- Introduction
- Conclusions
- Article Information
Data are from the National Health Interview Surveys. Shading denotes the 95% CI.
Data are from the National Health Interview Surveys. Shading denotes the 95% CIs. FPL indicates federal poverty level.
eTable 1. Smoking Prevalence Average Annual Percentage Change (AAPC) From 2011 to 2022 by Age and Educational Attainment
eTable 2. Smoking Prevalence Average Annual Percentage Change (AAPC) From 2011 to 2022 by Age and Race and Ethnicity
eFigure 1. US Annual Smoking Prevalence From 2011 to 2022 by Age and Educational Attainment (National Health Interview Survey)
eFigure 2. US Annual Smoking Prevalence From 2011 to 2022 by Age and Race and Ethnicity (National Health Interview Survey)
eFigure 3. US Annual Smoking Prevalence From 2011 to 2022 by Age and Race and Ethnicity With 95% CIs (National Health Interview Survey)
Data Sharing Statement

See More About
Select your interests.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Others Also Liked
- Download PDF
- X Facebook More LinkedIn
Meza R , Cao P , Jeon J , Warner KE , Levy DT. Trends in US Adult Smoking Prevalence, 2011 to 2022. JAMA Health Forum. 2023;4(12):e234213. doi:10.1001/jamahealthforum.2023.4213
Manage citations:
© 2024
- Permissions
Trends in US Adult Smoking Prevalence, 2011 to 2022
- 1 Department of Integrative Oncology, BC Cancer Research Institute, Vancouver, British Columbia, Canada
- 2 School of Population and Public Health, University of British Columbia, Vancouver, British Columbia, Canada
- 3 Department of Epidemiology, University of Michigan, Ann Arbor
- 4 Department of Health Management and Policy, University of Michigan, Ann Arbor
- 5 Lombardi Comprehensive Cancer Center, Georgetown University, Washington, DC
Question Is smoking still decreasing among US adults and do the trends vary by age, income, and race and ethnicity?
Findings In this cross-sectional study of 353 555 adults responding to the 2011 to 2022 National Health Interview Surveys, adults younger than 40 years had dramatic declines in smoking prevalence during the last decade, especially among those with higher incomes. In contrast, relatively slow declines were observed among adults aged 40 to 64 years, with no decrease in smoking among those 65 years or older.
Meaning These findings suggest that the precipitous decline in smoking among younger adults should be maintained, but that additional efforts are required to further reduce smoking in older adults.
Importance President Biden recently prioritized the fight against smoking as key to reducing cancer mortality.
Objective To assess trends in smoking and illuminate the association between smoking and reducing deaths due to cancer.
Design, Setting, and Participants This cross-sectional study used responses to National Health Interview Surveys from January 1, 2011, to December 31, 2022, to characterize trends in current smoking for key sociodemographic groups among US adults.
Exposures Age (18-24, 25-39, 40-64, and ≥65 years), family income (<200%, 200%-399%, and ≥400% of the federal poverty level [FPL]), educational level (less than high school, high school degree or General Educational Development, some college, and college degree or above), and race and ethnicity (Black, Hispanic, White, and other).
Main Outcomes and Measures Weighted current smoking prevalence with 95% CIs by analysis group from 2011 to 2022. Average annual percentage change (AAPC) in smoking prevalence by analysis group is calculated using Joinpoint regression.
Results Data from 353 555 adults surveyed by the National Health Interview Surveys from 2011 to 2022 were included (12.6% Black, 15.0% Hispanic, 65.2% White, and 7.3% other race or ethnicity). Overall, smoking prevalence decreased among adults aged 18 to 24 years from 19.2% (95% CI, 17.5%-20.9%) in 2011 to 4.9% (95% CI, 3.7%-6.0%) in 2022 at an AAPC of −11.3% (95% CI, −13.2% to −9.4%), while it remained roughly constant among adults 65 years or older at 8.7% (95% CI, 7.9%-9.5%) in 2011 and 9.4% (95% CI, 8.7%-10.2%) in 2022 (AAPC, −0.1% [95% CI, −0.8% to 0.7%]). Among adults 65 years or older, smoking prevalence increased from 13.0% (95% CI, 11.2%-14.7%) in 2011 to 15.8% (95% CI, 14.1%-17.6%) for those with income less than 200% FPL (AAPC, 1.1% [95% CI, 0.1%-2.1%]) and remained roughly constant with no significant change for those of higher income. Similar age patterns are seen across educational level and racial and ethnic groups.
Conclusions and Relevance This cross-sectional study found that smoking prevalence decreased from 2011 to 2022 in all age groups except adults 65 years or older, with faster decreases among younger than older adults. These findings suggest that the greatest gains in terms of reducing smoking-attributable morbidity and mortality could be achieved by focusing on individuals with low socioeconomic status, as this population has the highest smoking rates and the worst health prospects.
In a White House fact sheet issued prior to President Biden’s 2023 State of the Union speech, the Biden Administration announced that it would “[t]ackl[e] the biggest single driver of cancer deaths in this country—smoking.” 1 Smoking causes 30% of all cancer deaths and 80% of lung cancer deaths. Peaking in 1990, the age-adjusted male all-cause cancer mortality rate declined by an impressive 38.2% by 2019. Nearly half (47%) of that decrease is attributable to reductions in male lung cancer mortality. 2 Smoking prevention and treatment will also substantially reduce deaths due to other cancers, chronic obstructive pulmonary disease, heart disease, and stroke. Annually, smoking causes 480 000 US deaths.
Smoking rates can be reduced by continuing the recent rapid declines in smoking initiation by youths and young adults and by increasing cessation among older adults. We characterize trends from 2011 to 2022 in adult smoking prevalence by age, with those at younger ages indicating current patterns of initiation and those at older ages indicating the effects of cessation when smoking-attributable disease and death are most common. We also characterize prevalence trends by income, educational attainment, and race and ethnicity to gauge the association of current initiation and cessation with different socioeconomic groups, particularly those with lower socioeconomic status (SES) who are the most vulnerable due to their high smoking and death rates.
This study was approved by the University of Michigan Institutional Review Board and followed the Strengthening the Reporting of Observational Studies in Epidemiology ( STROBE ) reporting guideline. We applied data from the National Health Interview Surveys (NHISs) from January 1, 2011, to December 31, 2022. For each year, we defined people who currently smoke as those who reported smoking 100 or more cigarettes in their lifetime and smoking every day or some days. Informed consent was not required for the use of deidentified data.
We estimated annual smoking prevalence by age group (18-24, 25-39, 40-64, and ≥65 years) and family income, categorized as a percentage of the survey year’s federal poverty level (FPL). 3 We used 3 income categories: less than 200% FPL, 200% to 399% FPL, and 400% or greater FPL. We also conducted analyses by race and ethnicity (Black, Hispanic, White, and other race or ethnicity [American Indian or Alaska Native, Asian, other race or ethnicity, or multiple races or ethnicities]) and educational attainment (less than high school, high school degree or General Educational Development, some college, and college degree or above), as smoking prevalence is known to vary considerably by these variables. Analyses by educational level were restricted to those 25 years or older. Sociodemographic data are based on self-responses to the NHIS questionnaires.
Trends in annual weighted smoking prevalence with 95% CIs by analysis group were estimated using SAS, version 9.4 (SAS Institute Inc), accounting for survey sample weights. For each group, we also calculated the average annual percentage change (AAPC) in smoking prevalence from 2011 to 2022 using the National Cancer Institute Joinpoint Regression Program, version 4.9.1.0. The AAPCs are considered significantly different from zero at α = .05.
Data from 353 555 adults surveyed by the NHIS from 2011 to 2022 were included. Of these, 33.0% had less than 200% FPL income, 29.2% had 200% to 400% FPL income, and 37.8% had greater than 400% FPL income. With respect to race and ethnicity, 12.6% of the sample was Black, 15.0% was Hispanic, 65.2% was White, and 7.3% were of other race or ethnicity. Smoking prevalence decreased from 2011 to 2022 in all age groups except adults 65 years or older, with considerably faster decreases among younger than older adults ( Figure 1 and Table ). Specifically, smoking prevalence decreased among adults aged 18 to 24 years from 19.2% (95% CI, 17.5%-20.9%) in 2011 to 4.9% (95% CI, 3.7%-6.0%) in 2022 at an AAPC of −11.3% (95% CI, −13.2% to −9.4%); among adults aged 25 to 39 years from 22.4% (95% CI, 21.2%-23.6%) in 2011 to 11.4% (95% CI, 10.5%-12.3%) in 2022 at an AAPC of −5.5% (95% CI, −6.7% to −4.4%); and among adults aged 40 to 64 years from 21.2% (95% CI, 20.3%-22.2%) in 2011 to 15.2% (95% CI, 14.4%-16.1%) in 2022 at an AAPC of −3.0% (95% CI, −3.7% to −2.3%). In contrast, among adults 65 years and older, smoking prevalence increased slightly from 8.7% (95% CI, 7.9%-9.5%) in 2011 to 9.4% (95% CI, 8.7%-10.2%) in 2022 (AAPC, −0.1% [95% CI, −0.8% to 0.7%]).
Respondents with the lowest income had the highest smoking prevalence in all age categories. Except for adults 65 years or older ( Figure 2 and Table ), we observed decreases in prevalence across all income groups, albeit at different rates. Among adults 65 years or older with income less than 200% FPL, smoking prevalence increased from 13.0% (95% CI, 11.2%-14.7%) in 2011 to 15.8% (95% CI, 14.1%-17.6%) in 2022 (AAPC, 1.1% [95% CI, 0.1%-2.1%]) and remained roughly constant with no significant change for those with a higher income. In contrast, among adults aged 18 to 24 years, smoking prevalence decreased for all 3 income levels, albeit with the decreases increasing with income level, at an AAPC of −9.6% (95% CI, −11.1% to −8.1%) for those with income of less than 200% FPL, −11.0% (95% CI, −13.4% to −8.5%) for those with income of 200% to 399% FPL, and −14.7% (95% CI, −19.1% to −10.1%) for those with income of 400% FPL or greater. In every age group, the largest reductions in smoking were among those with higher income.
Trends by educational level and race and ethnicity are presented in eTables 1 and 2 in Supplement 1 . Similar age patterns are observed with considerable decline in smoking prevalence across all educational levels and race and ethnicity groups at younger ages and relatively constant or nondecreasing trends at older ages (eFigures 1 to 3 in Supplement 1 ). By educational level, among adults 65 years or older, smoking prevalence significantly decreased only among those with educational attainment of college or above, with a significant increase among those with educational attainment of high school or GED. By race and ethnicity, among adults 65 years or older, smoking prevalence remained constant across all groups, with non–statistically significant increases among Black, Hispanic, and other racial and ethnic groups.
While overall US adult smoking prevalence continues to decline, the constant or increasing trends among those 65 years or older and the relatively slow decreases among adults aged 40 to 64 years, especially for those with lower income and educational levels, are striking. In contrast, those younger than 40 years, particularly those aged 18 to 24 years, have seen dramatic declines in a relatively short period, reaching historically low levels of smoking prevalence, especially among those with higher incomes. While smoking trends since 2019 may reflect the impact of COVID-19, no clear patterns have emerged.
Recent studies have also reported low and rapidly declining rates of smoking among youths. 4 , 5 Our findings indicate that the decreases in youth initiation of smoking are now translating into rapid declines in smoking prevalence among young adults. This suggests further declines in adult prevalence as newer generations with low smoking levels continue to age. However, while the future looks promising for younger populations, relatively constant trends in smoking prevalence among adults 65 years or older and the relatively slow declines among adults aged 40 to 64 years are concerning, since most smoking-related deaths occur at older ages. Increasing smoking cessation, particularly among middle-aged and older adults, is thus critical to further reduce smoking-attributable mortality. Our results underscore the importance of responding to recent calls for increasing support for smoking cessation programs by the US Department of Health and Human Services, 6 the US Food and Drug Administration, 7 , 8 and the US Preventive Services Task Force. 9
The lack of decline among those with low SES (low income or low educational level) and racial and ethnic minority individuals 65 years or older and the consistently higher smoking prevalence among individuals with lower incomes in all age groups indicate the need to target cessation efforts to reduce disparities. 10 A ban on menthol in cigarettes and cigars is associated with reduced racial disparities. 11 Increasing taxes on combustible tobacco products in low-taxing states may reduce disparities across states. 12 These targeted interventions would reduce health disparities and improve health equity by reducing smoking-attributable deaths among those with lower SES. 10
The use of e-cigarettes may also play a role. 13 Increases in e-cigarette use have accompanied substantial reductions in smoking by youths and young adults, although a causal relationship has not been established. 4 , 5 While e-cigarette use is currently much less common among older adults, 14 e-cigarettes could play an important role as a smoking cessation aid for older adults. 15
This study has some limitations. First, we did not consider other tobacco products, such as cigars or e-cigarettes. Second, due to sample size limitations, we did not assess trends at the intersection of income or education and race and ethnicity. Third, we did not consider youth tobacco use.
This cross-sectional study found that smoking prevalence decreased from 2011 to 2022 among all age groups except adults 65 years or older, with faster decreases among younger than older adults. These findings suggest that the greatest gains in reducing smoking-attributable mortality could be attained by focusing efforts on smokers with low SES, the group with the highest smoking rates and worst health prospects.
Accepted for Publication: October 2, 2023.
Published: December 1, 2023. doi:10.1001/jamahealthforum.2023.4213
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2023 Meza R et al. JAMA Health Forum .
Corresponding Author: Rafael Meza, PhD, Department of Integrative Oncology, BC Cancer Research Institute, 675 W 10th Ave, Vancouver, BC V5Z 1L3, Canada ( [email protected] ).
Author Contributions: Dr Meza had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Meza, Levy.
Acquisition, analysis, or interpretation of data: Meza, Cao, Jeon, Warner.
Drafting of the manuscript: Meza, Levy.
Critical review of the manuscript for important intellectual content: Meza, Cao, Jeon, Warner.
Statistical analysis: Meza, Cao, Jeon.
Obtained funding: Meza, Levy.
Administrative, technical, or material support: Cao.
Conflict of Interest Disclosures: Dr Meza reported receiving grant funding from the National Cancer Institute (NCI) and US Food and Drug Administration (FDA) during the conduct of the study. Dr Cao reported receiving grant funding from the NCI and FDA during the conduct of the study. Dr Jeon reported receiving grant funding from the NCI and FDA during the conduct of the study. Dr Warner reported receiving grant funding from the NCI and FDA during the conduct of the study. Dr Levy reported receiving grant funding from the NCI and FDA during the conduct of the study. No other disclosures were reported.
Funding/Support: This research was supported by grant U54CA229974 from the NCI and FDA Center for Tobacco Products (all authors) and grant U01CA253858 from the NCI (Drs Meza, Cao, Jeon, and Levy).
Role of the Funder/Sponsor: The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Disclaimer: The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the FDA.
Data Sharing Statement: See Supplement 2 .
- Skip to main content
- Skip to FDA Search
- Skip to in this section menu
- Skip to footer links

The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
U.S. Food and Drug Administration
- Search
- Menu
- Tobacco Products
Tobacco Science & Research
FDA supports science and research to help us better understand tobacco use and associated risks so that we can reduce the public health burden of tobacco in the United States.
Research programs and projects include, but are not limited to, the scientific fields of epidemiology, behavior, biology, medicine, economics, chemistry, engineering, toxicology, pharmacology, addiction, public health, communications, marketing, and statistics.
Research News
- PATH Study: Wave 1 through 5 Location Characteristics Data now available
- PATH Study Data User Workshop: Apply Now for the Summer 2024 Events
- PATH Study: Wave 7 Restricted-Use Files (RUFs) now available
- CTP and NIDA Announce the Continuation of the Population Assessment of Tobacco and Health (PATH) Study
- FDA & NIH Announce Funding Awards for TCORS 3.0
- PATH Study: Wave 6 Public-Use Files now available
- PATH Study: Wave 6 Restricted-Use Files now available
- PATH Study: Wave 4 and Wave 5 Biomarker Restricted-Use Files (BRUFs) now available, including data from youth participants
- PATH Study: New Special Collection Public-Use Files (SCPUFs): Wave 5.5 and PATH Study Adult Telephone Survey (PATH-ATS)
- PATH Study: New Data Tables and Figures Available: Waves 1 - 5 (2013 – 2019)
- Find statistics about youth tobacco use from the most recent National Youth Tobacco Survey
CTP, in partnership with CDISC, released the Tobacco Implementation Guide (TIG) a resource for stakeholders to use to help standardize data for submission and facilitate tobacco product research and scientific review. Stay current on FDA's tobacco regulatory science and research efforts, tobacco scientific publications and study findings, and research grants by subscribing to CTP's quarterly Spotlight on Science newsletter.
Subscribe to Spotlight on Science
Studies involving administration of unauthorized tobacco products.
If you plan to study tobacco products that do not have marketing authorization or that do not comply with an applicable tobacco product standard, you may submit your proposed protocol to FDA for review. FDA intends to evaluate specific uses of investigational tobacco products on a case-by-case basis according to potential human subject protection concerns or other impacts on public health.
Using Investigational Tobacco Products
Investigators who are designing a protocol involving administration of a tobacco product to humans should review the information below regarding the need for submitting their protocol to Food and Drug Administration (FDA) Center for Tobacco Products (CTP) for review.
Investigators are encouraged to work with tobacco product manufacturers to ensure availability of products to complete planned studies. FDA evaluates the specific uses of investigational tobacco products (ITPs) on a case-by-case basis according to potential human subject protection concerns or other impacts on public health. Generally, submission of protocols by industry and academic researchers for FDA review is a voluntary process; however, FDA will review all protocols submitted. FDA recommends submission of proposed use of ITPs to FDA for review only if the study design is more likely to raise concerns about human subject protection, public health, or both. As discussed by FDA in its February 2019 guidance, Use of Investigational Tobacco Products , factors to consider would be studies that plan to enroll vulnerable populations, particularly those < 21 years old, studies that involve significant increases over the participants’ usual exposure to nicotine, studies that modify the tobacco product in a manner different from that described by the manufacturer or study of a novel product for which there is limited experience and knowledge.
For all clinical studies involving use of ITPs, we recommend that you notify FDA, all participating clinical investigators, and any committee or group formally designated to oversee the study of any serious or unexpected adverse experience associated with the tobacco product you are investigating within a few weeks after initial notification, and that you supply FDA with a completed case report form for the adverse experience. We encourage the reporting of adverse experiences associated with a clinical investigation of an investigational tobacco product to FDA through the FDACTP Safety Reporting Portal for Researchers.
FDA is committed to furthering scientific research on tobacco products and has a major investment in regulatory science. If you plan to study tobacco products that do not have marketing authorization or that do not comply with an applicable tobacco product standard, you may submit your proposed protocol to FDA for review based on the criteria described above. FDA will review any protocols submitted and intends to evaluate specific uses of investigational tobacco products on a case-by-case basis according to potential human subject protection concerns or other impacts on public health. Generally, FDA does not recommend that investigators correspond with us about the use of investigational tobacco products in nonclinical studies as these are not ordinarily reviewed. You may refer to the draft guidance, Use of Investigational Tobacco Products , for more information regarding how to submit your proposed use of an investigational tobacco product and how FDA intends to make enforcement decisions regarding the use of investigational tobacco products.
FDA understands that investigators may choose to obtain tobacco products directly from a tobacco product manufacturer with the sole intent to use the products for research investigations without commercializing the products. In such cases, FDA recommends that investigators add language to all product labels to indicate that these products are limited to investigational use, that study participants be instructed that the products may not be further distributed, and that study protocols include a plan to collect and account for all investigational tobacco products after the study has concluded.
If there are additional questions, investigators should reach out to the FDA CTP at: [email protected].
The email should:
- Clearly and uniquely identify the product(s) you wish to study by brand and sub-brand—including the type or category of tobacco product (e.g., cigarette, smokeless tobacco, cigar, electronic nicotine delivery systems [ENDS], waterpipe tobacco) and subcategory (e.g., closed or open e-cigarette, closed or open e-liquid).
- Provide additional available information such as packaging type, package quantity, and/or characterizing flavor that may help answer the specific question(s)
Once the FDA CTP receives the email, they will make every effort to respond via email within 2weeks.
Note that the FDA CTP intends to respond to investigators within 60 days of receipt of protocols for review. Investigators should receive acknowledgement of the submission with the name and contact information for the assigned Regulatory Health Project Manager (RHPM). If investigators do not receive a response within 60 days, they should contact the RHPM. Investigators may also contact their NIH Program Officer to discuss additional steps/actions.
If the marketed products will be used with investigator-manipulated modification(s), then the investigator should submit an ITP request. In addition to the protocol and other information described in the FDA Draft Guidance, the ITP request should also include:
- A description of the planned modification(s).
- A rationale for how these modification(s) support the study design and do not increase risk to human participants.
Tobacco Researcher Interviews: Meet some of the people who lead tobacco research

Ongoing Research
- Read about the research goals of the Population Assessment of Tobacco and Health (PATH) Study , a collaboration between FDA and NIH, as well as availability of Restricted Use Files (RUF) and Public Use Files (PUF) for Waves 1 & 2.
- Learn about CTP's research priorities that build the science base behind FDA's authority to regulate tobacco products.
- Find out more about the Tobacco Regulatory Science Program (TRSP), FDA's partnership with NIH to foster tobacco regulatory research, including the Tobacco Centers of Regulatory Science (TCORS).
- Learn about FDA's collaboration with CDC on the National Youth Tobacco Survey .
