

ANA Nursing Resources Hub
Search Resources Hub

Leadership in Nursing: Qualities & Why It Matters
4 min read • May, 19 2023
Strong leaders in nursing are vital to help navigate the constant evolution of health care. Nurse leaders do more than balance costs, monitor productivity, and maintain patient and staff satisfaction. They serve as role models and influence health care organizations at all levels. A strong nurse leader motivates their colleagues, setting the tone for a safe, civil workplace with a culture of high morale and job retention.
What Is a Nurse Leader?
A nurse leader is defined by their actions, and not always by a position of authority. Leaders in nursing inspire and influence others to achieve their maximum potential. They use applied leadership in nursing by drawing upon critical thinking skills to manage a team.
Nurse leaders take a broad view of how daily tasks impact the overall goals of the health care organization. They communicate expectations to their team and motivate them to achieve predetermined goals. Nurses can lead from various organizational areas if they project the necessary leadership qualities to influence others.
Leadership Qualities in Nursing
A nurse leader role combines essential nursing, business, and leadership skills developed through ongoing learning . They must be flexible enough to adapt to technological changes, fluctuating payment methods, new treatment modalities, and regulatory and legislative environments. Critical skills for effective nursing leadership include:
- Communication and Collaboration : These skills can reduce miscommunication, encourage shared decision making, and provide a sense of working together toward common goals.
- Education and Quality of Practice : Continued professional development allows leaders in nursing to keep pace with the ever-changing health care environment while striving for excellence by supporting quality, evidence-based practice.
- Environmental Health and Resource Utilization : Leadership in nursing ensures that patient care can be provided effectively in a safe and healthy environment while promoting wellness among all health care staff.
- Ethics and Professional Practice Evaluation : Influential nurse leaders model ethical practices to guide decisions, display honesty by being accountable for their actions, and evaluate their adherence to professional practice standards. Learn more about the Code of Ethics for Nurses .
- Professionalism and Leadership : Leaders in nursing build vital relationships and collaborate with various health care teams on sensitive topics. Using critical thinking skills allows those in nursing leadership roles to analyze decisions impacting the organization. They then clearly explain the rationale in a manner that encourages staff support.
Other nursing leadership skills, such as displaying compassion and empathy, can assist the nurse leader in developing interpersonal relationships and gaining respect in their role.
7 Leadership Styles in Nursing
Nursing leadership styles can impact job satisfaction , nurse retention rates , quality of care, and patient outcomes . The nurse’s educational background, personality, and work environment may influence their nursing leadership style. Each type of nurse leader role can be valuable when utilized in the right setting.
- The Transformational nurse leader works to inspire nurses to achieve a greater vision by helping with strength development. This nursing leadership style works well with mentoring.
- The Autocratic nurse leader makes quick decisions with little input from employees and excels at task delegation. This nursing leadership style may be most effective in an emergency.
- A Laissez-faire leadership style puts faith in every facet of a well-oiled machine. This method may work well with experienced teams or self-directed nurses.
- The Democratic nurse leader is collaborative and focuses on team success. This nurse leader might excel in quality improvement roles but may not be effective in situations requiring independent decisions.
- The Servant nurse leadership style focuses on employee development and individual needs. This method works well with goal-driven environments or as a nurse educator.
- The Situational leadership style is the most adaptable since it analyzes the situation and determines the appropriate approach. This nurse leader is flexible enough to modify their approach based on the organization or individual’s needs. This style works well with nursing students but may divert from the organization’s long-term goals.
- The Transactional nurse leader does well with short-term goals by focusing on efficiency and performance. This task-oriented style reduces errors and works well with tight deadlines.

Examples of Leadership in Nursing
Projecting leadership skills in nursing that influences others can allow a nurse to lead without being assigned a specific leadership position. The aspiring nurse leader might:
- Seek out a mentor or become one
- Volunteer for committee roles
- Become involved in the community
- Take educational courses
- Stay current on the latest health care trends
- Get involved with public policy
A nurse aspiring for a nursing leadership role can get a certification or obtain additional degrees specific to nursing leadership to increase their knowledge base and expand upon professional development. But a title and the education aren’t enough to create an effective leader. Nurses and other health care staff need to believe their contributions make a difference in the organization.
Why Is Nurse Leadership Important?
Nurse leaders make a difference in workplace culture and drive positive changes in health care legislation. When a team admires the qualities of their leader, it boosts morale and promotes a psychologically safe workplace, which leads to higher job satisfaction and retention rates. Influential leaders in nursing ensure that the organization's vision is communicated to the nursing staff while mentoring the nursing leadership of tomorrow .
Explore courses, webinars, and other nursing leadership and excellence resources offered by ANA .
Images sourced from Getty Images
You May Also Like
Specialty Certifications
Nurse Executive Certification (NE-BC®)
Price From: $395.00
ANA Member Price: $295.00
Nurse Executive, Advanced Certification (NEA-BC®)
Related Resources

