Lipek T, Spielau U, Keller E, et al. Acceleration of BMI in early childhood and risk of sustained obesity. N Engl J Med. 2018;379(14):1303–12.
Article PubMed Google Scholar
Colquitt JL, Loveman E, O'Malley C, Azevedo LB, Mead E, Al-Khudairy L, et al. Diet, physical activity, and behavioural interventions for the treatment of overweight or obesity in preschool children up to the age of 6 years. Cochrane Database Syst Rev. 2016;(3):CD012105.
Ling J, Robbins LB, Wen F, Zhang N. Lifestyle interventions in preschool children: a meta-analysis of effectiveness. Am J Prev Med. 2017;53(1):102–12.
Ek A, Chamberlain KL, Sorjonen K, Hammar U, Malek ME, Sandvik P, et al. A Parent Treatment Program for Preschoolers with Obesity: A Randomized Controlled Trial. Pediatrics. 2019; In Press.
Schippers M, Adam PC, Smolenski DJ, Wong HT, de Wit JB. A meta-analysis of overall effects of weight loss interventions delivered via mobile phones and effect size differences according to delivery mode, personal contact, and intervention intensity and duration. Obes Rev. 2017;18(4):450–9.
Article CAS PubMed Google Scholar
Flores Mateo G, Granado-Font E, Ferre-Grau C, Montana-Carreras X. Mobile phone apps to promote weight loss and increase physical activity: a systematic review and meta-analysis. J Med Internet Res. 2015;17(11):e253.
Article PubMed PubMed Central Google Scholar
Sharifi M, Dryden EM, Horan CM, Price S, Marshall R, Hacker K, et al. Leveraging text messaging and mobile technology to support pediatric obesity-related behavior change: a qualitative study using parent focus groups and interviews. J Med Internet Res. 2013;15(12):e272.
Schoeppe S, Alley S, Van Lippevelde W, Bray NA, Williams SL, Duncan MJ, et al. Efficacy of interventions that use apps to improve diet, physical activity and sedentary behaviour: a systematic review. Int J Behav Nutr Phys Act. 2016;13(1):127.
Darling KE, Sato AF. Systematic review and meta-analysis examining the effectiveness of Mobile health Technologies in Using Self-Monitoring for pediatric weight management. Child Obes. 2017;13(5):347–55.
Callender C, Thompson D. Family TXT: feasibility and acceptability of a mHealth obesity prevention program for parents of pre-adolescent African American girls. Children (Basel). 2018;5(6).
Article PubMed Central Google Scholar
Grutzmacher SK, Munger AL, Speirs KE, Vafai Y, Hilberg E, Braunscheidel Duru E, et al. Predicting attrition in a text-based nutrition education program: survival analysis of Text2BHealthy. JMIR mHealth uHealth. 2019;7(1):e9967.
Militello L, Melnyk BM, Hekler EB, Small L, Jacobson D. Automated behavioral text messaging and face-to-face intervention for parents of overweight or obese preschool children: results from a pilot study. JMIR mHealth uHealth. 2016;4(1):e21.
Militello LK, Melnyk BM, Hekler E, Small L, Jacobson D. Correlates of healthy lifestyle beliefs and behaviors in parents of overweight or obese preschool children before and after a cognitive behavioral therapy intervention with text messaging. J Pediatr Health Care. 2016;30(3):252–60.
Delisle C, Sandin S, Forsum E, Henriksson H, Trolle-Lagerros Y, Larsson C, et al. A web- and mobile phone-based intervention to prevent obesity in 4-year-olds (MINISTOP): a population-based randomized controlled trial. BMC Public Health. 2015;15:95.
Nystrom CD, Sandin S, Henriksson P, Henriksson H, Trolle-Lagerros Y, Larsson C, et al. Mobile-based intervention intended to stop obesity in preschool-aged children: the MINISTOP randomized controlled trial. Am J Clin Nutr. 2017;105(6):1327–35.
PubMed Google Scholar
Roth CL, Enriori PJ, Harz K, Woelfle J, Cowley MA, Reinehr T. Peptide YY is a regulator of energy homeostasis in obese children before and after weight loss. J Clin Endocrinol Metab. 2005;90(12):6386–91.
Egger G, Liang G, Aparicio A, Jones PA. Epigenetics in human disease and prospects for epigenetic therapy. Nature. 2004;429(6990):457–63.
van Dijk SJ, Molloy PL, Varinli H, Morrison JL, Muhlhausler BS. Epigenetics and human obesity. Int J Obes. 2015;39(1):85–97.
Article CAS Google Scholar
Dick KJ, Nelson CP, Tsaprouni L, Sandling JK, Aissi D, Wahl S, et al. DNA methylation and body-mass index: a genome-wide analysis. Lancet. 2014;383(9933):1990–8.
Godfrey KM, Sheppard A, Gluckman PD, Lillycrop KA, Burdge GC, McLean C, et al. Epigenetic gene promoter methylation at birth is associated with child's later adiposity. Diabetes. 2011;60(5):1528–34.
Article CAS PubMed PubMed Central Google Scholar
Adams BD, Arem H, Hubal MJ, Cartmel B, Li F, Harrigan M, et al. Exercise and weight loss interventions and miRNA expression in women with breast cancer. Breast Cancer Res Treat. 2018;170(1):55–67.
Arpon A, Milagro FI, Ramos-Lopez O, Mansego ML, Santos JL, Riezu-Boj JI, et al. Epigenome-wide association study in peripheral white blood cells involving insulin resistance. Sci Rep. 2019;9(1):2445.
Article PubMed PubMed Central CAS Google Scholar
Choudhury SM, Tan TM, Bloom SR. Gastrointestinal hormones and their role in obesity. Curr Opin Endocrinol Diabetes Obes. 2016;23(1):18–22.
Poslusna K, Ruprich J, de Vries JH, Jakubikova M, van't Veer P. Misreporting of energy and micronutrient intake estimated by food records and 24 hour recalls, control and adjustment methods in practice. Br J Nutr. 2009;101(Suppl 2):S73–85.
Lafay L, Mennen L, Basdevant A, Charles MA, Borys JM, Eschwege E, et al. Does energy intake underreporting involve all kinds of food or only specific food items? Results from the Fleurbaix Laventie Ville Sante (FLVS) study. Int J Obes Relat Metab Disord. 2000;24(11):1500–6.
Garcia-Perez I, Posma JM, Gibson R, Chambers ES, Hansen TH, Vestergaard H, et al. Objective assessment of dietary patterns by use of metabolic phenotyping: a randomised, controlled, crossover trial. Lancet Diabetes Endocrinol. 2017;5(3):184–95.
Ek A, Chamberlain KL, Ejderhamn J, Fisher PA, Marcus C, Chamberlain P, et al. The more and less study: a randomized controlled trial testing different approaches to treat obesity in preschoolers. BMC Public Health. 2015;15(1):735.
Chan AW, Tetzlaff JM, Gotzsche PC, Altman DG, Mann H, Berlin JA, et al. SPIRIT 2013 explanation and elaboration: guidance for protocols of clinical trials. BMJ. 2013;346:e7586.
Chan AW, Tetzlaff JM, Altman DG, Laupacis A, Gotzsche PC, Krleza-Jeric K, et al. SPIRIT 2013 statement: defining standard protocol items for clinical trials. Ann Intern Med. 2013;158(3):200–7.
Kleber M, Schaefer A, Winkel K, Hoffmann D, Wunsch R, Kersting M, et al. Lifestyle intervention "Obeldicks mini" for obese children aged 4 to 7 years. Klin Padiatr. 2009;221(5):290–4.
Cole TJ, Lobstein T. Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatr Obes. 2012;7(4):284–94.
R Core Team. https://www.R-project.org/ . Accessed 9 May 2019.
Price JM, Chamberlain P, Landsverk J, Reid JB, Leve LD, Laurent H. Effects of a foster parent training intervention on placement changes of children in foster care. Child Maltreat. 2008;13(1):64–75.
Chamberlain P, Price J, Leve LD, Laurent H, Landsverk JA, Reid JB. Prevention of behavior problems for children in foster care: outcomes and mediation effects. Prev Sci. 2008;9(1):17–27.
Forgatch MS, DeGarmo DS. Parenting through change: an effective prevention program for single mothers. J Consult Clin Psychol. 1999;67(5):711–24.
Horwitz SM, Chamberlain P, Landsverk J, Mullican C. Improving the mental health of children in child welfare through the implementation of evidence-based parenting interventions. Admin Pol Ment Health. 2010;37(1–2):27–39.
Bandura A. A social learning theory. New York: General Learning Press; 1971.
Google Scholar
Patterson GR, Forgatch MS, Degarmo DS. Cascading effects following intervention. Dev Psychopathol. 2010;22(4):949–70.
Patterson GR: Performance models for parenting: a social interactional perspective. In: parenting and children's internalization of values: a handbook of contemporary theory. Grusec JE, Kuczynski L, ediors. New York: Wiley; 1997: 193–235.
National Food Agency, Sweden. Swedish Food Database. https://www.livsmedelsverket.se/livsmedel-och-innehall/naringsamne/livsmedelsdatabasen . Accessed 14 May 2019.
The healthcare administration in Stockholm County. Action plan overweight and obesity 2016–2020, Stockholm County. http://dok.slso.sll.se/CES/FHG/Folkhalsoarbete/Informationsmaterial/Handlingsprogram-overvikt-fetma-2016-2020.pdf . Accessed May 9 2019.
Wardle J, Guthrie CA, Sanderson S, Rapoport L. Development of the Children's eating behaviour questionnaire. J Child Psychol Psychiatry. 2001;42(7):963–70.
Musher-Eizenman D, Holub S. Comprehensive feeding practices questionnaire: validation of a new measure of parental feeding practices. J Pediatr Psychol. 2007;32(8):960–72.
Oude Luttikhuis H, Baur L, Jansen H, Shrewsbury VA, O'Malley C, Stolk RP, et al. Interventions for treating obesity in children. Cochrane Database Syst Rev. 2009;(1):CD001872.
Carnell S, Wardle J. Measuring behavioural susceptibility to obesity: validation of the child eating behaviour questionnaire. Appetite. 2007;48(1):104–13.
Sleddens EF, Kremers SP, Thijs C. The children's eating behaviour questionnaire: factorial validity and association with body mass index in Dutch children aged 6-7. Int J Behav Nutr Phys Act. 2008;5:49.
Svensson V, Lundborg L, Cao Y, Nowicka P, Marcus C, Sobko T. Obesity related eating behaviour patterns in Swedish preschool children and association with age, gender, relative weight and parental weight--factorial validation of the Children's eating behaviour questionnaire. Int J Behav Nutr Phys Act. 2011;8:134.
Spence JC, Carson V, Casey L, Boule N. Examining behavioural susceptibility to obesity among Canadian pre-school children: the role of eating behaviours. IJPO. 2011;6(2–2):e501–7.
Sparks MA, Radnitz CL. Confirmatory factor analysis of the Children's eating behaviour questionnaire in a low-income sample. Eat Behav. 2012;13(3):267–70.
Mallan KM, Liu WH, Mehta RJ, Daniels LA, Magarey A, Battistutta D. Maternal report of young children's eating styles. Validation of the Children's eating behaviour questionnaire in three ethnically diverse Australian samples. Appetite. 2013;64:48–55.
Warkentin S, Mais LA, Latorre Mdo R, Carnell S, Taddei JA. Validation of the comprehensive feeding practices questionnaire in parents of preschool children in Brazil. BMC Public Health. 2016;16:603.
Arpon A, Milagro FI, Razquin C, Corella D, Estruch R, Fito M, et al. Impact of consuming extra-virgin olive oil or nuts within a Mediterranean diet on DNA methylation in peripheral white blood cells within the PREDIMED-Navarra randomized controlled trial: a role for dietary lipids. Nutrients. 2017;10(1).
Article PubMed Central CAS Google Scholar
Mansego ML, Garcia-Lacarte M, Milagro FI, Marti A, Martinez JA. DNA methylation of miRNA coding sequences putatively associated with childhood obesity. Pediatr Obes. 2017;12(1):19–27.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
Ulijaszek SJ, Pentecost M, Marcus C, Karpe F, Fruhbeck G, Nowicka P. Inequality and childhood overweight and obesity: a commentary. Pediatr Obes. 2017;12(3):195–202.
Bambra CL, Hillier FC, Cairns JM, Kasim A, Moore HJ, In SCD. How effective are interventions at reducing socioeconomic inequalities in obesity among children and adults? Two systematic reviews. Southampton (UK): NIHR J Libr. 2015.
Iguacel I, Fernandez-Alvira JM, Ahrens W, Bammann K, Gwozdz W, Lissner L, et al. Prospective associations between social vulnerabilities and children's weight status. Results from the IDEFICS study. Int J Obes. 2018;42(10):1691–703.
Peeters A, Backholer K. Reducing socioeconomic inequalities in obesity: the role of population prevention. Lancet Diabetes Endocrinol. 2015;3(11):838–40.
Chirita-Emandi A, Barbu CG, Cinteza EE, Chesaru BI, Gafencu M, Mocanu V, et al. Overweight and underweight prevalence trends in children from Romania - pooled analysis of cross-sectional studies between 2006 and 2015. Obes Facts. 2016;9(3):206–20.
Cadenas-Sanchez C, Intemann T, Labayen I, Artero EG, Alvarez-Bueno C, Sanchis-Moysi J, et al. Prevalence of severe/morbid obesity and other weight status and anthropometric reference standards in Spanish preschool children: the PREFIT project. Pediatr Res. 2019.
The Child Health Care Unit Stockholm County. Yearly Report Child Health Care in Stockholm County 2017. https://www.vardgivarguiden.se/globalassets/behandlingsstod/barnhalsovard/bhv-rapporter/arsrapport-barnhalsovard-2017.pdf . Accessed 20 Feb 2019.
Bandura A. Human agency in social cognitive theory. Am Psychol. 1989;44(9):1175–84.
Holm JC, Nowicka P, Farpour-Lambert NJ, O'Malley G, Hassapidou M, Weiss R, et al. The ethics of childhood obesity treatment - from the childhood obesity task force (COTF) of European Association for the Study of obesity (EASO). Obesity facts. 2014;7(4):274–81.
European Commission. Cordis EU research results. https://cordis.europa.eu/project/rcn/214762/factsheet/en. Accessed 13 May 2019 .
Download references
Acknowledgments
Many people have contributed with valuable ideas and practical support to this study. Among these are: (in Romania) Prof. Dr. Maria Puiu, Prof. Dr. Mihai Gafencu, Dr. Iulia Teodora Perva, Dr. Iulia Jurca Simina, Dr. Anamaria Dragomir, Casandra Chera (psychologist), Meda Bugi (dietician), (in Sweden) Fredika Gauffin (Head of the Astrid Lindgren’s Children’s Hospital’s out-patient pediatric clinics in Stockholm), Ola Eklund (Assisting Head of the Astrid Lindgren’s Children’s Hospital’s out-patient pediatric clinics in Stockholm), Christina Norling (Nursing Manager of the Astrid Lindgren’s Children’s Hospital’s out-patient pediatric clinics South Stockholm), Annelie Täppmark (Nursing Manager of the Astrid Lindgren’s Children’s Hospital’s out-patient pediatric clinics North Stockholm), Helena Martin (Head of the Stockholm County Child Health Care), Catharina Neovius (Child Health Care Developer in Stockholm County), Emmie Söderström (research assistant), My Sjunnestrand (research assistant) all child health care nurses, pediatricians and pediatric nurses that are involved in recruitment and providing standard care, (in Spain) David Mateos (nurse, Son Espases University Hospital), Diego de Sotto (Head of Pediatric Service, Rotger Clinics), Helena Corral (pediatrician, Hospital of Inca), Maria Àngels Martínez (pediatrician, Hospital of Inca), Maria Caimari (pediatric endocrinologist, Son Espases University Hospital), Marta Minguez (pediatrician, Hospital of Inca) for support and involvement in recruitment and providing standard care. The authors thank Nils Lidström and Jan Fjellström for help with the technical development of the MINISTOP app and Hanna Hennriksson for her work and support during the translation process of the app.
This study is funded through the STOP project, http://www.stopchildobesity.eu/ . The STOP project received funding from the European Union’s Horizon 2020 research and innovation programme under Grant Agreement No. 774548 [ 67 ]. The content of this document reflects only the authors’ views and the European Commission is not liable for any use that may be made of the information it contains. JAT, CB, EA and JAM are also funded by CIBEROBN (CB12/03/30038), Instituto de Salud Carlos III and the European Regional Development Fund. CB is also funded by a Fernando Tarongí Bauzà Grant. MS was also funded by CIBERESP, Instituto de Salud Carlos III. The funders had no role in the design; collection, analysis, and interpretation of data; or in writing the manuscript.
Author information
Anna Ek and Christine Delisle Nyström contributed equally to this work.
Authors and Affiliations
Division of Pediatrics, Department of Clinical Science Intervention and Technology, Karolinska Institutet, Stockholm, Sweden
Anna Ek, Karin Nordin & Paulina Nowicka
Department of Biosciences and Nutrition, Karolinska Institutet, Stockholm, Sweden
Christine Delisle Nyström & Marie Löf
Genetics Department, University of Medicine and Pharmacy “Victor Babes”, Timisoara, Romania
Adela Chirita-Emandi
“Louis Turcanu” Clinical Emergency Hospital for Children, Timisoara, Romania
Research Group on Community Nutrition & Oxidative Stress, University of the Balearic Islands, Palma de Mallorca, Spain
Josep A. Tur, Cristina Bouzas & Emma Argelich
CIBER of Physiology of Obesity and Nutrition (CIBEROBN), Instituto Carlos III, Madrid, Spain
Josep A. Tur, Cristina Bouzas, Emma Argelich & J. Alfredo Martínez
Department of Nutrition, Food Science, and Physiology, Centre for Nutrition Research, University of Navarra, Pamplona, Spain
J. Alfredo Martínez
IMDEA Food Precision Nutrition, Madrid, Spain
Section for Nutrition Research, Department of Medicine, Imperial College London, Hammersmith Campus, London, UK
Division of Systems and Digestive Medicine, Department of Surgery and Cancer, Faculty of Medicine, Imperial College London, South Kensington Campus, London, UK
Isabel Garcia-Perez
Research Group on Statistics, Econometrics and Health (GRECS), University of Girona, Campus de Montilivi, Girona, Spain
CIBER of Epidemiology and Public Health (CIBERESP), Instituto Carlos III, Madrid, Spain
Pediatrics Department, University of Medicine and Pharmacy “Victor Babes”, Timisoara, Romania
Corina Paul
2nd Pediatrics Clinic, Clinical Emergency County Hospital Timisoara, Timisoara, Romania
Department of Medical and Health Sciences, Linköping University, Linköping, Sweden
Department of Food Studies, Nutrition, and Dietetics, Uppsala University, Uppsala, Sweden
Paulina Nowicka
You can also search for this author in PubMed Google Scholar
Contributions
All authors were involved in the study design for More and Less Europe. AE is the project coordinator for the three sites and drafted the manuscript together with CDN who also aided in the development of the MINISTOP app’s content. ACE is the primary investigator for the Romanian site and JAT is the primary investigator for the Spanish site. Regarding recruitment and data collection KN is the coordinator in Sweden, CP in Romania and EA and CB in Spain. JAM is responsible for analyses of epigenetic and metabolic markers and their interpretations. GF and IGP are responsible for the analyses of gut hormones and validation of food intake through urine. MS is responsible for statistical analysis. ML created the original MINISTOP program and led the work when it was modified for ML Europe. PN is responsible for the Swedish site and the primary investigator of the ML Europe. All authors read and approved the final version of the manuscript.
Corresponding author
Correspondence to Anna Ek .
Ethics declarations
Ethics approval and consent to participate.
Ethics approval was obtained from: the Ethics Committee of Scientific Research in University of Medicine and Pharmacy “Victor Babes”, Timisoara, Romania, October 31st, 2018 (25/31.10.2018), the Balearic Islands Ethics Committee, Mallorca, Spain, February 13th, 2019 (IB 3814/18 PI), and the Research Ethics Committee, Stockholm, Sweden, December 11th, 2018 (2018/2082–31/1). Written informed consent is obtained from all parents or caregivers.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.

Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Ek, A., Delisle Nyström, C., Chirita-Emandi, A. et al. A randomized controlled trial for overweight and obesity in preschoolers: the More and Less Europe study - an intervention within the STOP project. BMC Public Health 19 , 945 (2019). https://doi.org/10.1186/s12889-019-7161-y
Download citation
Received : 03 June 2019
Accepted : 13 June 2019
Published : 15 July 2019
DOI : https://doi.org/10.1186/s12889-019-7161-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
August 21, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
Obese children are more likely to develop skin conditions related to the immune system, study finds
by Elsevier

Childhood obesity can contribute to the development of common immune-mediated skin diseases (IMSDs), such as alopecia areata, atopic dermatitis, and psoriasis, new research finds. Maintaining a healthy weight could potentially help lower the chances of developing these skin conditions.
A novel study in the Journal of Investigative Dermatology details the findings of an analysis of 2,161,900 Korean children from 2009 to 2020 to investigate the relationship between obesity or dynamic changes in body weight and the development of IMSDs.
IMSDs have detrimental effects on quality of life, including emotional, physical, social, and functional well-being, in children and their families. Although several biologics have proven effective for treating children with atopic dermatitis or psoriasis, limited treatment options and a lack of clinical trials for systemic therapy still present considerable challenges in treating children with IMSDs.
Childhood obesity rates have surged over the past years, transforming it into an undeniable public health crisis, which was compounded by the effects of the pandemic and national lockdowns. The precise mechanisms responsible for the involvement of obesity in the development of chronic inflammatory skin diseases, including psoriasis, atopic dermatitis, and skin malignancies, remains uncertain.
Co-lead investigator of the study, Seong Rae Kim, MD, Department of Dermatology, Seoul National University College of Medicine, Seoul, Republic of Korea, explains, "Previously, many studies have looked at the link between childhood obesity and IMSDs. However, most of these studies only looked at data from one point in time or compared groups with and without the condition (i.e., obesity or overweight), and they had small sample sizes.
"Very few studies have followed children over a long period to see how their body weight affects the development of these skin conditions. This means we still don't know for sure whether being obese or overweight causes atopic dermatitis and psoriasis or if the opposite is true. Also, no studies have yet looked at the effect of body weight on alopecia areata or how dynamic changes in a child's weight affect development of common IMSDs."
Co-lead investigator Hyunsun Park, MD, Ph.D., Department of Dermatology, Seoul National University College of Medicine; Laboratory of Intestinal Mucosa and Skin Immunology; and Department of Dermatology, Seoul Metropolitan Government-Seoul National University Boramae Medical Center, Seoul, Republic of Korea, adds, "Our research team is very interested in the skin-gut access. We think that various factors, including diet, obesity, or other lifestyles can affect gut environment and contribute to the development of IMSDs. We are trying to find the puzzle pieces to demonstrate how they are connected, and our current research is a step towards that understanding.
"We conducted a large study using data from a national database in Korea, which includes information on almost all infants and children across the country. Our goal was to see how a child's weight and changes in their weight are related to the development of alopecia areata , atopic dermatitis, and psoriasis."
The study revealed that children who were obese were more likely to develop common IMSDs compared to children with a normal weight. Among the three most common IMSDs, atopic dermatitis demonstrated the most obvious trend; children who gained weight (normal to overweight) had a higher risk of developing atopic dermatitis than children who maintained their normal weight, and children who lost weight (overweight to normal) had a lower risk of developing atopic dermatitis than children who maintained their overweight.
Co-lead investigator Seong-Joon Koh, MD, Ph.D., Department of Internal Medicine and Liver Research Institute, Seoul National University College of Medicine; and Laboratory of Intestinal Mucosa and Skin Immunology, Seoul, Republic of Korea, concludes, "Our findings support the importance of promoting weight maintenance among children who are already within the normal weight range because it may help reduce the risk of developing atopic dermatitis.
"In addition, prevention of excessive weight gain and purposeful weight loss, including adopting healthy diet strategies in children with obesity to prevent atopic dermatitis , particularly before school age, should be promoted. Implementing purposeful interventions, including nutritional strategies, to decrease body weight may aid in reducing the risk of developing IMSDs in children."
Explore further
Feedback to editors

Finding love: Study reveals where love lives in the brain
2 hours ago

Self-deployable, biodegradable electrode offers minimally invasive brain signal monitoring
23 hours ago

Study identifies metabolic switch essential for generation of memory T cells and anti-tumor immunity
Aug 24, 2024

Multiple sclerosis appears to protect against Alzheimer's disease
Aug 23, 2024

Good sleep habits important for overweight adults, study suggests

Mediterranean diet supplement can affect epigenetics associated with healthy aging

New method for quantifying boredom in the body during temporary stress

Cancer researchers develop new method that uses internal clock inside tumor cells to optimize therapies

Strength training activates cellular waste disposal, interdisciplinary research reveals

Being a 'weekend warrior' could be as good for brain health as exercising throughout the week
Related stories.

Atopic dermatitis linked to shorter stature in early childhood
Nov 18, 2021

Atopic dermatitis increases risk for inflammatory bowel disease
Sep 1, 2023

Atopic dermatitis has large impact on sexual function among women
Jul 29, 2024

Gen Z perceives atopic dermatitis to be more severe, researchers find
Jul 31, 2024

FDA approves Zoryve for atopic dermatitis
Jul 12, 2024

Questionnaire responses about dermatology history inconsistent
Jul 14, 2021
Recommended for you

New insights into blood flow fluctuations offer hope in fight against cardiovascular disease
Aug 22, 2024

New compound shows great potential for patients with neutrophil-associated inflammation

Mouse model suggests proteins cause damage in fetal abdominal inflammation

A potential pathway may guide new therapies for inflammatory bowel disease and other inflammatory diseases

Most baby foods in US grocery stores are unhealthy, study shows
Aug 21, 2024

Inhalation of live Lactobacilli lessens lung inflammation and improves lung function, preclinical study finds
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
Is Your Baby’s Food As Healthy as You Think? Study Unveils Shocking Nutritional Deficits