- Review information on Harmful and Potentially Harmful Constituents .
- Understand more about Modified Risk Tobacco Products and the rigorous standards in place to protect the public's health.
Additional Resources
- Products, Ingredients and Components
- FDA's New Regulations for E-Cigarettes, Cigars, and All Other Tobacco Products
- FDA Safety Reporting Portal for Tobacco Products
- Connect with Us
- Tobacco Control Act
Stay current on tobacco regulatory science and research, tobacco scientific publications and study findings, CTP grants, and more in this quarterly newsletter.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 24 March 2022
Tobacco and nicotine use
- Bernard Le Foll 1 , 2 ,
- Megan E. Piper 3 , 4 ,
- Christie D. Fowler 5 ,
- Serena Tonstad 6 ,
- Laura Bierut 7 ,
- Lin Lu ORCID: orcid.org/0000-0003-0742-9072 8 , 9 ,
- Prabhat Jha 10 &
- Wayne D. Hall 11 , 12
Nature Reviews Disease Primers volume 8 , Article number: 19 ( 2022 ) Cite this article
40k Accesses
93 Citations
107 Altmetric
Metrics details
- Disease genetics
- Experimental models of disease
- Preventive medicine
Tobacco smoking is a major determinant of preventable morbidity and mortality worldwide. More than a billion people smoke, and without major increases in cessation, at least half will die prematurely from tobacco-related complications. In addition, people who smoke have a significant reduction in their quality of life. Neurobiological findings have identified the mechanisms by which nicotine in tobacco affects the brain reward system and causes addiction. These brain changes contribute to the maintenance of nicotine or tobacco use despite knowledge of its negative consequences, a hallmark of addiction. Effective approaches to screen, prevent and treat tobacco use can be widely implemented to limit tobacco’s effect on individuals and society. The effectiveness of psychosocial and pharmacological interventions in helping people quit smoking has been demonstrated. As the majority of people who smoke ultimately relapse, it is important to enhance the reach of available interventions and to continue to develop novel interventions. These efforts associated with innovative policy regulations (aimed at reducing nicotine content or eliminating tobacco products) have the potential to reduce the prevalence of tobacco and nicotine use and their enormous adverse impact on population health.
Similar content being viewed by others

Associations between classic psychedelics and nicotine dependence in a nationally representative sample
Use of electronic cigarettes and heated tobacco products during the covid-19 pandemic.
Smoking cessation behaviors and reasons for use of electronic cigarettes and heated tobacco products among Romanian adults
Introduction.
Tobacco is the second most commonly used psychoactive substance worldwide, with more than one billion smokers globally 1 . Although smoking prevalence has reduced in many high-income countries (HICs), tobacco use is still very prevalent in low-income and middle-income countries (LMICs). The majority of smokers are addicted to nicotine delivered by cigarettes (defined as tobacco dependence in the International Classification of Diseases, Tenth Revision (ICD-10) or tobacco use disorder in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5)). As a result of the neuro-adaptations and psychological mechanisms caused by repeated exposure to nicotine delivered rapidly by cigarettes, cessation can also lead to a well-characterized withdrawal syndrome, typically manifesting as irritability, anxiety, low mood, difficulty concentrating, increased appetite, insomnia and restlessness, that contributes to the difficulty in quitting tobacco use 2 , 3 , 4 .
Historically, tobacco was used in some cultures as part of traditional ceremonies, but its use was infrequent and not widely disseminated in the population. However, since the early twentieth century, the use of commercial cigarettes has increased dramatically 5 because of automated manufacturing practices that enable large-scale production of inexpensive products that are heavily promoted by media and advertising. Tobacco use became highly prevalent in the past century and was followed by substantial increases in the prevalence of tobacco-induced diseases decades later 5 . It took decades to establish the relationship between tobacco use and associated health effects 6 , 7 and to discover the addictive role of nicotine in maintaining tobacco smoking 8 , 9 , and also to educate people about these effects. It should be noted that the tobacco industry disputed this evidence to allow continuing tobacco sales 10 . The expansion of public health campaigns to reduce smoking has gradually decreased the use of tobacco in HICs, with marked increases in adult cessation, but less progress has been achieved in LMICs 1 .
Nicotine is the addictive compound in tobacco and is responsible for continued use of tobacco despite harms and a desire to quit, but nicotine is not directly responsible for the harmful effects of using tobacco products (Box 1 ). Other components in tobacco may modulate the addictive potential of tobacco (for example, flavours and non-nicotine compounds) 11 . The major harms related to tobacco use, which are well covered elsewhere 5 , are linked to a multitude of compounds present in tobacco smoke (such as carcinogens, toxicants, particulate matter and carbon monoxide). In adults, adverse health outcomes of tobacco use include cancer in virtually all peripheral organs exposed to tobacco smoke and chronic diseases such as eye disease, periodontal disease, cardiovascular diseases, chronic obstructive pulmonary disease, stroke, diabetes mellitus, rheumatoid arthritis and disorders affecting immune function 5 . Moreover, smoking during pregnancy can increase the risk of adverse reproductive effects, such as ectopic pregnancy, low birthweight and preterm birth 5 . Exposure to secondhand cigarette smoke in children has been linked to sudden infant death syndrome, impaired lung function and respiratory illnesses, in addition to cognitive and behavioural impairments 5 . The long-term developmental effects of nicotine are probably due to structural and functional changes in the brain during this early developmental period 12 , 13 .
Nicotine administered alone in various nicotine replacement formulations (such as patches, gum and lozenges) is safe and effective as an evidence-based smoking cessation aid. Novel forms of nicotine delivery systems have also emerged (called electronic nicotine delivery systems (ENDS) or e-cigarettes), which can potentially reduce the harmful effects of tobacco smoking for those who switch completely from combustible to e-cigarettes 14 , 15 .
This Primer focuses on the determinants of nicotine and tobacco use, and reviews the neurobiology of nicotine effects on the brain reward circuitry and the functioning of brain networks in ways that contribute to the difficulty in stopping smoking. This Primer also discusses how to prevent tobacco use, screen for smoking, and offer people who smoke tobacco psychosocial and pharmacological interventions to assist in quitting. Moreover, this Primer presents emerging pharmacological and novel brain interventions that could improve rates of successful smoking cessation, in addition to public health approaches that could be beneficial.
Box 1 Tobacco products
Conventional tobacco products include combustible products that produce inhaled smoke (most commonly cigarettes, bidis (small domestically manufactured cigarettes used in South Asia) or cigars) and those that deliver nicotine without using combustion (chewing or dipping tobacco and snuff). Newer alternative products that do not involve combustion include nicotine-containing e-cigarettes and heat-not-burn tobacco devices. Although non-combustion and alternative products may constitute a lesser risk than burned ones 14 , 15 , 194 , no form of tobacco is entirely risk-free.
Epidemiology
Prevalence and burden of disease.
The Global Burden of Disease Project (GBDP) estimated that around 1.14 billion people smoked in 2019, worldwide, increasing from just under a billion in 1990 (ref. 1 ). Of note, the prevalence of smoking decreased significantly between 1990 and 2019, but increases in the adult population meant that the total number of global smokers increased. One smoking-associated death occurs for approximately every 0.8–1.1 million cigarettes smoked 16 , suggesting that the estimated worldwide consumption of about 7.4 trillion cigarettes in 2019 has led to around 7 million deaths 1 .
In most populations, smoking prevalence is much higher among groups with lower levels of education or income 17 and among those with mental health disorders and other co-addictions 18 , 19 . Smoking is also more frequent among men than women (Figs 1 – 3 ). Sexual and/or gender minority individuals have disproportionately high rates of smoking and other addictions 17 , 20 . In addition, the prevalence of smoking varies substantially between regions and ethnicities; smoking rates are high in some regions of Asia, such as China and India, but are lower in North America and Australia. Of note, the prevalence of mental health disorders and other co-addictions is higher in individuals who smoke compared with non-smokers 18 , 19 , 21 . For example, the odds of smoking in people with any substance use disorder is more than five times higher than the odds in people without a substance use disorder 19 . Similarly, the odds of smoking in people with any psychiatric disorder is more than three times higher than the odds of smoking in those without a psychiatric diagnosis 22 . In a study in the USA, compared with a population of smokers with no psychiatric diagnosis, subjects with anxiety, depression and phobia showed an approximately twofold higher prevalence of smoking, and subjects with agoraphobia, mania or hypomania, psychosis and antisocial personality or conduct disorders showed at least a threefold higher prevalence of smoking 22 . Comorbid disorders are also associated with higher rates of smoking 22 , 23 .
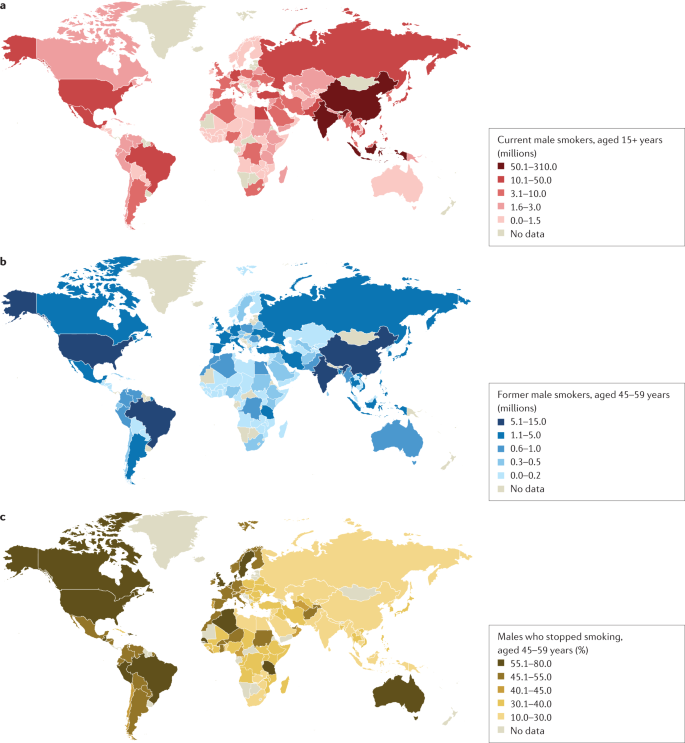
a | Number of current male smokers aged 15 years or older per country expressed in millions. b | Former male smokers aged 45–59 years per country expressed in millions. c | Former male smokers aged 45–59 years per country expressed as the percentage of smokers who stopped. The data shown are for male smokers for the period 2015–2019 from countries with direct smoking surveys. The prevalence of smoking among males is less variable than among females. Data from ref. 1 .
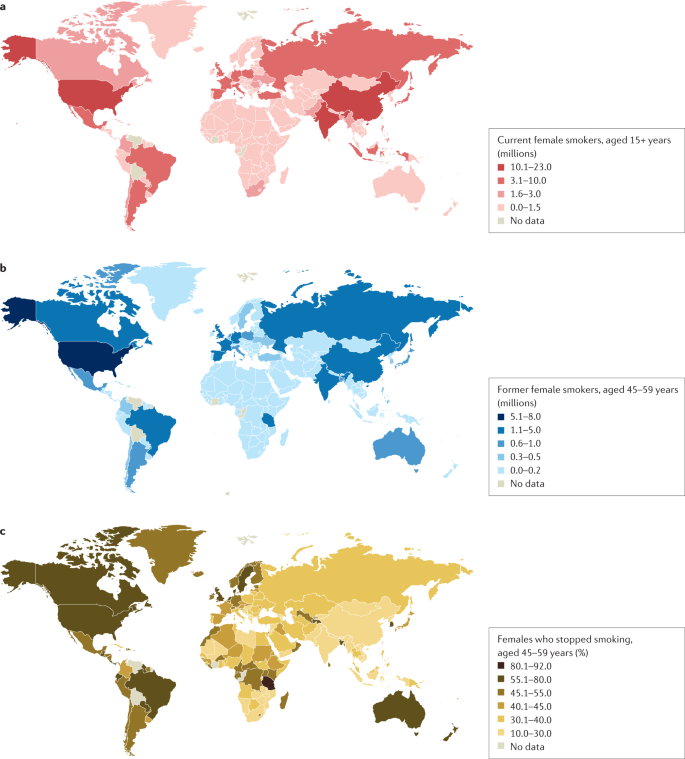
a | Number of current female smokers aged 15 years or older per country expressed in millions. b | Former female smokers aged 45–59 years per country expressed in millions. c | Former female smokers aged 45–59 years per country expressed as the percentage of smokers who stopped. The data shown are for female smokers for the period 2015–2019 from countries with direct smoking surveys. The prevalence of smoking among females is much lower in East and South Asia than in Latin America or Eastern Europe. Data from ref. 1 .
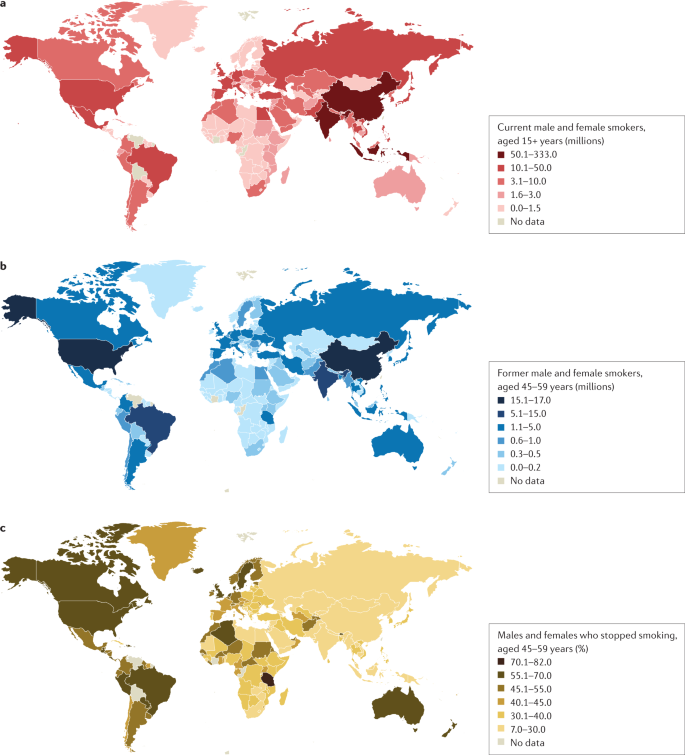
a | Number of current male and female smokers aged 15 years or older per country expressed in millions. b | Former male and female smokers aged 45–59 years per country expressed in millions. c | Former male and female smokers aged 45–59 years per country expressed as the percentage of smokers who stopped. The data shown are for the period 2015–2019 from countries with direct smoking surveys. Cessation rates are higher in high-income countries, but also notably high in Brazil. Cessation is far less common in South and East Asia and Russia and other Eastern European countries, and also low in South Africa. Data from ref. 1 .
Age at onset
Most smokers start smoking during adolescence, with almost 90% of smokers beginning between 15 and 25 years of age 24 . The prevalence of tobacco smoking among youths substantially declined in multiple HICs between 1990 and 2019 (ref. 25 ). More recently, the widespread uptake of ENDS in some regions such as Canada and the USA has raised concerns about the long-term effects of prolonged nicotine use among adolescents, including the possible notion that ENDS will increase the use of combustible smoking products 25 , 26 (although some studies have not found much aggregate effect at the population level) 27 .
Smoking that commences in early adolescence or young adulthood and persists throughout life has a more severe effect on health than smoking that starts later in life and/or that is not persistent 16 , 28 , 29 . Over 640 million adults under 30 years of age smoke in 22 jurisdictions alone (including 27 countries in the European Union where central efforts to reduce tobacco dependence might be possible) 30 . In those younger than 30 years of age, at least 320 million smoking-related deaths will occur unless they quit smoking 31 . The actual number of smoking-related deaths might be greater than one in two, and perhaps as high as two in three, long-term smokers 5 , 16 , 29 , 32 , 33 . At least half of these deaths are likely to occur in middle age (30–69 years) 16 , 29 , leading to a loss of two or more decades of life. People who smoke can expect to lose an average of at least a decade of life versus otherwise similar non-smokers 16 , 28 , 29 .
Direct epidemiological studies in several countries paired with model-based estimates have estimated that smoking tobacco accounted for 7.7 million deaths globally in 2020, of which 80% were in men and 87% were current smokers 1 . In HICs, the major causes of tobacco deaths are lung cancer, emphysema, heart attack, stroke, cancer of the upper aerodigestive areas and bladder cancer 28 , 29 . In some lower income countries, tuberculosis is an additional important cause of tobacco-related death 29 , 34 , which could be related to, for example, increased prevalence of infection, more severe tuberculosis/mortality and higher prevalence of treatment-resistant tuberculosis in smokers than in non-smokers in low-income countries 35 , 36 .
Despite substantial reductions in the prevalence of smoking, there were 34 million smokers in the USA, 7 million in the UK and 5 million in Canada in 2017 (ref. 16 ), and cigarette smoking remains the largest cause of premature death before 70 years of age in much of Europe and North America 1 , 16 , 28 , 29 . Smoking-associated diseases accounted for around 41 million deaths in the USA, UK and Canada from 1960 to 2020 (ref. 16 ). Moreover, as smoking-associated diseases are more prevalent among groups with lower levels of education and income, smoking accounts for at least half of the difference in overall mortality between these social groups 37 . Any reduction in smoking prevalence reduces the absolute mortality gap between these groups 38 .
Smoking cessation has become common in HICs with good tobacco control interventions. For example, in France, the number of ex-smokers is four times the number of current smokers among those aged 50 years or more 30 . By contrast, smoking cessation in LMICs remains uncommon before smokers develop tobacco-related diseases 39 . Smoking cessation greatly reduces the risks of smoking-related diseases. Indeed, smokers who quit smoking before 40 years of age avoid nearly all the increased mortality risks 31 , 33 . Moreover, individuals who quit smoking by 50 years of age reduce the risk of death from lung cancer by about two-thirds 40 . More modest hazards persist for deaths from lung cancer and emphysema 16 , 28 ; however, the risks among former smokers are an order of magnitude lower than among those who continue to smoke 33 .
Mechanisms/pathophysiology
Nicotine is the main psychoactive agent in tobacco and e-cigarettes. Nicotine acts as an agonist at nicotinic acetylcholine receptors (nAChRs), which are localized throughout the brain and peripheral nervous system 41 . nAChRs are pentameric ion channels that consist of varying combinations of α 2 –α 7 and β 2 –β 4 subunits, and for which acetylcholine (ACh) is the endogenous ligand 42 , 43 , 44 . When activated by nicotine binding, nAChR undergoes a conformational change that opens the internal pore, allowing an influx of sodium and calcium ions 45 . At postsynaptic membranes, nAChR activation can lead to action potential firing and downstream modulation of gene expression through calcium-mediated second messenger systems 46 . nAChRs are also localized to presynaptic membranes, where they modulate neurotransmitter release 47 . nAChRs become desensitized after activation, during which ligand binding will not open the channel 45 .
nAChRs with varying combinations of α-subunits and β-subunits have differences in nicotine binding affinity, efficacy and desensitization rate, and have differential expression depending on the brain region and cell type 48 , 49 , 50 . For instance, at nicotine concentrations found in human smokers, β 2 -containing nAChRs desensitize relatively quickly after activation, whereas α 7 -containing nAChRs have a slower desensitization profile 48 . Chronic nicotine exposure in experimental animal models or in humans induces an increase in cortical expression of α 4 β 2 -containing nAChRs 51 , 52 , 53 , 54 , 55 , but also increases the expression of β 3 and β 4 nAChR subunits in the medial habenula (MHb)–interpeduncular nucleus (IPN) pathway 56 , 57 . It is clear that both the brain localization and the type of nAChR are critical elements in mediating the various effects of nicotine, but other factors such as rate of nicotine delivery may also modulate addictive effects of nicotine 58 .
Neurocircuitry of nicotine addiction
Nicotine has both rewarding effects (such as a ‘buzz’ or ‘high’) and aversive effects (such as nausea and dizziness), with the net outcome dependent on dose and others factors such as interindividual sensitivity and presence of tolerance 59 . Thus, the addictive properties of nicotine involve integration of contrasting signals from multiple brain regions that process reward and aversion (Fig. 4 ).
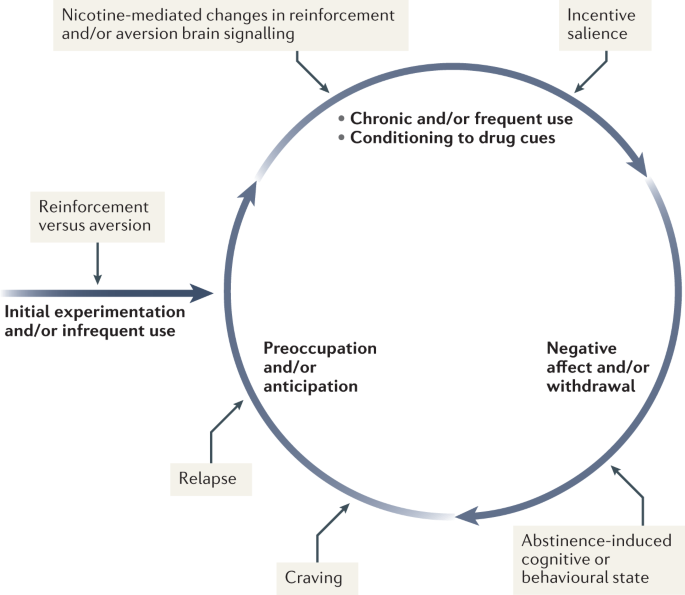
During initial use, nicotine exerts both reinforcing and aversive effects, which together determine the likelihood of continued use. As the individual transitions to more frequent patterns of chronic use, nicotine induces pharmacodynamic changes in brain circuits, which is thought to lead to a reduction in sensitivity to the aversive properties of the drug. Nicotine is also a powerful reinforcer that leads to the conditioning of secondary cues associated with the drug-taking experience (such as cigarette pack, sensory properties of cigarette smoke and feel of the cigarette in the hand or mouth), which serves to enhance the incentive salience of these environmental factors and drive further drug intake. When the individual enters into states of abstinence (such as daily during sleep at night or during quit attempts), withdrawal symptomology is experienced, which may include irritability, restlessness, learning or memory deficits, difficulty concentrating, anxiety and hunger. These negative affective and cognitive symptoms lead to an intensification of the individual’s preoccupation to obtain and use the tobacco/nicotine product, and subsequently such intense craving can lead to relapse.