Item(s) added to cart
- Open access
- Published: 03 July 2024
The impact of evidence-based nursing leadership in healthcare settings: a mixed methods systematic review
- Maritta Välimäki 1 , 2 ,
- Shuang Hu 3 ,
- Tella Lantta 1 ,
- Kirsi Hipp 1 , 4 ,
- Jaakko Varpula 1 ,
- Jiarui Chen 3 ,
- Gaoming Liu 5 ,
- Yao Tang 3 ,
- Wenjun Chen 3 &
- Xianhong Li 3
BMC Nursing volume 23 , Article number: 452 ( 2024 ) Cite this article
1431 Accesses
Metrics details
The central component in impactful healthcare decisions is evidence. Understanding how nurse leaders use evidence in their own managerial decision making is still limited. This mixed methods systematic review aimed to examine how evidence is used to solve leadership problems and to describe the measured and perceived effects of evidence-based leadership on nurse leaders and their performance, organizational, and clinical outcomes.
We included articles using any type of research design. We referred nurses, nurse managers or other nursing staff working in a healthcare context when they attempt to influence the behavior of individuals or a group in an organization using an evidence-based approach. Seven databases were searched until 11 November 2021. JBI Critical Appraisal Checklist for Quasi-experimental studies, JBI Critical Appraisal Checklist for Case Series, Mixed Methods Appraisal Tool were used to evaluate the Risk of bias in quasi-experimental studies, case series, mixed methods studies, respectively. The JBI approach to mixed methods systematic reviews was followed, and a parallel-results convergent approach to synthesis and integration was adopted.
Thirty-one publications were eligible for the analysis: case series ( n = 27), mixed methods studies ( n = 3) and quasi-experimental studies ( n = 1). All studies were included regardless of methodological quality. Leadership problems were related to the implementation of knowledge into practice, the quality of nursing care and the resource availability. Organizational data was used in 27 studies to understand leadership problems, scientific evidence from literature was sought in 26 studies, and stakeholders’ views were explored in 24 studies. Perceived and measured effects of evidence-based leadership focused on nurses’ performance, organizational outcomes, and clinical outcomes. Economic data were not available.
Conclusions
This is the first systematic review to examine how evidence is used to solve leadership problems and to describe its measured and perceived effects from different sites. Although a variety of perceptions and effects were identified on nurses’ performance as well as on organizational and clinical outcomes, available knowledge concerning evidence-based leadership is currently insufficient. Therefore, more high-quality research and clinical trial designs are still needed.
Trail registration
The study was registered (PROSPERO CRD42021259624).
Peer Review reports
Global health demands have set new roles for nurse leaders [ 1 ].Nurse leaders are referred to as nurses, nurse managers, or other nursing staff working in a healthcare context who attempt to influence the behavior of individuals or a group based on goals that are congruent with organizational goals [ 2 ]. They are seen as professionals “armed with data and evidence, and a commitment to mentorship and education”, and as a group in which “leaders innovate, transform, and achieve quality outcomes for patients, health care professionals, organizations, and communities” [ 3 ]. Effective leadership occurs when team members critically follow leaders and are motivated by a leader’s decisions based on the organization’s requests and targets [ 4 ]. On the other hand, problems caused by poor leadership may also occur, regarding staff relations, stress, sickness, or retention [ 5 ]. Therefore, leadership requires an understanding of different problems to be solved using synthesizing evidence from research, clinical expertise, and stakeholders’ preferences [ 6 , 7 ]. If based on evidence, leadership decisions, also referred as leadership decision making [ 8 ], could ensure adequate staffing [ 7 , 9 ] and to produce sufficient and cost-effective care [ 10 ]. However, nurse leaders still rely on their decision making on their personal [ 11 ] and professional experience [ 10 ] over research evidence, which can lead to deficiencies in the quality and safety of care delivery [ 12 , 13 , 14 ]. As all nurses should demonstrate leadership in their profession, their leadership competencies should be strengthened [ 15 ].
Evidence-informed decision-making, referred to as evidence appraisal and application, and evaluation of decisions [ 16 ], has been recognized as one of the core competencies for leaders [ 17 , 18 ]. The role of evidence in nurse leaders’ managerial decision making has been promoted by public authorities [ 19 , 20 , 21 ]. Evidence-based management, another concept related to evidence-based leadership, has been used as the potential to improve healthcare services [ 22 ]. It can guide nursing leaders, in developing working conditions, staff retention, implementation practices, strategic planning, patient care, and success of leadership [ 13 ]. Collins and Holton [ 23 ] in their systematic review and meta-analysis examined 83 studies regarding leadership development interventions. They found that leadership training can result in significant improvement in participants’ skills, especially in knowledge level, although the training effects varied across studies. Cummings et al. [ 24 ] reviewed 100 papers (93 studies) and concluded that participation in leadership interventions had a positive impact on the development of a variety of leadership styles. Clavijo-Chamorro et al. [ 25 ] in their review of 11 studies focused on leadership-related factors that facilitate evidence implementation: teamwork, organizational structures, and transformational leadership. The role of nurse managers was to facilitate evidence-based practices by transforming contexts to motivate the staff and move toward a shared vision of change.
As far as we are aware, however, only a few systematic reviews have focused on evidence-based leadership or related concepts in the healthcare context aiming to analyse how nurse leaders themselves uses evidence in the decision-making process. Young [ 26 ] targeted definitions and acceptance of evidence-based management (EBMgt) in healthcare while Hasanpoor et al. [ 22 ] identified facilitators and barriers, sources of evidence used, and the role of evidence in the process of decision making. Both these reviews concluded that EBMgt was of great importance but used limitedly in healthcare settings due to a lack of time, a lack of research management activities, and policy constraints. A review by Williams [ 27 ] showed that the usage of evidence to support management in decision making is marginal due to a shortage of relevant evidence. Fraser [ 28 ] in their review further indicated that the potential evidence-based knowledge is not used in decision making by leaders as effectively as it could be. Non-use of evidence occurs and leaders base their decisions mainly on single studies, real-world evidence, and experts’ opinions [ 29 ]. Systematic reviews and meta-analyses rarely provide evidence of management-related interventions [ 30 ]. Tate et al. [ 31 ] concluded based on their systematic review and meta-analysis that the ability of nurse leaders to use and critically appraise research evidence may influence the way policy is enacted and how resources and staff are used to meet certain objectives set by policy. This can further influence staff and workforce outcomes. It is therefore important that nurse leaders have the capacity and motivation to use the strongest evidence available to effect change and guide their decision making [ 27 ].
Despite of a growing body of evidence, we found only one review focusing on the impact of evidence-based knowledge. Geert et al. [ 32 ] reviewed literature from 2007 to 2016 to understand the elements of design, delivery, and evaluation of leadership development interventions that are the most reliably linked to outcomes at the level of the individual and the organization, and that are of most benefit to patients. The authors concluded that it is possible to improve individual-level outcomes among leaders, such as knowledge, motivation, skills, and behavior change using evidence-based approaches. Some of the most effective interventions included, for example, interactive workshops, coaching, action learning, and mentoring. However, these authors found limited research evidence describing how nurse leaders themselves use evidence to support their managerial decisions in nursing and what the outcomes are.
To fill the knowledge gap and compliment to existing knowledgebase, in this mixed methods review we aimed to (1) examine what leadership problems nurse leaders solve using an evidence-based approach and (2) how they use evidence to solve these problems. We also explored (3) the measured and (4) perceived effects of the evidence-based leadership approach in healthcare settings. Both qualitative and quantitative components of the effects of evidence-based leadership were examined to provide greater insights into the available literature [ 33 ]. Together with the evidence-based leadership approach, and its impact on nursing [ 34 , 35 ], this knowledge gained in this review can be used to inform clinical policy or organizational decisions [ 33 ]. The study is registered (PROSPERO CRD42021259624). The methods used in this review were specified in advance and documented in a priori in a published protocol [ 36 ]. Key terms of the review and the search terms are defined in Table 1 (population, intervention, comparison, outcomes, context, other).
In this review, we used a mixed methods approach [ 37 ]. A mixed methods systematic review was selected as this approach has the potential to produce direct relevance to policy makers and practitioners [ 38 ]. Johnson and Onwuegbuzie [ 39 ] have defined mixed methods research as “the class of research in which the researcher mixes or combines quantitative and qualitative research techniques, methods, approaches, concepts or language into a single study.” Therefore, we combined quantitative and narrative analysis to appraise and synthesize empirical evidence, and we held them as equally important in informing clinical policy or organizational decisions [ 34 ]. In this review, a comprehensive synthesis of quantitative and qualitative data was performed first and then discussed in discussion part (parallel-results convergent design) [ 40 ]. We hoped that different type of analysis approaches could complement each other and deeper picture of the topic in line with our research questions could be gained [ 34 ].
Inclusion and exclusion criteria
Inclusion and exclusion criteria of the study are described in Table 1 .
Search strategy
A three-step search strategy was utilized. First, an initial limited search with #MEDLINE was undertaken, followed by analysis of the words used in the title, abstract, and the article’s key index terms. Second, the search strategy, including identified keywords and index terms, was adapted for each included data base and a second search was undertaken on 11 November 2021. The full search strategy for each database is described in Additional file 1 . Third, the reference list of all studies included in the review were screened for additional studies. No year limits or language restrictions were used.
Information sources
The database search included the following: CINAHL (EBSCO), Cochrane Library (academic database for medicine and health science and nursing), Embase (Elsevier), PsycINFO (EBSCO), PubMed (MEDLINE), Scopus (Elsevier) and Web of Science (academic database across all scientific and technical disciplines, ranging from medicine and social sciences to arts and humanities). These databases were selected as they represent typical databases in health care context. Subject headings from each of the databases were included in the search strategies. Boolean operators ‘AND’ and ‘OR’ were used to combine the search terms. An information specialist from the University of Turku Library was consulted in the formation of the search strategies.
Study selection
All identified citations were collated and uploaded into Covidence software (Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia www.covidence.org ), and duplicates were removed by the software. Titles and abstracts were screened and assessed against the inclusion criteria independently by two reviewers out of four, and any discrepancies were resolved by the third reviewer (MV, KH, TL, WC). Studies meeting the inclusion criteria were retrieved in full and archived in Covidence. Access to one full-text article was lacking: the authors for one study were contacted about the missing full text, but no full text was received. All remaining hits of the included studies were retrieved and assessed independently against the inclusion criteria by two independent reviewers of four (MV, KH, TL, WC). Studies that did not meet the inclusion criteria were excluded, and the reasons for exclusion were recorded in Covidence. Any disagreements that arose between the reviewers were resolved through discussions with XL.
Assessment of methodological quality
Eligible studies were critically appraised by two independent reviewers (YT, SH). Standardized critical appraisal instruments based on the study design were used. First, quasi-experimental studies were assessed using the JBI Critical Appraisal Checklist for Quasi-experimental studies [ 44 ]. Second, case series were assessed using the JBI Critical Appraisal Checklist for Case Series [ 45 ]. Third, mixed methods studies were appraised using the Mixed Methods Appraisal Tool [ 46 ].
To increase inter-reviewer reliability, the review agreement was calculated (SH) [ 47 ]. A kappa greater than 0.8 was considered to represent a high level of agreement (0–0.1). In our data, the agreement was 0.75. Discrepancies raised between two reviewers were resolved through discussion and modifications and confirmed by XL. As an outcome, studies that met the inclusion criteria were proceeded to critical appraisal and assessed as suitable for inclusion in the review. The scores for each item and overall critical appraisal scores were presented.
Data extraction
For data extraction, specific tables were created. First, study characteristics (author(s), year, country, design, number of participants, setting) were extracted by two authors independently (JC, MV) and reviewed by TL. Second, descriptions of the interventions were extracted by two reviewers (JV, JC) using the structure of the TIDIeR (Template for Intervention Description and Replication) checklist (brief name, the goal of the intervention, material and procedure, models of delivery and location, dose, modification, adherence and fidelity) [ 48 ]. The extractions were confirmed (MV).
Third, due to a lack of effectiveness data and a wide heterogeneity between study designs and presentation of outcomes, no attempt was made to pool the quantitative data statistically; the findings of the quantitative data were presented in narrative form only [ 44 ]. The separate data extraction tables for each research question were designed specifically for this study. For both qualitative (and a qualitative component of mixed-method studies) and quantitative studies, the data were extracted and tabulated into text format according to preplanned research questions [ 36 ]. To test the quality of the tables and the data extraction process, three authors independently extracted the data from the first five studies (in alphabetical order). After that, the authors came together to share and determine whether their approaches of the data extraction were consistent with each other’s output and whether the content of each table was in line with research question. No reason was found to modify the data extraction tables or planned process. After a consensus of the data extraction process was reached, the data were extracted in pairs by independent reviewers (WC, TY, SH, GL). Any disagreements that arose between the reviewers were resolved through discussion and with a third reviewer (MV).
Data analysis
We were not able to conduct a meta-analysis due to a lack of effectiveness data based on clinical trials. Instead, we used inductive thematic analysis with constant comparison to answer the research question [ 46 , 49 ] using tabulated primary data from qualitative and quantitative studies as reported by the original authors in narrative form only [ 47 ]. In addition, the qualitizing process was used to transform quantitative data to qualitative data; this helped us to convert the whole data into themes and categories. After that we used the thematic analysis for the narrative data as follows. First, the text was carefully read, line by line, to reveal topics answering each specific review question (MV). Second, the data coding was conducted, and the themes in the data were formed by data categorization. The process of deriving the themes was inductive based on constant comparison [ 49 ]. The results of thematic analysis and data categorization was first described in narrative format and then the total number of studies was calculated where the specific category was identified (%).
Stakeholder involvement
The method of reporting stakeholders’ involvement follows the key components by [ 50 ]: (1) people involved, (2) geographical location, (3) how people were recruited, (4) format of involvement, (5) amount of involvement, (6) ethical approval, (7) financial compensation, and (8) methods for reporting involvement.
In our review, stakeholder involvement targeted nurses and nurse leader in China. Nurse Directors of two hospitals recommended potential participants who received a personal invitation letter from researchers to participate in a discussion meeting. Stakeholders’ participation was based on their own free will. Due to COVID-19, one online meeting (1 h) was organized (25 May 2022). Eleven participants joined the meeting. Ethical approval was not applied and no financial compensation was offered. At the end of the meeting, experiences of stakeholders’ involvement were explored.
The meeting started with an introductory presentation with power points. The rationale, methods, and preliminary review results were shared with the participants [ 51 ].The meeting continued with general questions for the participants: (1) Are you aware of the concepts of evidence-based practice or evidence-based leadership?; (2) How important is it to use evidence to support decisions among nurse leaders?; (3) How is the evidence-based approach used in hospital settings?; and (4) What type of evidence is currently used to support nurse leaders’ decision making (e.g. scientific literature, organizational data, stakeholder views)?
Two people took notes on the course and content of the conversation. The notes were later transcripted in verbatim, and the key points of the discussions were summarised. Although answers offered by the stakeholders were very short, the information was useful to validate the preliminary content of the results, add the rigorousness of the review, and obtain additional perspectives. A recommendation of the stakeholders was combined in the Discussion part of this review increasing the applicability of the review in the real world [ 50 ]. At the end of the discussion, the value of stakeholders’ involvement was asked. Participants shared that the experience of participating was unique and the topic of discussion was challenging. Two authors of the review group further represented stakeholders by working together with the research team throughout the review study.
Search results
From seven different electronic databases, 6053 citations were identified as being potentially relevant to the review. Then, 3133 duplicates were removed by an automation tool (Covidence: www.covidence.org ), and one was removed manually. The titles and abstracts of 3040 of citations were reviewed, and a total of 110 full texts were included (one extra citation was found on the reference list but later excluded). Based on the eligibility criteria, 31 studies (32 hits) were critically appraised and deemed suitable for inclusion in the review. The search results and selection process are presented in the PRISMA [ 52 ] flow diagram Fig. 1 . The full list of references for included studies can be find in Additional file 2 . To avoid confusion between articles of the reference list and studies included in the analysis, the studies included in the review are referred inside the article using the reference number of each study (e.g. ref 1, ref 2).
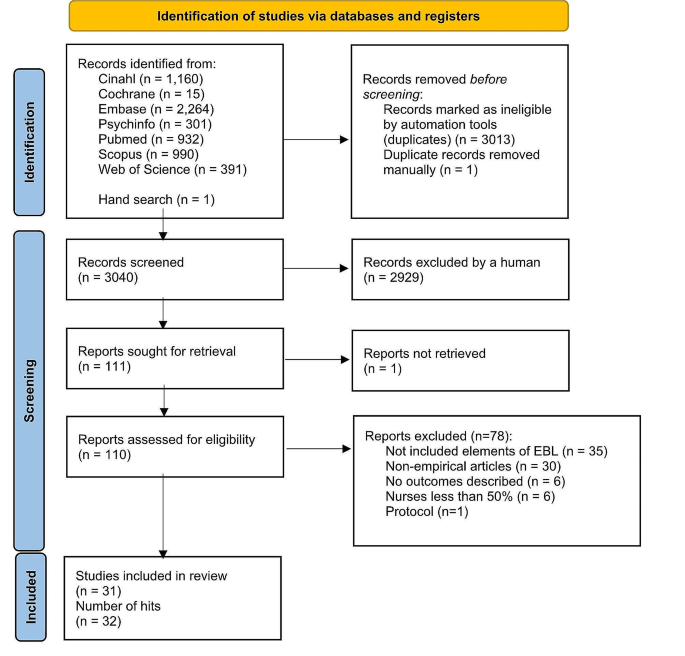
Search results and study selection and inclusion process [ 52 ]
Characteristics of included studies
The studies had multiple purposes, aiming to develop practice, implement a new approach, improve quality, or to develop a model. The 31 studies (across 32 hits) were case series studies ( n = 27), mixed methods studies ( n = 3) and a quasi-experimental study ( n = 1). All studies were published between the years 2004 and 2021. The highest number of papers was published in year 2020.
Table 2 describes the characteristics of included studies and Additional file 3 offers a narrative description of the studies.
Methodological quality assessment
Quasi-experimental studies.
We had one quasi-experimental study (ref 31). All questions in the critical appraisal tool were applicable. The total score of the study was 8 (out of a possible 9). Only one response of the tool was ‘no’ because no control group was used in the study (see Additional file 4 for the critical appraisal of included studies).
Case series studies . A case series study is typically defined as a collection of subjects with common characteristics. The studies do not include a comparison group and are often based on prevalent cases and on a sample of convenience [ 53 ]. Munn et al. [ 45 ] further claim that case series are best described as observational studies, lacking experimental and randomized characteristics, being descriptive studies, without a control or comparator group. Out of 27 case series studies included in our review, the critical appraisal scores varied from 1 to 9. Five references were conference abstracts with empirical study results, which were scored from 1 to 3. Full reports of these studies were searched in electronic databases but not found. Critical appraisal scores for the remaining 22 studies ranged from 1 to 9 out of a possible score of 10. One question (Q3) was not applicable to 13 studies: “Were valid methods used for identification of the condition for all participants included in the case series?” Only two studies had clearly reported the demographic of the participants in the study (Q6). Twenty studies met Criteria 8 (“Were the outcomes or follow-up results of cases clearly reported?”) and 18 studies met Criteria 7 (“Q7: Was there clear reporting of clinical information of the participants?”) (see Additional file 4 for the critical appraisal of included studies).
Mixed-methods studies
Mixed-methods studies involve a combination of qualitative and quantitative methods. This is a common design and includes convergent design, sequential explanatory design, and sequential exploratory design [ 46 ]. There were three mixed-methods studies. The critical appraisal scores for the three studies ranged from 60 to 100% out of a possible 100%. Two studies met all the criteria, while one study fulfilled 60% of the scored criteria due to a lack of information to understand the relevance of the sampling strategy well enough to address the research question (Q4.1) or to determine whether the risk of nonresponse bias was low (Q4.4) (see Additional file 4 for the critical appraisal of included studies).
Intervention or program components
The intervention of program components were categorized and described using the TiDier checklist: name and goal, theory or background, material, procedure, provider, models of delivery, location, dose, modification, and adherence and fidelity [ 48 ]. A description of intervention in each study is described in Additional file 5 and a narrative description in Additional file 6 .
Leadership problems
In line with the inclusion criteria, data for the leadership problems were categorized in all 31 included studies (see Additional file 7 for leadership problems). Three types of leadership problems were identified: implementation of knowledge into practice, the quality of clinical care, and resources in nursing care. A narrative summary of the results is reported below.
Implementing knowledge into practice
Eleven studies (35%) aimed to solve leadership problems related to implementation of knowledge into practice. Studies showed how to support nurses in evidence-based implementation (EBP) (ref 3, ref 5), how to engage nurses in using evidence in practice (ref 4), how to convey the importance of EBP (ref 22) or how to change practice (ref 4). Other problems were how to facilitate nurses to use guideline recommendations (ref 7) and how nurses can make evidence-informed decisions (ref 8). General concerns also included the linkage between theory and practice (ref 1) as well as how to implement the EBP model in practice (ref 6). In addition, studies were motivated by the need for revisions or updates of protocols to improve clinical practice (ref 10) as well as the need to standardize nursing activities (ref 11, ref 14).
The quality of the care
Thirteen (42%) focused on solving problems related to the quality of clinical care. In these studies, a high number of catheter infections led a lack of achievement of organizational goals (ref 2, ref 9). A need to reduce patient symptoms in stem cell transplant patients undergoing high-dose chemotherapy (ref 24) was also one of the problems to be solved. In addition, the projects focused on how to prevent pressure ulcers (ref 26, ref 29), how to enhance the quality of cancer treatment (ref 25) and how to reduce the need for invasive constipation treatment (ref 30). Concerns about patient safety (ref 15), high fall rates (ref 16, ref 19), dissatisfaction of patients (ref 16, ref 18) and nurses (ref 16, ref 30) were also problems that had initiated the projects. Studies addressed concerns about how to promote good contingency care in residential aged care homes (ref 20) and about how to increase recognition of human trafficking problems in healthcare (ref 21).
Resources in nursing care
Nurse leaders identified problems in their resources, especially in staffing problems. These problems were identified in seven studies (23%), which involved concerns about how to prevent nurses from leaving the job (ref 31), how to ensure appropriate recruitment, staffing and retaining of nurses (ref 13) and how to decrease nurses’ burden and time spent on nursing activities (ref 12). Leadership turnover was also reported as a source of dissatisfaction (ref 17); studies addressed a lack of structured transition and training programs, which led to turnover (ref 23), as well as how to improve intershift handoff among nurses (ref 28). Optimal design for new hospitals was also examined (ref 27).
Main features of evidence-based leadership
Out of 31 studies, 17 (55%) included all four domains of an evidence-based leadership approach, and four studies (13%) included evidence of critical appraisal of the results (see Additional file 8 for the main features of evidence-based Leadership) (ref 11, ref 14, ref 23, ref 27).
Organizational evidence
Twenty-seven studies (87%) reported how organizational evidence was collected and used to solve leadership problems (ref 2). Retrospective chart reviews (ref 5), a review of the extent of specific incidents (ref 19), and chart auditing (ref 7, ref 25) were conducted. A gap between guideline recommendations and actual care was identified using organizational data (ref 7) while the percentage of nurses’ working time spent on patient care was analyzed using an electronic charting system (ref 12). Internal data (ref 22), institutional data, and programming metrics were also analyzed to understand the development of the nurse workforce (ref 13).
Surveys (ref 3, ref 25), interviews (ref 3, ref 25) and group reviews (ref 18) were used to better understand the leadership problem to be solved. Employee opinion surveys on leadership (ref 17), a nurse satisfaction survey (ref 30) and a variety of reporting templates were used for the data collection (ref 28) reported. Sometimes, leadership problems were identified by evidence facilitators or a PI’s team who worked with staff members (ref 15, ref 17). Problems in clinical practice were also identified by the Nursing Professional Council (ref 14), managers (ref 26) or nurses themselves (ref 24). Current practices were reviewed (ref 29) and a gap analysis was conducted (ref 4, ref 16, ref 23) together with SWOT analysis (ref 16). In addition, hospital mission and vision statements, research culture established and the proportion of nursing alumni with formal EBP training were analyzed (ref 5). On the other hand, it was stated that no systematic hospital-specific sources of data regarding job satisfaction or organizational commitment were used (ref 31). In addition, statements of organizational analysis were used on a general level only (ref 1).
Scientific evidence identified
Twenty-six studies (84%) reported the use of scientific evidence in their evidence-based leadership processes. A literature search was conducted (ref 21) and questions, PICO, and keywords were identified (ref 4) in collaboration with a librarian. Electronic databases, including PubMed (ref 14, ref 31), Cochrane, and EMBASE (ref 31) were searched. Galiano (ref 6) used Wiley Online Library, Elsevier, CINAHL, Health Source: Nursing/Academic Edition, PubMed, and the Cochrane Library while Hoke (ref 11) conducted an electronic search using CINAHL and PubMed to retrieve articles.
Identified journals were reviewed manually (ref 31). The findings were summarized using ‘elevator speech’ (ref 4). In a study by Gifford et al. (ref 9) evidence facilitators worked with participants to access, appraise, and adapt the research evidence to the organizational context. Ostaszkiewicz (ref 20) conducted a scoping review of literature and identified and reviewed frameworks and policy documents about the topic and the quality standards. Further, a team of nursing administrators, directors, staff nurses, and a patient representative reviewed the literature and made recommendations for practice changes.
Clinical practice guidelines were also used to offer scientific evidence (ref 7, ref 19). Evidence was further retrieved from a combination of nursing policies, guidelines, journal articles, and textbooks (ref 12) as well as from published guidelines and literature (ref 13). Internal evidence, professional practice knowledge, relevant theories and models were synthesized (ref 24) while other study (ref 25) reviewed individual studies, synthesized with systematic reviews or clinical practice guidelines. The team reviewed the research evidence (ref 3, ref 15) or conducted a literature review (ref 22, ref 28, ref 29), a literature search (ref 27), a systematic review (ref 23), a review of the literature (ref 30) or ‘the scholarly literature was reviewed’ (ref 18). In addition, ‘an extensive literature review of evidence-based best practices was carried out’ (ref 10). However, detailed description how the review was conducted was lacking.
Views of stakeholders
A total of 24 studies (77%) reported methods for how the views of stakeholders, i.e., professionals or experts, were considered. Support to run this study was received from nursing leadership and multidisciplinary teams (ref 29). Experts and stakeholders joined the study team in some cases (ref 25, ref 30), and in other studies, their opinions were sought to facilitate project success (ref 3). Sometimes a steering committee was formed by a Chief Nursing Officer and Clinical Practice Specialists (ref 2). More specifically, stakeholders’ views were considered using interviews, workshops and follow-up teleconferences (ref 7). The literature review was discussed with colleagues (ref 11), and feedback and support from physicians as well as the consensus of staff were sought (ref 16).
A summary of the project findings and suggestions for the studies were discussed at 90-minute weekly meetings by 11 charge nurses. Nurse executive directors were consulted over a 10-week period (ref 31). An implementation team (nurse, dietician, physiotherapist, occupational therapist) was formed to support the implementation of evidence-based prevention measures (ref 26). Stakeholders volunteered to join in the pilot implementation (ref 28) or a stakeholder team met to determine the best strategy for change management, shortcomings in evidence-based criteria were discussed, and strategies to address those areas were planned (ref 5). Nursing leaders, staff members (ref 22), ‘process owners (ref 18) and program team members (ref 18, ref 19, ref 24) met regularly to discuss the problems. Critical input was sought from clinical educators, physicians, nutritionists, pharmacists, and nurse managers (ref 24). The unit director and senior nursing staff reviewed the contents of the product, and the final version of clinical pathways were reviewed and approved by the Quality Control Commission of the Nursing Department (ref 12). In addition, two co-design workshops with 18 residential aged care stakeholders were organized to explore their perspectives about factors to include in a model prototype (ref 20). Further, an agreement of stakeholders in implementing continuous quality services within an open relationship was conducted (ref 1).
Critical appraisal
In five studies (16%), a critical appraisal targeting the literature search was carried out. The appraisals were conducted by interns and teams who critiqued the evidence (ref 4). In Hoke’s study, four areas that had emerged in the literature were critically reviewed (ref 11). Other methods were to ‘critically appraise the search results’ (ref 14). Journal club team meetings (ref 23) were organized to grade the level and quality of evidence and the team ‘critically appraised relevant evidence’ (ref 27). On the other hand, the studies lacked details of how the appraisals were done in each study.
The perceived effects of evidence-based leadership
Perceived effects of evidence-based leadership on nurses’ performance.
Eleven studies (35%) described perceived effects of evidence-based leadership on nurses’ performance (see Additional file 9 for perceived effects of evidence-based leadership), which were categorized in four groups: awareness and knowledge, competence, ability to understand patients’ needs, and engagement. First, regarding ‘awareness and knowledge’, different projects provided nurses with new learning opportunities (ref 3). Staff’s knowledge (ref 20, ref 28), skills, and education levels improved (ref 20), as did nurses’ knowledge comprehension (ref 21). Second, interventions and approaches focusing on management and leadership positively influenced participants’ competence level to improve the quality of services. Their confidence level (ref 1) and motivation to change practice increased, self-esteem improved, and they were more positive and enthusiastic in their work (ref 22). Third, some nurses were relieved that they had learned to better handle patients’ needs (ref 25). For example, a systematic work approach increased nurses’ awareness of the patients who were at risk of developing health problems (ref 26). And last, nurse leaders were more engaged with staff, encouraging them to adopt the new practices and recognizing their efforts to change (ref 8).
Perceived effects on organizational outcomes
Nine studies (29%) described the perceived effects of evidence-based leadership on organizational outcomes (see Additional file 9 for perceived effects of evidence-based leadership). These were categorized into three groups: use of resources, staff commitment, and team effort. First, more appropriate use of resources was reported (ref 15, ref 20), and working time was more efficiently used (ref 16). In generally, a structured approach made implementing change more manageable (ref 1). On the other hand, in the beginning of the change process, the feedback from nurses was unfavorable, and they experienced discomfort in the new work style (ref 29). New approaches were also perceived as time consuming (ref 3). Second, nurse leaders believed that fewer nursing staff than expected left the organization over the course of the study (ref 31). Third, the project helped staff in their efforts to make changes, and it validated the importance of working as a team (ref 7). Collaboration and support between the nurses increased (ref 26). On the other hand, new work style caused challenges in teamwork (ref 3).