A wake-up call for parents and policymakers with widespread use of misleading claims.
Research shows that 60% of US infant and toddler foods do not align with nutritional recommendations, and none adhere to WHO promotional guidelines. With convenience foods on the rise, baby food pouches, despite their popularity, often fail health standards. Misleading marketing practices compound the issue, suggesting a need for stricter regulations.
Nutritional Shortcomings in Infant Foods
A staggering 60 percent of infant and toddler foods fail to meet nutritional recommendations, and none meet promotional requirements set by World Health Organization (WHO) guidelines, according to new research published today (August 21) in the scientific journal Nutrients . [1]
In the absence of US-specific nutrition or promotional guidelines for these foods, researchers at The George Institute for Global Health assessed data on 651 infant and toddler food products sold in the top ten US grocery chains held in the Institute’s FoodSwitch database against this international benchmark. [2]
Among all products, 70 percent failed to meet protein requirements and 44 percent exceeded total sugar requirements. A further one in four products did not meet calorie requirements and one in five exceeded recommended sodium limits.
Health Implications of Poor Nutrition
Dr. Elizabeth Dunford, Research Fellow at The George Institute, and Adjunct Assistant Professor, Department of Nutrition at the University of North Carolina said that the rising popularity of processed convenience foods for infants and young children was concerning.
“Early childhood is a crucial period of rapid growth and when taste preferences and dietary habits form, potentially paving the way for the development of chronic diseases such as obesity, diabetes, and some cancers later in life,” she said.
Growing Popularity of Convenience Foods
“Time-poor parents are increasingly choosing convenience foods, unaware that many of these products lack key nutrients needed for their child’s development and tricked into believing they are healthier than they really are.”
Researchers found that baby food pouches are the fastest-growing products in the sector, with a 900 percent increase in the proportion of sales deriving from pouches in the last 13 years. Concerningly, pouches ranked among the unhealthiest products assessed, with fewer than 7 percent meeting total sugar recommendations.*
Misleading Marketing in Baby Foods
The study also revealed the extent of misleading marketing practices, with almost all (99.4 percent) products featuring at least one prohibited claim on their packaging. On average, products displayed four prohibited claims, with some displaying as many as 11. Common claims included ‘non genetically modified (GM)’ (70 percent), ‘organic’ (59 percent), ‘no BPA ’ (37 percent), and ‘no artificial colors/flavors’ (25 percent).
Dr. Daisy Coyle, Research Fellow and Dietitian at The George Institute said that claims like these create a so-called ‘health halo’ around these products.
“The lack of regulation in this area leaves the door wide open for the food industry to deceive busy parents,” she said.
“We saw this not only in the use of misleading claims but also in the use of misleading names, where the product name did not reflect the main ingredients found on the ingredient list.”
“For example, snack and finger foods often referred to fruit or vegetables in the product name, despite primarily being made of flour or other starches,” Dr. Coyle added.
Rise in Childhood Obesity and Regulatory Challenges
Obesity in children aged two to five has more than doubled in the US since the 1970s, with approximately 13% of preschool children living with obesity. [3] This has only worsened since the COVID-19 pandemic. [4]
“While reducing childhood obesity was a priority under the Obama administration, the issue appears to have fallen by the wayside in recent years,” added Dr. Dunford.
Conclusion and Call for Action
“Our findings highlight the urgent need for better regulation and guidance in the infant and toddler foods market in the United States — the health of future generations depends on it.”
References:
- “An evaluation of the nutritional and promotional profile of commercial foods for infants and toddlers in the United States” by Coyle DH et al., 21 August 2024, Nutrients . DOI: 10.3390/nu16160000
- World Health Organization. Nutrient and Promotion Profile Model: Supporting appropriate promotion of food products for infants and young children 6–36 months in the WHO European Region. 2022 https://www.who.int/europe/publications/i/item/WHO-EURO-2022-6681-46447-67287
- Fryar CD, et al . Prevalence of overweight, obesity, and severe obesity among children and adolescents aged 2–19 years: United States, 1963–1965 through 2017–2018. NCHS Health E-Stats. 2020. https://www.cdc.gov/nchs/data/hestat/obesity-child-17-18/overweight-obesity-child-H.pdf
- Lange SJ et al . Longitudinal Trends in Body Mass Index Before and During the COVID-19 Pandemic Among Persons Aged 2–19 Years — United States, 2018–2020. MMWR Morb Mortal Wkly Rep 2021;70:1278–1283 https://www.cdc.gov/mmwr/volumes/70/wr/mm7037a3.htm?s_cid=mm7037a3_w
*This represents 7 percent of all pouches, but fruit-based pouches (which contain the most sugar) aren’t included in the WHO criteria. This figure becomes 69% if fruit-based pouches are excluded.
Related Articles
Industrial chemicals – linked to a long list of serious health problems – detected in us fast foods, highly processed foods harm memory in the aging brain – but omega-3 supplements may help, new nutrient profiling system: ranking healthfulness of foods from first to worst, small changes in diet could help you live much healthier and more sustainably, anti-nutrients they’re part of a normal diet and not as scary as they sound, study finds eating mangoes reduces women’s facial wrinkles, researchers warn: common food additive – banned in france but allowed in the u.s. – causes adverse health effects in mice, omega-3 fish oil can be as effective for attention as adhd drugs, child deaths significantly reduced with nutrient supplements.
Also, the pouches can leach chemicals into the food. Some of these are forever chemicals.
Save my name, email, and website in this browser for the next time I comment.
Type above and press Enter to search. Press Esc to cancel.
- Open access
- Published: 19 August 2024
Physical activity policies in Saudi Arabia and Oman: a qualitative study using stakeholder interviews
- Ali Ahmed Alzahrani 1 ,
- Peter Gelius 2 ,
- Adrian E. Bauman 3 &
- Klaus Gebel ORCID: orcid.org/0000-0003-0330-7756 1
Health Research Policy and Systems volume 22 , Article number: 111 ( 2024 ) Cite this article
163 Accesses
1 Altmetric
Metrics details
Countries in the Middle East have some of the lowest rates of physical activity and some of the highest rates of obesity in the world. Policies can influence population levels of physical activity. However, there is a dearth of research on physical activity policies in the Gulf region. This qualitative study analyses cross-sectoral barriers and facilitators for the development, implementation and evaluation of physical activity policies in Saudi Arabia and Oman, two of the largest countries in the region.
Semi-structured interviews were conducted with 19 senior policymakers from the Ministries of Health, Education, and Sport in Saudi Arabia and Oman, and were examined using thematic analysis.
We identified seven themes related to physical activity policies in Saudi Arabia and Oman: leadership; existing policies; physical activity programs related to policies; private sector policies; challenges; data/monitoring; and future opportunities. Both countries have a central document that guides policy-makers in promoting physical activity, and the available policies in both countries are implemented via multiple programs and initiatives to increase physical activity. Compared with Oman, in Saudi Arabia, programs from the non-profit sector, represented by community groups, play a more significant role in promoting physical activity outside the government framework. The private sector has contributed to promoting physical activity in both countries, but interviewees stated that more financial support is required. Policy limitations differ between Saudi Arabia and Oman: intersectoral collaboration in Oman is limited and mainly based on individuals’ own initiative, while the health transformation in Saudi Arabia tends to slow down policy implementation in relevant areas. Physical education in Saudi Arabia and Oman is similar; however, increased support and collaboration between government agencies and the private sector for out-of-school sports academies are needed.
Conclusions
This study addresses key gaps in analysing physical activity policies in Gulf Cooperation Council countries. Our study highlights the importance of increasing financial support, improving collaboration between governmental agencies and between them and the private sector and consolidating efforts to back physical activity policies and dismantle cross-sectoral barriers in Saudi Arabia and Oman. Educational institutions in Saudi Arabia and Oman play a crucial role in promoting physical activity from early childhood to young adults. Our insights assist policy-makers, public health officials and stakeholders in shaping effective physical activity-promoting policies, programs and interventions to prevent non-communicable diseases. Challenges identified in Saudi Arabia and Oman's policies will inform their future development.
Peer Review reports
Despite the health benefits of physical activity [ 1 , 2 , 3 ], in most countries, large proportions of the population remain insufficiently active [ 4 , 5 ]. In line with social–ecological models of health [ 6 ], the need for policies to increase population levels of physical activity has been highlighted [ 7 , 8 ]. Physical activity policy is defined as any formal or informal legislative or regulatory action or organized guidance provided by governments and organizations [ 9 , 10 , 11 , 12 ]. Policies can be cross-sectoral and encompass access to various forms of physical activity, including walking and cycling, regulate and promote programs and initiatives, and provide a comprehensive framework for the design, funding and implementation of diverse physical activity interventions [ 9 , 13 , 14 ].
Countries in the Middle East have amongst the lowest levels of physical activity and some of the highest rates of overweight and obesity in the world [ 4 , 15 ]. In Saudi Arabia and Oman, only 29.7% and 25.6% of the adult population, respectively, meet the physical activity recommendations. For the Middle East and North Africa (MENA) region the rate is 38.5% and the global average is 31.3% [ 4 ]. Moreover, in 2020 in Oman, Qatar, Bahrain, Kuwait and the United Arab Emirates, more than 80% of teenagers and 55% of adults (45% of men and 65% of women) were not sufficiently active [ 16 ]. In Saudi Arabia and Oman, dietary patterns are shifting due to increased consumption of processed foods, leading to higher rates of obesity, diabetes and cardiovascular diseases. Traditional diets rich in fruits, vegetables and lean meats are being replaced by fast food and sugary drinks. Moreover, reduced physical activity and increasingly sedentary lifestyles are major determinants of the obesity epidemic [ 17 , 18 ]. Therefore, there is an urgent need in this region for action on physical activity, including policy development, implementation and evaluation.
The 2014 report from the WHO Regional Office for the Eastern Mediterranean on promoting physical activity in the region included a policy mapping exercise on national policy and action on physical activity in all 22 member states [ 19 ]. National physical activity policies were reported for most countries, including all members of the Gulf Cooperation Council (GCC), a political and economic alliance of six Middle Eastern countries [Saudi Arabia, Kuwait, the United Arab Emirates (UAE), Qatar, Bahrain and Oman] that share a similar cultural, social and economic background. According to WHO’s recent Global Status Report on Physical Activity [ 16 ], only 11 of the 22 countries in the Eastern Mediterranean Region had a national physical activity strategy, while all GCC countries had one. The report also identified some partnerships to promote physical activity between various ministries in the Gulf states, particularly across the health, sports and education sectors.
In a systematic scoping review, Klepac Pogrmilovic et al. examined the academic literature on physical activity policy and identified 163 papers, covering 168 countries, including all 6 GCC members [ 20 ]. Few papers on physical activity policy across the Eastern Mediterranean region were identified, thus, the findings for the region were largely based on the 2014 report of the WHO Regional Office [ 20 ]. In another study by Klepac Pogrmilovic and colleagues, a survey on national physical activity policies was completed by representatives of 76 countries. However, this only included three of the 22 countries from the Eastern Mediterranean Region. The authors also emphasized that although national policies and strategies exist in all GCC countries, implementation is lacking. The authors recommended that further research be undertaken into physical activity and sedentary behaviour policy in the region [ 8 ]. It is essential to contextualize these findings with regard to physical activity policies in the Gulf region, including disparities and challenges in their implementation.
Recently, Albujulaya et al. analysed physical activity policy initiatives in Saudi Arabia by conducting semi-structured interviews with three policy-makers from the Ministries of Education and Sports and with six Saudi academics working in this field [ 21 ]. Surprisingly, they did not interview anyone from the Ministry of Health. They concluded that while physical activity amongst Saudis overall has increased, levels among women are still low. While Albujulaya et al. analysed aspects of physical activity policy development, implementation and evaluation in Saudi Arabia, they did not address potential cross-sectoral barriers and facilitators for these processes.
The primary objective of the present study was to analyse cross-sectoral barriers and facilitators for physical activity policy development, implementation and evaluation in GCC countries. The best research paradigm for this study is qualitative research. We chose interpretivist research to describe complex social realities, explore new or under-researched subjects and generate hypotheses for future quantitative research. This approach allows for a detailed examination of phenomena, which is difficult with quantitative methods. Practically, we also lacked a large, easily accessible sample to survey quantitatively. Therefore, interpretivism is particularly effective for understanding stakeholder perspectives on physical activity policies in unique cultural settings, such as those in Saudi Arabia and Oman, providing deep insights into subjective experiences and nuanced views. To achieve this, we interviewed policy-makers from the Ministries of Health, Sport and Education in Saudi Arabia and Oman, the two largest countries in the GCC. We picked these three ministries as previous research highlights that they are chiefly responsible for promoting physical activity and implementing related policies in the Gulf region [ 22 , 23 , 24 ].
Study design
This is a qualitative study using the interpretivist research paradigm [ 25 ], comprising semi-structured interviews with key stakeholders in physical activity policy-making in Saudi Arabia and Oman. We utilized the COREQ checklist to ensure the rigour and transparency of our qualitative methods (Appendix 1).
Sampling and recruitment
We defined stakeholders as those that are directly involved in the development, implementation and evaluation of physical activity policies. We initially sought to conduct interviews with stakeholders in all six GCC countries. We attempted to reach a contact in the Ministry of Health (MoH) in each GCC country by writing to the official email address of the ministries to introduce the study and request the contact details of relevant stakeholders. Despite following up with non-responders, we did not receive any replies from Qatar, Bahrain, Kuwait and the United Arab Emirates. Therefore, we narrowed the scope to Saudi Arabia and Oman, the two largest countries of the six, with 36.4 million and 4.6 million inhabitants, respectively, accounting for 70% of the GCC’s population [ 26 ]. After obtaining contact details of key stakeholders from the ministries, the participants were contacted directly via email or telephone. To recruit additional participants, we used snowball sampling by asking interviewees to provide contact details of other relevant stakeholders in their organization. Because of the documented previous involvement of the sports and education sectors in promoting physical activity in the Gulf States [ 19 ], we also asked participants to identify relevant stakeholders in the Ministries of Sports and Education in Saudi Arabia and Oman. Our study focussed on the Ministries of Sports, Health and Education as they are significantly involved in promoting physical activity within Gulf Cooperation Council countries [ 22 , 23 , 24 ]. Attempts to contact the ministers directly were unsuccessful. However, we managed to reach senior staff in the ministries and in university sports federations which belong to the Ministries of Education. Additionally, we employed different strategies to engage participants from the non-governmental sector in both countries, including networking through professional contacts of the first author, utilizing online platforms such as Twitter and Facebook and forums and capitalizing on established partnerships with both non-governmental organizations (NGOs) and governmental sectors.