The rewarding actions of nicotine have largely been attributed to the mesolimbic pathway, which consists of dopaminergic neurons in the ventral tegmental area (VTA) that project to the nucleus accumbens and prefrontal cortex 60 , 61 , 62 (Fig. 5 ). VTA integrating circuits and projection regions express several nAChR subtypes on dopaminergic, GABAergic, and glutamatergic neurons 63 , 64 . Ultimately, administration of nicotine increases dopamine levels through increased dopaminergic neuron firing in striatal and extrastriatal areas (such as the ventral pallidum) 65 (Fig. 6 ). This effect is involved in reward and is believed to be primarily mediated by the action of nicotine on α 4 -containing and β 2 -containing nAChRs in the VTA 66 , 67 .
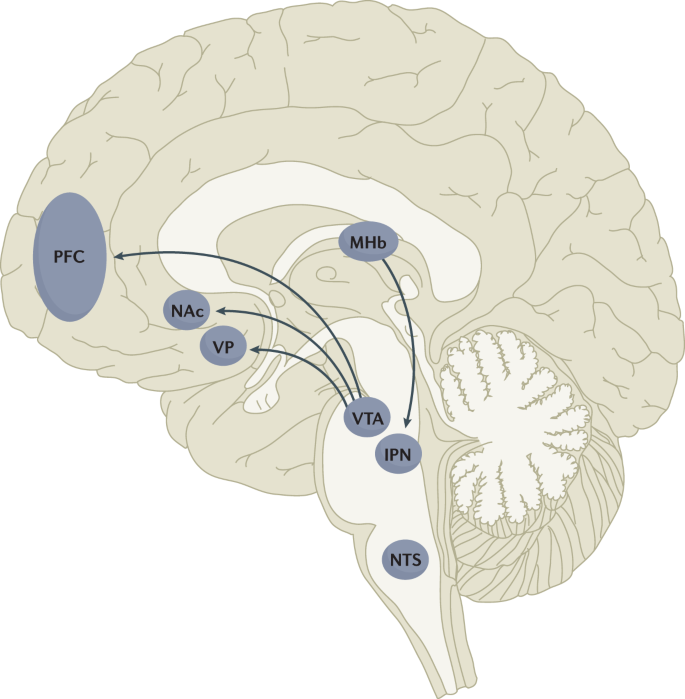
Multiple lines of research have demonstrated that nicotine reinforcement is mainly controlled by two brain pathways, which relay predominantly reward-related or aversion-related signals. The rewarding properties of nicotine that promote drug intake involve the mesolimbic dopamine projection from the ventral tegmental area (VTA) to the nucleus accumbens (NAc). By contrast, the aversive properties of nicotine that limit drug intake and mitigate withdrawal symptoms involve the fasciculus retroflexus projection from the medial habenula (MHb) to the interpeduncular nucleus (IPN). Additional brain regions have also been implicated in various aspects of nicotine dependence, such as the prefrontal cortex (PFC), ventral pallidum (VP), nucleus tractus solitarius (NTS) and insula (not shown here for clarity). All of these brain regions are directly or indirectly interconnected as integrative circuits to drive drug-seeking and drug-taking behaviours.
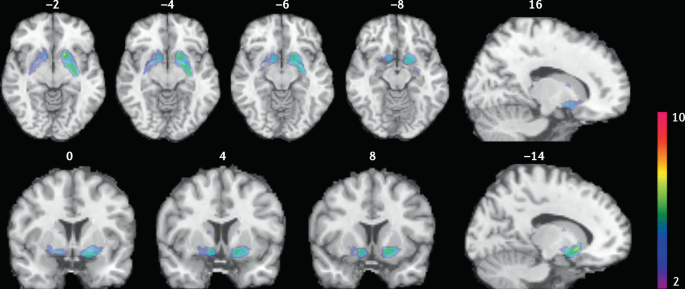
Smokers received brain PET scans with [ 11 C]PHNO, a dopamine D 2/3 PET tracer that has high sensitivity in detecting fluctuations of dopamine. PET scans were performed during abstinence or after smoking a cigarette. Reduced binding potential (BP ND ) was observed after smoking, indicating increased dopamine levels in the ventral striatum and in the area that corresponds to the ventral pallidum. The images show clusters with statistically significant decreases of [ 11 C]PHNO BP ND after smoking a cigarette versus abstinence condition. Those clusters have been superimposed on structural T1 MRI images of the brain. Reprinted from ref. 65 , Springer Nature Limited.
The aversive properties of nicotine are mediated by neurons in the MHb, which project to the IPN. Studies in rodents using genetic knockdown and knockout strategies demonstrated that the α 5 -containing, α 3 -containing and β 4 -containing nAChRs in the MHb–IPN pathway mediate the aversive properties of nicotine that limit drug intake, especially when animals are given the opportunity to consume higher nicotine doses 68 , 69 , 70 , 71 , 72 . In addition to nAChRs, other signalling factors acting on the MHb terminals in the IPN also regulate the actions of nicotine. For instance, under conditions of chronic nicotine exposure or with optogenetic activation of IPN neurons, a subtype of IPN neurons co-expressing Chrna5 (encoding the α 5 nAChR subunit) and Amigo1 (encoding adhesion molecule with immunoglobulin-like domain 1) release nitric oxide from the cell body that retrogradely inhibits MHb axon terminals 70 . In addition, nicotine activates α 5 -containing nAChR-expressing neurons that project from the nucleus tractus solitarius to the IPN, leading to release of glucagon-like peptide-1 that binds to GLP receptors on habenular axon terminals, which subsequently increases IPN neuron activation and decreases nicotine self-administration 73 . Taken together, these findings suggest a dynamic signalling process at MHb axonal terminals in the IPN, which regulates the addictive properties of nicotine and determines the amount of nicotine that is self-administered.
Nicotine withdrawal in animal models can be assessed by examining somatic signs (such as shaking, scratching, head nods and chewing) and affective signs (such as increased anxiety-related behaviours and conditioned place aversion). Interestingly, few nicotine withdrawal somatic signs are found in mice with genetic knockout of the α 2 , α 5 or β 4 nAChR subunits 74 , 75 . By contrast, β 2 nAChR-knockout mice have fewer anxiety-related behaviours during nicotine withdrawal, with no differences in somatic symptoms compared with wild-type mice 74 , 76 .
In addition to the VTA (mediating reward) and the MHb–IPN pathway (mediating aversion), other brain areas are involved in nicotine addiction (Fig. 5 ). In animals, the insular cortex controls nicotine taking and nicotine seeking 77 . Moreover, humans with lesions of the insular cortex can quit smoking easily without relapse 78 . This finding led to the development of a novel therapeutic intervention modulating insula function (see Management, below) 79 , 80 . Various brain areas (shell of nucleus accumbens, basolateral amygdala and prelimbic cortex) expressing cannabinoid CB 1 receptors are also critical in controlling rewarding effects and relapse 81 , 82 . The α 1 -adrenergic receptor expressed in the cortex also control these effects, probably through glutamatergic afferents to the nucleus accumbens 83 .
Individual differences in nicotine addiction risk
Vulnerability to nicotine dependence varies between individuals, and the reasons for these differences are multidimensional. Many social factors (such as education level and income) play a role 84 . Broad psychological and social factors also modulate this risk. For example, peer smoking status, knowledge on effect of tobacco, expectation on social acceptance, exposure to passive smoking modulate the risk of initiating tobacco use 85 , 86 .
Genetic factors have a role in smoking initiation, the development of nicotine addiction and the likelihood of smoking cessation. Indeed, heritability has been estimated to contribute to approximatively half of the variability in nicotine dependence 87 , 88 , 89 , 90 . Important advances in our understanding of such genetic contributions have evolved with large-scale genome-wide association studies of smokers and non-smokers. One of the most striking findings has been that allelic variation in the CHRNA5 – CHRNA3 – CHRNB4 gene cluster, which encodes α 5 , α 3 and β 4 nAChR subunits, correlates with an increased vulnerability for nicotine addiction, indicated by a higher likelihood of becoming dependent on nicotine and smoking a greater number of cigarettes per day 91 , 92 , 93 , 94 , 95 . The most significant effect has been found for a single-nucleotide polymorphism in CHRNA5 (rs16969968), which results in an amino acid change and reduced function of α 5 -containing nAChRs 92 .
Allelic variation in CYP2A6 (encoding the CYP2A6 enzyme, which metabolizes nicotine) has also been associated with differential vulnerability to nicotine dependence 96 , 97 , 98 . CYP2A6 is highly polymorphic, resulting in variable enzymatic activity 96 , 99 , 100 . Individuals with allelic variation that results in slow nicotine metabolism consume less nicotine per day, experience less-severe withdrawal symptoms and are more successful at quitting smoking than individuals with normal or fast metabolism 101 , 102 , 103 , 104 . Moreover, individuals with slow nicotine metabolism have lower dopaminergic receptor expression in the dopamine D2 regions of the associative striatum and sensorimotor striatum in PET studies 105 and take fewer puffs of nicotine-containing cigarettes (compared with de-nicotinized cigarettes) in a forced choice task 106 . Slower nicotine metabolism is thought to increase the duration of action of nicotine, allowing nicotine levels to accumulate over time, therefore enabling lower levels of intake to sustain activation of nAChRs 107 .
Large-scale genetic studies have identified hundreds of other genetic loci that influence smoking initiation, age of smoking initiation, cigarettes smoked per day and successful smoking cessation 108 . The strongest genetic contributions to smoking through the nicotinic receptors and nicotine metabolism are among the strongest genetic contributors to lung cancer 109 . Other genetic variations (such as those related to cannabinoid, dopamine receptors or other neurotransmitters) may affect certain phenotypes related to smoking (such as nicotine preference and cue-reactivity) 110 , 111 , 112 , 113 , 114 , 115 .
Diagnosis, screening and prevention
Screening for cigarette smoking.
Screening for cigarette smoking should happen at every doctor’s visit 116 . In this regard, a simple and direct question about a person’s tobacco use can provide an opportunity to offer information about its potential risks and treatments to assist in quitting. All smokers should be offered assistance in quitting because even low levels of smoking present a significant health risk 33 , 117 , 118 . Smoking status can be assessed by self-categorization or self-reported assessment of smoking behaviour (Table 1 ). In people who smoke, smoking frequency can be assessed 119 and a combined quantity frequency measure such as pack-year history (that is, average number of cigarettes smoked per day multiplied by the number of years, divided by 20), can be used to estimate cumulative risk of adverse health outcomes. The Association for the Treatment of Tobacco Use and Dependence recommends that all electronic health records should document smoking status using the self-report categories listed in Table 1 .
Owing to the advent of e-cigarettes and heat-not-burn products, and the popularity of little cigars in the US that mimic combustible cigarettes, people who use tobacco may use multiple products concurrently 120 , 121 . Thus, screening for other nicotine and tobacco product use is important in clinical practice. The self-categorization approach can also be used to describe the use of these other products.
Traditionally tobacco use has been classified according to whether the smoker meets criteria for nicotine dependence in one of the two main diagnostic classifications: the DSM 122 (tobacco use disorder) and the ICD (tobacco dependence) 123 . The diagnosis of tobacco use disorder according to DSM-5 criteria requires the presence of at least 2 of 11 symptoms that have produced marked clinical impairment or distress within a 12-month period (Box 2 ). Of note, these symptoms are similar for all substance use disorder diagnoses and may not all be relevant to tobacco use disorder (such as failure to complete life roles). In the ICD-10, codes allow the identification of specific tobacco products used (cigarettes, chewing tobacco and other tobacco products).
Dependence can also be assessed as a continuous construct associated with higher levels of use, greater withdrawal and reduced likelihood of quitting. The level of dependence can be assessed with the Fagerström Test for Nicotine Dependence, a short questionnaire comprising six questions 124 (Box 2 ). A score of ≥4 indicates moderate to high dependence. As very limited time may be available in clinical consultations, the Heaviness of Smoking Index (HSI) was developed, which comprises two questions on the number of cigarettes smoked per day and how soon after waking the first cigarette is smoked 125 . The HSI can guide dosing for nicotine replacement therapy (NRT).
Other measures of cigarette dependence have been developed but are not used in the clinical setting, such as the Cigarette Dependence Scale 126 , Hooked on Nicotine Checklist 127 , Nicotine Dependence Syndrome Scale 128 , the Wisconsin Inventory of Smoking Dependence Motives (Brief) 129 and the Penn State Cigarette Dependence Index 130 . However, in practice, these are not often used, as the most important aspect is to screen for smoking and encourage all smokers to quit smoking regardless of their dependence status.
Box 2 DSM-5 criteria for tobacco use disorder and items of the Fagerström Test for nicotine dependence
DSM-5 (ref. 122 )
Taxonomic and diagnostic tool for tobacco use disorder published by the American Psychiatric Association.
A problematic pattern of tobacco use leading to clinically significant impairment or distress as manifested by at least two of the following, occurring within a 12-month period.
Tobacco often used in larger amounts or over a longer period of time than intended
A persistent desire or unsuccessful efforts to reduce or control tobacco use
A great deal of time spent in activities necessary to obtain or use tobacco
Craving, or a strong desire or urge to use tobacco
Recurrent tobacco use resulting in a failure to fulfil major role obligations at work, school or home
Continued tobacco use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of tobacco (for example, arguments with others about tobacco use)
Important social, occupational or recreational activities given up or reduced because of tobacco use
Recurrent tobacco use in hazardous situations (such as smoking in bed)
Tobacco use continued despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by tobacco use
Tolerance, defined by either of the following.
A need for markedly increased amounts of tobacco to achieve the desired effect
A markedly diminished effect with continued use of the same amount of tobacco
Withdrawal, manifesting as either of the following.
Withdrawal syndrome for tobacco
Tobacco (or a closely related substance, such as nicotine) taken to relieve or avoid withdrawal symptoms
Fagerström Test for Nicotine Dependence 124
A standard instrument for assessing the intensity of physical addiction to nicotine.
How soon after you wake up do you smoke your first cigarette?
Within 5 min (scores 3 points)
5 to 30 min (scores 2 points)
31 to 60 min (scores 1 point)
After 60 min (scores 0 points)
Do you find it difficult not to smoke in places where you should not, such as in church or school, in a movie, at the library, on a bus, in court or in a hospital?
Yes (scores 1 point)
No (scores 0 points)
Which cigarette would you most hate to give up; which cigarette do you treasure the most?
The first one in the morning (scores 1 point)
Any other one (scores 0 points)
How many cigarettes do you smoke each day?
10 or fewer (scores 0 points)
11 to 20 (scores 1 point)
21 to 30 (scores 2 points)
31 or more (scores 3 points)
Do you smoke more during the first few hours after waking up than during the rest of the day?
Do you still smoke if you are so sick that you are in bed most of the day or if you have a cold or the flu and have trouble breathing?
A score of 7–10 points is classified as highly dependent; 4–6 points is classified as moderately dependent; <4 points is classified as minimally dependent.
DSM-5, Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition.
Young people who do not start smoking cigarettes between 15 and 25 years of age have a very low risk of ever smoking 24 , 131 , 132 . This age group provides a critical opportunity to prevent cigarette smoking using effective, evidence-based strategies to prevent smoking initiation and reduce escalation from experimentation to regular use 131 , 132 , 133 , 134 , 135 .
Effective prevention of cigarette uptake requires a comprehensive package of cost-effective policies 134 , 136 , 137 to synergistically reduce the population prevalence of cigarette smoking 131 , 135 . These policies include high rates of tobacco taxation 30 , 134 , 137 , 138 , widespread and rigorously enforced smoke-free policies 139 , bans on tobacco advertising and promotions 140 , use of plain packaging and graphic warnings about the health risks of smoking 135 , 141 , mass media and peer-based education programmes to discourage smoking, and enforcement of laws against the sale of cigarettes to young people below the minimum legal purchase age 131 , 135 . These policies make cigarettes less available and affordable to young people. Moreover, these policies make it more difficult for young people to purchase cigarettes and make smoking a much less socially acceptable practice. Of note, these policies are typically mostly enacted in HICs, which may be related to the declining prevalence of smoking in these countries, compared with the prevalence in LMICs.
Pharmacotherapy
Three evidence-based classes of pharmacotherapy are available for smoking cessation: NRT (using nicotine-based patches, gum, lozenges, mini-lozenges, nasal sprays and inhalers), varenicline (a nAChR partial agonist), and bupropion (a noradrenaline/dopamine reuptake inhibitor that also inhibits nAChR function and is also used as an antidepressant). These FDA-approved and EMA-approved pharmacotherapies are cost-effective smoking cessation treatments that double or triple successful abstinence rates compared with no treatment or placebo controls 116 , 142 .
Combinations of pharmacotherapies are also effective for smoking cessation 116 , 142 . For example, combining NRTs (such as the steady-state nicotine patch and as-needed NRT such as gum or mini-lozenge) is more effective than a single form of NRT 116 , 142 , 143 . Combining NRT and varenicline is the most effective smoking cessation pharmacotherapy 116 , 142 , 143 . Combining FDA-approved pharmacotherapy with behavioural counselling further increases the likelihood of successful cessation 142 . Second-line pharmacotherapies (for example, nortriptyline) have some potential for smoking cessation, but their use is limited due to their tolerability profile.
All smokers should receive pharmacotherapy to help them quit smoking, except those in whom pharmacotherapy has insufficient evidence of effectiveness (among adolescents, smokeless tobacco users, pregnant women or light smokers) or those in whom pharmacotherapy is medically contraindicated 144 . Table 2 provides specific information regarding dosing and duration for each FDA-approved pharmacotherapy. Extended use of pharmacotherapy beyond the standard 12-week regimen after cessation is effective and should be considered 116 . Moreover, preloading pharmacotherapy (that is, initiating cessation medication in advance of a quit attempt), especially with the nicotine patch, is a promising treatment, although further studies are required to confirm efficacy.
Cytisine has been used for smoking cessation in Eastern Europe for a long time and is available in some countries (such as Canada) without prescription 145 . Cytisine is a partial agonist of nAChRs and its structure was the precursor for the development of varenicline 145 . Cytisine is at least as effective as some approved pharmacotherapies for smoking cessation, such as NRT 146 , 147 , 148 , and the role of cytisine in smoking cessation is likely to expand in the future, notably owing to its much lower cost than traditional pharmacotherapies. E-cigarettes also have the potential to be useful as smoking cessation devices 149 , 150 . The 2020 US Surgeon General’s Report concluded that there was insufficient evidence to promote cytisine or e-cigarettes as effective smoking cessation treatments, but in the UK its use is recommended for smoking cessation (see ref. 15 for regularly updated review).
Counselling and behavioural treatments
Psychosocial counselling significantly increases the likelihood of successful cessation, especially when combined with pharmacotherapy. Even a counselling session lasting only 3 minutes can help smokers quit 116 , although the 2008 US Public Health Service guidelines and the Preventive Services Task Force 151 each concluded that more intensive counselling (≥20 min per session) is more effective than less intensive counselling (<20 min per session). Higher smoking cessation rates are obtained by using behavioural change techniques that target associative and self-regulatory processes 152 . In addition, behavioural change techniques that will favour commitment, social reward and identity associated with changed behaviour seems associated with higher success rates 152 . Evidence-based counselling focuses on providing social support during treatment, building skills to cope with withdrawal and cessation, and problem-solving in challenging situations 116 , 153 . Effective counselling can be delivered by diverse providers (such as physicians, nurses, pharmacists, social workers, psychologists and certified tobacco treatment specialists) 116 .
Counselling can be delivered in a variety of modalities. In-person individual and group counselling are effective, as is telephone counselling (quit lines) 142 . Internet and text-based intervention seem to be effective in smoking cessation, especially when they are interactive and tailored to a smoker’s specific circumstances 142 . Over the past several years, the number of smoking cessation smartphone apps has increased, but there the evidence that the use of these apps significantly increases smoking cessation rates is not sufficient.
Contingency management (providing financial incentives for abstinence or engagement in treatment) has shown promising results 154 , 155 but its effects are not sustained once the contingencies are removed 155 , 156 . Other treatments such as hypnosis, acupuncture and laser treatment have not been shown to improve smoking cessation rates compared with placebo treatments 116 . Moreover, no solid evidence supports the use of conventional transcranial magnetic stimulation (TMS) for long-term smoking cessation 157 , 158 .
Although a variety of empirically supported smoking cessation interventions are available, more than two-thirds of adult smokers who made quit attempts in the USA during the past year did not use an evidence-based treatment and the rate is likely to be lower in many other countries 142 . This speaks to the need to increase awareness of, and access to, effective cessation aids among all smokers.