Perceived effects on clinical outcomes
Five studies (16%) reported the perceived effects of evidence-based leadership on clinical outcomes (see Additional file 9 for perceived effects of evidence-based leadership), which were categorized in two groups: general patient outcomes and specific clinical outcomes. First, in general, the project assisted in connecting the guideline recommendations and patient outcomes (ref 7). The project was good for the patients in general, and especially to improve patient safety (ref 16). On the other hand, some nurses thought that the new working style did not work at all for patients (ref 28). Second, the new approach used assisted in optimizing patients’ clinical problems and person-centered care (ref 20). Bowel management, for example, received very good feedback (ref 30).
The measured effects of evidence-based leadership
The measured effects on nurses’ performance.
Data were obtained from 20 studies (65%) (see Additional file 10 for measured effects of evidence-based leadership) and categorized nurse performance outcomes for three groups: awareness and knowledge, engagement, and satisfaction. First, six studies (19%) measured the awareness and knowledge levels of participants. Internship for staff nurses was beneficial to help participants to understand the process for using evidence-based practice and to grow professionally, to stimulate for innovative thinking, to give knowledge needed to use evidence-based practice to answer clinical questions, and to make possible to complete an evidence-based practice project (ref 3). Regarding implementation program of evidence-based practice, those with formal EBP training showed an improvement in knowledge, attitude, confidence, awareness and application after intervention (ref 3, ref 11, ref 20, ref 23, ref 25). On the contrary, in other study, attitude towards EBP remained stable ( p = 0.543). and those who applied EBP decreased although no significant differences over the years ( p = 0.879) (ref 6).
Second, 10 studies (35%) described nurses’ engagement to new practices (ref 5, ref 6, ref 7, ref 10, ref 16, ref 17, ref 18, ref 21, ref 25, ref 27). 9 studies (29%) studies reported that there was an improvement of compliance level of participants (ref 6, ref 7, ref 10, ref 16, ref 17, ref 18, ref 21, ref 25, ref 27). On the contrary, in DeLeskey’s (ref 5) study, although improvement was found in post-operative nausea and vomiting’s (PONV) risk factors documented’ (2.5–63%), and ’risk factors communicated among anaesthesia and surgical staff’ (0–62%), the improvement did not achieve the goal. The reason was a limited improvement was analysed. It was noted that only those patients who had been seen by the pre-admission testing nurse had risk assessments completed. Appropriate treatment/prophylaxis increased from 69 to 77%, and from 30 to 49%; routine assessment for PONV/rescue treatment 97% and 100% was both at 100% following the project. The results were discussed with staff but further reasons for a lack of engagement in nursing care was not reported.
And third, six studies (19%) reported nurses’ satisfaction with project outcomes. The study results showed that using evidence in managerial decisions improved nurses’ satisfaction and attitudes toward their organization ( P < 0.05) (ref 31). Nurses’ overall job satisfaction improved as well (ref 17). Nurses’ satisfaction with usability of the electronic charting system significantly improved after introduction of the intervention (ref 12). In handoff project in seven hospitals, improvement was reported in all satisfaction indicators used in the study although improvement level varied in different units (ref 28). In addition, positive changes were reported in nurses’ ability to autonomously perform their job (“How satisfied are you with the tools and resources available for you treat and prevent patient constipation?” (54%, n = 17 vs. 92%, n = 35, p < 0.001) (ref 30).
The measured effects on organizational outcomes
Thirteen studies (42%) described the effects of a project on organizational outcomes (see Additional file 10 for measured effects of evidence-based leadership), which were categorized in two groups: staff compliance, and changes in practices. First, studies reported improved organizational outcomes due to staff better compliance in care (ref 4, ref 13, ref 17, ref 23, ref 27, ref 31). Second, changes in organization practices were also described (ref 11) like changes in patient documentation (ref 12, ref 21). Van Orne (ref 30) found a statistically significant reduction in the average rate of invasive medication administration between pre-intervention and post-intervention ( p = 0.01). Salvador (ref 24) also reported an improvement in a proactive approach to mucositis prevention with an evidence-based oral care guide. On the contrary, concerns were also raised such as not enough time for new bedside report (ref 16) or a lack of improvement of assessment of diabetic ulcer (ref 8).
The measured effects on clinical outcomes
A variety of improvements in clinical outcomes were reported (see Additional file 10 for measured effects of evidence-based leadership): improvement in patient clinical status and satisfaction level. First, a variety of improvement in patient clinical status was reported. improvement in Incidence of CAUTI decreased 27.8% between 2015 and 2019 (ref 2) while a patient-centered quality improvement project reduced CAUTI rates to 0 (ref 10). A significant decrease in transmission rate of MRSA transmission was also reported (ref 27) and in other study incidences of CLABSIs dropped following of CHG bathing (ref 14). Further, it was possible to decrease patient nausea from 18 to 5% and vomiting to 0% (ref 5) while the percentage of patients who left the hospital without being seen was below 2% after the project (ref 17). In addition, a significant reduction in the prevalence of pressure ulcers was found (ref 26, ref 29) and a significant reduction of mucositis severity/distress was achieved (ref 24). Patient falls rate decreased (ref 15, ref 16, ref 19, ref 27).
Second, patient satisfaction level after project implementation improved (ref 28). The scale assessing healthcare providers by consumers showed improvement, but the changes were not statistically significant. Improvement in an emergency department leadership model and in methods of communication with patients improved patient satisfaction scores by 600% (ref 17). In addition, new evidence-based unit improved patient experiences about the unit although not all items improved significantly (ref 18).
Stakeholder involvement in the mixed-method review
To ensure stakeholders’ involvement in the review, the real-world relevance of our research [ 53 ], achieve a higher level of meaning in our review results, and gain new perspectives on our preliminary findings [ 50 ], a meeting with 11 stakeholders was organized. First, we asked if participants were aware of the concepts of evidence-based practice or evidence-based leadership. Responses revealed that participants were familiar with the concept of evidence-based practice, but the topic of evidence-based leadership was totally new. Examples of nurses and nurse leaders’ responses are as follows: “I have heard a concept of evidence-based practice but never a concept of evidence-based leadership.” Another participant described: “I have heard it [evidence-based leadership] but I do not understand what it means.”
Second, as stakeholder involvement is beneficial to the relevance and impact of health research [ 54 ], we asked how important evidence is to them in supporting decisions in health care services. One participant described as follows: “Using evidence in decisions is crucial to the wards and also to the entire hospital.” Third, we asked how the evidence-based approach is used in hospital settings. Participants expressed that literature is commonly used to solve clinical problems in patient care but not to solve leadership problems. “In [patient] medication and care, clinical guidelines are regularly used. However, I am aware only a few cases where evidence has been sought to solve leadership problems.”
And last, we asked what type of evidence is currently used to support nurse leaders’ decision making (e.g. scientific literature, organizational data, stakeholder views)? The participants were aware that different types of information were collected in their organization on a daily basis (e.g. patient satisfaction surveys). However, the information was seldom used to support decision making because nurse leaders did not know how to access this information. Even so, the participants agreed that the use of evidence from different sources was important in approaching any leadership or managerial problems in the organization. Participants also suggested that all nurse leaders should receive systematic training related to the topic; this could support the daily use of the evidence-based approach.
To our knowledge, this article represents the first mixed-methods systematic review to examine leadership problems, how evidence is used to solve these problems and what the perceived and measured effects of evidence-based leadership are on nurse leaders and their performance, organizational, and clinical outcomes. This review has two key findings. First, the available research data suggests that evidence-based leadership has potential in the healthcare context, not only to improve knowledge and skills among nurses, but also to improve organizational outcomes and the quality of patient care. Second, remarkably little published research was found to explore the effects of evidence-based leadership with an efficient trial design. We validated the preliminary results with nurse stakeholders, and confirmed that nursing staff, especially nurse leaders, were not familiar with the concept of evidence-based leadership, nor were they used to implementing evidence into their leadership decisions. Our data was based on many databases, and we screened a large number of studies. We also checked existing registers and databases and found no registered or ongoing similar reviews being conducted. Therefore, our results may not change in the near future.
We found that after identifying the leadership problems, 26 (84%) studies out of 31 used organizational data, 25 (81%) studies used scientific evidence from the literature, and 21 (68%) studies considered the views of stakeholders in attempting to understand specific leadership problems more deeply. However, only four studies critically appraised any of these findings. Considering previous critical statements of nurse leaders’ use of evidence in their decision making [ 14 , 30 , 31 , 34 , 55 ], our results are still quite promising.
Our results support a previous systematic review by Geert et al. [ 32 ], which concluded that it is possible to improve leaders’ individual-level outcomes, such as knowledge, motivation, skills, and behavior change using evidence-based approaches. Collins and Holton [ 23 ] particularly found that leadership training resulted in significant knowledge and skill improvements, although the effects varied widely across studies. In our study, evidence-based leadership was seen to enable changes in clinical practice, especially in patient care. On the other hand, we understand that not all efforts to changes were successful [ 56 , 57 , 58 ]. An evidence-based approach causes negative attitudes and feelings. Negative emotions in participants have also been reported due to changes, such as discomfort with a new working style [ 59 ]. Another study reported inconvenience in using a new intervention and its potential risks for patient confidentiality. Sometimes making changes is more time consuming than continuing with current practice [ 60 ]. These findings may partially explain why new interventions or program do not always fully achieve their goals. On the other hand, Dubose et al. [ 61 ] state that, if prepared with knowledge of resistance, nurse leaders could minimize the potential negative consequences and capitalize on a powerful impact of change adaptation.
We found that only six studies used a specific model or theory to understand the mechanism of change that could guide leadership practices. Participants’ reactions to new approaches may be an important factor in predicting how a new intervention will be implemented into clinical practice. Therefore, stronger effort should be put to better understanding the use of evidence, how participants’ reactions and emotions or practice changes could be predicted or supported using appropriate models or theories, and how using these models are linked with leadership outcomes. In this task, nurse leaders have an important role. At the same time, more responsibilities in developing health services have been put on the shoulders of nurse leaders who may already be suffering under pressure and increased burden at work. Working in a leadership position may also lead to role conflict. A study by Lalleman et al. [ 62 ] found that nurses were used to helping other people, often in ad hoc situations. The helping attitude of nurses combined with structured managerial role may cause dilemmas, which may lead to stress. Many nurse leaders opt to leave their positions less than 5 years [ 63 ].To better fulfill the requirements of health services in the future, the role of nurse leaders in evidence-based leadership needs to be developed further to avoid ethical and practical dilemmas in their leadership practices.
It is worth noting that the perceived and measured effects did not offer strong support to each other but rather opened a new venue to understand the evidence-based leadership. Specifically, the perceived effects did not support to measured effects (competence, ability to understand patients’ needs, use of resources, team effort, and specific clinical outcomes) while the measured effects could not support to perceived effects (nurse’s performance satisfaction, changes in practices, and clinical outcomes satisfaction). These findings may indicate that different outcomes appear if the effects of evidence-based leadership are looked at using different methodological approach. Future study is encouraged using well-designed study method including mixed-method study to examine the consistency between perceived and measured effects of evidence-based leadership in health care.
There is a potential in nursing to support change by demonstrating conceptual and operational commitment to research-based practices [ 64 ]. Nurse leaders are well positioned to influence and lead professional governance, quality improvement, service transformation, change and shared governance [ 65 ]. In this task, evidence-based leadership could be a key in solving deficiencies in the quality, safety of care [ 14 ] and inefficiencies in healthcare delivery [ 12 , 13 ]. As WHO has revealed, there are about 28 million nurses worldwide, and the demand of nurses will put nurse resources into the specific spotlight [ 1 ]. Indeed, evidence could be used to find solutions for how to solve economic deficits or other problems using leadership skills. This is important as, when nurses are able to show leadership and control in their own work, they are less likely to leave their jobs [ 66 ]. On the other hand, based on our discussions with stakeholders, nurse leaders are not used to using evidence in their own work. Further, evidence-based leadership is not possible if nurse leaders do not have access to a relevant, robust body of evidence, adequate funding, resources, and organizational support, and evidence-informed decision making may only offer short-term solutions [ 55 ]. We still believe that implementing evidence-based strategies into the work of nurse leaders may create opportunities to protect this critical workforce from burnout or leaving the field [ 67 ]. However, the role of the evidence-based approach for nurse leaders in solving these problems is still a key question.
Limitations
This study aimed to use a broad search strategy to ensure a comprehensive review but, nevertheless, limitations exist: we may have missed studies not included in the major international databases. To keep search results manageable, we did not use specific databases to systematically search grey literature although it is a rich source of evidence used in systematic reviews and meta-analysis [ 68 ]. We still included published conference abstract/proceedings, which appeared in our scientific databases. It has been stated that conference abstracts and proceedings with empirical study results make up a great part of studies cited in systematic reviews [ 69 ]. At the same time, a limited space reserved for published conference publications can lead to methodological issues reducing the validity of the review results [ 68 ]. We also found that the great number of studies were carried out in western countries, restricting the generalizability of the results outside of English language countries. The study interventions and outcomes were too different across studies to be meaningfully pooled using statistical methods. Thus, our narrative synthesis could hypothetically be biased. To increase transparency of the data and all decisions made, the data, its categorization and conclusions are based on original studies and presented in separate tables and can be found in Additional files. Regarding a methodological approach [ 34 ], we used a mixed methods systematic review, with the core intention of combining quantitative and qualitative data from primary studies. The aim was to create a breadth and depth of understanding that could confirm to or dispute evidence and ultimately answer the review question posed [ 34 , 70 ]. Although the method is gaining traction due to its usefulness and practicality, guidance in combining quantitative and qualitative data in mixed methods systematic reviews is still limited at the theoretical stage [ 40 ]. As an outcome, it could be argued that other methodologies, for example, an integrative review, could have been used in our review to combine diverse methodologies [ 71 ]. We still believe that the results of this mixed method review may have an added value when compared with previous systematic reviews concerning leadership and an evidence-based approach.
Our mixed methods review fills the gap regarding how nurse leaders themselves use evidence to guide their leadership role and what the measured and perceived impact of evidence-based leadership is in nursing. Although the scarcity of controlled studies on this topic is concerning, the available research data suggest that evidence-based leadership intervention can improve nurse performance, organizational outcomes, and patient outcomes. Leadership problems are also well recognized in healthcare settings. More knowledge and a deeper understanding of the role of nurse leaders, and how they can use evidence in their own managerial leadership decisions, is still needed. Despite the limited number of studies, we assume that this narrative synthesis can provide a good foundation for how to develop evidence-based leadership in the future.
Implications
Based on our review results, several implications can be recommended. First, the future of nursing success depends on knowledgeable, capable, and strong leaders. Therefore, nurse leaders worldwide need to be educated about the best ways to manage challenging situations in healthcare contexts using an evidence-based approach in their decisions. This recommendation was also proposed by nurses and nurse leaders during our discussion meeting with stakeholders.
Second, curriculums in educational organizations and on-the-job training for nurse leaders should be updated to support general understanding how to use evidence in leadership decisions. And third, patients and family members should be more involved in the evidence-based approach. It is therefore important that nurse leaders learn how patients’ and family members’ views as stakeholders are better considered as part of the evidence-based leadership approach.
Future studies should be prioritized as follows: establishment of clear parameters for what constitutes and measures evidence-based leadership; use of theories or models in research to inform mechanisms how to effectively change the practice; conducting robust effectiveness studies using trial designs to evaluate the impact of evidence-based leadership; studying the role of patient and family members in improving the quality of clinical care; and investigating the financial impact of the use of evidence-based leadership approach within respective healthcare systems.
Data availability
The authors obtained all data for this review from published manuscripts.
World Health Organization. State of the world’s nursing 2020: investing in education, jobs and leadership. 2020. https://www.who.int/publications/i/item/9789240003279 . Accessed 29 June 2024.
Hersey P, Campbell R. Leadership: a behavioral science approach. The Center for; 2004.
Cline D, Crenshaw JT, Woods S. Nurse leader: a definition for the 21st century. Nurse Lead. 2022;20(4):381–4. https://doi.org/10.1016/j.mnl.2021.12.017 .
Article Google Scholar
Chen SS. Leadership styles and organization structural configurations. J Hum Resource Adult Learn. 2006;2(2):39–46.
Google Scholar
McKibben L. Conflict management: importance and implications. Br J Nurs. 2017;26(2):100–3.
Article PubMed Google Scholar
Haghgoshayie E, Hasanpoor E. Evidence-based nursing management: basing Organizational practices on the best available evidence. Creat Nurs. 2021;27(2):94–7. https://doi.org/10.1891/CRNR-D-19-00080 .
Majers JS, Warshawsky N. Evidence-based decision-making for nurse leaders. Nurse Lead. 2020;18(5):471–5.
Tichy NM, Bennis WG. Making judgment calls. Harvard Business Rev. 2007;85(10):94.
Sousa MJ, Pesqueira AM, Lemos C, Sousa M, Rocha Á. Decision-making based on big data analytics for people management in healthcare organizations. J Med Syst. 2019;43(9):1–10.
Guo R, Berkshire SD, Fulton LV, Hermanson PM. %J L in HS. Use of evidence-based management in healthcare administration decision-making. 2017;30(3): 330–42.
Liang Z, Howard P, Rasa J. Evidence-informed managerial decision-making: what evidence counts?(part one). Asia Pac J Health Manage. 2011;6(1):23–9.
Hasanpoor E, Janati A, Arab-Zozani M, Haghgoshayie E. Using the evidence-based medicine and evidence-based management to minimise overuse and maximise quality in healthcare: a hybrid perspective. BMJ evidence-based Med. 2020;25(1):3–5.
Shingler NA, Gonzalez JZ. Ebm: a pathway to evidence-based nursing management. Nurs 2022. 2017;47(2):43–6.
Farokhzadian J, Nayeri ND, Borhani F, Zare MR. Nurse leaders’ attitudes, self-efficacy and training needs for implementing evidence-based practice: is it time for a change toward safe care? Br J Med Med Res. 2015;7(8):662.
Article PubMed PubMed Central Google Scholar
American Nurses Association. ANA leadership competency model. Silver Spring, MD; 2018.
Royal College of Nursing. Leadership skills. 2022. https://www.rcn.org.uk/professional-development/your-career/nurse/leadership-skills . Accessed 29 June 2024.
Kakemam E, Liang Z, Janati A, Arab-Zozani M, Mohaghegh B, Gholizadeh M. Leadership and management competencies for hospital managers: a systematic review and best-fit framework synthesis. J Healthc Leadersh. 2020;12:59.
Liang Z, Howard PF, Leggat S, Bartram T. Development and validation of health service management competencies. J Health Organ Manag. 2018;32(2):157–75.
World Health Organization. Global Strategic Directions for Nursing and Midwifery. 2021. https://apps.who.int/iris/bitstream/handle/10665/344562/9789240033863-eng.pdf . Accessed 29 June 2024.
NHS Leadership Academy. The nine leadership dimensions. 2022. https://www.leadershipacademy.nhs.uk/resources/healthcare-leadership-model/nine-leadership-dimensions/ . Accessed 29 June 2024.
Canadian Nurses Association. Evidence-informed decision-making and nursing practice: Position statement. 2018. https://hl-prod-ca-oc-download.s3-ca-central-1.amazonaws.com/CNA/2f975e7e-4a40-45ca-863c-5ebf0a138d5e/UploadedImages/documents/Evidence_informed_Decision_making_and_Nursing_Practice_position_statement_Dec_2018.pdf . Accessed 29 June 2024.
Hasanpoor E, Hajebrahimi S, Janati A, Abedini Z, Haghgoshayie E. Barriers, facilitators, process and sources of evidence for evidence-based management among health care managers: a qualitative systematic review. Ethiop J Health Sci. 2018;28(5):665–80.
PubMed PubMed Central Google Scholar
Collins DB, Holton EF III. The effectiveness of managerial leadership development programs: a meta-analysis of studies from 1982 to 2001. Hum Res Dev Q. 2004;15(2):217–48.
Cummings GG, Lee S, Tate K, Penconek T, Micaroni SP, Paananen T, et al. The essentials of nursing leadership: a systematic review of factors and educational interventions influencing nursing leadership. Int J Nurs Stud. 2021;115:103842.
Clavijo-Chamorro MZ, Romero-Zarallo G, Gómez-Luque A, López-Espuela F, Sanz-Martos S, López-Medina IM. Leadership as a facilitator of evidence implementation by nurse managers: a metasynthesis. West J Nurs Res. 2022;44(6):567–81.
Young SK. Evidence-based management: a literature review. J Nurs Adm Manag. 2002;10(3):145–51.
Williams LL. What goes around comes around: evidence-based management. Nurs Adm Q. 2006;30(3):243–51.
Fraser I. Organizational research with impact: working backwards. Worldviews Evidence-Based Nurs. 2004;1:S52–9.
Roshanghalb A, Lettieri E, Aloini D, Cannavacciuolo L, Gitto S, Visintin F. What evidence on evidence-based management in healthcare? Manag Decis. 2018;56(10):2069–84.
Jaana M, Vartak S, Ward MM. Evidence-based health care management: what is the research evidence available for health care managers? Eval Health Prof. 2014;37(3):314–34.
Tate K, Hewko S, McLane P, Baxter P, Perry K, Armijo-Olivo S, et al. Learning to lead: a review and synthesis of literature examining health care managers’ use of knowledge. J Health Serv Res Policy. 2019;24(1):57–70.
Geerts JM, Goodall AH, Agius S, %J SS. Medicine. Evidence-based leadership development for physicians: a systematic literature review. 2020;246: 112709.
Barends E, Rousseau DM, Briner RB. Evidence-based management: The basic principles. Amsterdam; 2014. https://research.vu.nl/ws/portalfiles/portal/42141986/complete+dissertation.pdf#page=203 . Accessed 29 June 2024.
Stern C, Lizarondo L, Carrier J, Godfrey C, Rieger K, Salmond S, et al. Methodological guidance for the conduct of mixed methods systematic reviews. JBI Evid Synthesis. 2020;18(10):2108–18. https://doi.org/10.11124/JBISRIR-D-19-00169 .
Lancet T. 2020: unleashing the full potential of nursing. Lancet (London, England). 2019. p. 1879.
Välimäki MA, Lantta T, Hipp K, Varpula J, Liu G, Tang Y, et al. Measured and perceived impacts of evidence-based leadership in nursing: a mixed-methods systematic review protocol. BMJ Open. 2021;11(10):e055356. https://doi.org/10.1136/bmjopen-2021-055356 .
The Joanna Briggs Institute. Joanna Briggs Institute reviewers’ manual: 2014 edition. Joanna Briggs Inst. 2014; 88–91.
Pearson A, White H, Bath-Hextall F, Salmond S, Apostolo J, Kirkpatrick P. A mixed-methods approach to systematic reviews. JBI Evid Implement. 2015;13(3):121–31.
Johnson RB, Onwuegbuzie AJ. Mixed methods research: a research paradigm whose time has come. Educational Researcher. 2004;33(7):14–26.
Hong, Pluye P, Bujold M, Wassef M. Convergent and sequential synthesis designs: implications for conducting and reporting systematic reviews of qualitative and quantitative evidence. Syst Reviews. 2017;6(1):61. https://doi.org/10.1186/s13643-017-0454-2 .
Ramis MA, Chang A, Conway A, Lim D, Munday J, Nissen L. Theory-based strategies for teaching evidence-based practice to undergraduate health students: a systematic review. BMC Med Educ. 2019;19(1):1–13.
Sackett DL, Rosenberg WM, Gray JM, Haynes RB, Richardson WS. Evidence based medicine: what it is and what it isn’t. Bmj. British Medical Journal Publishing Group; 1996. pp. 71–2.
Goodman JS, Gary MS, Wood RE. Bibliographic search training for evidence-based management education: a review of relevant literatures. Acad Manage Learn Educ. 2014;13(3):322–53.
Aromataris E, Munn Z. Chapter 3: Systematic reviews of effectiveness. JBI Manual for Evidence Synthesis. 2020; https://synthesismanual.jbi.global .
Munn Z, Barker TH, Moola S, Tufanaru C, Stern C, McArthur A et al. Methodological quality of case series studies: an introduction to the JBI critical appraisal tool. 2020;18(10): 2127–33.
Hong Q, Pluye P, Fàbregues S, Bartlett G, Boardman F, Cargo M, et al. Mixed methods Appraisal Tool (MMAT) Version 2018: user guide. Montreal: McGill University; 2018.
McKenna J, Jeske D. Ethical leadership and decision authority effects on nurses’ engagement, exhaustion, and turnover intention. J Adv Nurs. 2021;77(1):198–206.
Maxwell M, Hibberd C, Aitchison P, Calveley E, Pratt R, Dougall N, et al. The TIDieR (template for intervention description and replication) checklist. The patient Centred Assessment Method for improving nurse-led biopsychosocial assessment of patients with long-term conditions: a feasibility RCT. NIHR Journals Library; 2018.
Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Res Psychol. 2006;3(2):77–101.
Pollock A, Campbell P, Struthers C, Synnot A, Nunn J, Hill S, et al. Stakeholder involvement in systematic reviews: a scoping review. Syst Reviews. 2018;7:1–26.
Braye S, Preston-Shoot M. Emerging from out of the shadows? Service user and carer involvement in systematic reviews. Evid Policy. 2005;1(2):173–93.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Reviews. 2021;10(1):1–11.
Porta M. Pilot investigation, study. A dictionary of epidemiology. Oxford University Press Oxford; 2014. p. 215.
Kreis J, Puhan MA, Schünemann HJ, Dickersin K. Consumer involvement in systematic reviews of comparative effectiveness research. Health Expect. 2013;16(4):323–37.
Joseph ML, Nelson-Brantley HV, Caramanica L, Lyman B, Frank B, Hand MW, et al. Building the science to guide nursing administration and leadership decision making. JONA: J Nurs Adm. 2022;52(1):19–26.
Gifford W, Davies BL, Graham ID, Tourangeau A, Woodend AK, Lefebre N. Developing Leadership Capacity for Guideline Use: a pilot cluster Randomized Control Trial: Leadership Pilot Study. Worldviews Evidence-Based Nurs. 2013;10(1):51–65. https://doi.org/10.1111/j.1741-6787.2012.00254.x .
Hsieh HY, Henker R, Ren D, Chien WY, Chang JP, Chen L, et al. Improving effectiveness and satisfaction of an electronic charting system in Taiwan. Clin Nurse Specialist. 2016;30(6):E1–6. https://doi.org/10.1097/NUR.0000000000000250 .
McAllen E, Stephens K, Swanson-Biearman B, Kerr K, Whiteman K. Moving Shift Report to the Bedside: an evidence-based Quality Improvement Project. OJIN: Online J Issues Nurs. 2018;23(2). https://doi.org/10.3912/OJIN.Vol23No02PPT22 .
Thomas M, Autencio K, Cesario K. Positive outcomes of an evidence-based pressure injury prevention program. J Wound Ostomy Cont Nurs. 2020;47:S24.
Cullen L, Titler MG. Promoting evidence-based practice: an internship for Staff nurses. Worldviews Evidence-Based Nurs. 2004;1(4):215–23. https://doi.org/10.1111/j.1524-475X.2004.04027.x .
DuBose BM, Mayo AM. Resistance to change: a concept analysis. Nursing forum. Wiley Online Library; 2020. pp. 631–6.
Lalleman PCB, Smid GAC, Lagerwey MD, Shortridge-Baggett LM, Schuurmans MJ. Curbing the urge to care: a bourdieusian analysis of the effect of the caring disposition on nurse middle managers’ clinical leadership in patient safety practices. Int J Nurs Stud. 2016;63:179–88.
Article CAS PubMed Google Scholar
Martin E, Warshawsky N. Guiding principles for creating value and meaning for the next generation of nurse leaders. JONA: J Nurs Adm. 2017;47(9):418–20.
Griffiths P, Recio-Saucedo A, Dall’Ora C, Briggs J, Maruotti A, Meredith P, et al. The association between nurse staffing and omissions in nursing care: a systematic review. J Adv Nurs. 2018;74(7):1474–87. https://doi.org/10.1111/jan.13564 .
Lúanaigh PÓ, Hughes F. The nurse executive role in quality and high performing health services. J Nurs Adm Manag. 2016;24(1):132–6.
de Kok E, Weggelaar-Jansen AM, Schoonhoven L, Lalleman P. A scoping review of rebel nurse leadership: descriptions, competences and stimulating/hindering factors. J Clin Nurs. 2021;30(17–18):2563–83.
Warshawsky NE. Building nurse manager well-being by reducing healthcare system demands. JONA: J Nurs Adm. 2022;52(4):189–91.
Paez A. Gray literature: an important resource in systematic reviews. J Evidence-Based Med. 2017;10(3):233–40.
McAuley L, Tugwell P, Moher D. Does the inclusion of grey literature influence estimates of intervention effectiveness reported in meta-analyses? Lancet. 2000;356(9237):1228–31.
Sarah S. Introduction to mixed methods systematic reviews. https://jbi-global-wiki.refined.site/space/MANUAL/4689215/8.1+Introduction+to+mixed+methods+systematic+reviews . Accessed 29 June 2024.
Whittemore R, Knafl K. The integrative review: updated methodology. J Adv Nurs. 2005;52(5):546–53.
Download references
Acknowledgements
We want to thank the funding bodies, the Finnish National Agency of Education, Asia Programme, the Department of Nursing Science at the University of Turku, and Xiangya School of Nursing at the Central South University. We also would like to thank the nurses and nurse leaders for their valuable opinions on the topic.
The work was supported by the Finnish National Agency of Education, Asia Programme (grant number 26/270/2020) and the University of Turku (internal fund 26003424). The funders had no role in the study design and will not have any role during its execution, analysis, interpretation of the data, decision to publish, or preparation of the manuscript.
Author information
Authors and affiliations.
Department of Nursing Science, University of Turku, Turku, FI-20014, Finland
Maritta Välimäki, Tella Lantta, Kirsi Hipp & Jaakko Varpula
School of Public Health, University of Helsinki, Helsinki, FI-00014, Finland
Maritta Välimäki
Xiangya Nursing, School of Central South University, Changsha, 410013, China
Shuang Hu, Jiarui Chen, Yao Tang, Wenjun Chen & Xianhong Li
School of Health and Social Services, Häme University of Applied Sciences, Hämeenlinna, Finland
Hunan Cancer Hospital, Changsha, 410008, China
Gaoming Liu
You can also search for this author in PubMed Google Scholar
Contributions
Study design: MV, XL. Literature search and study selection: MV, KH, TL, WC, XL. Quality assessment: YT, SH, XL. Data extraction: JC, MV, JV, WC, YT, SH, GL. Analysis and interpretation: MV, SH. Manuscript writing: MV. Critical revisions for important intellectual content: MV, XL. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Xianhong Li .
Ethics declarations
Ethics approval and consent to participate.
No ethical approval was required for this study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Differences between the original protocol
We modified criteria for the included studies: we included published conference abstracts/proceedings, which form a relatively broad knowledge base in scientific knowledge. We originally planned to conduct a survey with open-ended questions followed by a face-to-face meeting to discuss the preliminary results of the review. However, to avoid extra burden in nurses due to COVID-19, we decided to limit the validation process to the online discussion only.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, supplementary material 3, supplementary material 4, supplementary material 5, supplementary material 6, supplementary material 7, supplementary material 8, supplementary material 9, supplementary material 10, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Välimäki, M., Hu, S., Lantta, T. et al. The impact of evidence-based nursing leadership in healthcare settings: a mixed methods systematic review. BMC Nurs 23 , 452 (2024). https://doi.org/10.1186/s12912-024-02096-4
Download citation
Received : 28 April 2023
Accepted : 13 June 2024
Published : 03 July 2024
DOI : https://doi.org/10.1186/s12912-024-02096-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Evidence-based leadership
- Health services administration
- Organizational development
- Quality in healthcare
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]