Participants were provided with information on the study, and all gave written consent to participate. Additionally, participants were informed at the beginning of the interview that they could withdraw from the study at any time if they chose not to continue participating. An interview guide, based on a review of previous literature [ 22 , 24 ] and collaborative input from the authors, was developed (Appendix 2). In the interviews, we explored stakeholders’ perspectives and opinions regarding existing physical activity policy documents from the Ministries of Health, Education and Sport in their country, as well as facilitators and barriers to physical activity policy development, implementation and evaluation, with field notes made during the interviews. A.A. conducted the interviews via Zoom due to the coronavirus disease 2019 (COVID-19) pandemic between December 2021 and February 2022. Interviews were conducted in Arabic, were audio-recorded with permission obtained from the participants and transcribed verbatim, and lasted between 10 min and 45 min. Repeat interviews were not carried out. The following personal information was collected from each participant: name, organization, position, age, gender and previous work experience. The participants were provided with an opportunity to review the Arabic transcripts for accuracy, and the final transcripts were translated to English. Monitoring of data saturation, an ongoing process based on the notion of informational redundancy [ 27 ], was conducted to ensure that comprehensive insights were obtained. The determination of the number of samples needed to reach data saturation was done separately in each country.
Data analysis
Authors A.A., A.B. and P.G. reviewed the transcripts to familiarize themselves with the content, after which thematic analysis was jointly undertaken by A.A., A.B. and P.G. to code each transcript. Themes were subsequently developed through a partially deductive approach: Main categories in Table 1 were derived from existing frameworks of the policy process, such as the HARDWIRED framework [ 28 ] (covering aspects such as development process, partnerships, resources, communication, evaluation and evidence-base) and CAPPA criteria [ 29 ] (including sectors/institutions involved, implementation, legal status, target groups, goals and targets, timeframe, budget and evaluation/surveillance). Subsequently, sub-categories were added via an inductive process conducted by A.A. during the thematic exploration stage, involving a comprehensive review of all codes within the combined dataset encompassing both Saudi Arabia and Oman. A.A., A.B. and P.G. discussed the coding and the preliminary interpretations to cross-validate the findings. These themes were informed by a comprehensive analysis of the extant literature and relevant findings from previous studies [ 22 , 24 ]. As a medical doctor at King Faisal Medical City in the southern region of Saudi Arabia, the lead author’s professional background informed his approach to data analysis in this qualitative study.
Ethical approval
The study was approved by the Human Research Ethics Committee of the University of Technology Sydney (UTS HREC ref. no. ETH21-6428).
Interviews were conducted with 19 high-level stakeholders in physical activity policy; 12 from Saudi Arabia and 7 from Oman. A total of four of the participants (two from each country) were women. In Saudi Arabia, four participants were from the Ministry of Health (MoH, including one from an NGO that is supervised by the MoH), five were from the Ministry of Education (MoE) and three represented the Ministry of Sport (MoS). In Oman, one participant represented the Ministry of Health, three were from the Ministry of Education and three were from the Ministry of Sport.
We generated six themes regarding physical activity policies in Saudi Arabia and Oman: leadership; existing policy documents; implementation of physical activity policies; challenges; data/monitoring for physical activity policies; and future opportunities. The theme non-profit sector/community groups was generated only for Saudi Arabia. Table 1 provides an overview of the derived main themes and findings.
- Saudi Arabia
Participants from the Saudi MoH and MoS stated that the leadership in the legislation, regulation, and evaluation of physical activity policies is divided between the two ministries. They also collaborate with other government agencies, including the MoE and the Ministry of Municipal and Rural Affairs, to increase physical activity opportunities in schools, workplaces and communities. Two participants from the MoE mentioned that the University Affairs Council and the Supreme Economic Council also work in the promotion of physical activity by regulating the implementation of programs in their sectors according to policy documents from the MoH and MoE.
According to the participant from the NGO supervised by the MoH, the non-profit sector is instrumental in promoting physical activity through walking groups. These have been established throughout the country to provide opportunities for people to engage in physical activity and to socialize, and which are co-organized by various stakeholders, including local businesses, schools, healthcare providers and government agencies: “I firmly believe that the non-profit sector plays a pivotal role in advocating for physical activity in Saudi Arabia” (NGO participant).
Participants from the Saudi MoH underlined that Health in All Policies is one of the main objectives in the new health care transformation in the kingdom. Most participants from the three ministries identified a certain level of cooperation between different stakeholders, particularly between the Ministries of Health, Sport and Education.
The Omani MoH leads the policies and programs to promote physical activity. Participant 1 from the MoH said that their non-communicable disease (NCD) and Health Committees are crucial for leading policy-making and promoting physical activity related to the National Policy for Prevention and Control of NCDs document [ 30 ].
Regarding Health in All Policies, all participants from Oman stated that there is cooperation between the different ministries, but that it is limited and based on individual agencies’ own initiatives rather than combined efforts or a policy imprimatur: “Partnerships exist, but they are limited and based on individual initiatives” (participant 2 from the MoS).
Relevant existing policies
Most of the participants from all three ministries in Saudi Arabia referred to the Quality of Life document [ 31 ], an economic and social reform blueprint that is part of the government’s overarching Saudi Vision 2030 development program [ 32 ]. The Quality of Life document includes the most important physical activity policies implemented by the three ministries: “There is no doubt that the 2030 Vision is our basic guidance” (participant 3 from the MoH). “Before 2017 there were no clear policies. Everyone works on vision files, and everyone has to achieve the [Vision 2030] target to increase the quality of life of the Saudi community” (participant 2 from the MoE). The Quality of Life document emphasizes the need to enhance public health and healthcare services, promote healthy behaviours, and provide opportunities for physical activity and sports participation.
Interviewees from the MoE highlighted that the University Sports Federation strategy promotes physical activity and sport in tertiary education [ 33 ]. Some important miscellaneous policy documents were identified by staff of the three ministries, such as the National Strategy for Healthy Food and Physical Activity 2015–2025 [ 34 ], the Physical Activity Guidelines for Health Practitioners [ 35 ], the 24-Hour Movement Guidelines [ 36 ] (all by the MoH) and the annual report of the Sport for All Federation by the MoS [ 37 ].
Almost all participants across all three ministries stated that the government of Oman’s overarching Vision 2040 [ 38 ] is currently the most important policy document. Participants from the MoE reported that the Vision 2040 guides the promotion of student physical activity, with support from related documents such as the student learning calendar, education document, standards document and the school sports curriculum. These policy documents aim to promote physical activity among students by better integrating physical education (PE) classes into the overall curriculum to encourage regular physical activity and healthy habits. According to participant 1 from the MoH, the Education Document is a comprehensive strategy, including PE and promotion of physical activity in schools and universities. The document outlines various initiatives, policies and guidelines to ensure that education includes a focus on physical health and fitness [ 39 ]. Three participants from the three different Omani ministries referred to the National Policy for Prevention and Control of NCDs [ 30 ], published by the MoH, as the central policy document for physical activity promotion in Oman. Three study participants from the MoS suggested that the Omani Sports Strategy [ 40 ] is important for guiding the promotion of physical activity for different segments of society.
Implementation of physical activity policies
(a) physical activity programs.
The MoH and MoE collaborate on a range of health-related issues (obesity, diabetes, mental health and visual acuity) to improve the overall health of school students and to detect problems at an early stage [ 41 ]. This led to the development of the Rashaka initiative, a large-scale multi-component school-based obesity prevention program, which started in 2016 and involved nearly 1000 schools across the country. In 2020, Rashaka was replaced by an annual program composed of screening of students for early signs of chronic diseases and lectures highlighting the significance of physical activity and a healthy diet.
Participants 3 and 4 of the Saudi MoH mentioned the Walk 30 Minutes initiative, which was implemented in 2021 and intends to increase physical activity through mass media and social media, and forms part of the National Strategy for Healthy Food and Physical Activity 2015–2025 of the MoH. An initiative by the University Sports Federation [ 33 ] (related to policies from the MoS), aiming to support sports facilities and clubs for girls and women, was mentioned by three participants from the MoS, and one participant highlighted the MoS’s Talent Support Program to identify and develop talented athletes in different sports.
Participant 3 of the Saudi MoH and participant 5 of the MoE mentioned the Healthy Mall Campaign and the Healthy Campus Project to promote physical activity in air-conditioned malls and universities. These initiatives are related to policies of the National Strategy for Healthy Food and Physical Activity (MoH and MoE). Despite challenges, the study participants considered the Saudi physical activity programs to be effective.
Participants 1 and 2 of the MoE identified programs related to PE policies from the Education Document, which include increasing the number of PE classes per week and organizing tournaments in different sports. According to participants from the three different ministries, a range of physical activity programs took place during the COVID-19 pandemic, including campaigns calling for physical activity at home using apps with exercise videos. These initiatives, as reported by the participants, align with and are supported by the physical activity policy documents from the Ministries of Health, Sport and Education, that is, the National Policy for Prevention and Control of NCDs [ 30 ] and the Oman Sport Strategy [ 40 ].
According to multiple participants, several community-based initiatives were underway in Oman, such as Active Community, Healthy Cities and Healthy Villages and The Green Playgrounds Project. These initiatives had been set up in all Omani cities to make the built environment more activity friendly, for example, by improving neighbourhood walkability, which is also based on the National Policy for Prevention and Control of NCDs [ 30 ].
(B) Private sector
According to most of the participants, the private sector makes important contributions to physical activity promotion in Saudi Arabia by being directly involved in the policy development process. The Tatweer Educational Company, a private holding dedicated to implementing the government's education reform initiative, has developed programs to promote physical activity in schools, aligning with its commitment to a holistic education system. In line with the conceptualization of active travel as physical activity, the Red Sea Company drives the development of Saudi Arabia’s west coast and aims to improve neighbourhood walkability. Participants from the MoE were unanimous in the view that private universities make significant contributions to the promotion of physical activity among staff and students on the basis of financial support from their funders. International and local investors in the education sector are urging private universities to promote physical activity to enhance the universities’ reputation and to be more attractive for prospective students.
According to participant 1 from the Ministry of Health, walking and hiking groups supported by the Health Promotion Center [ 42 ] (a non-profit charitable organization under the umbrella of the Saudi Ministry of Labor and Social Affairs) play an important role in promoting physical activity in Saudi Arabia. This is despite a lack of governmental support, with influencers and celebrities utilizing social media platforms for the promotion of physical activity. This organization has internal policies for the promotion of physical activity through different programs: “The fact is that community groups working to spread this culture of walking have no ceilings, no limits, and no bureaucracy” (participant 1 from the MoH).
In contrast to Saudi Arabia, participants in Oman stated that more support from the private sector is needed to promote physical activity in the country. However, participant 3 from the MoE mentioned an agreement between the MoE and Muscat Pharmacy & Stores limited liability company (LLC) to hold a football tournament for elementary school students. Nevertheless, it is important to highlight that there is a prevailing perception that physical activity cannot be easily monetized. This contributes to the private sector’s limited interest in supporting such initiatives in the Gulf countries, as it is not perceived to yield immediate profits. Overall, the participants from both Saudi Arabia and Oman stated that, unlike in government-supported programs, in the private sector there are no performance indicators to track the progress of physical activity programs.
Data/monitoring
Two participants from the Saudi MoH and MoE mentioned challenges in relation to physical activity monitoring, as each of the three involved ministries independently conducts surveys on physical activity with different methodologies and tools, which may yield conflicting results in monitoring the effects or end-product of physical activity policies. Furthermore, participants from all three ministries confirmed the existence of national surveys for physical activity and emphasized their importance in assessing activity levels. They also shared insights about how they monitor the implementation of physical activity policies and evaluate the effectiveness of various initiatives in their respective sectors: “We follow and evaluate health through periodic national surveys, but each ministry has its own survey with different results. It is not clear how widely these data are utilized in different sectors, such as education, and sports, to inform policies and interventions” (participant 2 from the MoH).
Participants from the MoH and MoS stated that participation rates, policy compliance, budget allocation and health outcomes are being tracked to assess the effectiveness and progress of physical activity policies, with a specific focus on regular reports and data analysis. Furthermore, one participant from the MoE said that there is no monitoring happening for their education-specific policies.
Participant 4 from the MoH suggested that limited policy implementation is likely until the health transformation process is completed by 2030. The health transformation in Saudi Arabia is a recent, prominent project that aims to restructure the health sector to make it more comprehensive, effective and integrated. The transformation is mainly focussed on the prevention of chronic diseases and the promotion of a healthy lifestyle through physical activity and a nutritious diet. On the ground, this transformation entails significant changes in healthcare infrastructure, delivery and accessibility, as well as increased awareness campaigns and the implementation of various programs aimed at improving public health and wellbeing [ 43 ]. To expedite the health transformation in Saudi Arabia, the respondent considered it essential to implement the policies from the Quality of Life document, which is part of the Kingdom’s Vision 2030. This particularly involves promoting physical activity and healthy lifestyles. By fostering these habits, the country could achieve significant improvements in public health and wellbeing. Participant 3 suggested that bureaucracy is a limitation, as new policies and regulations take a long time to implement under different administrations. Moreover, participants from the MoH and MoE declared that a lack of sustainability of physical activity programs and funding were major limitations due to changes in administrations over short periods. Most participants representing the three Saudi ministries stated that a lack of collaboration and cooperation between government departments was a major challenge. For instance, some policies from the MoH need to be implemented by the MoE, such as the screening program of school students [ 41 ]. The hot climate and the desert environment in the Gulf region also present challenges when it comes to implementing physical activity policies.