Brain stimulation
The insula (part of the frontal cortex) is a critical brain structure involved in cigarette craving and relapse 78 , 79 . The activity of the insula can be modulated using an innovative approach called deep insula/prefrontal cortex TMS (deep TMS), which is effective in helping people quit smoking 80 , 159 . This approach has now been approved by the FDA as an effective smoking cessation intervention 80 . However, although this intervention was developed and is effective for smoking cessation, the number of people with access to it is limited owing to the limited number of sites equipped and with trained personnel, and the cost of this intervention.
Quality of life
Generic instruments (such as the Short-Form (SF-36) Health Survey) can be used to evaluate quality of life (QOL) in smokers. People who smoke rate their QOL lower than people who do not smoke both before and after they become smokers 160 , 161 . QOL improves when smokers quit 162 . Mental health may also improve on quitting smoking 163 . Moreover, QOL is much poorer in smokers with tobacco-related diseases, such as chronic respiratory diseases and cancers, than in individuals without tobacco-related diseases 161 , 164 . The dimensions of QOL that show the largest decrements in people who smoke are those related to physical health, day-to-day activities and mental health such as depression 160 . Smoking also increases the risk of diabetes mellitus 165 , 166 , which is a major determinant of poor QOL for a wide range of conditions.
The high toll of premature death from cigarette smoking can obscure the fact that many of the diseases that cause these deaths also produce substantial disability in the years before death 1 . Indeed, death in smokers is typically preceded by several years of living with the serious disability and impairment of everyday activities caused by chronic respiratory disease, heart disease and cancer 2 . Smokers’ QOL in these years may also be adversely affected by the adverse effects of the medical treatments that they receive for these smoking-related diseases (such as major surgery and radiotherapy).
Expanding cessation worldwide
The major global challenge is to consider individual and population-based strategies that could increase the substantially low rates of adult cessation in most LMICs and indeed strategies to ensure that even in HICs, cessation continues to increase. In general, the most effective tools recommended by WHO to expand cessation are the same tools that can prevent smoking initiation, notably higher tobacco taxes, bans on advertising and promotion, prominent warning labels or plain packaging, bans on public smoking, and mass media and educational efforts 29 , 167 . The effective use of these policies, particularly taxation, lags behind in most LMICs compared with most HICs, with important exceptions such as Brazil 167 . Access to effective pharmacotherapies and counselling as well as support for co-existing mental health conditions would also be required to accelerate cessation in LMICs. This is particularly important as smokers living in LMICs often have no access to the full range of effective treatment options.
Regulating access to e-cigarettes
How e-cigarettes should be used is debated within the tobacco control field. In some countries (for example, the UK), the use of e-cigarettes as a cigarette smoking cessation aid and as a harm reduction strategy is supported, based on the idea that e-cigarette use will lead to much less exposure to toxic compounds than tobacco use, therefore reducing global harm. In other countries (for example, the USA), there is more concern with preventing the increased use of e-cigarettes by youths that may subsequently lead to smoking 25 , 26 . Regulating e-cigarettes in nuanced ways that enable smokers to access those products whilst preventing their uptake among youths is critical.
Regulating nicotine content in tobacco products
Reducing the nicotine content of cigarettes could potentially produce less addictive products that would allow a gradual reduction in the population prevalence of smoking. Some clinical studies have found no compensatory increase in smoking whilst providing access to low nicotine tobacco 168 . Future regulation may be implemented to gradually decrease the nicotine content of combustible tobacco and other nicotine products 169 , 170 , 171 .
Tobacco end games
Some individuals have proposed getting rid of commercial tobacco products this century or using the major economic disruption arising from the COVID-19 pandemic to accelerate the demise of the tobacco industry 172 , 173 . Some tobacco producers have even proposed this strategy as an internal goal, with the idea of switching to nicotine delivery systems that are less harmful ( Philip Morris International ). Some countries are moving towards such an objective; for example, in New Zealand, the goal that fewer than 5% of New Zealanders will be smokers in 2025 has been set (ref. 174 ). The tobacco end-game approach would overall be the best approach to reduce the burden of tobacco use on society, but it would require coordination of multiple countries and strong public and private consensus on the strategy to avoid a major expansion of the existing illicit market in tobacco products in some countries.
Innovative interventions
The COVID-19 pandemic has shown that large-scale investment in research can lead to rapid development of successful therapeutic interventions. By contrast, smoking cessation has been underfunded compared with the contribution that it makes to the global burden of disease. In addition, there is limited coordination between research teams and most studies are small-scale and often underpowered 79 . It is time to fund an ambitious, coordinated programme of research to test the most promising therapies based on an increased understanding of the neurobiological basis of smoking and nicotine addiction (Table 3 ). Many of those ideas have not yet been tested properly and this could be carried out by a coordinated programme of research at the international level.
GBD 2019 Tobacco Collaborators. Spatial, temporal, and demographic patterns in prevalence of smoking tobacco use and attributable disease burden in 204 countries and territories, 1990-2019: a systematic analysis from the Global Burden of Disease Study 2019. Lancet 397 , 2337–2360 (2021). This study summarizes the burden of disease induced by tobacco worldwide .
Google Scholar
West, R. Tobacco smoking: health impact, prevalence, correlates and interventions. Psychol. Health 32 , 1018–1036 (2017).
PubMed PubMed Central Google Scholar
West, R. The multiple facets of cigarette addiction and what they mean for encouraging and helping smokers to stop. COPD 6 , 277–283 (2009).
PubMed Google Scholar
Fagerström, K. Determinants of tobacco use and renaming the FTND to the Fagerström test for cigarette dependence. Nicotine Tob. Res. 14 , 75–78 (2012).
National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. The Health Consequences of Smoking: 50 Years of Progress. A Report of the Surgeon General (Centers for Disease Control and Prevention, 2014).
Doll, R. & Hill, A. B. Smoking and carcinoma of the lung; preliminary report. Br. Med. J. 2 , 739–748 (1950).
CAS PubMed PubMed Central Google Scholar
Royal College of Physicians. Smoking and health. Summary of a report of the Royal College of Physicians of London on smoking in relation to cancer of the lung and other diseases (Pitman Medical Publishing, 1962).
Henningfield, J. E., Smith, T. T., Kleykamp, B. A., Fant, R. V. & Donny, E. C. Nicotine self-administration research: the legacy of Steven R. Goldberg and implications for regulation, health policy, and research. Psychopharmacology 233 , 3829–3848 (2016).
Le Foll, B. & Goldberg, S. R. Effects of nicotine in experimental animals and humans: an update on addictive properties. Hand. Exp. Pharmacol. https://doi.org/10.1007/978-3-540-69248-5_12 (2009).
Article Google Scholar
Proctor, R. N. The history of the discovery of the cigarette–lung cancer link: evidentiary traditions, corporate denial, global toll. Tob. Control. 21 , 87–91 (2012).
Hall, B. J. et al. Differential effects of non-nicotine tobacco constituent compounds on nicotine self-administration in rats. Pharmacol. Biochem. Behav. 120 , 103–108 (2014).
Musso, F. et al. Smoking impacts on prefrontal attentional network function in young adult brains. Psychopharmacology 191 , 159–169 (2007).
CAS PubMed Google Scholar
Goriounova, N. A. & Mansvelder, H. D. Short- and long-term consequences of nicotine exposure during adolescence for prefrontal cortex neuronal network function. Cold Spring Harb. Perspect. Med. 2 , a012120 (2012).
Fagerström, K. O. & Bridgman, K. Tobacco harm reduction: the need for new products that can compete with cigarettes. Addictive Behav. 39 , 507–511 (2014).
Hartmann-Boyce, J. et al. Electronic cigarettes for smoking cessation. Cochrane Database Syst. Rev. 9 , CD010216 (2021).
Jha, P. The hazards of smoking and the benefits of cessation: a critical summation of the epidemiological evidence in high-income countries. eLife https://doi.org/10.7554/eLife.49979 (2020).
Article PubMed PubMed Central Google Scholar
Palipudi, K. M. et al. Social determinants of health and tobacco use in thirteen low and middle income countries: evidence from Global Adult Tobacco Survey. PLoS ONE 7 , e33466 (2012).
Goodwin, R. D., Pagura, J., Spiwak, R., Lemeshow, A. R. & Sareen, J. Predictors of persistent nicotine dependence among adults in the United States. Drug Alcohol. Depend. 118 , 127–133 (2011).
Weinberger, A. H. et al. Cigarette use is increasing among people with illicit substance use disorders in the United States, 2002-14: emerging disparities in vulnerable populations. Addiction 113 , 719–728 (2018).
Evans-Polce, R. J., Kcomt, L., Veliz, P. T., Boyd, C. J. & McCabe, S. E. Alcohol, tobacco, and comorbid psychiatric disorders and associations with sexual identity and stress-related correlates. Am. J. Psychiatry 177 , 1073–1081 (2020).
Hassan, A. N. & Le Foll, B. Survival probabilities and predictors of major depressive episode incidence among individuals with various types of substance use disorders. J. Clin. Psychiatry https://doi.org/10.4088/JCP.20m13637 (2021).
Article PubMed Google Scholar
Smith, P. H., Mazure, C. M. & McKee, S. A. Smoking and mental illness in the U.S. population. Tob. Control. 23 , e147–e153 (2014).
Bourgault, Z., Rubin-Kahana, D. S., Hassan, A. N., Sanches, M. & Le Foll, B. Multiple substance use disorders and self-reported cognitive function in U.S. adults: associations and sex-differences in a nationally representative sample. Front. Psychiatry https://doi.org/10.3389/fpsyt.2021.797578 (2022).
Reitsma, M. B. et al. Spatial, temporal, and demographic patterns in prevalence of smoking tobacco use and initiation among young people in 204 countries and territories, 1990-2019. Lancet Public Health 6 , e472–e481 (2021).
Warner, K. E. How to think–not feel–about tobacco harm reduction. Nicotine Tob. Res. 21 , 1299–1309 (2019).
Soneji, S. et al. Association between initial use of e-cigarettes and subsequent cigarette smoking among adolescents and young adults: a systematic review and meta-analysis. JAMA Pediatr. 171 , 788–797 (2017).
Levy, D. T. et al. Examining the relationship of vaping to smoking initiation among US youth and young adults: a reality check. Tob. Control. 28 , 629–635 (2019).
National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. The health consequences of smoking — 50 years of progress: a report of the Surgeon General (Centers for Disease Control and Prevention, 2014).
Jha, P. & Peto, R. Global effects of smoking, of quitting, and of taxing tobacco. N. Engl. J. Med. 370 , 60–68 (2014). This review covers the impact of tobacco, of quitting smoking and the importance of taxation to impact prevalence of smoking .
Jha, P. & Peto., R. in Tobacco Tax Reform: At the Crossroads of Health and Development . (eds Marquez, P. V. & Moreno-Dodson, B.) 55–72 (World Bank Group, 2017).
Jha, P. et al. 21st-century hazards of smoking and benefits of cessation in the United States. N. Engl. J. Med. 368 , 341–350 (2013).
Banks, E. et al. Tobacco smoking and all-cause mortality in a large Australian cohort study: findings from a mature epidemic with current low smoking prevalence. BMC Med. 13 , 38 (2015).
Pirie, K. et al. The 21st century hazards of smoking and benefits of stopping: a prospective study of one million women in the UK. Lancet 381 , 133–141 (2013).
Jha, P. et al. A nationally representative case-control study of smoking and death in India. N. Engl. J. Med. 358 , 1137–1147 (2008).
Chan, E. D. et al. Tobacco exposure and susceptibility to tuberculosis: is there a smoking gun? Tuberculosis 94 , 544–550 (2014).
Wang, M. G. et al. Association between tobacco smoking and drug-resistant tuberculosis. Infect. Drug Resist. 11 , 873–887 (2018).
Jha, P. et al. Social inequalities in male mortality, and in male mortality from smoking: indirect estimation from national death rates in England and Wales, Poland, and North America. Lancet 368 , 367–370 (2006).
Jha, P., Gelband, H, Irving, H. & Mishra, S. in Reducing Social Inequalities in Cancer: Evidence and Priorities for Research (eds Vaccarella, S et al.) 161–166 (IARC, 2018).
Jha, P. Expanding smoking cessation world-wide. Addiction 113 , 1392–1393 (2018).
Jha, P. Avoidable global cancer deaths and total deaths from smoking. Nat. Rev. Cancer 9 , 655–664 (2009).
Wittenberg, R. E., Wolfman, S. L., De Biasi, M. & Dani, J. A. Nicotinic acetylcholine receptors and nicotine addiction: a brief introduction. Neuropharmacology 177 , 108256 (2020).
Boulter, J. et al. Functional expression of two neuronal nicotinic acetylcholine receptors from cDNA clones identifies a gene family. Proc. Natl Acad. Sci. USA 84 , 7763–7767 (1987).
Couturier, S. et al. A neuronal nicotinic acetylcholine receptor subunit (α7) is developmentally regulated and forms a homo-oligomeric channel blocked by α-BTX. Neuron 5 , 847–856 (1990).
Picciotto, M. R., Addy, N. A., Mineur, Y. S. & Brunzell, D. H. It is not “either/or”: activation and desensitization of nicotinic acetylcholine receptors both contribute to behaviors related to nicotine addiction and mood. Prog. Neurobiol. 84 , 329–342 (2008).
Changeux, J. P. Structural identification of the nicotinic receptor ion channel. Trends Neurosci. 41 , 67–70 (2018).
McKay, B. E., Placzek, A. N. & Dani, J. A. Regulation of synaptic transmission and plasticity by neuronal nicotinic acetylcholine receptors. Biochem. Pharmacol. 74 , 1120–1133 (2007).
Wonnacott, S. Presynaptic nicotinic ACh receptors. Trends Neurosci. 20 , 92–98 (1997).
Wooltorton, J. R., Pidoplichko, V. I., Broide, R. S. & Dani, J. A. Differential desensitization and distribution of nicotinic acetylcholine receptor subtypes in midbrain dopamine areas. J. Neurosci. 23 , 3176–3185 (2003).
Gipson, C. D. & Fowler, C. D. Nicotinic receptors underlying nicotine dependence: evidence from transgenic mouse models. Curr. Top. Behav. Neurosci. 45 , 101–121 (2020).
Hamouda, A. K. et al. Potentiation of (α4)2(β2)3, but not (α4)3(β2)2, nicotinic acetylcholine receptors reduces nicotine self-administration and withdrawal symptoms. Neuropharmacology 190 , 108568 (2021).
Lallai, V. et al. Nicotine acts on cholinergic signaling mechanisms to directly modulate choroid plexus function. eNeuro https://doi.org/10.1523/ENEURO.0051-19.2019 (2019).
Benwell, M. E., Balfour, D. J. & Anderson, J. M. Evidence that tobacco smoking increases the density of (-)-[3H]nicotine binding sites in human brain. J. Neurochem. 50 , 1243–1247 (1988).
Perry, D. C., Davila-Garcia, M. I., Stockmeier, C. A. & Kellar, K. J. Increased nicotinic receptors in brains from smokers: membrane binding and autoradiography studies. J. Pharmacol. Exp. Ther. 289 , 1545–1552 (1999).
Marks, M. J. et al. Nicotine binding and nicotinic receptor subunit RNA after chronic nicotine treatment. J. Neurosci. 12 , 2765–2784 (1992).
Le Foll, B. et al. Impact of short access nicotine self-administration on expression of α4β2* nicotinic acetylcholine receptors in non-human primates. Psychopharmacology 233 , 1829–1835 (2016).
Meyers, E. E., Loetz, E. C. & Marks, M. J. Differential expression of the beta4 neuronal nicotinic receptor subunit affects tolerance development and nicotinic binding sites following chronic nicotine treatment. Pharmacol. Biochem. Behav. 130 , 1–8 (2015).
Zhao-Shea, R., Liu, L., Pang, X., Gardner, P. D. & Tapper, A. R. Activation of GABAergic neurons in the interpeduncular nucleus triggers physical nicotine withdrawal symptoms. Curr. Biol. 23 , 2327–2335 (2013).
Jensen, K. P., Valentine, G., Gueorguieva, R. & Sofuoglu, M. Differential effects of nicotine delivery rate on subjective drug effects, urges to smoke, heart rate and blood pressure in tobacco smokers. Psychopharmacology 237 , 1359–1369 (2020).
Villanueva, H. F., James, J. R. & Rosecrans, J. A. Evidence of pharmacological tolerance to nicotine. NIDA Res. Monogr. 95 , 349–350 (1989).
Corrigall, W. A., Coen, K. M. & Adamson, K. L. Self-administered nicotine activates the mesolimbic dopamine system through the ventral tegmental area. Brain Res. 653 , 278–284 (1994).
Nisell, M., Nomikos, G. G., Hertel, P., Panagis, G. & Svensson, T. H. Condition-independent sensitization of locomotor stimulation and mesocortical dopamine release following chronic nicotine treatment in the rat. Synapse 22 , 369–381 (1996).
Rice, M. E. & Cragg, S. J. Nicotine amplifies reward-related dopamine signals in striatum. Nat. Neurosci. 7 , 583–584 (2004).
Mameli-Engvall, M. et al. Hierarchical control of dopamine neuron-firing patterns by nicotinic receptors. Neuron 50 , 911–921 (2006).
Picciotto, M. R., Higley, M. J. & Mineur, Y. S. Acetylcholine as a neuromodulator: cholinergic signaling shapes nervous system function and behavior. Neuron 76 , 116–129 (2012).
Le Foll, B. et al. Elevation of dopamine induced by cigarette smoking: novel insights from a [11C]-+-PHNO PET study in humans. Neuropsychopharmacology 39 , 415–424 (2014). This brain imaging study identified the brain areas in which smoking elevates dopamine levels .
Maskos, U. et al. Nicotine reinforcement and cognition restored by targeted expression of nicotinic receptors. Nature 436 , 103–107 (2005). This article discusses the implication of the β 2 - containing nAChRs in the VTA in mammalian cognitive function .
Picciotto, M. R. et al. Acetylcholine receptors containing the beta2 subunit are involved in the reinforcing properties of nicotine. Nature 391 , 173–177 (1998). This article discusses the implication of the β 2 - containing nAChRs in addictive effects of nicotine .
Fowler, C. D., Lu, Q., Johnson, P. M., Marks, M. J. & Kenny, P. J. Habenular alpha5 nicotinic receptor subunit signalling controls nicotine intake. Nature 471 , 597–601 (2011). This article discusses the implication of the α5 nicotinic receptor located in the MHb in a mechanism mediating the aversive effects of nicotine .
Elayouby, K. S. et al. α3* Nicotinic acetylcholine receptors in the habenula-interpeduncular nucleus circuit regulate nicotine intake. J. Neurosci. https://doi.org/10.1523/JNEUROSCI.0127-19.2020 (2020).
Ables, J. L. et al. Retrograde inhibition by a specific subset of interpeduncular α5 nicotinic neurons regulates nicotine preference. Proc. Natl Acad. Sci. USA 114 , 13012–13017 (2017).
Frahm, S. et al. Aversion to nicotine is regulated by the balanced activity of β4 and α5 nicotinic receptor subunits in the medial habenula. Neuron 70 , 522–535 (2011).
Jackson, K. J. et al. Role of α5 nicotinic acetylcholine receptors in pharmacological and behavioral effects of nicotine in mice. J. Pharmacol. Exp. Ther. 334 , 137–146 (2010).
Tuesta, L. M. et al. GLP-1 acts on habenular avoidance circuits to control nicotine intake. Nat. Neurosci. 20 , 708–716 (2017).
Salas, R., Pieri, F. & De Biasi, M. Decreased signs of nicotine withdrawal in mice null for the β4 nicotinic acetylcholine receptor subunit. J. Neurosci. 24 , 10035–10039 (2004).
Salas, R., Sturm, R., Boulter, J. & De Biasi, M. Nicotinic receptors in the habenulo-interpeduncular system are necessary for nicotine withdrawal in mice. J. Neurosci. 29 , 3014–3018 (2009).
Jackson, K. J., Martin, B. R., Changeux, J. P. & Damaj, M. I. Differential role of nicotinic acetylcholine receptor subunits in physical and affective nicotine withdrawal signs. J. Pharmacol. Exp. Ther. 325 , 302–312 (2008).
Le Foll, B. et al. Translational strategies for therapeutic development in nicotine addiction: rethinking the conventional bench to bedside approach. Prog. Neuropsychopharmacol. Biol. Psychiatry 52 , 86–93 (2014).
Naqvi, N. H., Rudrauf, D., Damasio, H. & Bechara, A. Damage to the insula disrupts addiction to cigarette smoking. Science 315 , 531–534 (2007). This article discusses the implication of the insular cortex in tobacco addiction .
Ibrahim, C. et al. The insula: a brain stimulation target for the treatment of addiction. Front. Pharmacol. 10 , 720 (2019).
Zangen, A. et al. Repetitive transcranial magnetic stimulation for smoking cessation: a pivotal multicenter double-blind randomized controlled trial. World Psychiatry 20 , 397–404 (2021). This study validated the utility of deep insula/prefrontal cortex rTMS for smoking cessation .
Le Foll, B., Forget, B., Aubin, H. J. & Goldberg, S. R. Blocking cannabinoid CB1 receptors for the treatment of nicotine dependence: insights from pre-clinical and clinical studies. Addict. Biol. 13 , 239–252 (2008).
Kodas, E., Cohen, C., Louis, C. & Griebel, G. Cortico-limbic circuitry for conditioned nicotine-seeking behavior in rats involves endocannabinoid signaling. Psychopharmacology 194 , 161–171 (2007).