Healthcare Leadership: What Is It and Why Is It Important?

Industry Advice Healthcare Leadership
There’s an immense need, now more than ever, for effective leadership in healthcare. Specifically, the global pandemic has highlighted the importance of innovative healthcare leaders who are able to quickly formulate effective solutions. Additional challenges such as healthcare accessibility and affordability require effective forward-thinking leaders.
If you’re interested in learning more about how you can make a mark in healthcare today, here’s an overview of what healthcare leadership is, why it’s important, and what makes an effective leader in the healthcare system.
What is healthcare leadership?
Leadership is often defined as the ability to manage a team effectively. This definition, however, is only a part of what makes an effective leader. Healthcare leadership isn’t about maintaining the status quo, but identifying challenges in the system and finding solutions to those problems.
“Healthcare leadership is taking an active role in the direction of healthcare today,” says Dr. Robert Baginski, director of interdisciplinary affairs in Northeastern University’s Department of Medical Sciences and associate clinical professor. “It ideally should be guiding healthcare in the direction that we feel it should go in the future.”
The importance of leadership in healthcare
Effective leadership in healthcare is incredibly important, especially when considering the expense of modern care. Here’s a closer look at the various ways that effective leadership can make a lasting impact.
1. Improves quality of care
Effective leadership is integral to quality healthcare . If a healthcare team is uncoordinated or unfocused, patients often pay the price. Great leaders facilitate communication, boost productivity, and put others first. This ability is critical to quality patient care since healthcare often requires a rapid response to issues that arise. In such situations, communication and efficiency are vital.
2. Creates adaptable leaders
One of the most prominent examples of needing adaptability in healthcare is the COVID-19 pandemic. In 2020, the American Psychological Association identified seven crucial leadership qualities necessary for combatting the pandemic.
- Effective stress management
- Empathy and optimism when sharing information
- Building trust with expertise and dependability
- Honesty and transparency
- Consistent communication
- Openness to feedback
- Ability to serve as role models
When unpredictability and uncertainty is rampant, effective leadership is crucial. An excellent leader will be able to not only navigate a stressful situation but also lead others through it and find solutions for the future.
3. Encourages forward thinking
Leadership and management are often used as synonyms, but the reality is that leadership involves much more than the day-to-day operations of a business. Healthcare in particular has a need for leaders who are looking to the future of healthcare and how to improve it.
While healthcare leadership is important to every country, according to the World Population Review , the United States has higher healthcare costs than any other country. Furthermore, while the number of uninsured individuals in the U.S. is lower than ever , the healthcare system is highly dependent on access to insurance coverage.
According to a report from the Peterson-KFF Health System Tracker , compared to similar countries, the United States has:
- The highest pregnancy-related mortality rate.
- A higher-than-average rate of diabetes and congestive heart failure.
- A higher percentage of reported medication and treatment errors than the majority of comparable countries.
According to Baginski, improvements to the healthcare system are possible with effective leadership. “Ideally, I feel healthcare should be looking to the future, toward solutions where we can provide the best and the most healthcare to those who need it most, regardless of insurance status, access to money, or where they live,” he says.
4. Produces innovative leaders
One of the most prevalent challenges facing the healthcare industry today is the chronic shortage of healthcare professionals . A 2022 survey of 1,000 healthcare staff found that 48% don’t believe their organization is doing enough to address burnout.
The healthcare industry is in need of leaders who are able to identify the problems that are leading to burnout and resolve them. Baginski explains that good leaders do two things differently when compared to ineffective leaders:
- Identification: They recognize problems as they arise, and proactively consider potential issues. For example, the same survey reported that 57% of healthcare workers are concerned that their highly repetitive tasks will ultimately lead to burnout.
- Innovation: They find solutions to those problems and contribute to the future of healthcare. To address the repetitive tasks in healthcare, many healthcare workers are hopeful that technology and automation will improve their overall experience and allow them to focus more closely on patient care.
What makes a healthcare leader effective?
Individuals who take on a leadership role in healthcare need several skills to be effective. Five essential leadership skills in healthcare are:
- Mentorship: An effective leader doesn’t stand above others but seeks to foster leadership qualities in them.
- Challenging the status quo: Leaders aren’t content with the status quo but are always seeking opportunities to innovate and improve.
- Educating others: In addition to mentoring others at the individual level, effective leaders seek to educate others outside of their direct influence.
- Humility: An effective leader isn’t afraid to accept feedback or criticism. Since much is unknown about healthcare, mistakes are often inevitable. A good leader will admit their mistakes or skill and expertise gaps.
- Creating opportunities for others: Leaders always look to the future. Instead of sole personal improvement, an effective leader will prioritize helping the next generation of healthcare professionals obtain leadership traits.
One of the most detrimental traits to quality healthcare is complacency. Self-satisfaction often leads to stagnation rather than proactivity. An effective leader recognizes their limitations and understands that there’s always something new to learn. According to Baginski, “Bad leadership is keeping things as they always have been because that’s the way they’ve been done previously. That doesn’t get you anywhere.”
Ready to develop your leadership skills?
If you’re hoping to advance your career in healthcare to a leadership position, it’s important to ensure that you’re prepared. One of the best ways to obtain the relevant skills and qualifications to advance to a leadership role is to obtain a relevant degree.
“Get all of your education and your experience first, and then get all of your information before you address that problem,” Baginski says. “Learn how to critically assess information and get all your ducks in a row before you start to confront change.”
If you want to become a more effective leader and advance your career, consider obtaining Northeastern University’s Doctor of Medical Science (DMSc) in Healthcare Leadership . This degree will provide you with the skills and knowledge necessary to take your first steps into a successful leadership role.
Editor’s Note: This post was originally published in January 2023. It has since been updated for relevance and accuracy.
Subscribe below to receive future content from the Graduate Programs Blog.
About michael boyles, related articles.