According to most participants, a lack of funding for the promotion of physical activity was a common challenge in Saudi Arabia because health budgets are mostly allocated to hospitals and curative services rather than to NCD prevention, including physical activity promotion. A lack of facilities (e.g. sports fields, recreation centres, indoor and outdoor courts and multi-use sporting hubs) is a further challenge according to most Saudi respondents. Moreover, negative societal attitudes towards physical activity were highlighted by one participant, citing challenges such as the prevalence of social norms that prioritize sedentary pastimes and leisure activities, thereby reinforcing a culture that tends to discourage physical activity [ 44 ].
According to most participants, insufficient collaboration between different stakeholders, as well as a lack of government funding and support from the private sector, were the most important barriers to physical activity promotion. Like in Saudi Arabia, participants from Oman said that the hot climate and desert environment in the Gulf region, a lack of facilities and/or a lack of access to them and negative attitudes in the population towards physical activity (social norms that prioritize sedentary pastimes and leisure activities) all pose obstacles to physical activity. Some participants from the MoE stated that a lack of support for PE facilities in schools has been a major obstacle to increasing students’ physical activity. Like in Saudi Arabia, respondents from Oman felt that the country should rapidly implement the provisions of the Vision 2040, specifically those related to the prevention of chronic diseases through the promotion of a healthy lifestyle and physical activity. Furthermore, an increase in government funding dedicated to promoting physical activity would be desirable.
Future opportunities
Participant 3 from the Saudi MoH stated that future policies might include investment in technology, such as developing smartphone apps for the promotion of physical activity during pandemics, and these could contribute to future physical activity programs. However, this requires direct support from the government, both financially and technically, by providing technical expertise, developing and implementing technology-based solutions and ensuring privacy and security. Furthermore, participant 1 from the MoS and participant 3 of the MoE claimed that programs, such as out-of- school academies for talented young athletes, could further encourage physical activity and foster athletic talent. Three participants from the MoE pointed out that unifying efforts between different stakeholders would be important. Moreover, more support in terms of funding, infrastructure, a skilled workforce, and research are considered promising opportunities by most participants from the three ministries.
Participants from the three ministries stated that community participation, such as activating schools as centres for physical activity promotion in the community, would be a great opportunity in the future if cooperation between different ministries is enhanced. Three participants from the Omani MoS and MoE said that improvements to facilities and the skills of the workforce (e.g. PE teachers, coaches, gym instructors, etc.) are required to increase activity levels. Despite the existence of the national plan for physical activity promotion in Oman [ 45 ], all participants emphasized that the lack of partnerships between the government and other relevant parties, such as schools, sports clubs and community organizations, is a common and significant obstacle. Furthermore, participant 1 from the MoS and participant 3 from the MoE said that more support for out-of-school sport academies, including improved collaboration between governmental agencies and the private sector, and supporting physical education as a part of the Omani education strategy, would be great opportunities.
Participants from the Ministries of Education of Saudi Arabia and Oman highlighted that physical education is crucial for the future in both countries, fostering healthy habits essential for a productive workforce. Integrating physical education into the curriculum promotes wellness and prevents lifestyle-related diseases, contributing to various sectors [ 39 ]. As both nations progress, emphasizing physical education will enhance individual health and serve as a strategic investment in a robust, dynamic workforce.
This study examined cross-sectoral barriers and facilitators for physical activity policy development, implementation and evaluation in Saudi Arabia and Oman by interviewing high-level stakeholders from their Ministries of Health, Sports and Education. Oman established a national policy framework for physical activity in 2014 [ 18 ] under the umbrella of the Oman Vision 2040 [ 38 ], 3 years before Saudi Arabia introduced its Quality of Life Program [ 46 ] under the umbrella of the Saudi Vision 2030 [ 31 ]. Many programs and initiatives to enhance physical activity in both countries were identified, particularly sports initiatives. However, it is worth noting that these efforts often lack comprehensiveness, encompassing a broad range of activities and demographics, and face challenges in effective implementation – observations that are in line with findings from a survey on national physical activity policies by Klepac Pogrmilovic et al. [ 8 ]. The programs and initiatives are predominantly focussed on urban areas and may neglect rural communities [ 44 , 47 ]. Interest in promoting gender equity in physical activity in Oman was prominent, with several programs for female participants [ 24 ]; there was less focus on gender equity in Saudi Arabia, although a positive development was the introduction of PE classes for female students in primary and secondary education in 2018. Policies for promoting physical activity should also support individuals with special needs, patients and the elderly by implementing community programs targeted at these groups, such as walking groups and fitness classes for older adults, and programs targeting people with chronic conditions. Additionally, it is important to focus on policies and programs that support gender equality in physical activity and health.
Our finding regarding insufficient backing of policy interventions to create environments supportive of physical activity in both countries aligns with a study by Allender et al., who interviewed stakeholders in local government in Victoria, Australia, to analyse physical activity policies and initiatives. Similar to our findings from Saudi Arabia and Oman, they identified a lack of relevance and competing priorities (i.e. promoting healthy eating environments was not considered a priority above food safety) as reasons for the lack of support towards creating supportive environments for physical activity and healthy eating [ 48 ].
Health in All Policies has been embraced in Saudi Arabia by integrating the promotion of physical activity into policy development across various areas such as education, sports and the private sector. However, while this integration is mentioned in the respective documents, challenges in implementation may have arisen due to limited cooperation between sectors. Many partnerships have been established with multiple parties in the Kingdom (MoH, MoS, MoE, and the Ministry of Municipal and Rural Affairs) to further develop physical activity policies in each sector and to remove obstacles to the implementation of physical activity programs. According to a WHO report from 2017, promoting Health in All Policies in Saudi Arabia has been identified as a national priority, monitored by the Ministry of Health [ 49 ]. Intersectoral collaboration in Oman is apparently less developed than in Saudi Arabia, hindering the integration of physical activity policies across sectors. Unlike Saudi Arabia’s comprehensive approach of Health in All Policies, Oman relies more on individual agency initiatives. However, there is potential for improvement in Oman to strengthen intersectoral collaboration and enhance the integration of physical activity policies by establishing a comprehensive policy framework and promoting coordinated efforts among sectors. For instance, the Omani government could create an intersectoral task force or committee dedicated to fostering collaboration.
In Saudi Arabia, the non-profit sector, represented by community groups, plays a significant role in promoting physical activity outside of the government framework, aided by the promotion of physical activity by influencers and celebrities through social media platforms [ 42 ]. By contrast, our study participants did not mention any significant involvement of the non-profit sector in physical activity promotion in Oman, either because these types of organizations do not play a role or because their role is not valued by the government stakeholders who we interviewed. The private sector contributes to promoting physical activity in both countries, with particularly strong partnerships with the governmental sector in Saudi Arabia. This may be because tax benefits exist for companies that encourage and promote physical activity in Saudi Arabia [ 31 ]. There are previous examples of these types of partnerships in Oman, such as a collaboration between the education and private sector aiming to create a healthier environment and lifestyle in schools. These partnerships have been achieved through the provision of financial support and sponsorships, specifically targeting sports equipment, facilities and physical activity programs in schools [ 50 ]. However, insufficient budget allocation in this area was considered a challenge, which is consistent with our study, with most participants from the sultanate expressing the need for greater financial support from the private sector.
Policy limitations differ between both countries, mainly due to the health transformation in Saudi Arabia, specifically with the Kingdom’s Vision 2030 [ 51 ]. The slow pace of transformation in various Saudi public health, infrastructure, urban planning, sports and recreation policies may impact their likelihood of being fully implemented by 2030, potentially falling short of WHO’s target for increased physical activity by that year set in their Global Action Plan on Physical Activity [ 52 ]. One of the objectives of the health sector transformation and the Quality of Life Program is to decrease the proportion of the Saudi population who are not sufficiently physically active below (67%) by 2030 [ 51 ]. The government has taken proactive measures to promote physical activity, investing in initiatives that raise awareness about its importance and the associated health benefits. This includes campaigns, public awareness programs and the establishment of recreational facilities to facilitate physical activity. In Oman, more collaboration between political parties is essential to improve the implementation of physical activity policies. According to participant 1 from the Omani MoH, several meetings were recently held with all parties to create plans to better implement physical activity policies. These meetings have led to increased monitoring and stricter enforcement by the Omani government regarding the implementation of physical activity policies in all relevant ministries. Effective health system policies significantly depend on inter-institutional collaboration. While primary health institutions play a central role, the impact of related entities is equally crucial. Educational bodies, sports organizations and community health centres contribute significantly to decision-making processes. Their closer involvement would ensure a more comprehensive approach to promoting physical activity, enhancing wellness and preventing lifestyle-related diseases [ 53 ].
According to previous studies, insufficient funding for promoting physical activity, and more broadly for NCD prevention, is a challenge in both Saudi Arabia and Oman [ 23 , 24 ]. Similarly, in a US study, state public health practitioners were interviewed about the National Physical Activity Plan, who also identified implementation costs and the complexity of physical activity policies as significant challenges [ 54 ]. Financial incentives and private sector involvement, while valuable, do not ensure adequate funding for all aspects of public health initiatives. The private sector’s contribution is often focussed on areas aligned with their business interests or corporate social responsibility. Nevertheless, in Saudi Arabia, certain private sector companies run national programs, such as the Tatweer Educational Company, a private holding dedicated to implementing the government's education reform initiative [ 55 , 56 ]. Enhancing funding for the implementation of physical activity policies in the Gulf region holds great promise in advancing infrastructure, cultivating a proficient workforce, and fostering research initiatives. On the basis of the Saudi Quality of Life document 2030 [ 46 ], the budget of the Ministries of Health, Sport and Education for promoting physical activity will likely increase until 2030.
The monitoring and evaluation of policy implementation across ministries in both countries is challenging due to the absence of comprehensive and precise data on physical activity prevalence in key sectors such as health, sport and education. Therefore, there is an urgent need to address data quality issues, such as inconsistent measurement methods employed across different sectors, which make it difficult to compare and consolidate data, and the lack of standardized protocols which undermines the accuracy and reliability of prevalence estimates. To efficiently monitor policy implementation, the responsibility could, for instance, be entrusted to the MoH for coordination with all pertinent sectors, while the General Statistics Authority should be designated to collect data on physical activity.
Responsibility for ensuring data quality rests with various stakeholders involved in the data collection, including researchers, survey administrators, data analysts and policy-makers. These stakeholders must work collectively to implement robust data collection methodologies, appropriate sampling techniques, rigorous quality control measures and transparent reporting practices. Monitoring of the impact of policies on population levels of physical activity in Saudi Arabia and Oman has improved, but more work is needed, particularly in the education sector in Oman, which requires evaluation of the progress and impact of policies.
To create and implement comprehensive policies, programs and supporting environments, a variety of sectors must collaborate in both countries. This may include transport, urban planning, media, social work, religious and cultural affairs [ 23 ]. In Saudi Arabia, one of the most effective health-promoting practices is physician-recommended physical activity [ 57 ], which is recognized as one of the eight best investments for physical activity by the International Society for Physical Activity and Health [ 58 ]. Therefore, the primary healthcare system in the Gulf region has a critical role in the promotion of physical activity, and further policy development in this area would be promising [ 57 ]. In addition, physical education policies in schools play an integral part in the Gulf states [ 59 ]. Educational institutions in Saudi Arabia and Oman are crucial in promoting physical activity among various age groups. From childhood through adolescence to young adulthood, schools offer structured physical education programs, health education and gender-inclusive activities. Universities support these efforts by providing sports facilities and activities as well as by conducting research on active lifestyles. Coordinated national policies amplify the effectiveness of these initiatives [ 22 , 39 , 60 ]. Furthermore, active transport and urban design policies have not yet been developed sufficiently to become potential contributors to population levels of physical activity in these countries due to cultural, environmental and climatic differences [ 23 ].
Strengths and limitations