Forget, B. et al. Noradrenergic α1 receptors as a novel target for the treatment of nicotine addiction. Neuropsychopharmacology 35 , 1751–1760 (2010).
Garrett, B. E., Dube, S. R., Babb, S. & McAfee, T. Addressing the social determinants of health to reduce tobacco-related disparities. Nicotine Tob. Res. 17 , 892–897 (2015).
Polanska, K., Znyk, M. & Kaleta, D. Susceptibility to tobacco use and associated factors among youth in five central and eastern European countries. BMC Public Health 22 , 72 (2022).
Volkow, N. D. Personalizing the treatment of substance use disorders. Am. J. Psychiatry 177 , 113–116 (2020).
Li, M. D., Cheng, R., Ma, J. Z. & Swan, G. E. A meta-analysis of estimated genetic and environmental effects on smoking behavior in male and female adult twins. Addiction 98 , 23–31 (2003).
Carmelli, D., Swan, G. E., Robinette, D. & Fabsitz, R. Genetic influence on smoking–a study of male twins. N. Engl. J. Med. 327 , 829–833 (1992).
Broms, U., Silventoinen, K., Madden, P. A. F., Heath, A. C. & Kaprio, J. Genetic architecture of smoking behavior: a study of Finnish adult twins. Twin Res. Hum. Genet. 9 , 64–72 (2006).
Kendler, K. S., Thornton, L. M. & Pedersen, N. L. Tobacco consumption in Swedish twins reared apart and reared together. Arch. Gen. Psychiat 57 , 886–892 (2000).
Saccone, N. L. et al. The CHRNA5-CHRNA3-CHRNB4 nicotinic receptor subunit gene cluster affects risk for nicotine dependence in African-Americans and in European-Americans. Cancer Res. 69 , 6848–6856 (2009).
Bierut, L. J. et al. Variants in nicotinic receptors and risk for nicotine dependence. Am. J. Psychiatry 165 , 1163–1171 (2008). This study demonstrates that nAChR gene variants are important in nicotine addiction .
Bierut, L. J. et al. Novel genes identified in a high-density genome wide association study for nicotine dependence. Hum. Mol. Genet. 16 , 24–35 (2007).
Berrettini, W. et al. α-5/α-3 nicotinic receptor subunit alleles increase risk for heavy smoking. Mol. Psychiatry 13 , 368–373 (2008).
Sherva, R. et al. Association of a single nucleotide polymorphism in neuronal acetylcholine receptor subunit alpha 5 (CHRNA5) with smoking status and with ‘pleasurable buzz’ during early experimentation with smoking. Addiction 103 , 1544–1552 (2008).
Thorgeirsson, T. E. et al. Sequence variants at CHRNB3-CHRNA6 and CYP2A6 affect smoking behavior. Nat. Genet. 42 , 448–453 (2010).
Ray, R., Tyndale, R. F. & Lerman, C. Nicotine dependence pharmacogenetics: role of genetic variation in nicotine-metabolizing enzymes. J. Neurogenet. 23 , 252–261 (2009).
Bergen, A. W. et al. Drug metabolizing enzyme and transporter gene variation, nicotine metabolism, prospective abstinence, and cigarette consumption. PLoS ONE 10 , e0126113 (2015).
Mwenifumbo, J. C. et al. Identification of novel CYP2A6*1B variants: the CYP2A6*1B allele is associated with faster in vivo nicotine metabolism. Clin. Pharmacol. Ther. 83 , 115–121 (2008).
Raunio, H. & Rahnasto-Rilla, M. CYP2A6: genetics, structure, regulation, and function. Drug Metab. Drug Interact. 27 , 73–88 (2012).
CAS Google Scholar
Patterson, F. et al. Toward personalized therapy for smoking cessation: a randomized placebo-controlled trial of bupropion. Clin. Pharmacol. Ther. 84 , 320–325 (2008).
Rodriguez, S. et al. Combined analysis of CHRNA5, CHRNA3 and CYP2A6 in relation to adolescent smoking behaviour. J. Psychopharmacol. 25 , 915–923 (2011).
Strasser, A. A., Malaiyandi, V., Hoffmann, E., Tyndale, R. F. & Lerman, C. An association of CYP2A6 genotype and smoking topography. Nicotine Tob. Res. 9 , 511–518 (2007).
Liakoni, E. et al. Effects of nicotine metabolic rate on withdrawal symptoms and response to cigarette smoking after abstinence. Clin. Pharmacol. Ther. 105 , 641–651 (2019).
Di Ciano, P. et al. Influence of nicotine metabolism ratio on [11C]-(+)-PHNO PET binding in tobacco smokers. Int. J. Neuropsychopharmacol. 21 , 503–512 (2018).
Butler, K. et al. Impact of Cyp2a6 activity on nicotine reinforcement and cue-reactivity in daily smokers. Nicotine Tob. Res. https://doi.org/10.1093/ntr/ntab064 (2021).
Benowitz, N. L., Swan, G. E., Jacob, P. 3rd, Lessov-Schlaggar, C. N. & Tyndale, R. F. CYP2A6 genotype and the metabolism and disposition kinetics of nicotine. Clin. Pharmacol. Ther. 80 , 457–467 (2006).
Liu, M. et al. Association studies of up to 1.2 million individuals yield new insights into the genetic etiology of tobacco and alcohol use. Nat. Genet. 51 , 237–244 (2019).
McKay, J. D. et al. Large-scale association analysis identifies new lung cancer susceptibility loci and heterogeneity in genetic susceptibility across histological subtypes. Nat. Genet. 49 , 1126–1132 (2017).
Chukwueke, C. C. et al. The CB1R rs2023239 receptor gene variant significantly affects the reinforcing effects of nicotine, but not cue reactivity, in human smokers. Brain Behav. 11 , e01982 (2021).
Ahrens, S. et al. Modulation of nicotine effects on selective attention by DRD2 and CHRNA4 gene polymorphisms. Psychopharmacology 232 , 2323–2331 (2015).
Harrell, P. T. et al. Dopaminergic genetic variation moderates the effect of nicotine on cigarette reward. Psychopharmacology 233 , 351–360 (2016).
Lerman, C. et al. Role of functional genetic variation in the dopamine D2 receptor (DRD2) in response to bupropion and nicotine replacement therapy for tobacco dependence: results of two randomized clinical trials. Neuropsychopharmacology 31 , 231–242 (2006).
Le Foll, B., Gallo, A., Le Strat, Y., Lu, L. & Gorwood, P. Genetics of dopamine receptors and drug addiction: a comprehensive review. Behav. Pharmacol. 20 , 1–17 (2009).
Chukwueke, C. C. et al. Exploring the role of the Ser9Gly (rs6280) dopamine D3 receptor polymorphism in nicotine reinforcement and cue-elicited craving. Sci. Rep. 10 , 4085 (2020).
The Clinical Practice Guideline Treating Tobacco Use and Dependence 2008 Update Panel, Liaisons, and Staff A clinical practice guideline for treating tobacco use and dependence: 2008 update: a U.S. Public Health Service report. Am. J. Prev. Med. 35 , 158–176 (2008).
Hackshaw, A., Morris, J. K., Boniface, S., Tang, J. L. & Milenković, D. Low cigarette consumption and risk of coronary heart disease and stroke: meta-analysis of 141 cohort studies in 55 study reports. BMJ 360 , j5855 (2018).
Qin, W. et al. Light cigarette smoking increases risk of all-cause and cause-specific mortality: findings from the NHIS cohort study. Int. J. Env. Res. Public Health https://doi.org/10.3390/ijerph17145122 (2020).
Rodu, B. & Plurphanswat, N. Mortality among male smokers and smokeless tobacco users in the USA. Harm Reduct. J. 16 , 50 (2019).
Kasza, K. A. et al. Tobacco-product use by adults and youths in the United States in 2013 and 2014. N. Engl. J. Med. 376 , 342–353 (2017).
Richardson, A., Xiao, H. & Vallone, D. M. Primary and dual users of cigars and cigarettes: profiles, tobacco use patterns and relevance to policy. Nicotine Tob. Res. 14 , 927–932 (2012).
American Psychiatric Association. Diagnostic and Statistical Manual of Mental disorders 5th edn (American Psychiatric Association, 2013).
World Health Organization. Tobacco fact sheet. WHO https://www.who.int/news-room/fact-sheets/detail/tobacco (2021).
Heatherton, T. F., Kozlowski, L. T., Frecker, R. C. & Fagerström, K. O. The Fagerström test for nicotine dependence: a revision of the Fagerström tolerance questionnaire. Br. J. Addict. 86 , 1119–1127 (1991).
Heatherton, T. F., Kozlowski, L. T., Frecker, R. C., Rickert, W. & Robinson, J. Measuring the heaviness of smoking: using self-reported time to the first cigarette of the day and number of cigarettes smoked per day. Br. J. Addict. 84 , 791–799 (1989).
Etter, J. F., Le Houezec, J. & Perneger, T. V. A self-administered questionnaire to measure dependence on cigarettes: the cigarette dependence scale. Neuropsychopharmacology 28 , 359–370 (2003).
DiFranza, J. R. et al. Measuring the loss of autonomy over nicotine use in adolescents: the DANDY (Development and Assessment of Nicotine Dependence in Youths) study. Arch. Pediatr. Adolesc. Med. 156 , 397–403 (2002).
Shiffman, S., Waters, A. & Hickcox, M. The Nicotine Dependence Syndrome Scale: a multidimensional measure of nicotine dependence. Nicotine Tob. Res. 6 , 327–348 (2004).
Smith, S. S. et al. Development of the Brief Wisconsin Inventory of Smoking Dependence Motives. Nicotine Tob. Res. 12 , 489–499 (2010).
Foulds, J. et al. Development of a questionnaire for assessing dependence on electronic cigarettes among a large sample of ex-smoking E-cigarette users. Nicotine Tob. Res. 17 , 186–192 (2015).
National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. Preventing tobacco use among youth and young adults: a report of the Surgeon General (Centers for Disease Control and Prevention, 2012).
World Health Organization. Tobacco control to improve child health and development. Thematic brief (WHO, 2021).
Lantz, P. M. et al. Investing in youth tobacco control: a review of smoking prevention and control strategies. Tob. Control. 9 , 47–63 (2000).
Leão, T., Kunst, A. E. & Perelman, J. Cost-effectiveness of tobacco control policies and programmes targeting adolescents: a systematic review. Eur. J. Public Health 28 , 39–43 (2018).
Royal College of Physicians. Smoking and health 2021: a coming of age for tobacco control? (RCP, 2021).
Higashi, H. et al. Cost effectiveness of tobacco control policies in Vietnam: the case of population-level interventions. Appl. Health Econ. Health Policy 9 , 183–196 (2011).
Ranson, M. K., Jha, P., Chaloupka, F. J. & Nguyen, S. N. Global and regional estimates of the effectiveness and cost-effectiveness of price increases and other tobacco control policies. Nicotine Tob. Res. 4 , 311–319 (2002).
International Agency for Research on Cancer. I ARC Handbooks of Cancer Prevention: Tobacco control Vol. 14 (IARC, 2011).
Frazer, K. et al. Legislative smoking bans for reducing harms from secondhand smoke exposure, smoking prevalence and tobacco consumption. Cochrane Database Syst. Rev. 2 , CD005992 (2016).
Hoffman, S. J. & Tan, C. Overview of systematic reviews on the health-related effects of government tobacco control policies. BMC Public Health 15 , 744 (2015).
McNeill, A. et al. Tobacco packaging design for reducing tobacco use. Cochrane Database Syst. Rev. 4 , CD011244 (2017).
National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. Smoking cessation: a report of the Surgeon General (Department of Health and Human Services, 2020).
Lindson, N. et al. Different doses, durations and modes of delivery of nicotine replacement therapy for smoking cessation. Cochrane Database Syst. Rev. 4 , CD013308 (2019).
Krist, A. H. et al. Interventions for tobacco smoking cessation in adults, including pregnant persons: US Preventive Services Task Force recommendation statement. JAMA 325 , 265–279 (2021).
Tutka, P. & Zatonski, W. Cytisine for the treatment of nicotine addiction: from a molecule to therapeutic efficacy. Pharmacol. Rep. 58 , 777–798 (2006).
Courtney, R. J. et al. Effect of cytisine vs varenicline on smoking cessation: a randomized clinical trial. JAMA 326 , 56–64 (2021).
Walker, N. et al. Cytisine versus nicotine for smoking cessation. N. Engl. J. Med. 371 , 2353–2362 (2014). This study validated the utility of cytisine for smoking cessation .
West, R. et al. Placebo-controlled trial of cytisine for smoking cessation. N. Engl. J. Med. 365 , 1193–1200 (2011).
Hajek, P. et al. E-cigarettes compared with nicotine replacement therapy within the UK Stop Smoking Services: the TEC RCT. Health Technol. Assess. 23 , 1–82 (2019).
Walker, N. et al. Nicotine patches used in combination with e-cigarettes (with and without nicotine) for smoking cessation: a pragmatic, randomised trial. Lancet Respir. Med. 8 , 54–64 (2020).
Siu, A. L., U.S. Preventive Services Task Force. Behavioral and pharmacotherapy interventions for tobacco smoking cessation in adults, including pregnant women: U.S. Preventive Services Task Force recommendation statement. Ann. Intern. Med. 163 , 622–634 (2015).
Black, N. et al. Behaviour change techniques associated with smoking cessation in intervention and comparator groups of randomized controlled trials: a systematic review and meta-regression. Addiction 115 , 2008–2020 (2020).
Center for Substance Abuse and Treatment. Detoxification and Substance Abuse Treatment (Center for Substance Abuse and Treatment, 2006).
Cahill, K., Hartmann-Boyce, J. & Perera, R. Incentives for smoking cessation. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD004307.pub5 (2015).
Secades-Villa, R., Aonso-Diego, G., García-Pérez, Á. & González-Roz, A. Effectiveness of contingency management for smoking cessation in substance users: a systematic review and meta-analysis. J. Consult. Clin. Psychol. 88 , 951–964 (2020).
Cahill, K. & Perera, R. Competitions and incentives for smoking cessation. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD004307.pub4 (2011).
Trojak, B. et al. Transcranial magnetic stimulation combined with nicotine replacement therapy for smoking cessation: a randomized controlled trial. Brain Stimul. 8 , 1168–1174 (2015).
Wing, V. C. et al. Brain stimulation methods to treat tobacco addiction. Brain Stimul. 6 , 221–230 (2013).
Dinur-Klein, L. et al. Smoking cessation induced by deep repetitive transcranial magnetic stimulation of the prefrontal and insular cortices: a prospective, randomized controlled trial. Biol. Psychiatry 76 , 742–749 (2014).
Goldenberg, M., Danovitch, I. & IsHak, W. W. Quality of life and smoking. Am. J. Addict. 23 , 540–562 (2014).
Heikkinen, H., Jallinoja, P., Saarni, S. I. & Patja, K. The impact of smoking on health-related and overall quality of life: a general population survey in Finland. Nicotine Tob. Res. 10 , 1199–1207 (2008).
Moayeri, F., Hsueh, Y. A., Dunt, D. & Clarke, P. Smoking cessation and quality of life: insights from analysis of longitudinal Australian data, an application for economic evaluations. Value Health 24 , 724–732 (2021).
Taylor, G. M. et al. Smoking cessation for improving mental health. Cochrane Database Syst. Rev. 3 , CD013522 (2021).
López-Nicolás, Á., Trapero-Bertran, M. & Muñoz, C. Smoking, health-related quality of life and economic evaluation. Eur. J. Health Econ. 19 , 747–756 (2018).
Morris, A. Linking nicotine addiction and T2DM. Nat. Rev. Endocrinol. 16 , 6 (2020).
Willi, C., Bodenmann, P., Ghali, W. A., Faris, P. D. & Cornuz, J. Active smoking and the risk of type 2 diabetes: a systematic review and meta-analysis. Jama 298 , 2654–2664 (2007).
World Health Organization. WHO report on the global tobacco epidemic (WHO, 2019).
Donny, E. C. et al. Randomized trial of reduced-nicotine standards for cigarettes. N. Engl. J. Med. 373 , 1340–1349 (2015). This study tested the impact of reducing the quantity of nicotine present in cigarettes on smoking .
Benowitz, N. L. & Henningfield, J. E. Establishing a nicotine threshold for addiction. The implications for tobacco regulation. N. Engl. J. Med. 331 , 123–125 (1994).
Benowitz, N. L. & Henningfield, J. E. Reducing the nicotine content to make cigarettes less addictive. Tob. Control. 22 , i14–i17 (2013).
Gottlieb, S. & Zeller, M. A nicotine-focused framework for public health. N. Engl. J. Med. 377 , 1111–1114 (2017).
Hall, W. & West, R. Thinking about the unthinkable: a de facto prohibition on smoked tobacco products. Addiction 103 , 873–874 (2008).
Ioannidis, J. P. A. & Jha, P. Does the COVID-19 pandemic provide an opportunity to eliminate the tobacco industry? Lancet Glob. Health 9 , e12–e13 (2021).
Smokefree. Smokefree 2025. Smokefree https://www.smokefree.org.nz/smokefree-in-action/smokefree-aotearoa-2025 (2021).
Morgan, C. J., Das, R. K., Joye, A., Curran, H. V. & Kamboj, S. K. Cannabidiol reduces cigarette consumption in tobacco smokers: preliminary findings. Addict. Behav. 38 , 2433–2436 (2013).
Elsaid, S., Kloiber, S. & Le Foll, B. Effects of cannabidiol (CBD) in neuropsychiatric disorders: a review of pre-clinical and clinical findings. Prog. Mol. Biol. Transl. Sci. 167 , 25–75 (2019).
Butler, K. & Le Foll, B. Novel therapeutic and drug development strategies for tobacco use disorder: endocannabinoid modulation. Expert Opin. Drug Discov. 15 , 1065–1080 (2020).
D’Souza, D. C. et al. Efficacy and safety of a fatty acid amide hydrolase inhibitor (PF-04457845) in the treatment of cannabis withdrawal and dependence in men: a double-blind, placebo-controlled, parallel group, phase 2a single-site randomised controlled trial. Lancet Psychiatry 6 , 35–45 (2019).
Robinson, J. D. et al. Pooled analysis of three randomized, double-blind, placebo controlled trials with rimonabant for smoking cessation. Addict. Biol. 23 , 291–303 (2018).
Gueye, A. B. et al. The CB1 neutral antagonist AM4113 retains the therapeutic efficacy of the inverse agonist rimonabant for nicotine dependence and weight loss with better psychiatric tolerability. Int. J. Neuropsychopharmacol. https://doi.org/10.1093/ijnp/pyw068 (2016).
Yammine, L. et al. Exenatide adjunct to nicotine patch facilitates smoking cessation and may reduce post-cessation weight gain: a pilot randomized controlled trial. Nicotine Tob. Res. 23 , 1682–1690 (2021).
Eren-Yazicioglu, C. Y., Yigit, A., Dogruoz, R. E. & Yapici-Eser, H. Can GLP-1 be a target for reward system related disorders? A qualitative synthesis and systematic review analysis of studies on palatable food, drugs of abuse, and alcohol. Front. Behav. Neurosci. 14 , 614884 (2020).
Vanderkam, P. et al. Effectiveness of drugs acting on adrenergic receptors in the treatment for tobacco or alcohol use disorders: systematic review and meta-analysis. Addiction 116 , 1011–1020 (2021).
Sokoloff, P. & Le Foll, B. The dopamine D3 receptor, a quarter century later. Eur. J. Neurosci. 45 , 2–19 (2017).
David, S. P., Lancaster, T., Stead, L. F., Evins, A. E. & Prochaska, J. J. Opioid antagonists for smoking cessation. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD003086.pub3 (2013).
Ray, L. A. et al. Efficacy of combining varenicline and naltrexone for smoking cessation and drinking reduction: a randomized clinical trial. Am. J. Psychiatry 178 , 818–828 (2021).
Mooney, M. E. et al. Bupropion and naltrexone for smoking cessation: a double-blind randomized placebo-controlled clinical trial. Clin. Pharmacol. Ther. 100 , 344–352 (2016).
Justinova, Z., Le Foll, B., Redhi, G. H., Markou, A. & Goldberg, S. R. Differential effects of the metabotropic glutamate 2/3 receptor agonist LY379268 on nicotine versus cocaine self-administration and relapse in squirrel monkeys. Psychopharmacology 233 , 1791–1800 (2016).
Le Foll, B., Wertheim, C. E. & Goldberg, S. R. Effects of baclofen on conditioned rewarding and discriminative stimulus effects of nicotine in rats. Neurosci. Lett. 443 , 236–240 (2008).
Franklin, T. R. et al. The GABA B agonist baclofen reduces cigarette consumption in a preliminary double-blind placebo-controlled smoking reduction study. Drug Alcohol. Depend. 103 , 30–36 (2009).
Lotfy, N., Elsawah, H. & Hassan, M. Topiramate for smoking cessation: systematic review and meta-analysis. Tob. Prev. Cessat. 6 , 14 (2020).
Shanahan, W. R., Rose, J. E., Glicklich, A., Stubbe, S. & Sanchez-Kam, M. Lorcaserin for smoking cessation and associated weight gain: a randomized 12-week clinical trial. Nicotine Tob. Res. 19 , 944–951 (2017).
Higgins, G. A., Fletcher, P. J. & Shanahan, W. R. Lorcaserin: a review of its preclinical and clinical pharmacology and therapeutic potential. Pharmacol. Ther. 205 , 107417 (2020).