Healthcare Law: Navigating Our Complex System

Healthcare Management vs. Leadership: What’s the Difference?

4 Ways Artificial Intelligence is Transforming Healthcare
Did you know.
Advanced degree holders earn a salary an average 25% higher than bachelor's degree holders. (Economic Policy Institute, 2021)
Northeastern University Graduate Programs
Explore our 200+ industry-aligned graduate degree and certificate programs.
Most Popular:
Tips for taking online classes: 8 strategies for success, public health careers: what can you do with an mph, 7 international business careers that are in high demand, edd vs. phd in education: what’s the difference, 7 must-have skills for data analysts, in-demand biotechnology careers shaping our future, the benefits of online learning: 8 advantages of online degrees, how to write a statement of purpose for graduate school, the best of our graduate blog—right to your inbox.
Stay up to date on our latest posts and university events. Plus receive relevant career tips and grad school advice.
By providing us with your email, you agree to the terms of our Privacy Policy and Terms of Service.
Keep Reading:

Top Higher Education Conferences To Attend in 2024

Grad School or Work? How To Balance Both

Is a Master’s in Computer Science Worth the Investment?

Should I Go to Grad School: 4 Questions To Consider
Volume 20 Supplement 2
Peer Teacher Training in health professional education
- Open access
- Published: 03 December 2020
Leadership in healthcare education
- Christie van Diggele 1 , 2 ,
- Annette Burgess 2 , 3 ,
- Chris Roberts 2 , 3 &
- Craig Mellis 4
BMC Medical Education volume 20 , Article number: 456 ( 2020 ) Cite this article
118k Accesses
65 Citations
17 Altmetric
Metrics details
Effective leadership is a complex and highly valued component of healthcare education, increasingly recognised as essential to the delivery of high standards of education, research and clinical practice. To meet the needs of healthcare in the twenty-first century, competent leaders will be increasingly important across all health professions, including allied health, nursing, pharmacy, dentistry, and medicine. Consequently, incorporation of leadership training and development should be part of all health professional curricula. A new type of leader is emerging: one who role models the balance between autonomy and accountability, emphasises teamwork, and focuses on improving patient outcomes. Healthcare education leaders are required to work effectively and collaboratively across discipline and organisational boundaries, where titles are not always linked to leadership roles. This paper briefly considers the current theories of leadership, and explores leadership skills and roles within the context of healthcare education.
Leadership has many interpretations, and has been likened to “ the abominable snowman whose footprints are everywhere but who is nowhere to be seen” [ 1 ]. It is an influential process, through which groups of people work towards the achievement of a common goal [ 2 ]. Leaders have the ability to shape and influence their followers’ values, attitudes and behaviours through a dyadic relationship. They are able to gain and enlist the support of others in order to achieve shared goals [ 3 , 4 ]. Effective leadership is a complex and highly valued component of healthcare education, increasingly recognised as essential to the delivery of high standards of education, research and clinical practice [ 3 ]. In order to achieve more effective outcomes, leadership and management skills are now an expectation and requirement in the healthcare education setting [ 5 ]. However, leaders within healthcare education should not rely on formal positions of authority, but instead, utilise their own appropriate leadership qualities irrespective of their level within the organisation [ 3 ]. A new type of leader is emerging: one who role models the balance between autonomy and accountability, emphasises teamwork, and focuses on improving patient outcomes [ 3 ]. This paper briefly considers the theories of leadership, and explores leadership skills and roles within the context of healthcare education.
Management versus leadership
Management and leadership are considered just as important as each other in accomplishing organisational goals. However, there are differences in the functions of the two roles. Management produces order and consistency, while leadership produces change and movement [ 2 ]. Management has the responsibility of organising all elements within the organisation, so that the leader’s vision and goals are successfully achieved. If poor management is in place, then goals cannot be achieved; and if poor leadership is in place, then there is no clear goal or vision to work towards. Leadership is seen as “setting direction, influencing others and managing change: with management concerned with the marshalling and organisation of resources and maintaining stability” [ 6 ]. These differences are summarised in Table 1 [ 6 , 7 ].
Transactional and transformational leadership
Leadership is a social construct, and there are many different leadership models [ 6 ]. Two broad types of leadership are identifiable: “transactional” and “transformational”. And their respective features are a useful way to think about the many types of leadership. Transactional and transformational leadership models are normally amalgamated within organisations to “empower others” (transformational) while holding individuals “accountable” (transactional) for their actions [ 7 , 8 , 9 ]. While it is clear that both transformational and transactional leadership paradigms are needed for an organisation to be effective, the optimal leader predominantly practices the transformational aspects of leadership, rather than transactional [ 10 ].
Transactional leadership
The transactional model is seen as an authoritative relationship that is transaction based, where exchanges occur between a leader and follower, once specific goals are identified or decided upon. Transactional leaders value order and structure, and have formal authority, with positions of responsibility within organisations. They achieve organisational goals through a rewards system and through positive reinforcement. A weakness of this model is the lack of innovation, as individuals are driven by predetermined outcomes, and there is lack of incentive and motivation to perform beyond what is expected [ 6 ].
Transformational leadership
Since the introduction of transformational leadership, the concept of leadership has undergone a major shift from representing an authoritative relationship (transactional), to a process of influencing individuals (transformational). Transformational leadership involves leadership through the transformation of individuals or ‘followers’, to work towards a common organisational goal [ 9 , 10 , 11 ]. This contemporary form of leadership is based on inspiring individuals, and forming teams to achieve goals. Transformational leaders define organisations through the articulation of a clear vision and clear values. The four “I”s of transformational leadership are outlined in Table 2 [ 9 ].
Team leadership
More recently, the focus has shifted towards “team leadership” , with distributed leadership becoming more prevalent within healthcare education, where different professions share influence [ 12 , 13 ]. Increasingly, leadership involves a collaborative role, with an emphasis on shared leadership and thoughtful allocation of responsibilities. Team-based organisations shift central control from the one leader, to the team. Teams are comprised of members who are interdependent, needing to coordinate their activities in order to accomplish their shared goals [ 14 , 15 ]. Personal autonomy, accountability, appropriate recognition, and clarity of roles, are all elements that contribute to optimal team performance. However, to ensure success, the organisational culture needs to support the involvement of individuals in these teams, and encourage leadership qualities [ 15 ]. Teams often fail when they exist in a traditional authority structure, where organisational culture is not supportive of collaborative work, and lower level decision making. Distributed leadership entails sharing of influence by team members, who step forward, or take a step back as needed. Leadership is provided by the person who meets the specific needs of the team at the time, hence providing faster responses to more complex issues in today’s organisations [ 15 , 16 , 17 ]. Effective leaders have an understanding of the conditions needed for teams to function well. For a team to achieve its potential, the operational roles of its members should be matched to their members’ abilities [ 18 ]. Belbin (1991) classified nine roles of team members that contribute to its process and function [ 19 ], outlined in Table 3 . Importantly, within team leadership, no single team role should be regarded as more important than another. Successful teams thrive on their diversity, drawing from the strengths of each member [ 13 ].
Effective leadership
Leaders need to have good time management and organisational skills, the ability to network professionally, display political nous and most importantly, they need to have strong communication skills [ 4 , 20 , 21 ]. Ready acceptance of feedback and self-awareness are important in development of leadership skills [ 20 , 21 ]. Behaviour, habits and biases can be deliberately corrected by utilising received feedback. Although there is not one set of qualities that apply to being an effective leader, certain competencies are valued and contribute to the leadership model in different ways [ 5 ]. Leadership competencies relevant for all health professional educators are outlined in Table 4 [ 3 ].
Language of leadership
Just as education and healthcare organisations have evolved, so too has the team leader. The role of the modern leader reinforces the tenets of stepping forward, collaborating and contributing. This role involves encouraging others by practising followership, and lending meaningful support to other leaders. As already stated, when it comes to leadership, excellent communication skills are a must. In order for successful communication to occur, both the sender and receiver must understand the message. This means that active listening is just as important as active talking [ 22 ]. Language used needs to be [ 22 ]:
Communicate with clarity of your purpose and the role of others
Stimulating
Deliver messages in a powerful, inspiring and dramatic way
Lead by example and walk the talk
Include active listening
Acknowledge what has been communicated, and use questioning skills
Show that you value others and their contributions
Challenges for leaders in healthcare education
There are a number of unique challenges in healthcare education. Healthcare education is delivered across professional disciplines, and notably, across organisational boundaries, involving universities, hospitals, and healthcare services. In turn, these organisations are bound by their own systems, structures, policies, cultures and values. At some point, most leaders in healthcare education need to make a decision about their leadership direction, and whether it lies predominantly in higher education or the clinical setting; and whether it lies in undergraduate education or postgraduate education. It can be difficult to merge roles between organisations, and McKimm (2004) has identified a number of issues and challenges specific to health education leaders, outlined in Table 5 [ 22 , 23 ]. Throughout a career, it may be necessary to maintain an awareness of available opportunities within organisations, and match these to the required experiences and capabilities [ 22 , 23 ] (see Fig. 1 ).
Reflection task
Development of leadership skills
Workforce data indicates that many experienced clinicians and healthcare educators will retire over the next ten years [ 24 , 25 ]. The need for effective succession planning and leadership training is well recognised [ 25 , 26 , 27 ], with a current shortage of emerging leaders moving into leadership roles. Effective leaders need to be nurtured and supported by the organisations in which they are educated, train and work [ 6 ]. As a learned skill, the topic of leadership is gathering momentum as a key curriculum area. Leadership development, assessment and feedback are necessary throughout the education and training of health professionals. Aspiring and current leaders can be identified, trained and assessed through formal leadership development programs, and through supportive organisational cultures. This requires embedding leadership training programs, opportunities for leadership practice, and promotion of professional networks within and beyond the organisation. The importance of mentorship within healthcare education is well recognised, offering a means to further enhance leadership and engagement within the workforce [ 28 ].
While many are assigned as leaders through their job title, it is important to identify, support and develop emerging leaders [ 2 ]. Leadership consists of a learnable set of practices and skills that can be developed by reading literature and attending leadership courses [ 29 ]. Additionally, investment in the social capital of organisations, fostering interprofessional learning and communication in the work setting, and collaboration across organisations assists in leadership development. Developing leadership skills is a life-long process [ 21 ]. Resources and opportunities should be considered to assist in the development of leadership skills. Some examples include:
Reading about leadership e.g. theories on leadership styles
Attending leadership training workshops
Participating in mentorship programs either as mentee or mentor
Joining small group seminars on leadership development
Accepting more responsibilities when required, or when opportunities arise.
Process for effective leadership
A title is not required to enable effective leadership. Leadership may occur in everyday work, and occurs in collaboration with other professionals within the education and healthcare systems. For example, leadership in teaching, administration, research, and/or excellence in clinical practice.
Leadership roles include the important concept of management of both personal and professional practice. Priorities need to be set and time managed to integrate work and personal life. Tools can be used to stay organised, and deliberately manage busy schedules. Effective delegation may be used to share the work of new projects:
Organisation to ensure an understanding of tasks, priorities and deadlines
Establish steps and a sequence to achieve the desired outcomes
List required resources, considering the competencies of individual team members, and match tasks appropriately (also consider skill development needs)
Communicate with team members, monitor progress in activities and provide guidance to team members.
Leadership competencies, and the incorporation of leadership development as part of curricula, are identified as important across all health professions, including allied health, nursing, pharmacy, dentistry, and medicine, in meeting the needs of healthcare in the twenty-first century [ 30 ]. With an increase in interprofessional teams and an emphasis on collaboration, more effective outcomes are achieved [ 5 ]. Healthcare education leaders are required to work effectively and collaboratively across discipline and organisational boundaries, where titles are not always linked to leadership roles, but may occur in everyday work. Good leadership also means knowing when, and how to support others in their endeavours. Provision of opportunities for leadership development is crucial in improving education sectors and health services, and effecting change. The future belongs to healthcare education leaders who demonstrate excellence in teamwork, clinical skills, patient centred care [ 3 ], and responsibly balance accountability with autonomy.
Take-home message
• Titles are not always linked to leadership roles. • The role of today’s leader requires stepping forward, collaborating and contributing. • A good leader is a good team player who values and seeks the opinions of others. • Leadership requires clear, respectful communication that acknowledges the input and achievements of others. |
Availability of data and materials
Not applicable.
Abbreviations
Human Resources
Bennis W, Nanus. Leaders: the strategies for taking charge. New York: Harper & Row; 1985.
Google Scholar
Northouse P. Leadership: theory and practice. 6th ed. London: Sage; 2011.
Oates K. The new clinical leader. J Paediatr Child Health. 2012;48(6):472–5.
Article Google Scholar
Laverack G. The pocket guide to health promotion. McGraw-Hill Education: Maidenhead; 2014.
Clarke J. In: Patole S, editor. Management and Leadership – A Guide for Clinical Professionals. Switzerland: Springer International Publishing; 2015.
Swanwick T, McKimm J. What is clinical leadership and why is it important. Clin Teach. 2011;8:22–6.
Byrman A. Leadership in organisations. In: Clegg SR, Harvey C, Nord WR, editors. Handbook of Organisational studies. London: Sage; 2006.
Westley F, Minztberg H. Visionary leadership and strategic management. Strateg Manag J. 1989;10:17–37.
Bass B, Avolio B. Improving Organisational effectiveness through transformational leadership. Thousand Oaks, CA: Sage; 1994.
Coulson A. The managerial work of Headteachers. Sheffield: Sheffield City Polytechnic; 1986.
Alimo-Metcalfe B, Alban-Metcalfe J. Leadership in public organisations. In: Storey, editor. Leadership in Organisations: current issues and key trends. London: Routledge; 2004.
McKimm J, Swanwick T. Educational leadership. Scotland, Edinburgh: Associate for the Study of Medical Education; 2007.
Levi D. Group dynamics for teams. Thousand Oaks, CA: Sage; 2011.
Burgess A, McGregor D, Mellis C. Applying guidelines in a systematic review of team-based learning in medical schools. Acad Med. 2014;89(4):678–88.
Pearce CL, Manz CC, Sims HP. Where do we go from here? Is shared leadership the key to team success? Orgnisational Dynamics. 2009;38(3):234–8.
Morgeson FP, DeRue DS, Karan EP. Leadership in teams: a functional approach to understanding leadership structures and processes. J Manag. 2010;36(1):5–39.
Kozlowski SWJ, Gully SM, Salas E, Cannon-Bowers JA. Team leadership and development: theory, principles, and guidelines for training leaders and teams. Dallas, TX: Third Symposium on Work Teams, University of North Texas; 1995.
Tuckman B. Developmental sequence in small groups. Psychol Bull. 1965;63:384–9.
Belbin RM. Management teams: why they succeed or fail. London: Heinmann; 1991.
Glover Takahshi S, Abbott C, Oswalk A, Frank JR. CanMEDS Teaching and Assessment Tools Guide. Royal College of Physicians and Surgeons of Canada; 2015.
Clawson J. Level three leadership: Getting below the surface (3rd ed.). Saddle River, N.J: Pearson Prentice Hall; 2006.
McKimm J. Developing tomorrow’s leaders in health and social care education. Case studies in leadership in medical and health care education. Special report 5. Newcastle-upon-Tyne: Higher Education Academy, Medicine Dentistry and Veterinary Medicine, 2004.
McKimm J, Swanwick T. Leadership development for clinicians: what are we trying to achieve? Clin Teach. 2011;8:181–5.
Norcini JJ, Banda SS. The global health workforce shortage: role of surgeons and other providers. Adv Surg. 2008;42:63–85.
Kim T. Succession planning in hospitals and association with organizational performance. Nurs Econ. 2012;30(1):14–20.
Swanwick T, McKimm J. Clinical leadership development requires system-wide interventions, not just courses. Clin Teach. 2012;9:89–93.
Matthews JH, Morley GL, Crossley E, Bhanderi S. Teaching leadership: the medical student society model. Clin Teach. 2017;15:2.
Burgess A, van Diggele C, Mellis C. Mentorship in the health professions: a review. Clin Teach. 2018;14:1–6.
Burgess A, Dornan T, Clarke A, Menezes A, Mellis C. Peer tutoring in a medical school: perceptions of tutors and tutees. BMC Medical Education. 2016;16:85.
Druker PF. What makes an effective executive? Harv Bus Rev. 2004;82(6):58–63 136.
Download references
Acknowledgements
About this supplement.
This article has been published as part of BMC Medical Education Volume 20 Supplement 2, 2020: Peer Teacher Training in health professional education. The full contents of the supplement are available online at URL. https://bmcmedicaleducation.biomedcentral.com/articles/supplements/volume-20-supplement-2 .
No funding was received.
Author information
Authors and affiliations.
The University of Sydney, Faculty of Medicine and Health, The University of Sydney, Edward Ford Building A27, Sydney, NSW, 2006, Australia
Christie van Diggele
The University of Sydney, Faculty of Medicine and Health, Sydney Health Professional Education Research Network, The University of Sydney, Sydney, Australia
Christie van Diggele, Annette Burgess & Chris Roberts
The University of Sydney, Faculty of Medicine and Health, Sydney Medical School – Education Office, The University of Sydney, Sydney, Australia
Annette Burgess & Chris Roberts
The University of Sydney, Faculty of Medicine and Health, Sydney Medical School – Central Clinical School, The University of Sydney, Sydney, Australia
Craig Mellis
You can also search for this author in PubMed Google Scholar
Contributions
CVD, AB and CM contributed to the drafting, and critical review of the manuscript. CR contributed to the critical review of the manuscript. All authors read and reviewed the final version of the manuscript.
Corresponding author
Correspondence to Christie van Diggele .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors have no competing interests to declare.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
van Diggele, C., Burgess, A., Roberts, C. et al. Leadership in healthcare education. BMC Med Educ 20 (Suppl 2), 456 (2020). https://doi.org/10.1186/s12909-020-02288-x
Download citation
Published : 03 December 2020
DOI : https://doi.org/10.1186/s12909-020-02288-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Leadership theory
- Role models
- Organisational goals
BMC Medical Education
ISSN: 1472-6920
- General enquiries: [email protected]