Strengths of this study include a sample of high-level stakeholders who are directly involved in the formulation of physical activity policies from three ministries in Saudi Arabia and Oman, the two largest countries in the GCC. Additionally, we recruited one prominent participant from an NGO that is supervised by the Saudi Ministry of Health. We were not able to reach participants from the non-governmental sector in Oman. The original research plan was targeted at all six member countries of the Gulf Cooperation Council, but we were not able to recruit participants from the other GCC states due to political sensitivities surrounding the subject and a lack of responsiveness from relevant authorities. This may limit the generalizability of our findings beyond these specific contexts. However, we managed to recruit senior participants from the two largest GCC countries, which account for 70% of the GCC population. As in many countries, governmental representatives may have been constrained in what they reported in these interviews. Regarding the limitation of interview responses, some participants spoke about the existence of physical activity policies but did not want to provide further information on how they are being implemented, and this kind of information is not easy to obtain from other sources either. Thus, these gaps constitute a need for future research. To ensure research quality based on Lincoln and Guba’s criteria [ 61 ], we implemented several strategies. For credibility, we used investigator triangulation (involving multiple researchers) and theoretical triangulation (utilizing multiple policy frameworks). We did not use methodological triangulation, as we only conducted interviews, nor data triangulation, relying solely on audio transcripts. To ensure dependability, we kept detailed records of data collection and assessed coding accuracy and reliability among our team. For transferability, we addressed inherent challenges by collecting data from two countries, Saudi Arabia and Oman, enhancing the applicability of our findings to similar contexts. Although achieving confirmability was challenging due to our focus on individual perceptions, we aimed for transparency and objectivity in documenting our procedures and decisions.
This study fills important gaps in the analysis of physical activity policies in the Gulf region. Understanding the unique challenges, barriers and successes in promoting physical activity in the GCC countries is essential for developing relevant policies and strategies in the future. Our study highlights the importance of increasing financial support, improving collaboration between governmental agencies and between them and the private sector, and consolidating efforts to back physical activity policies and dismantle cross-sectoral barriers in Saudi Arabia and Oman. Educational institutions in Saudi Arabia and Oman play a crucial role in promoting physical activity from early childhood to young adults. Schools offer structured physical education, health education and gender-inclusive activities, while universities provide sport facilities and conduct research on active lifestyles. Coordinated national policies enhance the effectiveness of these efforts.
Specifically, we recommend allocating dedicated funds, establishing a centralized task force for coordinated policy implementation, creating incentives for private sector investment, developing a national strategy with measurable targets and conducting comprehensive policy reviews to remove bureaucratic obstacles. These steps will facilitate sustained progress and broader engagement in physical activity initiatives.
Our findings provide valuable insights and evidence for policy-makers, public health officials and other stakeholders in the region to develop targeted policies, programs and interventions that promote physical activity and prevent non-communicable diseases. The identified challenges and limitations of physical activity policies in Saudi Arabia and Oman will guide their future development.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available to maintain participants’ confidentiality. However, they can be obtained from the corresponding author upon reasonable request.
Abbreviations
Coronavirus disease 2019
Gulf Cooperation Council
Health in all policies
Limited liability company
Ministry of Education
Ministry of Health
Ministry of Sport
Non-communicable disease
Non-governmental organization
- Physical activity
Physical education
United Arab Emirates
United States
World Health Organization
Physical Activity Guidelines Advisory Committee. 2018 physical activity guidelines advisory committee scientific report. Washington DC: US Department of Health and Human Services; 2018.
Google Scholar
World Health Organization. WHO guidelines on physical activity and sedentary behaviour. Geneva: World Health Organization; 2020.
Dishman RK, Heath G, Schmidt MD, Lee I-M. Physical activity epidemiology. Champaign: Human Kinetics; 2022.
Strain T, Flaxman S, Guthold R, Semenova E, Cowan M, Riley LM, Bull FC, Stevens GA. National, regional, and global trends in insufficient physical activity among adults from 2000 to 2022: a pooled analysis of 507 population-based surveys with 5·7 million participants. Lancet Glob Health. 2024;12(8):e1232–43.
Article PubMed PubMed Central CAS Google Scholar
Guthold R, Stevens GA, Riley LM, Bull FC. Global trends in insufficient physical activity among adolescents: a pooled analysis of 298 population-based surveys with 1·6 million participants. Lancet Child Adolesc Health. 2020;4(1):23–35.
Article PubMed PubMed Central Google Scholar
Sallis JF, Owen N, Fisher E. Ecological models of health behavior. In: Glanz K, Rimer BK, Viswanath K, editors. Health behavior: theory, research, and practice. 5th ed. Hoboken: John Wiley and Sons; 2015.
Calvert HG, Turner L, Leider J, Piekarz-Porter E, Chriqui JF. Comprehensive policies to support comprehensive practices: physical activity in elementary schools. J Phys Act Health. 2020;17(3):313–22.
Article PubMed Google Scholar
Klepac Pogrmilovic B, Ramirez Varela A, Pratt M, Milton K, Bauman A, Biddle SJ, Pedisic Z. National physical activity and sedentary behaviour policies in 76 countries: availability, comprehensiveness, implementation, and effectiveness. Int J Behav Nutr Phys Act. 2020;17(1):1–13.
Article Google Scholar
Gelius P, Messing S, Goodwin L, Schow D, Abu-Omar K. What are effective policies for promoting physical activity? A systematic review of reviews. Prev Med Rep. 2020;18:101095.
Sallis J, Bauman A, Pratt M. Environmental and policy interventions to promote physical activity. Am J Prev Med. 1998;15(4):379–97.
Article PubMed CAS Google Scholar
Schmid TL, Pratt M, Witmer L. A framework for physical activity policy research. J Phys Act Health. 2006;3(s1):S20–9.
Bull F, Milton K, Kahlmeier S, Arlotti A, Juričan AB, Belander O, Martin B, Martin-Diener E, Marques A, Mota J. Turning the tide: national policy approaches to increasing physical activity in seven European countries. Br J Sports Med. 2015;49(11):749–56.
Volf K, Kelly L, García Bengoechea E, Casey B, Gobis A, Lakerveld J, Zukowska J, Gelius P, Messing S, Forberger S. Policy Evaluation Network (PEN): protocol for systematic literature reviews examining the evidence for impact of policies on physical activity across seven different policy domains. HRB Open Res. 2022;3:62.
Volf K, Kelly L, García Bengoechea E, Casey B, Gelius P, Messing S, Forberger S, Lakerveld J, Den Braver NR, Zukowska J. Evidence of the impact of sport policies on physical activity and sport participation: a systematic mixed studies review. Int J Sport Pol Polit. 2022;14(4):697–712.
Abarca-Gómez L, Abdeen ZA, Hamid ZA, Abu-Rmeileh NM, Acosta-Cazares B, Acuin C, Adams RJ, Aekplakorn W, Afsana K, Aguilar-Salinas CA. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 2017;390(10113):2627–42.
World Health Organization. Global status report on physical activity. Geneva: World Health Organization; 2022.
Al-Hazzaa HM. Physical inactivity in Saudi Arabia revisited: a systematic review of inactivity prevalence and perceived barriers to active living. Int J Health Sci. 2018;12(6):50.
Al Siyabi H, Mabry RM, Al Siyabi A, Al Subhi M, Milton K. The development of a national policy framework for physical activity in Oman. J Phys Act Health. 2021;18(12):1471–2.
World Health Organization. Promoting physical activity in the Eastern Mediterranean Region through a life-course approach. Geneva: World Health Organization; 2014.
Klepac Pogrmilovic B, O’Sullivan G, Milton K, Biddle SJ, Bauman A, Bull F, Kahlmeier S, Pratt M, Pedisic Z. A global systematic scoping review of studies analysing indicators, development, and content of national-level physical activity and sedentary behaviour policies. Int J Behav Nutr Phys Act. 2018;15(1):1–17.
Albujulaya N, Stevinson C, Piggin J. Physical activity policy in Saudi Arabia: analysis of progress and challenges. Int J Sport Pol Polit. 2023. https://doi.org/10.1080/19406940.2023.2228812 .
Al-Hazzaa HM, AlMarzooqi MA. Descriptive analysis of physical activity initiatives for health promotion in Saudi Arabia. Front Public Health. 2018;6:329.
Al-Hazzaa HM. Physical activity research in the Gulf Cooperation Council Countries: progress made but work still to do. J Phys Act Health. 2022;19(11):769–70.
Al Siyabi H, Mabry RM, Al Siyabi A, Milton K. A critique of national physical activity policy in Oman using 3 established policy frameworks. J Phys Act Health. 2021;18(12):1473–8.
Denzin NK, Lincoln YS. The Sage handbook of qualitative research. 5th ed. Los Angeles: Sage; 2018.
The World Bank: Data for Saudi Arabia and Oman. https://data.worldbank.org/?locations=SA-OM . Accessed 5 Jan 2024.
Saunders B, Sim J, Kingstone T, Baker S, Waterfield J, Bartlam B, Burroughs H, Jinks C. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant. 2018;52(4):1893–907.
Bellew B, Bauman A, Bull FC, Schoeppe S. The rise and fall of Australian physical activity policy 1996–2006: a national review framed in an international context. Aust N Z Health Policy. 2008. https://doi.org/10.1186/1743-8462-5-18 .
Klepac Pogrmilovic B, O’Sullivan G, Milton K, Biddle SJH, Bauman A, Bellew W, Cavill N, Kahlmeier S, Kelly MP, Mutrie N, et al. The development of the Comprehensive Analysis of Policy on Physical Activity (CAPPA) framework. Int J Behav Nutr Phys Act. 2019;16(1):60.
Omani Ministry of Health: The national policy for prevention and control of NCDs. https://extranet.who.int/nutrition/gina/sites/default/filesstore/OMN_2016_%20%D8%A7%D9%84%D8%AE%D8%B7%D8%A9%20%D8%A7%D9%84%D9%88%D8%B7%D9%86%D9%8A%D8%A9%20%D9%84%D9%84%D9%88%D9%82%D8%A7%D9%8A%D8%A9%20%D9%85%D9%86%20%D8%A7%D9%84%D8%A7%D9%85%D8%B1%D8%A7%D8%B6%20%D8%A7%D9%84%D9%85%D8%B2%D9%85%D9%86%D8%A9%20%D8%BA%D9%8A%D8%B1%20%D8%A7%D9%84%D9%85%D8%B9%D8%AF%D9%8A%D8%A9%20%D9%88%D9%85%D9%83%D8%A7%D9%81%D8%AD%D8%AA%D9%87%D8%A7_1.pdf . Accessed 12 Dec 2023.
Saudi Vision 2030: Quality of life program. https://www.vision2030.gov.sa/v2030/vrps/qol/ . Accessed 25 Dec 2023.
Kingdom of Saudi Arabia: National transformation program. https://vision2030.gov.sa/sites/default/files/NTP_En.pdf . Accessed 2 Jan 2024.
University Sports Federation: University sports federation strategy. https://m.susfweb.com/publication/f-a4f22d74-b999-465c-9cd0-2a89895555a8.pdf . Accessed 17 Nov 2023.
Ministry of Health 2015: The National Diet and Physical Activity Strategy (DPAS) 2015–2025. https://extranet.who.int/nutrition/gina/sites/default/filesstore/SAU_2015_%D8%A7%D9%84%D8%A7%D8%B3%D8%AA%D8%B1%D8%A7%D8%AA%D9%8A%D8%AC%D9%8A%D8%A9%20%D8%A7%D9%84%D9%88%D8%B7%D9%86%D9%8A%D8%A9%20%D9%84%D9%84%D8%BA%D8%B0%D8%A7%D8%A1%20%D8%A7%D9%84%D8%B5%D8%AD%D9%8A%20%D8%A9%D8%A7%D9%84%D9%86%D8%B4%D8%A7%D8%B7%20%D8%A7%D9%84%D8%A8%D8%AF%D9%86%D9%8A.pdf . Accessed 23 Dec 2023.
Saudi Ministry of Health: Physical activity guidelines for health practitioners. https://www.moh.gov.sa/Ministry/About/Health%20Policies/037.pdf . Accessed 2 Nov 2023.
Public Health Authority: 24-hour movement guidance Saudi Arabia. https://covid19.cdc.gov.sa/wp-content/uploads/2021/10/24-hrs-ar.pdf . Accessed 4 Jan 2024.
Saudi Sports for All Federation: Annual report. https://sportsforall.com.sa/wp-content/uploads/2021/03/SFA-Annual-Report-2020-EN-V2-4.pdf . Accessed 24 Oct 2023.
Oman Vision 2040: Vision Document. https://www.oman2040.om/assets/books/oman2040-en/index.html#p=51 . Accessed 10 Sept 2023.
Omani Ministry of Education: The physical education standards document. https://ict.moe.gov.om/omcust/PDF/Sport1_9_Oman.pdf . Accessed 26 Dec 2023.
Oman Olympic Committee: Regulations. https://ooc.om/wp-content/uploads/2021/08/RulesAndRegulationsArabic.pdf . Accessed 7 Jan 2024.
Saudi Ministry of Health: Exploratory examination for students. https://www.my.gov.sa/downloads/manuals/87d1f31c-1c7a-41a2-8a89-650a718a4a9d.pdf . Accessed 2 Dec 2023.
Saudi Health Promotion Centre 2021: HPC. https://saudihpc.com/ . Accessed 21 Sept 2023.
Chowdhury S, Mok D, Leenen L. Transformation of health care and the new model of care in Saudi Arabia: Kingdom’s Vision 2030. J Med Life. 2021;14(3):347–54.
Alqahtani BA, Alenazi AM, Alhowimel AS, Elnaggar RK. The descriptive pattern of physical activity in Saudi Arabia: analysis of national survey data. Int Health. 2021;13(3):232–9.
Omani Ministry of Health: National nutrition strategy. https://extranet.who.int/nutrition/gina/sites/default/filesstore/OMN%202014%20National%20Nutrition%20Startegy.pdf . Accessed 8 Jan 2024.
Quality of Life Program 2020: Vision 2030. https://planipolis.iiep.unesco.org/sites/default/files/ressources/saudi_arabia_quality_of_life.pdf . Accessed 27 Nov 2023.
Evenson KR, Alhusseini N, Moore CC, Hamza MM, Al-Qunaibet A, Rakic S, Alsukait RF, Herbst CH, AlAhmed R, Al-Hazzaa HM. Scoping review of population-based physical activity and sedentary behavior in Saudi Arabia. J Phys Act Health. 2023;20(6):471–86.
Allender S, Gleeson E, Crammond B, Sacks G, Lawrence M, Peeters A, Loff B, Swinburn B. Policy change to create supportive environments for physical activity and healthy eating: which options are the most realistic for local government? Health Promot Int. 2012;27(2):261–74.
World Health Organization: Country cooperation strategy at glance. https://apps.who.int/iris/bitstream/handle/10665/136842/ccsbrief_sau_en.pdf?sequence=1 . Accessed 18 Oct 2023.
World Health Organization. Health-promoting schools initiative in Oman: a WHO case study in intersectoral action. Cairo: Regional Office for the Eastern Mediterranean; 2013.
Government of Saudi Arabia: Vision 2030. https://www.vision2030.gov.sa/media/rc0b5oy1/saudi_vision203.pdf . Accessed 9 Jan 2024.
World Health Organization: Global action plan on physical activity 2018–2030. https://apps.who.int/iris/bitstream/handle/10665/272722/9789241514187-eng.pdf . Accessed 11 Nov 2023.
Aunger JA, Millar R, Greenhalgh J, Mannion R, Rafferty A-M, McLeod H. Why do some inter-organisational collaborations in healthcare work when others do not? A realist review. Syst Rev. 2021;10(1):82.
Evenson KR, Satinsky SB, Valko C, Gustat J, Healy I, Litt JS, Hooker SP, Reed HL, Tompkins NOH. In-depth interviews with state public health practitioners on the United States National Physical Activity Plan. Int J Behav Nutr Phys Act. 2013;10(1):1–9.
Al-Otaibi HH. Measuring stages of change, perceived barriers and self efficacy for physical activity in Saudi Arabia. Asian Pac J Cancer Prev. 2013;14(2):1009–16.
Abdel-Salam D, Abdel-Khalek E. Pattern and barriers of physical activity among medical students of Al-Jouf University, Saudi Arabia. J High Inst Public Health. 2016;46(2):41–8.
Alahmed Z, Lobelo F. Physical activity promotion in Saudi Arabia: a critical role for clinicians and the health care system. J Epidemiol Global Health. 2018;7:S7–15.
International Society for Physical Activity and Health (ISPAH): ISPAH’s eight investments that work for physical activity. www.ISPAH.org/Resources . Accessed 2 Oct 2023.
Alhumaid MM, Khoo S, Bastos T. The effect of an adapted physical activity intervention program on pre-service physical education teachers’ self-efficacy towards inclusion in Saudi Arabia. Sustainability. 2021;13(6):3459.
Alghannam AF, Malkin JD, Al-Hazzaa HM, AlAhmed R, Evenson KR, Rakic S, Alsukait R, Herbst CH, Alqahtani SA, Finkelstein EA. Public policies to increase physical activity and reduce sedentary behavior: a narrative synthesis of “reviews of reviews.” Glob Health Action. 2023;16(1):2194715.
Lincoln YS, Guba EG. But is it rigorous? Trustworthiness and authenticity in naturalistic evaluation. New Dir Eval. 1986;1986(30):73–84.
Download references
Acknowledgements
We would like to express our sincere thanks to the policy-makers in the Kingdom of Saudi Arabia and Oman for their participation in this research.
This project is kindly supported through a PhD scholarship from King Faisal Medical City in Saudi Arabia and PhD funding from the Faculty of Health of the University of Technology Sydney.
Author information
Authors and affiliations.
School of Public Health, Faculty of Health, University of Technology Sydney, City Campus, Ultimo, NSW, 2007, Australia
Ali Ahmed Alzahrani & Klaus Gebel
Faculty of Social and Political Sciences, Institute of Sport Sciences, Quartier UNIL-Centre, Bâtiment Synathlon, CH-1015, Lausanne, Switzerland
Peter Gelius
Prevention Research Collaboration, Sydney School of Public Health, University of Sydney, Sydney, NSW, Australia
Adrian E. Bauman
You can also search for this author in PubMed Google Scholar
Contributions
A.A. recruited participants and conducted interviews with policy-makers. A.A., A.B. and P.G. collectively analysed the transcripts. K.G., A.B. and P.G. made significant contributions to the thorough review and editing of the manuscript.
Corresponding author
Correspondence to Klaus Gebel .
Ethics declarations
Ethics approval and consent to participate, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., supplementary material 2., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ .
Reprints and permissions
About this article
Cite this article.
Alzahrani, A.A., Gelius, P., Bauman, A.E. et al. Physical activity policies in Saudi Arabia and Oman: a qualitative study using stakeholder interviews. Health Res Policy Sys 22 , 111 (2024). https://doi.org/10.1186/s12961-024-01192-w
Download citation
Received : 17 January 2024
Accepted : 20 July 2024
Published : 19 August 2024
DOI : https://doi.org/10.1186/s12961-024-01192-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Health policy
- Gulf region
Health Research Policy and Systems
ISSN: 1478-4505
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Spotify is currently not available in your country.
Follow us online to find out when we launch., spotify gives you instant access to millions of songs – from old favorites to the latest hits. just hit play to stream anything you like..