Stead, L. F. & Lancaster, T. Interventions to reduce harm from continued tobacco use. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD005231.pub2 (2007).
Download references
Acknowledgements
B.Le F. is supported by a clinician-scientist award from the Department of Family and Community Medicine at the University of Toronto and the Addiction Psychiatry Chair from the University of Toronto. The funding bodies had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication. The authors thank H. Fu (University of Toronto) for assistance with Figs 1–3.
Author information
Authors and affiliations.
Translational Addiction Research Laboratory, Campbell Family Mental Health Research Institute, Centre for Addiction and Mental Health, University of Toronto, Toronto, Ontario, Canada
Bernard Le Foll
Departments of Family and Community Medicine, Psychiatry, Pharmacology and Toxicology, University of Toronto, Toronto, Ontario, Canada
Department of Medicine, University of Wisconsin, Madison, WI, USA
Megan E. Piper
University of Wisconsin Center for Tobacco Research and Intervention, Madison, WI, USA
Department of Neurobiology and Behaviour, University of California Irvine, Irvine, CA, USA
Christie D. Fowler
Section for Preventive Cardiology, Department of Endocrinology, Morbid Obesity and Preventive Medicine, Oslo University Hospital, Oslo, Norway
Serena Tonstad
Department of Psychiatry, Washington University School of Medicine, St. Louis, MO, USA
Laura Bierut
Institute of Mental Health, Peking University Sixth Hospital, Peking University, Beijing, China
National Institute on Drug Dependence, Peking University Health Science Center, Beijing, China
Centre for Global Health Research, Unity Health Toronto, University of Toronto, Toronto, Ontario, Canada
- Prabhat Jha
National Centre for Youth Substance Use Research, The University of Queensland, St Lucia, Queensland, Australia
Wayne D. Hall
Queensland Alliance for Environmental Health Sciences, The University of Queensland, Woolloongabba, Queensland, Australia
You can also search for this author in PubMed Google Scholar
Contributions
Introduction (B.Le F.); Epidemiology (P.J. and W.D.H.); Mechanisms/pathophysiology (C.D.F., L.B., L.L. and B.Le F.); Diagnosis, screening and prevention (P.J., M.E.P., S.T. and B.Le F.); Management (M.E.P., S.T., W.D.H., L.L. and B.Le F.); Quality of life (P.J. and W.D.H.); Outlook (all); Conclusions (all). All authors contributed substantially to the review and editing of the manuscript.
Corresponding author
Correspondence to Bernard Le Foll .
Ethics declarations
Competing interests.
B.Le F. has obtained funding from Pfizer (GRAND Awards, including salary support) for investigator-initiated projects. B.Le F. has received some in-kind donations of cannabis product from Aurora and medication donation from Pfizer and Bioprojet and was provided a coil for TMS study from Brainsway. B.Le F. has obtained industry funding from Canopy (through research grants handled by CAMH or the University of Toronto), Bioprojet, ACS, Indivior and Alkermes. B.Le F. has received in-kind donations of nabiximols from GW Pharma for past studies funded by CIHR and NIH. B.Le F. has been an advisor to Shinoghi. S.T. has received honoraria from Pfizer the manufacturer of varenicline for lectures and advice. All other authors declare no competing interests.
Peer review
Peer reviewer information.
Nature Reviews Disease Primers thanks Jamie Brown, Elisardo Iglesias and Ming Li for their contribution to the peer review of this work.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
CTRI website: https://d3futrf33lk36a.cloudfront.net/wp-content/uploads/sites/240/2019/04/Meds-Chart.pdf
Philip Morris International: https://www.pmi.com/
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Le Foll, B., Piper, M.E., Fowler, C.D. et al. Tobacco and nicotine use. Nat Rev Dis Primers 8 , 19 (2022). https://doi.org/10.1038/s41572-022-00346-w
Download citation
Accepted : 07 February 2022
Published : 24 March 2022
DOI : https://doi.org/10.1038/s41572-022-00346-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Integrated mrna- and mirna-sequencing analyses unveil the underlying mechanism of tobacco pollutant-induced developmental toxicity in zebrafish embryos.
- Jiasheng Chen
- Xiaoping Zhong
Journal of Translational Medicine (2024)
Reductions in smoking due to ratification of the Framework Convention for Tobacco Control in 171 countries
- Guillermo Paraje
- Mauricio Flores Muñoz
Nature Medicine (2024)
Nicotinic regulation of microglia: potential contributions to addiction
- Alexa R. Soares
- Marina R. Picciotto
Journal of Neural Transmission (2024)
Improving the Quality of Low-grade Tobacco by Enzymatic Treatment and Co-fermentation with Yeast and Lactic Acid Bacteria
Applied Biochemistry and Biotechnology (2024)
Modulation of Nicotine-Associated Behaviour in Rats By μ-Opioid Signals from the Medial Prefrontal Cortex to the Nucleus Accumbens Shell
- Hirosato Kanda
Neuroscience Bulletin (2024)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
Tobacco, Nicotine, and E-Cigarettes Research Report What research is being done on tobacco use?
New scientific developments can improve our understanding of nicotine addiction and spur the development of better prevention and treatment strategies.
Genetics and Epigenetics
An estimated 50-75 percent of the risk for nicotine addiction is attributable to genetic factors. 221 A cluster of genes (CHRNA5-CHRNA3-CHRNB4) on chromosome 15 that encode the α5, α3, and β4 protein subunits that make up the brain receptor for nicotine 221–223 are particularly implicated in nicotine dependence and smoking among people of European descent. Variation in the CHRNA5 gene influences the effectiveness of combination NRT, but not varenicline. 224 Other research has identified genes that influence nicotine metabolism and therefore, the number of cigarettes smoked, 225 responsiveness to medication, 204,205 and chances of successfully quitting. 226 For example, the therapeutic response to varenicline is associated with variants for the CHRNB2, CHRNA5, and CHRNA4 genes, while bupropion-related cessation is linked with variation in genes that affect nicotine metabolism. 227
Smoking can also lead to persistent changes in gene expression (epigenetic changes), which may contribute to associated medical consequences over the long term, even following cessation. 228 Epigenetic changes may serve as a potential biomarker for prenatal tobacco smoke exposure. Researchers found tobacco-specific changes at 26 sites on the epigenome, and this pattern predicted prenatal exposure with 81 percent accuracy. 229 A large scale meta-analysis of data on epigenetic changes associated with prenatal exposure to cigarette smoke also identified many epigenetic changes that persisted into later childhood. 230 More research is needed to understand the long-term health impacts of these changes.
Neuroimaging
Cutting-edge neuroimaging technologies have identified brain changes associated with nicotine dependence and smoking. Using functional magnetic resonance imaging (fMRI), scientists can visualize smokers’ brains as they respond to cigarette-associated cues that can trigger craving and relapse. 231 Such research may lead to a biomarker for relapse risk and for monitoring treatment progress, as well as point to regions of the brain involved in the development of nicotine addiction. 29
A neuroimaging technology called default-mode or resting-state fMRI (rs-fMRI) reveals intrinsic brain activity when people are alert but not performing a particular task. Using this technique, researchers are examining the neurobiological profile associated with withdrawal and how nicotine impacts cognition. 232 Comparisons between smokers and nonsmokers suggest that chronic nicotine may weaken connectivity within brain circuits involved in planning, paying attention, and behavioral control—possibly contributing to difficulty with quitting. 233 fMRI studies also reveal the impact of smoking cessation medications on the brain—particularly how they modulate the activity of different brain regions to alleviate withdrawal symptoms and reduce smoking. A review of these studies suggested that NRT enhances cognition during withdrawal by modulating activity in default-network regions, but may not affect neural circuits associated with nicotine addiction. 234
Some imaging techniques allow researchers to visualize neurotransmitters and their receptors, further informing our understanding of nicotine addiction and its treatment. 27 Using these techniques, researchers have established that smoking increases the number of brain receptors for nicotine. Individuals who show greater receptor upregulation are less likely to stop smoking. 28 Combining neuroimaging and genetics may yield particularly useful information for improving and tailoring treatment. For example, nonsmoking adolescents with a particular variant in the CHRNA5-CHRNA3-CHRNB4 gene cluster (which is associated with nicotine dependence and smoking) showed reduced brain activity in response to reward in the striatum as well as the orbitofrontal and anterior cingulate cortex. This finding suggests that genetics can influence how the brain processes rewards which may influence vulnerability to nicotine dependence. 235 Neuroimaging genetics also shows that other genes, including ones that influence dopamine neurotransmission, influence reward sensitivity and risk for addiction to nicotine. 236
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Perceptions of health risks of cigarette smoking: A new measure reveals widespread misunderstanding
Affiliation Department of Communication, Stanford University, Stanford, California, United States of America
Affiliation Graduate School of Business, Stanford University, Stanford, California, United States of America
* E-mail: [email protected]
Affiliations Department of Political Science, Vanderbilt University, Nashville, Tennessee, United States of America, Hoover Institution, Stanford University, Stanford, California, United States of America
Affiliation U.S. Department of Treasury, Washington, D.C., United States of America
Affiliation LinChiat Chang Consulting, LLC, San Francisco, California, United States of America
Affiliation Department of Communication Studies, University of Michigan, Ann Arbor, Michigan, United States of America
Affiliation GfK Custom Research North America, New York City, New York, United States of America
- Jon A. Krosnick,
- Neil Malhotra,
- Cecilia Hyunjung Mo,
- Eduardo F. Bruera,
- LinChiat Chang,
- Josh Pasek,
- Randall K. Thomas

- Published: August 14, 2017
- https://doi.org/10.1371/journal.pone.0182063
- Reader Comments
15 Feb 2019: Krosnick JA, Malhotra N, Mo CH, Bruera EF, Chang L, et al. (2019) Correction: Perceptions of health risks of cigarette smoking: A new measure reveals widespread misunderstanding. PLOS ONE 14(2): e0212705. https://doi.org/10.1371/journal.pone.0212705 View correction
Most Americans recognize that smoking causes serious diseases, yet many Americans continue to smoke. One possible explanation for this paradox is that perhaps Americans do not accurately perceive the extent to which smoking increases the probability of adverse health outcomes. This paper examines the accuracy of Americans’ perceptions of the absolute risk, attributable risk, and relative risk of lung cancer, and assesses which of these beliefs drive Americans’ smoking behavior. Using data from three national surveys, statistical analyses were performed by comparing means, medians, and distributions, and by employing Generalized Additive Models. Perceptions of relative risk were associated as expected with smoking onset and smoking cessation, whereas perceptions of absolute risk and attributable risk were not. Additionally, the relation of relative risk with smoking status was stronger among people who held their risk perceptions with more certainty. Most current smokers, former smokers, and never-smokers considerably underestimated the relative risk of smoking. If, as this paper suggests, people naturally think about the health consequences of smoking in terms of relative risk, smoking rates might be reduced if public understanding of the relative risks of smoking were more accurate and people held those beliefs with more confidence.
Citation: Krosnick JA, Malhotra N, Mo CH, Bruera EF, Chang L, Pasek J, et al. (2017) Perceptions of health risks of cigarette smoking: A new measure reveals widespread misunderstanding. PLoS ONE 12(8): e0182063. https://doi.org/10.1371/journal.pone.0182063
Editor: Raymond Niaura, Legacy, Schroeder Institute for Tobacco Research and Policy Studies, UNITED STATES
Received: May 7, 2016; Accepted: June 20, 2017; Published: August 14, 2017
This is an open access article, free of all copyright, and may be freely reproduced, distributed, transmitted, modified, built upon, or otherwise used by anyone for any lawful purpose. The work is made available under the Creative Commons CC0 public domain dedication.
Data Availability: Data are available at: https://dataverse.harvard.edu/dataset.xhtml?persistentId=doi:10.7910/DVN/JP2JHH , doi: 10.7910/DVN/JP2JHH .
Funding: LC and RKT have commercial affiliations with LinChiat Chang Consulting and GfK Custom Research North America, respectively. These companies provided support in the form of salaries for authors LC and RKT, but did not have any additional role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript. The specific roles of these authors are articulated in the ‘author contributions’ section.
Competing interests: LC and RKT have commercial affiliations with LinChiat Chang Consulting and GfK Custom Research North America, respectively. This does not alter our adherence to PLOS ONE policies on sharing data and materials.
Introduction
Despite a constant flow of messages reminding Americans of the health risks of cigarette smoking, and despite a steady decline in the proportion of Americans who smoke during the last 50 years, more than 20% of Americans continue to smoke regularly today [ 1 ]. This paper explores whether the continued prevalence of smoking may, in part, stem from a failure to acknowledge these risks. At first blush, this assertion may seem patently implausible; much research indicates that increasingly large proportions of Americans recognize the various dangers of smoking, and some studies even suggest that most Americans overestimate the proportion of smokers who suffer from certain smoking-related ailments [ 2 ]. Nonetheless, it is possible that people underestimate the magnitude of some of the health risks caused by smoking. Because individuals seem to base their decisions about whether to smoke on how they believe the act of smoking changes the risk of contracting specific diseases, correcting any underestimation of risk may yield future reductions in smoking onset and increases in cessation [ 3 ]. To explore these possibilities, we conducted three studies of national samples of American adults documenting risk perceptions and their relations to smoking behavior.
Challenges in the study of risk perception
One way to gauge the accuracy of people’s perceptions of the health dangers of smoking is to focus simply on the list of maladies that become more likely as a result of smoking. This list includes various cancers, heart diseases, respiratory diseases, premature death, and more [ 4 , 5 ]. By asking representative national samples of American adults to identify which diseases and medical conditions on a provided list are linked with smoking, researchers have illuminated three interesting patterns. First, since the 1950s, the proportion of Americans who failed to identify any health risks of smoking dropped consistently [ 6 ]. Second, according to Gallup [ 7 ], a sizable proportion of Americans still fails to recognize a link between smoking and some related ailments (see S1 Fig ). Other contemporary surveys support these same conclusions [ 8 – 10 ]. The proportion of American adults who associate smoking with a particular ailment varies considerably across ailments, from a high of 81% who report a link between smoking and cancer to single-digit proportions who identify links with asthma, hypertension, bronchitis, and stroke [ 11 ]. Thus, even today, Americans apparently underestimate the breadth of the danger.
A more refined way to gauge the accuracy of perceptions is to focus on the amount of increased risk of each malady that results from smoking. According to epidemiological studies, each of these increases is a function of many attributes, including age of smoking onset, number of years of regular smoking, number of cigarettes consumed per day, and more [ 4 , 5 ]. Therefore, actual risks must be expressed as variables that are functions of such factors, and perceptions of these risks must be ascertained specifying such factors.
Furthermore, even holding constant age of onset, length of smoking, and dosage, a smoking-related risk can be perceived in three different ways: (1) absolute risk (i.e., “what is the chance that a person will get lung cancer if he/she smokes?”), (2) attributable risk (i.e., “how much does smoking raise the chances that a person will get lung cancer compared to not smoking?”), and (3) relative risk (i.e., “how much more likely is a person to get lung cancer if he/she smokes?”) [ 12 , 13 ]. Mausner and Bahn [ 14 ] provide a thorough review of how epidemiologists calculate and use each of these different measures of risk. Assessing Americans’ perceptions of all three seems most sensible in order to determine whether people tend to perceive all types of risk accurately, overestimate all types of risk, underestimate all types of risk, or overestimate some while underestimating others. Attributable fraction is another measure of risk perceptions, but we do not investigate this measure in this study [ 15 ].
One way to think about the goal of such an investigation is to identify any ways in which people underestimate risk, so that public health education campaigns can correct this misunderstanding. But it could turn out that people underestimate one particular type of risk (e.g., absolute risk) and yet do not use that particular perception of risk in their decision-making about whether to start or stop smoking. Therefore, efforts to correct the public’s misunderstanding would not translate into changes in smoking behavior. So to draw out implications of measurements of perceived risk, we need evidence indicating which perceptions may be behaviorally consequential.
The research described in this paper set out to do so by gauging perceptions of absolute risk, attributable risk, and relative risk with a focus specifically on lung cancer. And we explored which of these risk perceptions might drive smoking onset and cessation. We focus on lung cancer specifically rather than all health risks associated with smoking following Viscusi’s seminal work on smoking-related risks [ 2 ]. While the share of American adults who associate smoking with a particular health malady varies across maladies [ 11 ], an assessment of which type of risk perception—absolute risk, attributable risk, and relative risk—impacts Americans’ smoking behavior the most should not be sensitive to the health malady of interest. In other words, if perceptions of relative risk of lung cancer affects smoking behavior more than perceptions of absolute and attributable risk of lung cancer, then perceptions of relative risk of another disease should similarly be most effective at driving smoking behavior.
Prior studies of perceptions of the magnitude of risk
A number of past studies have attempted to measure perceptions of the magnitude of the risk of smoking in representative samples of American adults, but their methodologies entailed a series of limitations, as we outline next. It is worth noting that this paper focuses on the U.S. and therefore does not discuss the many interesting studies of smoking-related risk perceptions that have been done in countries other than the U.S [ 16 – 18 ].
We also do not discuss studies that examined people’s perceptions of their own personal smoking-related risks (e.g., Boney-McCoy et al. [ 19 ]; Strecher et al. [ 20 ]) because our focus is on Americans’ perceptions of the risk of smoking to people in general. Many studies have produced interesting results involving people’s perceptions of their own personal risks of smoking-related health problems (e.g., [ 19 , 21 – 27 ]). However, according to Gigerenzer [ 28 ], people naturally think about the population rather than personal chance, and perceptions of personal risk likely mediate the relationship between general risk and behavior.
Because this paper is focused on the beliefs of adults, we also do not discuss the findings of many interesting studies of youth. For example, Romer and Jamieson [ 29 ] asked questions similar to Viscusi’s [ 2 ] of a national sample of 14- and 15-year-olds: “Out of every 100 cigarette smokers, how many do you think will: (a) get lung cancer because they smoke? (b) have heart problems, like a heart attack, because they smoke? (c) die from a smoking-related illness?” Their results mirror Viscusi’s [ 2 ]: on average; respondents said 61.4% of smokers would develop lung cancer, much higher than the true rate. Likewise, a representative sample of 20–22 year olds said 52.6% on average. Many other studies have explored the beliefs of children and adolescents as well [ 21 , 30 – 37 ].
Some past studies have asked people to describe their perceptions of the magnitude of a smoking-related risk of some malady by asking people to select a point on a rating scale with a small number of verbally labeled response options. For example, Weinstein et al. [ 27 ] asked “How likely do you think it is that (the average male cigarette smoker/the average female cigarette smoker/you) will develop lung cancer in the future?” and offered a 5-point scale ranging from “very low” to “very high.” Similarly, Romer and Jamieson [ 29 ] asked respondents “In your opinion, is smoking very risky for a person’s health, somewhat risky, only a little risky, or not risky at all?” It is not clear whether “somewhat risky” or “very risky” is an overestimate or underestimate of risk. In other words, measures that assess perceptions of smoking’s dangers on these non-numeric subjective probability scales do not permit assessing the degree to which magnitudes of perceived risk reflect true numeric risk levels.
Other studies have measured perceptions of risks quantitatively but did not specify the population of people being described or the dosage of smoking being addressed. For example, in a survey conducted by Audits & Surveys Worldwide, respondents were asked, “Among 100 cigarette smokers, how many of them do you think will get lung cancer because they smoke?” [ 2 ]. The characteristics of a smoker are important contextual considerations with regards to actual health risks a given smoker faces. The probabilities of various smoking-related ailments differ for occasional and daily smokers and depend on the age of a smoker as well as the duration of smoking. Because this type of question does not specify what population is to be described or how much smoking was done for how long, it is impossible to gauge the accuracy of responses by comparing them with the results of epidemiological studies, which show risk to vary across populations and age, smoking duration, and dosage. Some scholarly work has begun to remedy this issue, specifying the exact quantity of cigarettes smoked per day [ 38 ].
Another potential limitation of the Audits & Surveys question is the phrase “because they smoke.” This phrase was presumably meant to lead respondents to estimate the number of lung cancer cases completely attributable to smoking. As Slovic [ 36 ] observed, this phrase can be interpreted in various different ways. Specifically, people may believe that smoking, along with other factors, enhances the chances of contracting lung cancer, leading them to respond that smoking is partially responsible for some lung cancer cases. This, too, makes it difficult to identify the appropriate true rate of smoking-induced lung cancer cases to which to compare risk perceptions.
Finally, the notions of “subadditivity” and “the focus of judgment effect” point to another potential problem with the Audits & Surveys question [ 39 – 41 ]. The question, “Among 100 cigarette smokers, how many of them do you think will get lung cancer because they smoke?” focuses respondents’ attention on just one possible outcome of smoking: getting lung cancer. This approach typically leads to overestimation of the probability of the event in question. Asking respondents instead to report the number of smokers who will not get lung cancer would focus attention on that outcome instead, probably leading to overstatement of that probability. So the sum of the average answers to these two forms of the question would most likely total more than 100. A more desirable measurement approach would overcome the bias induced by arbitrarily asking about only one outcome (e.g., either getting lung cancer or not getting lung cancer).