High-Impact Leadership: Improve Care, Improve the Health of Populations, and Reduce Costs
This white paper presents three interdependent dimensions of leadership that together define high-impact leadership in health care: new mental models, High-Impact Leadership Behaviors, and the IHI High-Impact Leadership Framework.
- Three interdependent dimensions of leadership that together define high-impact leadership in health care
- IHI High-Impact Leadership Framework: A guide for where leaders need to focus efforts and resources to drive improvement and innovation
- Examples to illustrate High-Impact Leadership Behaviors in real-world practice
Note: French translation of this paper also available for download.
Leaders at all levels in care delivery organizations, not just senior executives, are struggling with how to focus their leadership efforts and achieve Triple Aim results — better health, better care, at lower cost — for the populations they serve. High-impact leadership is required.
This white paper presents three interdependent dimensions of leadership that together define high-impact leadership in health care.
- New Mental Models: We propose a set of ideas that constitute new mental models for leaders as they redesign care delivery systems to compete on value, rather than on volume, and deliver Triple Aim results for the populations they serve.
- High-Impact Leadership Behaviors: Aligned with the mental models, we recommend five leadership behaviors to accelerate cultural change and support efforts to achieve Triple Aim results. These leadership behaviors, when practiced systematically, are cross-cutting, supporting many key leadership efforts and initiatives at once.
- IHI High-Impact Leadership Framework: Building on IHI’s legacy leadership models and thinking, the IHI High-Impact Leadership Framework presents an updated, simpler leadership framework that serves as a guide for where leaders need to focus efforts and resources in order to drive improvement and innovation. This updated framework adds three essential areas of leadership efforts: driven by persons and community; shape desired organizational culture; and engage across traditional boundaries of health care systems.
The white paper also includes examples from a variety of health care leaders, to help illustrate High-Impact Leadership Behaviors in real-world practice.
How to Cite This Paper: Swensen S, Pugh M, McMullan C, Kabcenell A. High-Impact Leadership: Improve Care, Improve the Health of Populations, and Reduce Costs . IHI White Paper. Cambridge, MA: Institute for Healthcare Improvement; 2013. (Available at ihi.org)
Overview of High-Impact Leadership
White paper co-author Michael Pugh gives a synopsis of the white paper's three major sections and explains why all leaders should read the paper.
Download High-Impact Leadership White Paper
* Required fields
Related Resources
This website is intended for healthcare professionals

- { $refs.search.focus(); })" aria-controls="searchpanel" :aria-expanded="open" class="hidden lg:inline-flex justify-end text-gray-800 hover:text-primary py-2 px-4 lg:px-0 items-center text-base font-medium"> Search
Search menu
Alban-Metcalfe J, Alimo-Metcalfe B. Reliability and validity of the ‘leadership competencies and engaging leadership scale’. International Journal of Public Sector Management. 2013; 26:(1)56-73 https://doi.org/10.1108/09513551311294281
Avery GC. Understanding leadership: paradigms and cases.London: Sage; 2004
Avolio BJ, Waldman DA, Yammarino FJ. Leading in the 1990s: the four I's of transformational leadership. Journal of European Industrial Training. 1991; 15:(4) https://doi.org/10.1108/03090599110143366
Baker SD. Followership: the theoretical foundation of a contemporary construct. Journal of Leadership & Organizational Studies. 2007; 14:(1)50-60 https://doi.org/10.1177/0002831207304343
Binci D, Cerruti C, Braganza A. Do vertical and shared leadership need each other in change management?. Leadership and Organization Development Journal. 2016; 37:(5)558-578 https://doi.org/10.1108/LODJ-08-2014-0166
Braun S, Peus C, Weisweiler S, Frey D. Transformational leadership, job satisfaction, and team performance: a multilevel mediation model of trust. Leadership Quarterly. 2013; 24:(1)270-283 https://doi.org/10.1016/j.leaqua.2012.11.006
Carson JB, Tesluk PE, Marrone JA. Shared Leadership in teams: an investigation of antecedent conditions and performance. Academy of Management Journal. 2007; 50:(5)1217-1234
Summary of key research findings from the NHS staff survey. NHS Survey Coordination Centre. 2018. https://tinyurl.com/y4ofshoy (accessed 13 March 2019)
Deinert A, Homan AC, Boer D, Voelpel SC, Gutermann D. Transformational leadership sub-dimensions and their link to leaders' personality and performance. Leadership Quarterly. 2015; 26:(6)1095-1120 https://doi.org/10.1016/j.leaqua.2015.08.001
Report of the committee of inquiry into allegations of ill-treatment of patients and other irregularities at the Ely Hospital.Cardiff. London: HMSO; 1969
D'Innocenzo L, Mathieu JE, Kukenberger MR. A meta-analysis of different forms of shared leadership–team performance relations. Journal of Management. 2016; 42:(7)1964-1991 https://doi.org/10.1177/0149206314525205
Authentic leadership theory and practice: origins, effects and development. In: Gardner WL, Avolio BJ, Walumbwa FO (eds). Bingley: Emerald Press; 2005
Gillespie NA, Mann L. Transformational leadership and shared values: the building blocks of trust. Journal of Managerial Psychology. 2004; 19:(6)588-607 https://doi.org/10.1108/02683940410551507
Improving quality in the English NHS. A strategy for action. 2016. https://tinyurl.com/yxavguvr (accessed 13 March 2013)
Hamlin RG. A study and comparative analysis of managerial and leadership effectiveness in the National Health Service: an empirical factor analytic study within an NHS trust hospital. Health Serv Manage Res.. 2002; 15:(4)245-263 https://doi.org/10.1258/095148402320589046
Health Foundation. Transformational change in NHS providers. 2015. https://tinyurl.com/y5jryfgu (accessed 13 March 2013)
Jackson B, Parry K. A very short, fairly interesting and reasonably cheap book about studying leadership, 2nd edn. London: Sage; 2011
Investigating collaborative leadership for communities of practice in learning and skills. 2007. https://tinyurl.com/y5uuhly9 (accessed 13 March 2019)
The King's Fund. The future of management and leadership: no more heroes. 2011. https://tinyurl.com/yakyju8b (accessed 13 March 2019)
Merkens BJ., Spencer JS. A successful and necessary evolution to shared leadership: a hospital's story. Leadership in Health Services. 1998; 11:(1)1-4
NHS Leadership Academy. Healthcare leadership model: the nine dimensions of leadership behaviour. 2013. https://tinyurl.com/ybwfg7b7 (accessed 13 March 2019)
NHS Survey Coordination Centre. NHS staff survey 2017. National briefing. 2018. https://tinyurl.com/y6tla4bw (accessed 13 March 2019)
Nicolaides VC, LaPort KA, Chen TR The shared leadership of teams: a meta-analysis of proximal, distal, and moderating relationships. The Leadership Quarterly. 2014; 25:(5)923-942
Pearce CL, Sims HP. Shared leadership: toward a multi-level theory of leadership. Advances in Interdisciplinary Studies of Work Teams. 2000; 7:115-139
Robert LP, You S. Are you satisfied yet? Shared leadership, individual trust, autonomy, and satisfaction in virtual teams. Journal of the Association of Information Science and Technology. 2018; 69:(4)503-511
Saks AM. Antecedents and consequences of employee engagement. Journal of Managerial Psychology. 2006; 21:(7)600-619
Can we never learn? Abuse, complaints and inquiries in the NHS. History and Policy. 2015. https://tinyurl.com/yypm45ae (accessed 13 March 2019)
Tsai Y, Wu S-W. The relationships between organisational citizenship behaviour, job satisfaction and turnover intention. J Clin Nurs.. 2010; 19:(23–24)3564-3574 https://doi.org/10.1111/j.1365-2702.2010.03375.x
Tse H, Chiu W. Transformational leadership and job performance: a social identity perspective. Journal of Business Research. 2014; 67:(1)2827-2835 https://doi.org/10.1016/j.jbusres.2012.07.018
Uhl-Bien M, Riggio R, Lowe K, Carsten M. Followership theory: a review and research agenda. Leadership Quarterly. 2014; 25:(1)83-104 https://doi.org/10.1016/j.leaqua.2013.11.007
Wang XF., Howell JM. A multilevel study of transformational leadership, identification, and follower outcomes. Leadership Quarterly. 2012; 23:(5)775-790 https://doi.org/10.1016/j.leaqua.2012.02.001
It's not about the money: staff engagement comes first. 2018. https://tinyurl.com/yxnpqhj3 (accessed 13 March 2019)
Leadership and leadership development in health care: the evidence base. 2015. https://tinyurl.com/ybsmpmwn (accessed 13 March 2019)
Zhua W, Avolio BJ, Riggio RE, Sosik JJ. The effect of authentic transformational leadership on follower and group ethics. Leadership Quarterly. 2011; 22:(5)801-817
Models of leadership and their implications for nursing practice
S'thembile Thusini
MSc Student, Florence Nightingale Faculty of Nursing, Midwifery and Palliative Care, King's College London
View articles · Email S'thembile
Julia Mingay
Lecturer, Florence Nightingale Faculty of Nursing, Midwifery and Palliative Care, King's College London
View articles
Leadership in today's NHS, either as a leader or follower, is everybody's business. In this article, an MSc student undertaking the Developing Professional Leadership module at King's College London describes two leadership models and considers their application to two dimensions of the NHS Healthcare Leadership Model: ‘Engaging the team’ and ‘Leading with care’. The author demonstrates the value of this knowledge to all those involved in health care with a case scenario from clinical practice and key lessons to help frontline staff in their everyday work.
The Ely inquiry into the systematic brutal treatment of patients in a Cardiff mental institution was the first formal inquiry into NHS failings ( Department of Health and Social Security, 1969 ). Since that time there have been more than 100 inquiries with inadequate leadership persistently identified as a major concern ( Sheard, 2015 ). National responses have included the NHS Healthcare Leadership Model, delivered by the NHS Leadership Academy and its partners (2013) . A range of online and face-to-face programmes aim to increase an organisation's leadership capacity by developing leaders who pay close attention to their frontline staff, understand the contexts in which they work and the situations they face and empower them to lead continuous improvements that enhance patient outcomes and safety ( NHS Leadership Academy, 2013 ).
At King's College London, ‘Developing Professional Leadership’ is a core module of the Advanced Practice (Leadership) pathway. The module critically appraises theoretical and professional perspectives on leadership and supports participants to take up leadership roles with attention to ethical practice. Both national and college leadership activities promote an understanding of vertical transformational leadership (VTL) and shared leadership (SL).
Register now to continue reading
Thank you for visiting British Journal of Nursing and reading some of our peer-reviewed resources for nurses. To read more, please register today. You’ll enjoy the following great benefits:
What's included
Limited access to clinical or professional articles
Unlimited access to the latest news, blogs and video content
Signing in with your registered email address

- Admission Requirements
- Student Outcomes
- Student Support
Necessary Skills for Leadership in Healthcare
March 6, 2019
View all blog posts under Articles | View all blog posts under Online Healthcare MBA

Effective healthcare leadership requires applying a variety of skills, including being able to manage conflicts between team members, respond to changes across the industry, adhere to patient safety guidelines and optimize a health organization’s financial performance. In leadership roles such as hospital administrator and medical practice manager, today’s healthcare leaders are expected to excel in all of these capacities and many others. So what’s the best way to develop these abilities?
Earning an online MBA with a healthcare focus ― like the HCMBA from the George Washington University ― is a start, as this advanced degree combines traditional MBA coursework with electives and graduate certificate options in multiple aspects of health management. MBA graduates have the managerial and health-specific expertise to implement well-designed strategies at hospitals, clinics and other practices. Let’s look at some of the particular leadership skills that help healthcare professionals stand out in the job market and thrive in their roles.
An Understanding of Costs, Reimbursements and The Bottom Line
The costs of medical care as well as how providers are reimbursed for their services have changed significantly over time. High-deductible insurance plans have become more common, while premiums have also increased substantially. From 2003 to 2018, the average premium for single coverage nearly doubled to $6,896, according to the Kaiser Family Foundation.
At the same time, some medical providers have begun shifting from traditional fee-for-service compensation for services to value-based reimbursement (VBR). The latter model, which is supported by some Centers for Medicare and Medicaid Services programs, evaluates the quality of the care provided in an effort to better align outcomes and costs. It has major ramifications for how providers are paid, and it’s up to health leaders to navigate the transition.
For example, a hospital administrator with an MBA might need to work out the right payment and collection plans, service rates, and patient satisfaction and quality metrics to ensure that the facility is on track to hit its VBR goals. The financial acumen developed in MBA courses in accounting, strategic management, and healthcare quality and outcomes is valuable in handling such tasks.
Conflict Management and Resolution Skills
Conflicts between personnel and departments are common in healthcare settings, due in part to the large number of stakeholders in an environment such as a hospital or clinic. Aside from patients and doctors, nurses and medical staff, there are other engaged parties including department heads, administrators and boards of trustees whose interests also have to be reconciled.
Transformational team leadership in healthcare will ensure that standard processes are in place for remediating conflicts and in turn producing positive outcomes for as many involved individuals or groups as possible. For example, a leader might set up negotiations for a complex problem related to which practitioners patients see when they visit an orthopedics practice.
Such a situation can be tricky to navigate, since it might entail dealing with doctors who prioritize their autonomy, along with patients who have simple ailments that could be treated by a physician’s assistant (PA) but who prefer to see an actual MD. Each conflict will be unique and require a specialized approach.
Healthcare leaders should have the communication skills to serve as effective negotiators and mediators who can minimize the damage of conflicts while also making necessary improvements to processes and working relationships. They should also apply what they have learned in resolving conflicts to the recruiting and hiring processes that they often oversee.
Organizational Change Management
Healthcare environments are constantly evolving. Whether the changes involve new reimbursement models or adjustments in the workloads of doctors and PAs, there’s always the possibility of significant shifts in how a medical practice operates, and health leaders have to be prepared.
A change management strategy in healthcare must encompass everything from how medical personnel and vendors are credentialed to the upgrade cycles for equipment and software in the IT department. Accordingly, a healthcare leader might perform tasks such as:
- Keeping up with applicable changes in the regulatory landscape, including shifts to VBR and rules pertaining to electronic health records
- Identifying causes of medical error and implementing improvements that prioritize patient safety and satisfaction
- Managing an organization after a merger or acquisition, or preparing for the possibility of such a transaction
- Better aligning care delivery with patient expectations, such as through the implementation of telehealth programs or online scheduling portals
- Planning and conducting trainings for personnel so they follow institutional guidelines and regulatory obligations
- Overseeing the rollout of a new IT system such as one that uses cloud-based components
Ultimately, leaders must be proactive in how they manage change in their healthcare organizations. The high stakes of delivering safe and effective care, plus the many moving parts of the health ecosystem, means that a purely reactive approach can put patients and providers at risk. Transformative leaders will anticipate and plan for major changes so patients and teams aren’t left behind.
A Concerted Focus on Patient Safety
We mentioned medical errors earlier, but this issue deserves more attention, as it is one that leaders like hospital administrators will have to confront regularly. Between 250,000 and 400,000 people die annually in the U.S. from preventable errors in hospitals.
These issues can include anything from incorrect dosages of medications to computer errors that misclassify a patient or corrupt data about their condition. Healthcare leaders are responsible for recognizing where and why life-threatening errors occur and introducing the appropriate measures for eliminating them.
An administrator might set up a standardized reporting process for documenting errors, implement specialized technologies that help minimize routine errors in workflows like physician order entry and oversee trainings on best practices for error avoidance. All of these measures can help make the environment safer for patients.
How Can an Online Health MBA Help Develop Leadership Skills?
The online GW HCMBA features a wide-ranging curriculum with courses in MBA subjects such as accounting and strategic management, alongside healthcare-specific electives and graduate certificate options. Moreover, the program’s applied focus helps students reliably put what they’ve learned into practice in real-world healthcare environments so they’re prepared to take on the diverse responsibilities of a modern healthcare leadership role.
To learn more about actual student outcomes for MBA graduates, visit this page . You can also download the program’s brochure for additional details.
Recommended Reading
7 Careers in Healthcare That Leverage Strategic Leadership
How Healthcare Leaders Are Braving Turbulent Times
George Washington University Healthcare MBA Program
The Third-leading Cause of Death in America
Four Steps to Resolving Conflicts in Health Care
What Are The Value-based Programs?
Learn More About the Healthcare MBA Program at GW
Pardon Our Interruption
As you were browsing something about your browser made us think you were a bot. There are a few reasons this might happen:
- You've disabled JavaScript in your web browser.
- You're a power user moving through this website with super-human speed.
- You've disabled cookies in your web browser.
- A third-party browser plugin, such as Ghostery or NoScript, is preventing JavaScript from running. Additional information is available in this support article .
To regain access, please make sure that cookies and JavaScript are enabled before reloading the page.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- BMC Health Serv Res