Listen everywhere
Spotify works on your computer, mobile, tablet and TV.

Unlimited, ad-free music
No ads. No interruptions. Just music.

Download music & listen offline
Keep playing, even when you don't have a connection.

Premium sounds better
Get ready for incredible sound quality.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Family Med Prim Care
- v.4(2); Apr-Jun 2015
Childhood obesity: causes and consequences
Krushnapriya sahoo.
1 Phd Scholar, Department of Human Development and Family Studies, Maharana Pratap University of Agriculture and Technology, Udaipur, Rajasthan, India
Bishnupriya Sahoo
2 Senior Resident, Department of Pediatrics, Vardhmann Medical College and Safdarjung Hospital, New Delhi, India
Ashok Kumar Choudhury
3 Assistant Professor, Department of Hepatology, Institute of Liver and Biliary Sciences, New Delhi, India
Nighat Yasin Sofi
4 Research Scientist, Human Nutrition Unit, All India Institute of Medical Sciences, New Delhi, India
Raman Kumar
5 CMO In Charge Emergency, Department of Clinical Research, Institute of Liver and Biliary Sciences, New Delhi, India
Ajeet Singh Bhadoria
6 Epidemiologist and Public Health Specialist, Department of Clinical Research, Institute of Liver and Biliary Sciences, New Delhi, India
Childhood obesity has reached epidemic levels in developed as well as in developing countries. Overweight and obesity in childhood are known to have significant impact on both physical and psychological health. Overweight and obese children are likely to stay obese into adulthood and more likely to develop non-communicable diseases like diabetes and cardiovascular diseases at a younger age. The mechanism of obesity development is not fully understood and it is believed to be a disorder with multiple causes. Environmental factors, lifestyle preferences, and cultural environment play pivotal roles in the rising prevalence of obesity worldwide. In general, overweight and obesity are assumed to be the results of an increase in caloric and fat intake. On the other hand, there are supporting evidence that excessive sugar intake by soft drink, increased portion size, and steady decline in physical activity have been playing major roles in the rising rates of obesity all around the world. Childhood obesity can profoundly affect children's physical health, social, and emotional well-being, and self esteem. It is also associated with poor academic performance and a lower quality of life experienced by the child. Many co-morbid conditions like metabolic, cardiovascular, orthopedic, neurological, hepatic, pulmonary, and renal disorders are also seen in association with childhood obesity.
Introduction
The world is undergoing a rapid epidemiological and nutritional transition characterized by persistent nutritional deficiencies, as evidenced by the prevalence of stunting, anemia, and iron and zinc deficiencies. Concomitantly, there is a progressive rise in the prevalence of obesity, diabetes and other nutrition related chronic diseases (NRCDs) like obesity, diabetes, cardiovascular disease, and some forms of cancer. Obesity has reached epidemic levels in developed countries. The highest prevalence rates of childhood obesity have been observed in developed countries; however, its prevalence is increasing in developing countries as well.[ 1 ] Females are more likely to be obese as compared to males, owing to inherent hormonal differences.[ 2 ]
It is emerging convincingly that the genesis of Type 2 Diabetes and Coronary Heart Disease begins in childhood, with childhood obesity serving as an important factor.[ 3 ] There has been a phenomenal rise in proportions of children having obesity in the last 4 decades, especially in the developed world. Studies emerging from different parts of India within last decade are also indicative of similar trend.[ 4 , 5 , 6 , 7 , 8 , 9 ] This view has been challenged over recent years and we presently consider these as different forms of the global malnutrition problem. This new conceptualization leads us to simultaneously address the root causes of nutritional deficiencies which in turn will contribute to the control of under nutrition and the prevention of obesity, diabetes, and other NRCDs. This summary provides a public health overview of selected key issues related to the prevention of obesity and chronic diseases with a life-course perspective of nutrition and child growth.
Childhood obesity is one of the most serious public health challenges of the 21 st century. The problem is global and is steadily affecting many low and middle income countries, particularly in urban settings. The prevalence has increased at an alarming rate. Globally in 2010, the number of overweight children under the age of five is estimated to be over 42 million. Close to 35 million of these are living in developing countries.
Definition of Childhood Obesity
Although definition of obesity and overweight has changed over time, it can be defined as an excess of body fat (BF). There is no consensus on a cut-off point for excess fatness of overweight or obesity in children and adolescents. A study by conducted by Williams et al . (1992), on 3,320 children in the age-group of 5–18 years classified children as fat if their percentage of body fat was at least 25% for males and 30% for females, respectively.[ 10 ] The Center for Disease Control and Prevention defined overweight as at or above the 95 th percentile of body mass index (BMI) for age and “at risk for overweight” as between 85 th to 95 th percentile of BMI for age.[ 11 , 12 ] European researchers classified overweight as at or above 85 th percentile and obesity as at or above 95 th percentile of BMI.[ 13 ]
An Indian research study has defined overweight and obesity as overweight (between ≥85 th and <95 th percentile) and obesity (≥95 th percentile).[ 14 ] Another study has followed World Health Organization 2007 growth reference for defining overweight and obesity.[ 15 ]
There are also several methods to measure the percentage of body fat. In research, techniques include underwater weighing (densitometry), multi-frequency bioelectrical impedance analysis (BIA), and magnetic resonance imaging (MRI). In the clinical environment, techniques such as BMI, waist circumference, and skin-fold thickness have been used extensively. Although, these methods are less accurate than research methods, they are satisfactory to identify risk. While BMI seems appropriate for differentiating adults, it may not be as useful in children because of their changing body shape as they progress through normal growth. In addition, BMI fails to distinguish between fat and fat-free mass (muscle and bone) and may exaggerate obesity in large muscular children. Furthermore, maturation pattern differs between genders and different ethnic groups. Studies that used BMI to identify overweight and obese children based on percentage of body fat have found high specificity (95–100%), but low sensitivity (36–66%) for this system of classification.[ 16 ] While health consequences of obesity are related to excess fatness, the ideal method of classification should be based on direct measurement of fatness. Although methods such as densitometry can be used in research practice, they are not feasible for clinical settings. For large population-based studies and clinical situations, bioelectrical impedance analysis (BIA) is widely used. Waist circumference seems to be more accurate for children because it targets central obesity, which is a risk factor for type II diabetes and coronary heart disease.
Causes of Childhood Obesity
It is widely accepted that increase in obesity results from an imbalance between energy intake and expenditure, with an increase in positive energy balance being closely associated with the lifestyle adopted and the dietary intake preferences. However, there is increasing evidence indicating that an individual's genetic background is important in determining obesity risk. Research has made important contributions to our understanding of the factors associated with obesity. The ecological model, as described by Davison et al ., suggests that child risk factors for obesity include dietary intake, physical activity, and sedentary behavior.[ 17 ] The impact of such risk factors is moderated by factors such as age, gender. Family characteristics parenting style, parents’ lifestyles also play a role. Environmental factors such as school policies, demographics, and parents’ work-related demands further influence eating and activity behaviors.
Genetics are one of the biggest factors examined as a cause of obesity. Some studies have found that BMI is 25–40% heritable.[ 18 ] However, genetic susceptibility often needs to be coupled with contributing environmental and behavioral factors in order to affect weight.[ 19 ] The genetic factor accounts for less than 5% of cases of childhood obesity.[ 18 ] Therefore, while genetics can play a role in the development of obesity, it is not the cause of the dramatic increase in childhood obesity.
Basal metabolic rate has also been studied as a possible cause of obesity. Basal metabolic rate, or metabolism, is the body's expenditure of energy for normal resting functions. Basal metabolic rate is accountable for 60% of total energy expenditure in sedentary adults. It has been hypothesized that obese individuals have lower basal metabolic rates. However, differences in basal metabolic rates are not likely to be responsible for the rising rates of obesity.[ 18 ]
Review of the literature investigates factors behind poor diet and offers numerous insights into how parental factors may impact on obesity in children.[ 20 ] They note that children learn by modeling parents’ and peers’ preferences, intake and willingness to try new foods. Availability of, and repeated exposure to, healthy foods is key to developing preferences and can overcome dislike of foods. Mealtime structure is important with evidence suggesting that families who eat together consume more healthy foods. Furthermore, eating out or watching TV while eating is associated with a higher intake of fat. Parental feeding style is also significant. The author's found that authoritative feeding (determining which foods are offered, allowing the child to choose, and providing rationale for healthy options) is associated with positive cognitions about healthy foods and healthier intake. Interestingly authoritarian restriction of “junk-food” is associated with increased desire for unhealthy food and higher weight.[ 21 ]
Government and social policies could also potentially promote healthy behavior. Research indicates taste, followed by hunger and price, is the most important factor in adolescents snack choices.[ 22 ] Other studies demonstrate that adolescents associate junk food with pleasure, independence, and convenience, whereas liking healthy food is considered odd.[ 23 ] This suggests investment is required in changing meanings of food, and social perceptions of eating behavior. As proposed by the National Taskforce on Obesity (2005), fiscal policies such as taxing unhealthy options, providing incentives for the distribution of inexpensive healthy food, and investing in convenient recreational facilities or the esthetic quality of neighborhoods can enhance healthy eating and physical activity.[ 24 ]
Dietary factors have been studied extensively for its possible contributions to the rising rates of obesity. The dietary factors that have been examined include fast food consumption, sugary beverages, snack foods, and portion sizes.
Fast food Consumption: Increased fast food consumption has been linked with obesity in the recent years. Many families, especially those with two parents working outside the home, opt for these places as they are often favored by their children and are both convenient and inexpensive.[ 25 ] Foods served at fast food restaurants tend to contain a high number of calories with low nutritional values. A study conducted examined the eating habits of lean and overweight adolescents at fast food restaurants.[ 26 ] Researchers found that both groups consumed more calories eating fast food than they would typically in a home setting but the lean group compensated for the higher caloric intake by adjusting their caloric intake before or after the fast food meal in anticipation or compensation for the excess calories consumed during the fast food meal. Though many studies have shown weight gain with regular consumption of fast food, it is difficult to establish a causal relationship between fast food and obesity.
Sugary beverages
A study examining children aged 9–14 from 1996–1998, found that consumption of sugary beverages increased BMI by small amounts over the years.[ 18 ] Sugary drinks are another factor that has been examined as a potential contributing factor to obesity. Sugary drinks are often thought of as being limited to soda, but juice and other sweetened beverages fall into this category. Many studies have examined the link between sugary drink consumption and weight and it has been continually found to be a contributing factor to being overweight.[ 18 ] Sugary drinks are less filling than food and can be consumed quicker, which results in a higher caloric intake.[ 19 ]
Snack foods
Another factor that has been studied as a possible contributing factor of childhood obesity is the consumption of snack foods. Snack foods include foods such as chips, baked goods, and candy. Many studies have been conducted to examine whether these foods have contributed to the increase in childhood obesity. While snacking has been shown to increase overall caloric intake, no studies have been able to find a link between snacking and overweight.[ 18 ]
Portion size
Portion sizes have increased drastically in the past decade. Consuming large portions, in addition to frequent snacking on highly caloric foods, contribute to an excessive caloric intake. This energy imbalance can cause weight gain, and consequently obesity.[ 18 ]
Activity level
One of the factors that is most significantly linked to obesity is a sedentary lifestyle. Each additional hour of television per day increased the prevalence of obesity by 2%.[ 18 ] Television viewing among young children and adolescents has increased dramatically in recent years.[ 18 , 27 ] The increased amount of time spent in sedentary behaviors has decreased the amount of time spent in physical activity. Research which indicates the number of hours children spend watching TV correlates with their consumption of the most advertised goods, including sweetened cereals, sweets, sweetened beverages, and salty snacks.[ 22 ] Despite difficulties in empirically assessing the media impact, other research discussed emphasizes that advertising effects should not be underestimated. Media effects have been found for adolescent aggression and smoking and formation of unrealistic body ideals. Regulation of marketing for unhealthy foods is recommended, as is media advocacy to promote healthy eating.
Environmental factors
While extensive television viewing and the use of other electronic media has contributed to the sedentary lifestyles, other environmental factors have reduced the opportunities for physical activity. Opportunities to be physically active and safe environments to be active in have decreased in the recent years. The majority of children in the past walked or rode their bike to school. A study conducted in 2002 found that 53% of parents drove their children to school.[ 18 ] Of these parents, 66% said they drove their children to school since their homes were too far away from the school. Other reasons parents gave for driving their children to school included no safe walking route, fear of child predators, and out of convenience for the child.[ 18 ] Children who live in unsafe areas or who do not have access to safe, well-lit walking routes have fewer opportunities to be physically active.[ 18 ]
Socio-cultural factors
Socio-cultural factors have also been found to influence the development of obesity. Our society tends to use food as a reward, as a means to control others, and as part of socializing.[ 28 ] These uses of food can encourage the development of unhealthy relationships with food, thereby increasing the risk of developing obesity.
Family factors
Family factors have also been associated with the increase of cases of obesity. The types of food available in the house and the food preferences of family members can influence the foods that children eat. In addition, family mealtimes can influence the type of food consumed and the amount thereof. Lastly, family habits, whether they are sedentary or physically active, influence the child.[ 28 ] Studies have shown that having an overweight mother and living in a single parent household are associated with overweight and childhood obesity.[ 29 ]
Psychological factors
Depression and anxiety.
A recent review concluded that the majority of studies find a prospective relationship between eating disturbances and depression.[ 30 ] However, this relationship is not unidirectional; depression may be both a cause and a consequence of obesity.[ 31 ] Additionally, in a clinical sample of obese adolescents, a higher life-time prevalence of anxiety disorders was reported compared to non-obese controls.[ 32 ] Although some studies demonstrate no significant relationship between increased BMI and increased anxiety symptoms.[ 33 ] Thus, the relationship between obesity and anxiety may not be unidirectional and is certainly not conclusive.
Self-esteem
Research findings comparing overweight/obese children with normal-weight children in regards to self-esteem have been mixed.[ 34 ] Some studies have found that obese children have lower self-esteem while others do not.[ 35 , 36 , 37 ] There is some consensus in the literature that the global approach to self-esteem measurement with children who are overweight/obese is misleading as the physical and social domains of self-esteem seem to be where these children are most vulnerable.[ 38 ]
Body dissatisfaction
Research has consistently found that body satisfaction is higher in males than females at all ages.[ 39 ] Gender differences may reflect the westernized cultural ideals of beauty in that thinness is the only culturally defined ideal for females, while males are encouraged to be both lean and muscular. Thus, there is a linear relationship between body dissatisfaction and increasing BMI for girls; while for boys a U-shaped relationship suggests that boys with BMIs at the low and high extremes experience high levels of body dissatisfaction.[ 40 , 41 ]
Eating disorder symptoms
Traits associated with eating disorders appear to be common in adolescent obese populations, particularly for girls.[ 42 ] A number of studies have shown higher prevalence of eating-related pathology (i.e. Anorexia, Bulimia Nervosa, and impulse regulation) in obese children/youth.[ 43 , 44 ]
Emotional problems
In one of the few studies to investigate the psychological impact of being overweight/obese in children, a review of 10 published studies over a 10-year period (1995-2005) with sample sizes greater than 50 revealed that all participants reported some level of psychosocial impact as a result of their weight status.[ 45 ] Being younger, female, and with an increased perceived lack of control over eating seemed to heighten the psychosocial consequences.
Consequences of childhood obesity
Childhood obesity can profoundly affect children's physical health, social, and emotional well-being, and self esteem. It is also associated with poor academic performance and a lower quality of life experienced by the child. These potential consequences are further examined in the following sections.
Medical consequences
Childhood obesity has been linked to numerous medical conditions. These conditions include, but are not limited to, fatty liver disease, sleep apnea, Type 2 diabetes, asthma, hepatic steatosis (fatty liver disease), cardiovascular disease, high cholesterol, cholelithiasis (gallstones), glucose intolerance and insulin resistance, skin conditions, menstrual abnormalities, impaired balance, and orthopedic problems.[ 25 , 46 ] Until recently, many of the above health conditions had only been found in adults; now they are extremely prevalent in obese children. Although most of the physical health conditions associated with childhood obesity are preventable and can disappear when a child or adolescent reaches a healthy weight, some continue to have negative consequences throughout adulthood.[ 46 ] In the worst cases, some of these health conditions can even result in death. Below, three of the more common health problems associated with childhood obesity are discussed, diabetes, sleep apnea, and cardiovascular disease.
Socio-emotional consequences
In addition to being implicated in numerous medical concerns, childhood obesity affects children's and adolescent's social and emotional health. Obesity has been described as being “one of the most stigmatizing and least socially acceptable conditions in childhood.”[ 38 ] Overweight and obese children are often teased and/or bullied for their weight. They also face numerous other hardships including negative stereotypes, discrimination, and social marginalization.[ 46 ] Discrimination against obese individuals has been found in children as young as 2 years old.[ 28 ] Obese children are often excluded from activities, particularly competitive activities that require physical activity. It is often difficult for overweight children to participate in physical activities as they tend to be slower than their peers and contend with shortness of breath.[ 25 ] These negative social problems contribute to low self esteem, low self confidence, and a negative body image in children and can also affect academic performance.[ 46 ] All of the above-mentioned negative effects of overweight and obesity can be devastating to children and adolescents.
The social consequences of obesity may contribute to continuing difficulty in weight management. Overweight children tend to protect themselves from negative comments and attitudes by retreating to safe places, such as their homes, where they may seek food as a comfort. In addition, children who are overweight tend to have fewer friends than normal weight children, which results in less social interaction and play, and more time spent in sedentary activities.[ 25 ] As aforementioned, physical activity is often more difficult for overweight and obese children as they tend to get shortness of breath and often have a hard time keeping up with their peers. This in turn inevitably results in weight gain, as the amount of calories consumed exceeds the amount of energy burned.[ 25 ]
Academic consequences
Childhood obesity has also been found to negatively affect school performance. A research study concluded that overweight and obese children were four times more likely to report having problems at school than their normal weight peers.[ 38 ] They are also more likely to miss school more frequently, especially those with chronic health conditions such as diabetes and asthma, which can also affect academic performance.
The growing issue of childhood obesity can be slowed, if society focuses on the causes. There are many components that play into childhood obesity, some being more crucial than others. A combined diet and physical activity intervention conducted in the community with a school component is more effective at preventing obesity or overweight. Moreover, if parents enforce a healthier lifestyle at home, many obesity problems could be avoided. What children learn at home about eating healthy, exercising and making the right nutritional choices will eventually spill over into other aspects of their life. This will have the biggest influence on the choices kids make when selecting foods to consume at school and fast-food restaurants and choosing to be active. Focusing on these causes may, over time, decrease childhood obesity and lead to a healthier society as a whole.
Source of Support: Nil.
Conflict of Interest: None declared.