The present research
To overcome the limitations of past studies, we conducted three surveys measuring Americans’ beliefs about smoking-related health risks in different ways. To gauge perceived risk, we asked two questions: one about the risk to nonsmokers, and the other about the risk to smokers. This approach is advantageous if a researcher wants to measure perceptions of attributable risk or relative risk, because (1) subadditivity is likely to bias both reports upward, so subtracting or dividing one judgment from or by the other will minimize the impact of overestimation, (2) answers to these questions can be used to generate assessments of perceived absolute risk, attributable risk, and relative risk, and (3) this approach employs the principle of decomposition, which enhances the accuracy of measures of people’s beliefs [ 15 ]. It is worth noting one limitation of our research is the fact that we only ask about lung cancer, and do not consider other health risks linked with smoking. However, most likely people’s perceptions of risk across multiple disease categories would be positively correlated. Consequently, our general conclusions about lung cancer would likely be similar if respondents were forced to consider multiple disease categories.
In decomposition, a single, global judgment is broken down into a series of sub-judgments, each of which a respondent must make in the process of generating the global judgment. Here, in order to gauge people’s perceptions of relative risk, we could ask, “how many more times likely is a smoker to get lung cancer than a nonsmoker?” To answer the global question, a respondent must estimate both the likelihood a nonsmoker will get lung cancer and estimate the likelihood that a smoker will get lung cancer, and then mentally compute the ratio of the probabilities. Because respondents can accidentally make a computational error when executing that last step, surveyors can more accurately measure people’s beliefs by asking directly about the sub-judgments, leaving the researcher to compute the ratio. The same logic applies to the measurement of perceived attributable risk (see S1 Appendix for a discussion of measuring probabilities and numeracy).
When measuring perceptions of the lung cancer risks of nonsmokers and smokers, we expressed specifically a volume of smoking and at what age it began, so we could more accurately gauge the extent to which people overestimated or under-estimated the health risks of smoking. And rather than asking survey respondents to report probabilities, we asked them to report frequencies, since a variety of studies suggest that people think more naturally in terms of frequencies [ 42 , 43 ].
We compared the three risk perception measures (absolute, attributable, and relative risk) in terms of their associations with cessation among a sample of current and former smokers. We also compared the risk perception measures in terms of their associations with the desire to quit among current smokers. Although previous studies have found positive and significant correlations between risk perceptions and the desire to quit, none of these studies compared different risk perception measures to one another or analyzed numerical risk estimates [ 27 , 44 , 45 ].
Such associations can occur for at least two reasons. First, beliefs about the health risks of smoking may be instigators of smoking cessation (for a review of this literature, see S2 Appendix ). Second, people may adjust their beliefs about smoking’s health risks in order to rationalize their status as a smoker or a non-smoker [ 46 – 48 ]. If perceptions of health risks are motivators of smoking cessation and/or if quitting smoking induces people to inflate their risk perceptions, then perceived risk should be lower among people who currently smoke than among people who have quit. That is, the higher a person’s perceived risk, the more likely he or she is to have quit. Likewise, the higher a current smoker’s perception of risk, the more motivated he or she should be to quit smoking. Therefore, the more strongly a risk perception measure is associated with whether a person has quit smoking and a smoker’s desire to quit, the more likely that risk perception is to capture the way people naturally think about risk in this arena.
Many possible patterns of risk perception types could be found in a population. The most heterogeneous pattern would be one in which one-third of people think in terms of absolute risk, while another one-third of people think in terms of attributable risk, and the remaining people think in terms of relative risk. The most homogeneous case would be one in which everyone thinks in terms of just one of these risk perceptions to make behavioral choices regarding smoking. Our analyses explored the extent of use of each of the three risk perception measures.
We also explored whether people who felt more certain about risk perceptions manifested stronger relations of those perceptions with cessation and desire to quit. Psychological research on attitude strength suggests that people hold beliefs and attitudes with varying degrees of certainty, and beliefs held with more certainty are more likely to shape thinking and action [ 49 ]. Therefore, we explored whether any of the risk perceptions were more strongly related to cessation among people who held their risk perceptions with more certainty.
Three studies
Our three studies explored five main questions: (1) How many people overestimate and underestimate absolute risk, attributable risk, and relative risk of lung cancer due to smoking? (2) How strongly are perceived absolute risk, attributable risk, and relative risk related to quitting? (3) How strongly are perceived absolute risk, attributable risk, and relative risk related to desire to quit among current smokers? (4) Are the relations between risk perceptions and quitting strongest among respondents who are most certain about their risk perceptions? (5) How strongly are perceived absolute risk, attributable risk, and relative risk related to having initiated smoking?
Study 1 was a random digit dial telephone survey of a nationally representative sample of American adults who were current or former smokers, conducted in 2000 by Schulman, Ronca, and Bucuvalas, Inc. (hereafter SRBI). Study 2 was a 2006 survey of a national non-representative sample of current and former smokers who volunteered to complete Internet surveys for Harris Interactive in exchange for points that could be redeemed for gifts. Study 3 was a 2009 survey of a nationally representative sample of all Americans, including people who had never smoked, via the Face-to-Face Recruited Internet Survey Platform (the FFRISP; see S3 Appendix for descriptions of the methodologies of the three studies, and see S4 Appendix for the demographic characteristics of the three samples).
The telephone survey respondents who were current or former smokers were asked:
(1) “Next, I'd like to turn to a different topic: what you personally think about the effect of cigarette smoking on people's health. I'm going to read these next two questions very slowly to let you think about each part of them, and I can repeat each question as many times as you like before you answer, so you can be sure they are clear to you. First, if we were to randomly choose one thousand American adults who never smoked cigarettes at all during their lives, how many of those one thousand people do you think would get lung cancer sometime during their lives?” (2) “And if we were to randomly choose one thousand American adults who each smoked one pack of cigarettes a day every day for 20 years starting when they were 20 years old, how many of those one thousand people do you think would get lung cancer sometime during their lives?” (3) “You said that smokers are [more likely/as likely/less likely] to get lung cancer than nonsmokers. How certain are you about this? Extremely certain, very certain, moderately certain, slightly certain, or not certain at all?”
We ask respondents to assess the prospect of lung cancer incidence generally like Viscusi [ 2 ]. We emphasized “personally” so that people would feel comfortable providing their own best guess of a fact, specifically general population risk of contracting lung cancer. This wording is designed to avoid the question seeming like a “quiz” (or their guess of what a public health authority might say), but rather their personal assessment of risk. For the two Internet surveys, the wording was adapted for self-administration. In all three studies, the response choices for the last question were presented in descending order for a randomly chosen half of the respondents and in ascending order for the other half. By implementing the same internally valid research design three separate times, it is possible to assess whether our findings are replicable.
Each of the three studies discussed above were deemed as suitable for exempt IRB review status by Stanford University’s review board, as no identifying information on the respondents was retained, and disclosure of answers to the survey questions would not place the respondents at risk. Informed consent for Study 1 was provided verbally given that Study 1 was a telephone survey. Written informed consent was provided for both Study 2 and Study 3, and Stanford’s IRB approved use of oral consent in Study 1 and written consent in Study 2 and 3.
Actual risk
We used data reported by Peto et al. [ 50 ] to compute the actual absolute risk, attributable risk, and relative risk of contracting lung cancer for one-pack-a-day smokers who started smoking at age 20 and smoked for 20 years. To do so, we divided the absolute risk of mortality due to lung cancer among these smokers (about 3%) by the absolute risk of mortality due to lung cancer among non-smokers (about 0.4%, yielding a relative risk of about 7). Although Peto et al. [ 50 ] examined mortality instead of incidence, the probability of dying from lung cancer conditional on developing lung cancer is 74.4% within a thirteen-year period according to Marcus et al. [ 51 ], and even higher among smokers [ 52 ]. If relative risk is higher, then our results understate the proportion of Americans who underestimate this relative risk. According to these figures, the attributable risk of lung cancer due to smoking is then about 3% (3% minus 0.4%, rounds to 3%). It is worth noting that although one might imagine that it is difficult to estimate risk rates because of complex functional forms, interactions of smoking with other risk factors, cohort effects, and other complications, research suggests that in fact, risk rates are largely robust to some potential complexities [ 53 – 55 ].
Perceived risk
In Study 1, the mean of current and former smokers’ perceptions of absolute risk of lung cancer among smokers was 48% (i.e., 480.1 smokers out of 1,000 smokers would get lung cancer); the median was 50% (see columns 1 and 2 of Table 1 ). 10.3% of respondents perceived absolute risks between 0% and 5.0%, and the remaining respondents gave answers above 5.0%. 99.5% of respondents overestimated absolute risk, only about 0.3% estimated it correctly (by giving an answer of 30), and 0.2% underestimated it (by giving an answer less than 30).
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0182063.t001
As expected, the mean and median perceived absolute risk of nonsmokers getting lung cancer were less: 22% and 10%, respectively. Thirty-six percent of respondents gave answers between 0% and 5.0%. Thus, most people vastly overestimated this absolute risk.
Only 5.2% of respondents thought smokers were less likely to get lung cancer than nonsmokers (a belief revealed by attributable risks less than 0; see columns 1 and 2 of Table 2 ). Attributable risk was calculated by subtracting each respondent’s answer to the question about nonsmokers from his or her answer to the question about smokers. 9.6% of respondents thought smokers and nonsmokers were equally likely to contract lung cancer, reporting an attributable risk of 0. A large majority, 85.2% of respondents, reported that smokers were more likely than nonsmokers to contract lung cancer. 76.1% overestimated attributable risk by reporting figures greater than 4%. The mean perceived attributable risk was about 27%, and the median was 20%.
https://doi.org/10.1371/journal.pone.0182063.t002
In contrast, a large majority of respondents (74.6%) underestimated relative risk, because they reported perceptions that implied a relative risk less than 7 (see columns 1 and 2 of Table 3 ). Relative risk was computed by dividing each respondent's answer to the question about 1,000 smokers by his or her answer to the question about 1,000 nonsmokers. Because this quantity is undefined for respondents who said none of the 1,000 nonsmokers would get lung cancer (because the denominator would be zero), 1 was added to these respondents’ answers to the questions about smokers and nonsmokers to allow the relative risk quantity to be defined for all respondents. Note that re-computing all analyses reported below treating these people as having missing data on the relative risk measure had negligible impact on the reported results. 54.6% of the respondents could be said to have vastly underestimated relative risk, because their reports implied a value less than 3. Only about 1.5% of respondents perceived relative risk approximately correctly (e.g., 7), and only 23.9% of respondents overestimated relative risk. 5.2% of respondents perceived a relative risk of less than 1, meaning they thought smokers developed lung cancer less often than nonsmokers, and 9.6% of the sample perceived a relative risk of 1.0, meaning they thought smokers and nonsmokers were equally likely to develop lung cancer. Mean perceived relative risk was 26.7, much higher than the true value, and the median was 2.5, lower than the true value. Thus, relative risk tells a very different story about the prevalent errors in risk perceptions than does attributable risk: most people overestimated the latter, whereas most people underestimated the former.
https://doi.org/10.1371/journal.pone.0182063.t003
Compared to the representative sample of current and formers smokers interviewed in Study 1, Study 2’s non-probability sample of current and former smokers reported: (1) lower perceived absolute risk of lung cancer among nonsmokers and smokers (e.g., 49.5% and 25.7%, respectively, gave answers between 0 and 50 out of 1,000 who would get lung cancer, compared to 36.0% and 10.3% in Study 1; see seventh and eighth columns in Table 1 ); (2) lower perceived attributable risk (e.g., 50.9% had a value of 99 or less, compared to 30.7% of the Study 1 respondents; see the eighth column of Table 2 ); and (3) lower perceived relative risk (e.g., 59.5% had values of 2.99 or less, as compared with 54.6% of the Study 1 respondents; see the eighth column of Table 3 ).
Using all three risk measures, Study 3’s representative sample of current and former smokers perceived less risk than the Study 1’s respondents did 9 years earlier. Study 3’s current and former smokers reported lower absolute risk among nonsmokers (mean = 11.9%, median = 5%) than did the Study 1 respondents (mean = 21.5%, median = 10%; see columns nine and one, respectively, of Table 1 ). Study 3’s current and former smokers perceived lower absolute risk for smokers than did the Study 1 respondents (means = 33.1% vs. 48.0%; medians = 30.0% vs. 50.0%; see columns ten and two, respectively, of Table 1 ). And Study 3’s current and former smokers perceived lower attributable risk of smoking than did the Study 1 respondents (means = 21.1% vs. 26.7%; medians = 11.5% vs. 20.0%; see columns nine and one, respectively, of Table 2 ) and lower relative risk than did the Study 1 respondents (means = 12.9 vs. 26.7; medians = 2.5 vs. 2.5; see columns 9 and 1, respectively, of Table 3 ).
Study 3 suggests that the perceived risk of lung cancer may have declined among current and former smokers between 2000 and 2009. That is, the two representative sample surveys indicated that respondents’ assessments of the absolute risk of lung cancer for both smokers and non-smokers became notably more accurate during this period.
Comparing risk measures
Which of these measures is an appropriate focus for claims about public risk perceptions and their accuracy? One way to answer this question is to determine which of these risk perceptions drives people’s decisions about whether or not to smoke. Many possible patterns of risk perception use are possible in any population. The most heterogeneous pattern would be one in which some people decide whether to smoke or quit based upon their perceptions of the attributable risk, while others make this decision with reference to perceptions of relative risk, and still others make their decisions based on perceptions of absolute risk, with the three groups being of roughly equal size. The most homogeneous case is that in which everyone uses just one of these risk perceptions to make their behavioral choices regarding smoking. By gauging which risk perceptions have how much impact for how many people, we can begin to understand whether smoking behavior overall in a population is driven mostly by perceptions that overestimate risk, mostly by perceptions that underestimate risk, or by a mixture of perceptions that sometimes overestimate and other times underestimate.
The data of all three studies allowed us to explore whether perceptions of attributable risk, relative risk, and absolute risk inspire people to quit smoking by comparing current and former smokers. If perceptions of health risks are indeed a principal motivator of smoking cessation, then perceived risk should be lower among people who currently smoke than among people who used to smoke but have quit. In other words, the higher a person’s perceived risk, the more likely he or she should be to have quit smoking. Based upon this assumption, the better a risk perception measure predicts whether a person has quit smoking, the more likely that risk perception is to have driven quitting decisions.
To adjudicate whether absolute risk, attributable risk, or relative risk drove people’s decisions to quit, we estimated the parameters of generalized additive models (GAMs) comparing current smokers to former smokers by using a Gaussian link function predicting a binary variable representing whether a respondent was a current or former smoker using the various measures of perceived risk and the weights for unequal probability of selection and demographic post-stratification (see S5 Appendix for more details on GAMs). GAMs are especially useful for estimating models containing two highly correlated predictors (as we have here) because relaxing the assumption of linearity prevents model misspecification, allowing for better isolation of the unique relations of different risk perceptions with other variables.
Using this flexible approach, we first estimated a model in which relative and attributable risk predicted quitting (more precisely, having quit). It might seem appealing to estimate GAMs predicting quitting using all three measures, but non-independence among the three measures of perceived risk makes that impossible. When examining Study 1’s data, we see that perceptions of relative risk were sensibly correlated with diminished chances of remaining a smoker (see the top-left panel of S2 Fig ). The dark line in the figure represents the estimated relation, and the two light lines demark the bounds of the 95% confidence interval around the estimates. The small vertical lines at the bottom of the figure (called “rugmarks”) indicate whether one or more respondents provided a data point at each point along the x-axis. Increasing perceived relative risk was associated with decreased log-odds of remaining a smoker. Movement from the 25 th percentile to the 75 th percentile (weighted) of relative risk increased the probability of quitting by 13.8 percentage points (see the first row of the first column of Table 4 ).
https://doi.org/10.1371/journal.pone.0182063.t004
In contrast, over the range of the bulk of the data (where the majority of the rugmarks on the x-axis are located), the relation between attributable risk and quitting was fairly flat (see bottom-left panel of S2 Fig ). Movement across the interquartile range of attributable risk increased the probability of quitting negligibly, by only 0.3% (see second row of the first column of Table 4 ).
To more formally gauge and compare these relations, we estimated a set of nested GAMs. First, we estimated a model predicting quitting using only attributable risk and then observed the improvement in goodness of fit of the model when we added relative risk as a predictor. A likelihood ratio (hereafter LR) test comparing the log likelihood of the two-variable model to the nested one-variable model indicated that the addition of the extra variable resulted in a significantly better fit (p=.03), meaning that relative risk was a reliable unique predictor of quitting (see third row of the first column of Table 4 ). Next, we estimated a model predicting quitting using only relative risk and then estimated the improvement in goodness of fit when attributable risk was added as a predictor. This addition did not improve the model’s fit significantly (p=.64; see fourth row of the first column of Table 4 ). Thus, relative risk perceptions appear to have been related to decisions to quit smoking, whereas perceptions of attributable risk were not.
To explore whether absolute risk outperforms relative risk, we estimated a GAM in which quitting was predicted by both measures. As shown in the right panels of S2 Fig , relative risk was again sensibly related to quitting (with probability of remaining a smoker declining smoothly as perceived risk increased), whereas absolute risk was not. Again, adding relative risk to a model fitted with only absolute risk improved the fit significantly (p=.002), whereas adding absolute risk to a model with relative risk did not yield a significant improvement in fit (p=.15; see rows seven and eight of the first column of Table 4 ). Movement across the interquartile range of absolute risk was associated with a 10.5% decrease in the chances of quitting, whereas movement across the interquartile range of relative risk was associated with a sizable and more reasonable 15.2% increase in the likelihood of quitting (see rows five and six of the first column of Table 4 ). As shown in columns two and three of Table 4 (as well as S3 and S4 Figs), these same results were replicated in Studies 2 and 3.
There may be an illusion hidden in these results. When people are asked to report a probability but do not know the answer, they sometimes answer “50,” meaning “fifty-fifty” or “I don’t know,” rather than meaning a 50% chance [ 56 ]. To explore the impact of this potential source of measurement error on our conclusions, we re-estimated the logistic GAM by: (1) dropping the respondents who answered “500” to the question about nonsmokers or to the question about smokers; (2) replacing the 500s with values generated by multiple imputation; and (3) replacing the 500s with answers obtained by a follow-up probe. The results supported the above conclusions even more strongly (for details of these approaches and results, see S6 Appendix ).
Next, we explored whether certainty moderated the associations of risk perceptions with quitting behavior. In Study 1, as expected, the correlation of relative risk with quitting was significantly stronger among high certainty respondents (people who were extremely certain, 27% of the sample) than among lower certainty respondents. Among the high certainty respondents, the probability of quitting increased over the interquartile range of relative risk by 23.7 percentage points (p=.008), a much larger increase than among the low certainty respondents, whose positive change was just 10.5 percentage points (p=.054). Accounting for certainty significantly improved the goodness of fit of the model (p=.03).
Likewise, in Study 2, the positive relation between perceived relative risk and quitting was significantly stronger among high certainty respondents than among low certainty respondents (p=.009). Among the high certainty respondents (18% of the sample), movement across the interquartile range of relative risk increased the probability of quitting by 44.1% (p<.001), whereas movement across this interquartile range in the low certainty group was associated with an increase in quitting probability of only 13.6% (p<.001). Accounting for certainty significantly improved the goodness of fit of the model (p=.009).
In Study 3, among high certainty individuals (30.5% of the sample), movement across the interquartile range of relative risk was associated with an increased probability of quitting smoking of 15.8% (p=.06), whereas movement across this interquartile range in the low certainty group was associated with an increase in quitting probability of 11.1% (p=.03). Accounting for certainty again significantly improved the goodness of fit of the model (p=.03).
Desire to quit.
Next, we examined whether current smokers’ risk perceptions were associated with their desire to quit. While a desire to quit does not automatically translate to smoking cessation, a strong desire to quit is predictive of subsequent quitting behavior, and is a necessary condition for quitting [ 57 ]. In Study 1, adding relative risk to a GAM model predicting desire to quit among current smokers with attributable risk caused a marginally non-significant improvement in fit (p=.09; see the third row of column four in Table 4 ). Movement from the 25 th to the 75 th percentile of relative risk raised the probability of wanting to quit by 17.0% (see the first row of column four in Table 4 ). But adding attributable risk to a model predicting desire to quit with relative risk did not improve fit significantly (p=.27; see row four of column four in Table 4 ). Movement across the interquartile range of attributable risk slightly lowered desire to quit by 1.1% (see row two of column four in Table 4 ). Likewise, adding relative risk to a model including absolute risk yielded a significant improvement in fit (p=.046; see row seven of column four in Table 4 ). Movement across the interquartile range of relative risk increased desire to quit by 13.9% (see row five in Table 4 ). But adding absolute risk to a model including relative risk marginally significantly decreased desire to quit (interquartile range movement = 15.6%, p=.06; see rows six and eight of column four in Table 4 ). The data from Studies 2 and 3 yielded similar results (see columns five and six of Table 4 ). This further supports the contention that people think in terms of relative risk perceptions.
Smoking onset.
We observed the expected results when we used the three measures in Study 3 to explore whether perceived risk was greater among people who ever smoked than among people who never smoked. Comparing the distributions in the ninth and tenth columns in Table 1 with the distributions in the last two columns of the table, we see that: (1) both groups had similar expectations for the proportion of nonsmokers who would get lung cancer (mean = 11% for people who never smoked vs. 12% for people who ever smoked), but (2) the expected proportion of smokers who would get lung cancer was higher among people who had never smoked (mean = 43.3%) than among people who ever smoked (mean = 33.1%).