Priorities and challenges for health leadership and workforce management globally: a rapid review
Carah alyssa figueroa.
School of Public Health and Community Medicine, University of New South Wales, UNSW, Sydney, 2052 Australia
Reema Harrison
Ashfaq chauhan, associated data.
The data that support the findings of this review are included in this published article.
Health systems are complex and continually changing across a variety of contexts and health service levels. The capacities needed by health managers and leaders to respond to current and emerging issues are not yet well understood. Studies to date have been country-specific and have not integrated different international and multi-level insights. This review examines the current and emerging challenges for health leadership and workforce management in diverse contexts and health systems at three structural levels, from the overarching macro (international, national) context to the meso context of organisations through to the micro context of individual healthcare managers.
A rapid review of evidence was undertaken using a systematic search of a selected segment of the diverse literature related to health leadership and management. A range of text words, synonyms and subject headings were developed for the major concepts of global health, health service management and health leadership. An explorative review of three electronic databases (MEDLINE®, Pubmed and Scopus) was undertaken to identify the key publication outlets for relevant content between January 2010 to July 2018. A search strategy was then applied to the key journals identified, in addition to hand searching the journals and reference list of relevant papers identified. Inclusion criteria were independently applied to potentially relevant articles by three reviewers. Data were subject to a narrative synthesis to highlight key concepts identified.
Sixty-three articles were included. A set of consistent challenges and emerging trends within healthcare sectors internationally for health leadership and management were represented at the three structural levels. At the macro level these included societal, demographic, historical and cultural factors; at the meso level, human resource management challenges, changing structures and performance measures and intensified management; and at the micro level shifting roles and expectations in the workplace for health care managers.
Contemporary challenges and emerging needs of the global health management workforce orient around efficiency-saving, change and human resource management. The role of health managers is evolving and expanding to meet these new priorities. Ensuring contemporary health leaders and managers have the capabilities to respond to the current landscape is critical.
Health systems are increasingly complex; encompassing the provision of public and private health services, primary healthcare, acute, chronic and aged care, in a variety of contexts. Health systems are continually evolving to adapt to epidemiological, demographic and societal shifts. Emerging technologies and political, economic, social, and environmental realities create a complex agenda for global health [ 1 ]. In response, there has been increased recognition of the role of non-state actors to manage population needs and drive innovation. The concept of ‘collaborative governance,’ in which non-health actors and health actors work together, has come to underpin health systems and service delivery internationally [ 1 ] in order to meet changing expectations and new priorities. Seeking the achievement of universal health coverage (UHC) and the Sustainable Development Goals (SDGs), particularly in low- and middle-income countries, have been pivotal driving forces [ 2 ]. Agendas for change have been encapsulated in reforms intended to improve the efficiency, equity of access, and the quality of public services more broadly [ 1 , 3 ].
The profound shortage of human resources for health to address current and emerging population health needs across the globe was identified in the World Health Organization (WHO) landmark publication ‘Working together for health’ and continues to impede progress towards the SDGs [ 4 ]. Despite some improvements overall in health workforce aggregates globally, the human resources for health challenges confronting health systems are highly complex and varied. These include not only numerical workforce shortages but imbalances in skill mix, geographical maldistribution, difficulty in inter-professional collaboration, inefficient use of resources, and burnout [ 2 , 5 , 6 ]. Effective health leadership and workforce management is therefore critical to addressing the needs of human resources within health systems and strengthening capacities at regional and global levels [ 4 , 6 – 8 ].
While there is no standard definition, health leadership is centred on the ability to identify priorities, provide strategic direction to multiple actors within the health system, and create commitment across the health sector to address those priorities for improved health services [ 7 , 8 ]. Effective management is required to facilitate change and achieve results through ensuring the efficient mobilisation and utilisation of the health workforce and other resources [ 8 ]. As contemporary health systems operate through networks within which are ranging levels of responsibilities, they require cooperation and coordination through effective health leadership and workforce management to provide high quality care that is effective, efficient, accessible, patient-centred, equitable, and safe [ 9 ]. In this regard, health leadership and workforce management are interlinked and play critical roles in health services management [ 7 , 8 ].
Along with health systems, the role of leaders and managers in health is evolving. Strategic management that is responsive to political, technological, societal and economic change is essential for health system strengthening [ 10 ]. Despite the pivotal role of health service management in the health sector, the priorities for health service management in the global health context are not well understood. This rapid review was conducted to identify the current challenges and priorities for health leadership and workforce management globally.
This review utilised a rapid evidence assessment (REA) methodology structured using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist [ 11 ]. An REA uses the same methods and principles as a systematic review but makes concessions to the breadth or depth of the process to address key issues about the topic under investigation [ 12 – 14 ]. An REA provides a balanced assessment of what is already known about an issue, and the strength of evidence. The narrower research focus, relative to full systematic reviews, make REAs helpful for systematically exploring the evidence around a particular issue when there is a broad evidence base to explore [ 14 ]. In the present review, the search was limited to contemporary literature (post 2010) selected from leading health service management and global health journals identified from exploring major electronic databases.
Search strategy
An explorative review of three core databases in the area of public health and health services (MEDLINE®, Pubmed and Scopus) was undertaken to identify the key publication outlets for relevant content. These databases were selected as those that would be most relevant to the focus of the review and have the broadest range of relevant content. A range of text words, synonyms and subject headings were developed for the major constructs: global health, health service management and health leadership, priorities and challenges. Regarding health service management and health leadership, the following search terms were used: “healthcare manag*” OR “health manag*” OR “health services manag*” OR “health leader*”. Due to the large volume of diverse literature generated, a systematic search was then undertaken on the key journals that produced the largest number of relevant articles. The journals were selected as those identified as likely to contain highly relevant material based on an initial scoping of the literature.
Based on the initial database search, a systematic search for articles published in English between 1 January 2010 and 31 July 2018 was undertaken of the current issues and archives of the following journals: Asia-Pacific Journal of Health Management; BMC Health Services Research; Healthcare Management Review; International Journal of Healthcare Management; International Journal of Health Planning and Management; Journal of Healthcare Management; Journal of Health Organisation and Management; and, Journal of Health Management. Hand-searching of reference lists of identified papers were also used to ensure that major relevant material was captured.
Study selection and data extraction
Results were merged using reference-management software (Endnote) and any duplicates removed. The first author (CF) screened the titles and abstracts of articles meeting the eligibility criteria (Table (Table1). 1 ). Full-text publications were requested for those identified as potentially relevant. The inclusion and exclusion criteria were then independently applied by two authors. Disagreements were resolved by consensus or consultation with a third person, and the following data were extracted from each publication: author(s), publication year, location, primary focus and main findings in relation to the research objective. Sixty-three articles were included in the final review. The selection process followed the PRISMA checklist [ 11 ] as shown in Fig. Fig.1 1 .
Eligibility criteria for selecting studies for the review
| Inclusion criteria | Exclusion criteria |
|---|---|
| Date and language limits | |
| Between 1 January 2010 and 31 July 2018, English | Pre-2010, Non-English |
| Type of publication | |
| Peer-reviewed research articles | Editorials, expert opinions, perspectives, viewpoints, commentaries and other articles where an abstract and methods are not described |
| Study design | |
| All study designs | Description of methods, models and theories without empirical data or findings |
| Content | |
| Reported outcomes relating to global challenges, issues, needs, with reference to health management or leadership. | Analysis of the clinical aspects of management of a specific disease or health condition. Specifically focused on competencies and capabilities in managers and leaders |
| Target group | |
| Managers and leaders in health | Other health care professionals |