IMAGES
COMMENTS
Moreover, effective action to prevent the childhood obesity epidemic requires evidence-based on early life risk factors, and this evidence, unfortunately, is still incomplete. Furthermore, a research study has attempted to capture the complete picture of childhood obesity early life course risk factors.
Society in general and primary care providers in particular are often highly biased toward people with obesity. 24 A study with obese children aged 9 to 11 years found implicit bias to be around 5%. 25 ... Future childhood obesity research should evaluate the best methods for educating primary care providers in providing family-centered care ...
Introduction. Childhood obesity is a major public health challenge, with one in three US children between the ages of 2 and 5 meeting criteria for overweight or obesity. 1 The urgency to reverse the course of childhood obesity has led to significant growth in the scientific literature evaluating childhood obesity interventions. Extant reviews of this research have provided limited guidance ...
The childhood obesity research that NIH supports includes studies in pregnancy, infancy, childhood, adolescence, and prevention and treatment approaches in families, schools, and other community settings, as well as in health care settings. The NIH also supports basic behavioral and social science research that is providing insights into ...
10.1542/6305605703112Video AbstractPEDS-VA_2021-0537086305605703112OBJECTIVES. Examine childhood obesity incidence across recent cohorts.METHODS. We examined obesity incidence and prevalence across 2 cohorts of children in the United States 12 years apart using the Early Childhood Longitudinal Studies, parallel data sets following the kindergarten cohorts of 1998 and 2010 with direct ...
This updated synthesis of obesity prevention interventions for children aged 6-18 years, found a small beneficial impact on child BMI for school-based obesity prevention interventions. A more comprehensive assessment of interventions is required to identify mechanisms of effective interventions to inform future obesity prevention public health policy, which may be particularly salient in for ...
This review summarizes the current evidence for the management of obesity in terms of medical and surgical options. Both future therapeutic agents and those which cause weight loss but have an alternative indication are also included and discussed as part of the review. The review summarizes the most recent research for each intervention and ...
To our knowledge, currently the largest genome-wide association study meta-analysis on childhood obesity in >13,000 individuals with obesity and >15,500 controls.
This Review describes current knowledge on the epidemiology and causes of child and adolescent obesity, considerations for assessment, and current management approaches. Before the COVID-19 pandemic, obesity prevalence in children and adolescents had plateaued in many high-income countries despite levels of severe obesity having increased. However, in low-income and middle-income countries ...
Keywords used included childhood obesity, adolescents, pharmacotherapy, metformin, orlistat, glucagon-like peptide 1, sibutramine, topiramate ... recommend this treatment due to the lack of long-term evidence and potential for overall high costs. 126 The Contrave Obesity Research I (COR-I) study included participants aged between 18 and 65 ...
Launched in 2009, the National Collaborative on Childhood Obesity Research (NCCOR) brings together four of the nation's leading research funders — the Centers for Disease Control and Prevention (CDC), the National Institutes of Health (NIH), the Robert Wood Johnson Foundation (RWJF), and the U.S. Department of Agriculture (USDA) — to accelerate progress in reducing childhood obesity in ...
Childhood obesity rates have increased substantially over the past year in the UK, according to a new report from the UK Government's National Child Measurement Programme. This rise in prevalence is the largest single-year increase since the programme began 15 years ago and highlights the worldwide rising trend for obesity among children and adolescents. Once considered a problem mainly in ...
10.1542/6305605698112Video AbstractPEDS-VA_2021-0555716305605698112BACKGROUND AND OBJECTIVES. Addressing food insecurity while promoting healthy body weights among children is a major public health challenge. Our objective is to examine longitudinal associations between food insecurity and obesity in US children aged 1 to 19 years.METHODS. Sources for this research include PubMed, CINAHL, and ...
With the creation of the Duke Center for Childhood Obesity Research (DCCOR) in January 2017 under the leadership of Eliana Perrin, MD, MPH, the Department of Pediatrics and School of Medicine strengthened its commitment to the multidisciplinary research necessary to develop effective and efficient evidence-based behavioral interventions to prevent childhood obesity.
Obesity is a complex condition that interweaves biological, developmental, environmental, behavioral, and genetic factors; it is a significant public health problem. The most common cause of obesity throughout childhood and adolescence is an inequity in energy balance; that is, excess caloric intake without appropriate caloric expenditure.
Childhood overweight and obesity is a serious public health issue with an increase being observed in preschool-aged children. Treating childhood obesity is difficult and few countries use standardized treatments. Therefore, there is a need to find effective approaches that are feasible for both health care providers and families. Thus, the overall aim of this study is to assess the acceptance ...
The Childhood Obesity Research Summit provided an overview of childhood obesity, and participants identified key questions that need to be answered, as well as recommendations for future work in the areas of education, public policy, and research. The recommendations and outcomes of the conference will help inform the American Heart Association ...
Despite national school and community-based efforts to promote healthy behaviors at a young age, childhood obesity is becoming more common in the United States, a recent study found.. The research ...
Childhood obesity. Approximately one third of the children and adolescents in the United States are either overweight or obese. Childhood obesity disproportionately affects specific racial and ethnic groups and households with low socioeconomic status and low parental education. The Alternative Learning Center (ALC) within Rochester School ...
Citation searching of relevant studies was also done. We found studies that estimated the potential effect of weight-management interventions on childhood obesity prevalence and modelling studies that estimated the effect of population-wide policies, such as fiscal interventions, on the prevalence of childhood obesity.
As shown in Table 2, one study from a prospective British birth cohort study, the National Child Development Study (NCDS) of 1958, examined the association between childhood neglect and MetS. Citation 65 There was no significant association (OR 1.08 95% CIs (0.89-1.32)) in individuals who were neglected in childhood in relation to MetS in ...
A novel study in the Journal of Investigative Dermatology details the findings of an analysis of 2,161,900 Korean children from 2009 to 2020 to investigate the relationship between obesity or ...
Rise in Childhood Obesity and Regulatory Challenges. Obesity in children aged two to five has more than doubled in the US since the 1970s, with approximately 13% of preschool children living with obesity. [3] This has only worsened since the COVID-19 pandemic. [4]
1. Introduction. In recent decades, the increase in the prevalence of childhood obesity has become a worldwide public health problem [1,2].Recent studies in the United States analyzed the prevalence of obesity in children and found that it increases with age such that at 14 years of age, 20.8% of children are obese and 17% are overweight [].In Spain, the Aladino study (2019), which analyzed ...
• Approved on May 23, 2013 - Revisions to the triceps skinfold measurement - when to collect 3rd measurement and when QC out of range. Changed 10mm to 20mm such that the revised
Countries in the Middle East have some of the lowest rates of physical activity and some of the highest rates of obesity in the world. Policies can influence population levels of physical activity. However, there is a dearth of research on physical activity policies in the Gulf region. This qualitative study analyses cross-sectoral barriers and facilitators for the development, implementation ...
The first iteration of the Childhood Obesity Research Demonstration Projects (CORD 1.0), a program of research administered by the CDC, examined multi-sector intervention implementation in schools, community centers, early care and health centers, and pediatric primary care practices. ... from the Study of Latino Youth and the Hispanic ...
Episode · The Out of the Cave Podcast · Welcome to the premier episode of the Out of the Cave Podcast hosted by Lisa Schlosberg, LMSW. This podcast is a resource for all who struggle with emotional eating, stress eating, undereating, overeating, mindless eating, weight gain, weight loss and have a complicated relationship to food, eating, and body image. Topics Include: Plato's "Allegory ...
Childhood obesity has also been found to negatively affect school performance. A research study concluded that overweight and obese children were four times more likely to report having problems at school than their normal weight peers. They are also more likely to miss school more frequently, especially those with chronic health conditions ...