PRISMA flow chart of the literature search, identification, and inclusion for the review
Data extraction and analysis
A narrative synthesis was used to explore the literature against the review objective. A narrative synthesis refers to “an approach to the systematic review and synthesis of findings from multiple studies that relies primarily on the use of words and text to summarise and explain the findings of the synthesis” [ 15 ]. Firstly, an initial description of the key findings of included studies was drafted. Findings were then organised, mapped and synthesised to explore patterns in the data.
Search results
A total of 63 articles were included; Table Table2 2 summarizes the data extraction results by region and country. Nineteen were undertaken in Europe, 16 in North America, and one in Australia, with relatively fewer studies from Asia, the Middle East, and small island developing countries. Eighteen qualitative studies that used interviews and/or focus group studies [ 16 – 32 ] were identified. Other studies were quantitative [ 33 – 39 ] including the use of questionnaires or survey data, or used a mixed-method approach [ 40 – 44 ]. Other articles combined different types of primary and secondary data (key informant interviews, observations, focus groups, questionnaire/survey data, and government reports). The included literature also comprised 28 review articles of various types that used mixed data and bibliographic evidence.
Literature included in this review, by context and their references
| Context | Literature describing challenges and emerging trends |
|---|---|
| International | [ , , , , , ] |
| Europe | [ , , , ] |
| Africa | [ ] |
| Australia | [ , ] |
| Botswana | [ ] |
| Brazil | [ , ] |
| Canada | [ – , ] |
| Caribbean | [ ] |
| Costa Rica | [ ] |
| Finland | [ ] |
| Germany | [ ] |
| India | [ , , ] |
| Indonesia | [ ] |
| Iran | [ , , ] |
| Ireland | [ ] |
| Italy | [ ] |
| Netherlands | [ ] |
| Norway | [ ] |
| Pacific Islands | [ ] |
| Portugal | [ ] |
| Spain | [ ] |
| South Korea | [ ] |
| South Africa | [ ] |
| Sweden | [ , ] |
| Switzerland | [ ] |
| Syria | [ ] |
| Tanzania | [ ] |
| Thailand | [ ] |
| Turkey | [ ] |
| United Kingdom (UK) | [ , , , ] |
| United States of America (USA) | [ – , , , , , , , , , ] |
a refers to more than one country situated in different regions including Europe, North America, Asia, and Africa
Key challenges and emerging trends
A set of challenges and emerging trends were identified across healthcare sectors internationally. These were grouped at three levels: 1) macro, system context (society, demography, technology, political economy, legal framework, history, culture), 2) meso, organisational context (infrastructure, resources, governance, clinical processes, management processes, suppliers, patients), and 3) micro context related to the individual healthcare manager (Table (Table3). 3 ). This multi-levelled approach has been used in previous research to demonstrate the interplay between different factors across different levels, and their direct and indirect reciprocal influences on healthcare management policies and practices [ 45 ].
Overview and types of challenges and emerging trends for healthcare managers internationally within the included literature
| Level | Challenge or emerging trend | Aspects of the challenge or emerging trend | References |
|---|---|---|---|
| Societal and system-wide (macro) | Demographic and epidemiological transitions | Population growth | [ , , , ] |
| Ageing populations | [ , , , , , , ] | ||
| Rise in chronic, non-communicable disease and lifestyle-related health issues | [ , – , ] | ||
| High disease burdens and poor health indicators | [ , , ] | ||
| Growing and shifting supply and demand patterns | More patients with complex needs requiring multiple healthcare providers | [ , , , , ] | |
| Hospital capacity issues | [ , ] | ||
| More knowledgeable and health-literate consumers | [ , , ] | ||
| Higher expectations from healthcare organizations (value-for-money) | [ , , , , , ] | ||
| Increasing dissatisfaction with healthcare system | [ ] | ||
| Greater treatment affordability, increased medical tourism, growing health insurance use, rising incomes | [ ] | ||
| Inequalities in access to healthcare | [ , ] | ||
| Advances in science and technology | New Information and communication Technology (ICT) systems | [ , , , , , , ] | |
| Innovations in healthcare services and delivery (electronic medical records, telemedicine, internet-based care, hospital and ward redesign) | [ , , – ] | ||
| New categories or specialization of service providers | [ , ] | ||
| Greater integration and interdisciplinary teams and collaborative healthcare practice | [ , ] | ||
| Political and economic change | Adapting to changes in government and health sector reforms | [ , , , , , , , , , ] | |
| Decentralisation of healthcare | [ , , , , ] | ||
| Budget constraints, measures to avoid deficits | [ , , , , ] | ||
| Disconnection between population needs and resource allocation | [ , , , , , ] | ||
| Lack of or increasing collaboration between governments, health providers, community representatives and other stakeholders to address the needs of healthcare systems | [ , , ] | ||
| Shifting to patient-focused care; greater attention to community health and addressing social determinants of health | [ , , , , , , – , ] | ||
| Corporatisation and privatisation | Emergence of new business models for healthcare; Public–Private Partnership (PPP) models | [ , , , , , ] | |
| Move from independent health organisations to large, networked health systems | [ , , ] | ||
| High or uneven demand for specialist tertiary care | [ , ] | ||
| Growth of the private sector; competition for health professionals | [ , , , , , ] | ||
| Increasing costs | Healthcare costs | [ , , , , , ] | |
| Managerial costs | [ , ] | ||
| Costs associated with developing new programmes | [ , , ] | ||
| Crises in human resources for health | Shortage of trained health personnel, out-migration of skilled health workers | [ , , , , , , , ] | |
| Lack of effective retention strategies and poor working conditions | [ , ] | ||
| Challenge to maintain health services with appropriate skill mixes | [ , , , , ] | ||
| Limited resources and health infrastructure and their maintenance | [ , , , ] | ||
| Deficiencies in health information systems | [ , , ] | ||
| Organisational (meso) | Human resource management challenges | Inefficiency and insufficiencies in provision of health services and use of resources; increased demands for efficiency and cost-cutting | [ , , , , , , – ] |
| Barriers to implementing lean healthcare: outsourcing hospital activities, limited knowledge of lean | [ , ] | ||
| Inadequate planning and performance evaluation systems; poor talent identification; poor deployment and underutilization of staff | [ , , , , , , , , ] | ||
| Lack of support and opportunities in management training and leadership development within organisations | [ , , , , , , , , , ] | ||
| Poor quality of services or concerns of declining quality; poor culture regarding patient safety | [ , , , , , ] | ||
| Changes in organisational structures and measures | Dominant hierarchical culture | [ , , , , , , , ] | |
| Selective recruitment into leadership positions; need for robust succession planning and management | [ , , ] | ||
| Excessive bureaucracy or lack of transparency in organisational rules and processes | [ , , , , ] | ||
| Inadequate systems to prevent and control healthcare associated infections (HAIs) | [ , ] | ||
| Target-driven approach to performance measurement | [ ] | ||
| Fee-for-service payment models encouraging volume not quality of care | [ , , , ] | ||
| Value-based payment models, other new payment models | [ , , , , , , ] | ||
| Intensification of front-line and middle management work | Broad responsibility; balancing clinical, teaching, research and management roles | [ , , , , , , , ] | |
| Long working hours, unpredictable work patterns, tight deadlines, stress and reduced productivity | [ , , , , ] | ||
| Difficulties of middle-level and front-line managers to operationalise executive strategic directions and initiatives (lack of incentives, lack of support, resource constraints, conflict between organisational priorities and employees’ own goals and values) | [ , , , , , , , , , , , ] | ||
| Informal and shared leadership in the front-line in the absence of formal management | [ ] | ||
| Individual (micro) | Shifting health manager role | No universal standard definition for a health manager nor defined competency standards | [ , ] |
| Lack of transparency and accountability | [ , , , , ] | ||
| Increasing dual clinician and manager and leadership roles | [ , , , , , , , ] | ||
| More physicians becoming senior healthcare managers | [ , , ] | ||
| More non-physician health managers, new types of professional healthcare managers | [ , ] |
Societal and system-wide (macro)
Population growth, ageing populations, and increased disease burdens are some of the common trends health systems are facing globally. Developing and developed countries are going through demographic and epidemiological transitions; people are living longer with increasing prevalence of chronic diseases requiring health managers and leaders to adjust to shifting healthcare needs at the population level, delivering preventative and long-term care beyond acute care. Countries in Africa, Europe, the Pacific Islands, Middle East, Asia and Caribbean are seeing an increase in number of patients with non-communicable diseases and communicable diseases [ 21 , 46 – 52 ].
Although many countries have similar emerging health system concerns, there are some differences in the complexities each country faces. For many small countries, outmigration, capacity building and funding from international aid agencies are affecting how their health systems operate, while in many larger countries, funding cuts, rise in private health insurance, innovations, and health system restructuring are major influences [ 21 , 34 , 50 , 53 , 54 ]. In addition, patients are increasingly health literate and, as consumers, expect high-quality healthcare [ 34 , 53 , 54 ]. However, hospitals and healthcare systems are lacking capacity to meet the increased demand [ 16 , 34 , 43 ].
Scientific advances have meant more patients are receiving care across the health system. It is imperative to have processes for communication and collaboration between different health professionals for high-quality care. However, health systems are fragmented; increasing specialisation is leading to further fragmentation and disassociation [ 31 , 54 , 55 ]. Adoption of technological innovations also require change management, hospital restructure, and capacity building [ 56 – 58 ].
Changes in health policies and regulations compound the challenge faced by healthcare managers and leaders to deliver high quality care [ 53 , 54 , 59 ]. Political reforms often lead to health system restructuring requiring change in the values, structures, processes and systems that can constrain how health managers and leaders align their organisations to new agendas [ 24 , 28 , 31 , 60 ]. For example, the distribution of health services management to local authorities through decentralisation has a variable impact on the efficacy and efficiency of healthcare delivery [ 24 , 27 , 35 , 59 ].
Governments’ decisions are often made focusing on cost savings, resulting in budgetary constraints within which health systems must operate [ 16 , 19 , 53 , 61 ]. Although some health systems have delivered positive results under such constraint [ 53 ], often financial resource constraints can lead to poor human and technical resource allocation, creating a disconnect between demand and supply [ 23 , 27 , 40 , 47 , 57 ]. To reduce spending in acute care, there is also a push to deliver health services in the community and focus on social determinants of health, though this brings further complexities related to managing multiple stakeholder collaborations [ 27 , 32 , 34 , 38 , 40 , 49 , 55 ].
Due to an increase in demand and cost constraints, new business models are emerging, and some health systems are resorting to privatisation and corporatisation [ 22 , 48 , 62 ]. This has created competition in the market, increased uptake of private health insurance and increased movement of consumers between various organisations [ 22 , 48 ]. Health managers and leaders need to keep abreast with continuously changing business models of care delivery and assess their impact [ 59 , 62 ]. The evolving international health workforce, insufficient numbers of trained health personnel, and maintaining and improving appropriate skill mixes comprise other important challenges for managers in meeting population health needs and demands (Table (Table3 3 ).
Organisational level (meso)
At the organisation level, human resource management issues were a central concern. This can be understood in part within the wider global human resources for health crisis which has placed healthcare organisations under intense pressure to perform. The evidence suggests healthcare organisations are evolving to strengthen coordination between primary and secondary care; there is greater attention to population-based perspectives in disease prevention, interdisciplinary collaboration, and clinical governance. These trends are challenged by the persistence of bureaucratic and hierarchical cultures, emphasis on targets over care quality, and the intensification of front-line and middle-management work that is limiting capacity.
Healthcare managers and leaders also face operational inefficiencies in providing primary health and referral services to address highly complex and shifting needs which often result in the waste of resources [ 49 , 63 , 64 ]. Considering the pace of change, organisations are required to be flexible and deliver higher quality care at lower cost [ 21 , 53 , 65 ]. To achieve this, many organisations in developing and developed countries alike are adopting a lean model [ 17 , 21 ]. However, there are challenges associated with ensuring sustainability of the lean system, adjusting organisational hierarchies, and improving knowledge of the lean model, especially in developing countries [ 17 , 21 ].
Healthcare organisations require various actors with different capabilities to deliver high quality care. However, a dominant hierarchical culture and lack of collaborative and distributed culture can limit the performance of healthcare organisations [ 22 , 36 , 54 ]. In addition, considering high turnover of executive leadership, healthcare organisations often rely on external talent for succession management which can reduce hospital efficiency [ 44 , 66 ]. Other contributors to weakened hospital performance include: the lack of allocative efficiency and transparency [ 24 , 30 , 64 , 67 ]; poor hospital processes that hamper the development of effective systems for the prevention and control of hospital acquired infections (HAIs) [ 53 , 68 ]; and, payment reforms such as value-based funding and fee-for-service that encourage volume [ 18 , 23 , 24 , 61 , 62 , 69 , 70 ].
Managerial work distribution within organisations is often not clearly defined, leading to extra or extreme work conditions for middle and front-line managers [ 29 , 42 , 53 , 70 ]. Unregulated and undefined expectations at the organisation level leads to negative effects such as stress, reduced productivity, and unpredictable work hours, and long-term effects on organisational efficiency and delivery of high quality care [ 22 , 28 , 29 , 37 , 42 , 51 , 71 ]. Furthermore, often times front-line clinicians are also required to take the leadership role in the absence of managers without proper training [ 20 ]. Despite this, included studies indicate that the involvement of middle and front-line managers in strategic decision-making can be limited due to various reasons including lack of support from the organisation itself and misalignment of individual and organisational goals [ 16 , 26 , 31 , 72 ].
Individual level (micro)
Worldwide, middle and front-line health managers and leaders are disproportionately affected by challenges at the system and organisational level, which has contributed to increasing and often conflicting responsibilities. Some countries are experiencing a growth in senior health managers with a clinical background, while in other countries, the converse is apparent. Indistinct organisational boundaries, increasing scope of practice, and lack of systemic support at policy level are leaving healthcare managers with undefined roles [ 28 , 59 ]. Poorly defined roles contribute to reduced accountability, transparency, autonomy, and understanding of responsibilities [ 24 , 30 , 31 , 67 ]. Studies also indicate a lack of recognition of clinical leaders in health organisations and inadequate training opportunities for them as such [ 20 , 67 ].
The number of hybrid managers (performing clinical and managerial work concurrently) in developed countries is increasing, with the perception that such managers improve the clinical governance of an organization. In contrast, the number of non-clinical managers in many developing countries appears to be increasing [ 63 , 73 – 75 ]. Included studies suggest this approach does not necessarily improve manager-clinical professional relationships or the willingness of clinicians becoming managers, limiting their participation in strategic decisions [ 28 , 70 , 71 , 74 ].
This rapid review highlights the current global climate in health service management, the key priority areas, and current health management approaches being utilised to address these. The multitude of issues emerging demonstrate the complex and evolving role of health service management in the wider complex functioning of health systems globally in a changing healthcare landscape. Key themes of achieving high quality care and sustainable service delivery were apparent, often evidenced through health reforms [ 5 ]. The influence of technological innovation in both its opportunities and complexities is evident worldwide. In the context of changing healthcare goals and delivery approaches, health management is seeking to professionalise as a strategy to build strength and capacity. In doing so, health managers are questioning role scope and the skills and knowledge they need to meet the requirements of the role.
Global challenges facing health management
Understanding how the features of the macro, meso and micro systems can create challenges for managers is critical [ 19 ]. With continual healthcare reform and increasing health expenditure as a proportion of GDP, distinct challenges are facing high-income Organisation for Economic Co-operation and Development (OECD) countries, middle-income rapidly-developing economies, and low-income, resource-limited countries. Reforms, especially in OECD countries, have been aimed at controlling costs, consolidating hospitals for greater efficiencies, and reconfiguring primary healthcare [ 1 , 76 ]. The changing business models for the delivery of care have wider implications for the way in which health managers conceptualise healthcare delivery and the key stakeholders [ 59 ], for example, the emerging role of private healthcare providers and non-health actors in public health. Changes to the business model of healthcare delivery also has implications for the distribution of power amongst key actors within the system. This is evident in the evolved role of general practitioners (GPs) in the UK National Health Service as leaders of Clinical Commissioning Groups (CCGs). Commissioning requires a different skill set to clinical work, in terms of assessing financial data, the nature of statutory responsibilities, and the need to engage with a wider stakeholder group across a region to plan services [ 77 ]. With new responsibilities, GPs have been required to quickly equip themselves with new management capabilities, reflecting the range of studies included in this review around clinician managers and the associated challenges [ 18 , 28 , 53 , 63 , 70 , 71 , 74 , 75 ].
Central to the role of healthcare managers is the ability to transition between existing and new cultures and practices within healthcare delivery [ 59 ]. Bridging this space is particularly important in the context of increasingly personalized and technologically-driven healthcare delivery [ 54 ]. While advances in knowledge and medical technologies have increased capability to tackle complex health needs, the integration of innovations into existing healthcare management practices requires strong change management [ 73 ]. Health leaders and managers need to be able to rapidly and continually assess the changes required or upon them, the implications, and to transform their analysis into a workable plan to realise change [ 10 ]. Focusing only on the clinical training of health professionals rather than incorporating managerial and leadership roles, and specifically, change management capability may limit the speed and success of innovation uptake [ 22 ].
Implications
Our findings highlight the implications of current priorities within the health sector for health management practice internationally; key issues are efficiency savings, change management and human resource management. In the context of efficiency approaches, health system and service managers are facing instances of poor human and technical resource allocation, creating a disconnect between demand and supply. At the service delivery level, this has intensified and varied the role of middle managers mediating at two main levels. The first level of middle-management is positioned between the front-line and C-suite management of an organisation. The second level of middle-management being the C-suite managers who translate regional and/or national funding decisions and policies into their organisations. Faced with increasing pace of change, and economic and resource constraints, middle managers across both levels are now more than ever exposed to high levels of stress, low morale, and unsustainable working patterns [ 29 ]. Emphasis on cost-saving has brought with it increased attention to the health services that can be delivered in the community and the social determinants of health. Connecting disparate services in order to meet efficiency goals is a now a core feature of the work of many health managers mediating this process.
Our findings also have implications for the conceptualisation of healthcare management as a profession. The scale and increasing breadth of the role of health leaders and managers is evident in the review. Clarifying the professional identity of ‘health manager’ may therefore be a critical part of building and maintaining a robust health management workforce that can fulfil these diverse roles [ 59 ]. Increasing migration of the healthcare workforce and of population, products and services between countries also brings new challenges for healthcare. In response, the notion of transnational competence among healthcare professionals has been identified [ 78 ]. Transnational competence progresses cultural competence by considering the interpersonal skills required for engaging with those from diverse cultural and social backgrounds. Thus, transnational competence may be important for health managers working across national borders. A key aspect of professionalisation is the education and training of health managers. Our findings provide a unique and useful theoretical contribution that is globally-focused and multi-level to stimulate new thinking in health management educators, and for current health leaders and managers. These findings have considerable practical utility for managers and practitioners designing graduate health management programs.
Limitations
Most of the studies in the field have focused on the Anglo-American context and health systems. Notwithstanding the importance of lessons drawn from these health systems, further research is needed in other regions, and in low- and middle-income countries in particular [ 79 ]. We acknowledge the nuanced interplay between evidence, culture, organisational factors, stakeholder interests, and population health outcomes. Terminologies and definitions to express global health, management and leadership vary across countries and cultures, creating potential for bias in the interpretation of findings. We also recognise that there is fluidity in the categorisations, and challenges arising may span multiple domains. This review considers challenges facing all types of healthcare managers and thus lacks discrete analysis of senior, middle and front-line managers. That said, managers at different levels can learn from one another. Senior managers and executives may gain an appreciation for the operational challenges that middle and front-line managers may face. Middle and front-line managers may have a heightened awareness of the more strategic decision-making of senior health managers. Whilst the findings indicate consistent challenges and needs for health managers across a range of international contexts, the study does not capture country-specific issues which may have consequences at the local level. Whilst a systematic approach was taken to the literature in undertaking this review, relevant material may have been omitted due to the limits placed on the rapid review of the vast and diverse health management literature. The inclusion of only materials in English language may have led to further omissions of relevant work.
Health managers within both international and national settings face complex challenges given the shortage of human resources for health worldwide and the rapid evolution of national and transnational healthcare systems. This review addresses the lack of studies taking a global perspective of the challenges and emerging needs at macro (international, national and societal), meso (organisational), and micro (individual health manager) levels. Contemporary challenges of the global health management workforce orient around demographic and epidemiological change, efficiency-saving, human resource management, changing structures, intensified management, and shifting roles and expectations. In recognising these challenges, researchers, management educators, and policy makers can establish global health service management priorities and enhance health leadership and capacities to meet these. Health managers and leaders with adaptable and relevant capabilities are critical to high quality systems of healthcare delivery.
Acknowledgements
Not applicable
The rapid review is part of a larger study on global health management priorities and qualities, supported by the University of New South Wales, Sydney.
Availability of data and materials
Abbreviations.
| CCGs | Clinical Commissioning Groups |
| GPs | General practitioners |
| HAIs | Hospital acquired infections |
| OECD | Organisation for Economic Co-operation and Development |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| REA | Rapid evidence assessment |
| SDGs | Sustainable Development Goals |
| UHC | Universal health coverage |
| WHO | World Health Organization |
Authors’ contributions
CF conducted the database searches and identification of relevant literature. RH and AC assessed the selected literature. RH and LM conceived the design of the review and contributed to the interpretation of the review results. CF drafted the initial manuscript while RH, AC and LM reviewed and revised subsequent drafts of the manuscript for important intellectual content. All authors read and approved the final version of the manuscript.
Ethics approval and consent to participate
Consent for publication, competing interests.
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Carah Alyssa Figueroa, Email: ua.ude.wsnu@harac .
Reema Harrison, Email: [email protected] .
Ashfaq Chauhan, Email: [email protected] .
Lois Meyer, Email: [email protected] .

IMAGES
VIDEO
COMMENTS
This leadership style provides a leader without any official assignment, known as an "opinion leader", whose educational and behavioral background is suitable for the working context. ... [6,13,14], a leader should have both a high education in healthcare leadership and the behavioral qualities necessary for establishing strong human ...
Nurse leaders make a difference in workplace culture and drive positive changes in health care legislation. When a team admires the qualities of their leader, it boosts morale and promotes a psychologically safe workplace, which leads to higher job satisfaction and retention rates. Influential leaders in nursing ensure that the organization's ...
The central component in impactful healthcare decisions is evidence. Understanding how nurse leaders use evidence in their own managerial decision making is still limited. This mixed methods systematic review aimed to examine how evidence is used to solve leadership problems and to describe the measured and perceived effects of evidence-based leadership on nurse leaders and their performance ...
The importance of leadership in healthcare. Effective leadership in healthcare is incredibly important, especially when considering the expense of modern care. Here's a closer look at the various ways that effective leadership can make a lasting impact. 1. Improves quality of care. Effective leadership is integral to quality healthcare.
Abstract. Effective leadership by healthcare professionals is vital in modern healthcare settings. The major factor underpinning this is the drive to improve the quality of healthcare provision on a background of ever increasing healthcare demands and need for increased efficiency and productivity. There are many reasons why quality improvement ...
Introduction. Changes in healthcare worldwide have led to an emphasis on leadership development in healthcare professions, which include medical, dental, public health, nursing, and allied health providers (eg, audiology, nutrition, occupational therapy, physical therapy, pharmacy, respiratory therapy, radiography, speech-language therapy) to meet current healthcare needs. 1-3 These changes ...
We used a concept mapping approach to create a model specific to the needs of learning in healthcare leadership. Our model was developed based on a comprehensive literature review, focus groups, concept mapping, and hierarchical clustering. Each of the 33 competency statements is an important concept of healthcare leadership.
Effective leadership is a complex and highly valued component of healthcare education, increasingly recognised as essential to the delivery of high standards of education, research and clinical practice. To meet the needs of healthcare in the twenty-first century, competent leaders will be increasingly important across all health professions, including allied health, nursing, pharmacy ...
The white paper also includes examples from a variety of health care leaders, to help illustrate High-Impact Leadership Behaviors in real-world practice. How to Cite This Paper: Swensen S, Pugh M, McMullan C, Kabcenell A. High-Impact Leadership: Improve Care, Improve the Health of Populations, and Reduce Costs. IHI White Paper.
Here are some traits and habits of effective leaders in health care: 1. Take mentorship roles. Leaders often take an interest in guiding and supporting others, especially those who are new to the industry or their workplace. As mentors, leaders work directly with junior members of their team to support them in gaining the skills needed to excel ...
Research Evidence. Despite thousands of publications on the topic of leadership in healthcare, a recent review (West et al. 2015) reveals relatively little research conducted to a high academic standard. In addition, much of what is written about leadership and much effort on leadership development in the NHS is based on fads and fashions ...
health care settings. Medical trainees at all levels and their supervisors should be trained in the principles and application of transformational leadership. Introduction There are many books and publications on leaders, leadership and the qualities physicians and others must have or learn to become successful leaders. As
Effective leadership is a complex and highly valued component of healthcare education, increasingly recognised as essential to the delivery of high standards of education, research and clinical practice [3]. In order to achieve more effective outcomes, leadership and management skills are now an expectation and requirement in the healthcare ...
Effective. Reliable. Patient-centered. Efficient. Equitable. Quality of care serves a critical role in achieving high levels of productivity, an important goal for any healthcare facility. In healthcare, high levels of productivity refer to increasing the probability of achieving desired health results.
We used a concept mapping approach to create a model specific to the needs of learning in healthcare leadership. Our model was developed based on a comprehensive literature review, focus groups, concept mapping, and hierarchical clustering. Each of the 33 competency statements is an important concept of healthcare leadership.
Abstract. Leadership in today's NHS, either as a leader or follower, is everybody's business. In this article, an MSc student undertaking the Developing Professional Leadership module at King's College London describes two leadership models and considers their application to two dimensions of the NHS Healthcare Leadership Model: 'Engaging the team' and 'Leading with care'.
Charismatic authority stems from an individual's personal qualities and the ability to harness them to inspire and recruit others. This type of leadership is often associated with confidence. Traditional authority. This style of leadership gains its power from tradition. It's often associated with customs and beliefs.
TASK 1 Interprofessional Communication AND Leadership IN Healthcare Reflection ( Revision) Coursework 100%(10) 6. D235 NZM2 Task 1 (1) - task 1. Other 100%(2) 8. Ashley Rhye - interpersonal comm. Coursework None. 6.
Effective healthcare leadership requires applying a variety of skills, including being able to manage conflicts between team members, respond to changes across the industry, adhere to patient safety guidelines and optimize a health organization's financial performance. In leadership roles such as hospital administrator and medical practice ...
Review. Individual-level leadership. According to Day et al. (2014) [], three aspects of leader development are broadly addressed in the literature: identity development, cognitive abilities, and self-leadership.First, leader identity development in healthcare is a complex dynamic process that is shaped by various factors.
In the book Leadership Theory and Practice written by Peter Northouse, he defines 'Leadership as a process whereby an individual influences a group of individuals to achieve a common goal' (Northouse, 2016). Leadership has four main components: (1) it is a process, (2) involves influence, (3) transpires in groups and (4) includes shared goals.
Next, we will consider how the models and processes you've read about in the Leadership Toolkit apply to the events of the assignment. Finally, we'll work through ways you can integrate what you've learned with future clinical practice.
Setting effective leadership as a priority in health care units is expected to enhance a variety of measurable indicators, even in fragmented health systems . Nowadays, more and more regional and national health systems tend to undergo structural changes and redesign their functions and priorities in order to face modern societal, economic, and ...
Medical students have a place in shaping the future of medicine through the AMA. For medical students looking to hone their leadership skills, the AMA offers the chance to distinguish yourself through more than 1,000 leadership opportunities and skill building through online training modules, project-based learning and more. A faculty member and current attending physician offered some ...
AMN Healthcare's hands-on approach to healthcare leadership job search and placement means your specialized skillsets will be used to their maximum potential. Learn more about Leadership opportunities. ... Each new assignment comes with its own set of challenges, including adapting to new work environments, team members, and protocols. This ...
A rapid review of evidence was undertaken using a systematic search of a selected segment of the diverse literature related to health leadership and management. A range of text words, synonyms and subject headings were developed for the major concepts of global health, health service management and health leadership.