Also as expected, people who never smoked perceived higher attributable risk of smoking than did people who ever smoked (see the last two columns in Table 2 ): (1) 3.9% thought that smokers were less likely to contract lung cancer than nonsmokers (attributable risk of less than 0); (2) 6.3% thought that smokers and nonsmokers were equally likely to get lung cancer (attributable risk of 0); and (3) 89.7% thought that smokers were more likely to contract lung cancer than nonsmokers. Respondents who never smoked thought smokers were 32 percentage points more likely than nonsmokers to get lung cancer, on average (see columns 11 and 12 of Table 2 ). Thus, these individuals perceived a higher attributable risk than did current and former smokers (21.1 percentage points; see column nine of Table 2 ). Likewise, respondents who never smoked also perceived higher relative risk than did current and former smokers (compare the last two columns of Table 3 with the ninth and tenth columns of that table).
As expected, perceptions of relative risk were strongly associated with status as a never smoker vs. a current smoker in GAMs (see the left panels of S5 Fig ). Adding relative risk to a model predicting current smoking with attributable risk considerably improved fit (p<.001), whereas adding attributable risk to a model with relative risk did not significantly improve fit (p=.57). Movement across the interquartile range of relative risk yielded a 22.7 percentage point decrease in the likelihood that respondents were smokers. Movement across the interquartile range of attributable risk yielded a decrease in the probability of being a smoker of only 0.7 percentage points.
Likewise, adding relative risk to a model with only absolute risk improved fit significantly (p<.001), whereas adding absolute risk to a model including relative risk was associated with only a marginally significant improvement in fit (p=.07). Movement across the interquartile range of relative risk (when controlling for absolute risk) was associated with a 22.3 percentage point decrease in the probability of ever having smoked (see the right panels of S5 Fig ). In contrast, movement across the interquartile range of absolute risk (when controlling for relative risk) produced only an 8.5 percentage point decrease in the likelihood of ever having smoked.
Summary and implications
Taken together, this evidence suggests that while Americans have overestimated the absolute risk and risk difference of lung cancer associated with cigarette smoking, Americans have generally underestimated the relative risk. Furthermore, this evidence suggests that people may think more about smoking health risks in terms of relative risk than in terms of absolute risk or risk difference. The relations we saw here may result from the influence of health risk beliefs on decisions to quit smoking, decisions to start smoking, and regret about smoking, or these relations may occur because people rationalize their smoking status by adjusting their risk perceptions, or from some other process. Having seen here that these are possibilities, we look forward to future research exploring them to characterize the basis for the relations we observed.
Communication of risk has been a difficult task for medical professionals, and our findings encourage consideration of a different approach to communicating health risks than has been typical on American cigarette packages and in other prominent health communications [ 58 , 59 ]. There are a large number of studies that show that the design of and warnings on cigarette packs can influence perceptions of the risks of smoking [ 60 – 68 ]. However, much constructive work can perhaps still be done by informing individuals about how much smoking increases their health risks. If the findings reported here are correct in suggesting that people use perceptions of relative risk when deciding whether to quit smoking, and if relative risk is indeed underestimated by most current and former smokers, corrective steps in this regard might be consequential. More specifically, if public health efforts are initiated in the future to encourage Americans to more accurately recognize the magnitudes of relative risks for various undesirable health outcomes of cigarette consumption, this may well lead to a reduction in the nation’s smoking rate and a consequent reduction in smoking-related morbidity and mortality. This may be why quantitative information about relative risk on cigarette packages in Australia (e.g., “Tobacco smoking causes more than four times the number of deaths caused by car accidents.”) appears to have been effective in encouraging smoking cessation [ 69 ].
Future research could explore these possibilities with experiments gauging the effects of different ways of describing risks on cigarette packages and other health communication mediums like television advertisements, poster campaigns, and doctor-patient communication [ 70 ]. Our findings suggest that when conducting such experiments, it may be desirable to attempt to alter people’s perceptions of relative risk in order to most directly address people’s natural approach to thinking about health risks in this arena. Perceptions of relative risk might be changed best by making such direct statements. But it may also be that such perceptions can be changed even more effectively by inducing affective reactions or in other non-quantitative ways, while simultaneously maximizing trust in the source of the information [ 71 , 72 ]. It is important to bear in mind that even successful efforts to change risk perceptions may not produce changes in behavior, so it will be important for future investigations to assess whether risk perception changes are translated into action [ 73 ].
In addition to their applied value, the findings reported here are interesting in basic psychological terms. By distinguishing between absolute, attributable, and relative risk, the present findings encourage future study with such measures to understand how people make many types of risky decisions and, more generally, how people trade off probabilities when making choices. And many important questions remain regarding risk perceptions involving smoking, such as how people arrive at their perceptions of relative, attributable, and absolute risk, and when and why some people use one measure rather than another to make behavioral decisions. Future studies of these sorts of issues seem merited, both in the smoking and other domains.
Resonance with other findings
Various findings reported here resonate with findings of some past studies. For example, Viscusi [ 2 ] and Borland [ 69 ] found that people overestimated the absolute risk of smoking. Khwaja et al. [ 74 ] found that both smokers and non-smokers overestimated their risks of dying from all sorts of causes [ 69 ]. When Weinstein et al. [ 27 ] asked respondents to assess the relative risk of smoking (“Would you say the average smoker has about the same lung cancer risk as a nonsmoker, a little higher lung cancer risk than a nonsmoker, twice the nonsmoker’s risk, five times the nonsmoker’s risk, or ten times the nonsmoker’s risk?”), smokers offered underestimates.
Boney-McCoy et al. [ 19 ] found that current smokers perceived the absolute risk of smoking to be significantly lower than that perceived by former smokers. This is consistent with the evidence reported here that when considered alone, absolute risk perceptions are related to quitting in the same way. However, when controlling for relative risk, the relation of quitting to absolute risk perceptions was close to zero in the present data.
Antoñanzas et al. [ 75 ] found distributions of Spaniards’ perceptions of attributable and relative risk (regarding the impact of cigarette smoking on lung cancer and heart disease) very similar to those reported here. Viscusi et al. [ 76 ] found that each of these risk perceptions predicted Spaniards’ status as a smoker or nonsmoker when considered alone, and relative risk was a considerably stronger predictor than attributable risk, though Viscusi et al. [ 76 ] did not assess the predictive abilities of perceived attributable risk and relative risk in a single regression equation.
The present evidence that people seem to think in terms of relative risk rather than attributable or absolute risk resonates with research on effective ways to communicate risks to patients [ 77 , 78 ]. For example, Malenka et al. [ 13 ] asked respondents to imagine they had a disease and could choose to take one of two medications—one described in terms of its impact on relative risk (“reduces risk of dying by 80%”) and the other (statistically equivalent) described in terms of impact on attributable risk (“can prevent 8 deaths per 100 people”). Most respondents preferred the medication described in terms of relative risk, perhaps because this portrayal resonated with people’s natural way of thinking about medication benefits found that relative risk information had more impact than did attributable risk information [ 79 – 83 ]. These findings contrast with Saitz’s [ 84 ] and Gigerenzer et al.’s [ 85 ] speculations that people will respond as well or better to attributable risk information (presented as two absolute risks) than to relative risk information, a finding challenged by our data as well.
A preference for thinking about health risks in terms of relative risk is also apparent in news media stories. In one study, 83% of such stories reported benefits of medications in terms of relative risk only, 2% reported benefits in terms of attributable risk only, and 15% reported benefits in terms of both indicators [ 86 ]. Similarly, medical journal articles tend to focus on reports of relative risk rather than attributable risk [ 87 ].
Other directions for further research
Future research might gain more insight into people’s natural ways of thinking about health risks by asking people to describe the health risks of smoking with whatever language they wish. With enough probing, open-ended data gathering might reveal whether people naturally use language evoking absolute risk, attributable risks, or relative risk levels, or a non-numeric representation, and such evidence is worthwhile to collect in future research [ 37 , 88 ]. Future work should also incorporate how much life is lost when calculating risk (see Viscusi [ 38 ] for a discussion of how this might affect an understanding of these results).
Generalizing beyond lung cancer
The focus of the analyses reported here has been people’s perceptions of the risk of getting lung cancer due to smoking. Because lung cancer is one of the best-known health risks of smoking [ 11 ], Americans may be less likely to underestimate the relative risk of lung cancer than of other diseases that are known to be caused by smoking. If we had asked survey questions about heart disease, oral cancers, or stroke instead of lung cancer, the prevalence of underestimation of relative risk may have been even greater than was observed for lung cancer. Correcting these misunderstandings may decrease the expected smoking rate even more. Future studies can explore these possibilities.
Implications regarding other domains of risk perception.
Differentiating perceived relative risk from perceived attributable risk may be useful in other health domains as well. For example, Meltzer and Egleston [ 89 ] reported that patients with diabetes vastly overestimated their own absolute risk of experiencing various complications. But perhaps their perceptions of relative risk are more accurate.
Implications for health education.
Psychological research on health counseling communication has revealed errors in people’s understanding of risk information [ 90 – 92 ]. However, educational efforts can present risk rates in various different ways, and some presentation approaches can cause misunderstandings [ 93 , 92 ]. The present evidence bolsters the conclusions of some past studies suggesting that future research may be most successful when presenting relative risk information to yield better quality decisions [ 94 – 99 ].
Supporting information
S1 fig. proportions of americans who failed to assert that smoking is dangerous to human health: gallup organization surveys..
https://doi.org/10.1371/journal.pone.0182063.s001
S2 Fig. Generalized Additive Models predicting the probability of being a current smoker: SRBI Survey (n = 456).
https://doi.org/10.1371/journal.pone.0182063.s002
S3 Fig. Generalized Additive Models predicting the probability of being a current smoker: Harris Interactive Survey (n = 795).
https://doi.org/10.1371/journal.pone.0182063.s003
S4 Fig. Generalized Additive Models predicting the probability of being a current smoker vs. former smoker: FFRISP (n = 471).
https://doi.org/10.1371/journal.pone.0182063.s004
S5 Fig. Generalized Additive Models predicting the probability of being a current smoker vs. never smoker: FFRISP (n = 714).
https://doi.org/10.1371/journal.pone.0182063.s005
S1 Appendix. Measuring risk.
https://doi.org/10.1371/journal.pone.0182063.s006
S2 Appendix. Literature on the relation of health risk perceptions with quitting smoking.
https://doi.org/10.1371/journal.pone.0182063.s007
S3 Appendix. Survey methodology.
https://doi.org/10.1371/journal.pone.0182063.s008
S4 Appendix. Demographics of current and former smokers in the SRBI Survey, current and former smokers in the Harris Interactive Survey, all individuals in the FFRISP Survey, and the nation’s population.
https://doi.org/10.1371/journal.pone.0182063.s009
S5 Appendix. GAMs.
https://doi.org/10.1371/journal.pone.0182063.s010
S6 Appendix. Exploring responses of 500.
https://doi.org/10.1371/journal.pone.0182063.s011
S7 Appendix. References for supporting information.
https://doi.org/10.1371/journal.pone.0182063.s012
Acknowledgments
The first survey described in this paper was funded by Empire Blue Cross/Blue Shield of New York. The third data set described was collected via the Face-to-Face Recruited Internet Survey Platform (FFRISP), funded by NSF Grant 0619956, Jon A. Krosnick, Principal Investigator. The authors thank Geoffrey Fong and Paul Slovic for very helpful suggestions. The authors acknowledge the excellent research assistance of Virginia Lovison. Jon Krosnick is University Fellow at Resources for the Future.
Author Contributions
- Conceptualization: JAK LC.
- Data curation: JAK NM CHM LC JP RKT.
- Formal analysis: NM CHM LC JP.
- Funding acquisition: JAK RKT.
- Investigation: JAK LC RKT.
- Methodology: NM LC JP.
- Project administration: JAK NM CHM.
- Resources: JAK RKT.
- Software: NM CHM LC JP RKT.
- Supervision: JAK.
- Validation: NM CHM JP.
- Visualization: NM CHM LC JP.
- Writing – original draft: JAK NM CHM EFB JP.
- Writing – review & editing: JAK NM CHM EFB JP.
- 1. Centers for Disease Control and Prevention. Cigarette smoking among adults—United States, 2007.
- 2. Viscusi WK. Smoking: Making the risky decision. New York: Oxford University Press; 1992.
- View Article
- Google Scholar
- PubMed/NCBI
- 6. Newport F, Moore DW, Saad L (Gallup O. Long term Gallup Poll trends: A portrait of American public opinion through the century [Internet]. http://www.gallup.com/poll/3400/longterm-gallup-poll-trends-portrait-american-public-opinion.aspx
- 7. Gallup Organization. National survey. Retrieved from iPOLL Databank, The Roper Center for Public Opinion Research, University of Connecticut. http://www.ropercenter.uconn.edu/ipoll.html . Accessed August 1, 2014.
- 8. Department of Health and Human Services, Public Health Service, Office of the Assistant Secretary for Health, Office on Smoking and Health. Use of Tobacco Survey (ARC Identifier 607143),1986.
- 9. American Lung Association and Gallup Organization. National survey, June 1987. Retrieved from iPOLL Databank, The Roper Center for Public Opinion Research, University of Connecticut. http://www.ropercenter.uconn.edu/ipoll.html . Accessed.
- 12. Manski CF. Identification problems in the social sciences. Cambridge, MA: Harvard University Press; 1995.
- 14. Mausner JS, Bahn JK. Epidemiology: An introductory text. Philadelphia, PA: Saunders; 1974.
- 47. Festinger L. A theory of cognitive dissonance. Stanford, CA: Stanford University Press; 1957.
- 49. Petty RE, Krosnick JA. Attitude strength: Antecedents and consequences. Hillsdale, NJ: Erlbaum; 1995.

Alonzo Mourning, Prostate Cancer Survivor
Online Help
Our 24/7 cancer helpline provides information and answers for people dealing with cancer. We can connect you with trained cancer information specialists who will answer questions about a cancer diagnosis and provide guidance and a compassionate ear.
Chat live online
Select the Live Chat button at the bottom of the page
Call us at 1-800-227-2345
Available any time of day or night
Our highly trained specialists are available 24/7 via phone and on weekdays can assist through online chat. We connect patients, caregivers, and family members with essential services and resources at every step of their cancer journey. Ask us how you can get involved and support the fight against cancer. Some of the topics we can assist with include:
- Referrals to patient-related programs or resources
- Donations, website, or event-related assistance
- Tobacco-related topics
- Volunteer opportunities
- Cancer Information
For medical questions, we encourage you to review our information with your doctor.
- ACS Research
- Lung Cancer
- Smoking Tobacco
The Study That Helped Spur the U.S. Stop-Smoking Movement

Most Americans born into the generations that came after the Baby Boom have gone their entire lives aware that smoking can cause lung cancer. But this fact has not always been well-known – and at one time it wasn’t known at all.
Actually, it wasn’t even until cigarettes were mass produced and popularized by manufacturers in the first part of the 20th century that there was cause for alarm. Prior to the 1900s, lung cancer was a rare disease. Turn-of-the-century changes though, gave way to an era of rapidly increasing lung cancer rates. New technology allowed cigarettes to be produced on a large scale, and advertising glamorized smoking. The military got in on it too – giving cigarettes out for free to soldiers during World Wars I and II.
Cigarette smoking increased rapidly through the 1950s, becoming much more widespread. Per capita cigarette consumption soared from 54 per year in 1900, to 4,345 per year in 1963. And, lung cancer went from rarity to more commonplace – by the early 1950s it became “the most common cancer diagnosed in American men,” writes American Cancer Society Chief Medical Officer Otis Brawley, M.D., in an article published November 2013 in CA: A Cancer Journal for Clinicians .
However, though tobacco usage and lung cancer rates increased in tandem, few experts suspected a connection, according to Brawley and his co-authors.
The 1950 Turning Point
This began to change in the 1950s. Five larger retrospective studies were published in the early 1950’s that again showed a link between cigarette smoking and lung cancer. Though important, these studies still didn’t make a convincing enough case as they relied on the self-reported smoking habits of people who already had lung cancer, and compared them to those who didn’t. One potential problem with this type of study is that people with lung cancer are more likely to overestimate how much they smoked, while those who don’t have lung cancer are more likely to underestimate how much they smoked.
To address this issue, a prospective (cohort) study was needed – recruiting healthy people and following them over time to see who develops or dies from lung cancer and who does not. Without such evidence, the tobacco industry was able to cast doubt on the link between smoking and death from lung cancer and other diseases, says Eric Jacobs, Ph.D., an epidemiologist at the American Cancer Society.
Two American Cancer Society Researchers Get to Work
To address the criticism of the retrospective studies – and to strengthen the evidence that smoking is a cause of lung cancer – E. Cuyler Hammond, Ph.D., and Daniel Horn, Ph.D., scientists working for the American Cancer Society, started work on what is known as a cohort study.
In January 1952, Hammond and Horn engaged 22,000 American Cancer Society volunteers to help recruit a large group of American men aged 50 to 69 across 10 U.S. states and ask these men about their smoking habits. The scientists ended up with a cohort of about 188,000 men, who they eventually followed through 1955.
The participants were asked whether they smoked cigarettes, if they did smoke how often they smoked, and how many cigarettes they smoked. They were asked about both their current and past smoking habits. The questionnaire also asked about cigar and pipe smoking.
In November 1952, the volunteers began the first follow up. Each volunteer was in charge of 5 to 10 men. When the volunteer researchers followed up with their participants, they were required to check on the questionnaire whether the man was “alive,” “dead,” or “don’t know.” Hammond and Horn then obtained copies of the official death certificates of all the men who died to confirm their cause of death.
‘Cause and Effect Relationships’
After following the men for about 20 months, Hammond and Horn had enough information to publish what they called “preliminary” findings in an August 7, 1954 Journal of the American Medical Association article. Their conclusion was clear: “It was found that men with a history of regular cigarette smoking have a considerably higher death rate than men who have never smoked or men who have smoked only cigars or pipes,” the researchers wrote.
Hammond and Horn noted that the higher death rate in smokers was due primarily to heart disease and cancer. “Deaths from cancer were definitely associated with regular cigarette smoking.” They called out lung cancer in particular: “The death rate from lung cancer was much higher among men with a history of regular cigarette smoking than among men who never smoked regularly.”
These two researchers finally felt they had the convincing evidence that cigarette smoking was a cause of lung cancer that the world was previously lacking. They ended their 1954 paper stating “… we are of the opinion that the associations found between regular cigarette smoking and death rates from diseases of the coronary arteries and between regular cigarette smoking and death rates from lung cancer reflect cause and effect relationships.”
Hammond and Horn were so convinced by these findings that they had presented them a couple months earlier, in June of 1954, at the American Medical Association’s annual conference. Previously heavy cigarette smokers, Hammond and Horn changed to pipes by the time of the meeting (although they later concluded that pipe smoking was also cancer causing).
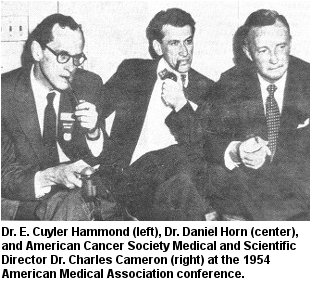
Hammond and Horn’s results were uniquely important at the time, says Susan Gapstur, Ph.D., vice president of the American Cancer Society’s epidemiology research program. “Their study – along with the British Doctor’s study conducted around the same time – were the first two large prospective studies to establish a link between smoking and the subsequent risk of death from lung cancer and other diseases.”
An Even Bigger Study and a Letter to President Kennedy
After his success with the first cohort study, Hammond and the American Cancer Society in 1959 started a larger and more robust long-term follow-up study, called Cancer Prevention Study I (CPS-I). This time, 68,000 volunteers, across 25 states, recruited more than 1 million men and women.
The data Hammond collected through this study provided further conclusive evidence about the harmful effects of smoking and were a major contributor to the landmark 1964 Surgeon General’s Report on Smoking and Health. That report led to sweeping tobacco policy changes in the United States and played a significant role in curbing smoking throughout the nation.
The creation of that landscape-altering report began with a letter sent to President John F. Kennedy in June 1961. In it, leaders from the American Cancer Society, the American Public Health Association, and the National Tuberculosis Association urged Kennedy to form a national commission on smoking to find “a solution to this health problem …” Kennedy asked his surgeon general, Luther Terry, to tackle this.
Terry formed an advisory committee to study the available evidence on smoking and health. Over the course of more than a year, the members analyzed 16 independent studies, conducted in 5 different countries, over a period of 18 years.
“The principal data on the death rates of smokers of various types and of nonsmokers come from 7 large prospective studies of men,” according to the 1964 surgeon general’s report. These studies, when combined, consisted of data from 1,123,000 men, more than half of whom came from the American Cancer Society’s Hammond-Horn Study and Cancer Prevention Study-I.
Terry published the final report January 11, 1964 – 50 years ago. It concluded that: “Cigarette smoking is a health hazard of sufficient importance in the United States to warrant appropriate remedial action.”
That strong judgment fueled stop-smoking efforts across the United States. And since that time, the U.S. smoking rate has dropped by more than half.
Though it took many years after smoking started to decline for the lung cancer death rate to begin to come down, over time, it did – dramatically so for men. In men, lung cancer death rates have declined about 34% from their peak in 1990. In women, lung cancer death rates did not begin to decrease until 2003 because women started smoking in large numbers about 2 decades later than men. The lung cancer death rate among women is now 9% less than it was at its peak in 2002 and is expected to continue declining.

Questions Yet to Answer About Smoking and Health
Although progress has been made, millions of Americans still smoke – and die from – cigarettes. To review the strides the U.S. has made over the past 50 years and provide a call to action for what is left to be done to address tobacco use, the surgeon general will publish a new report on smoking and health in late January.
The report draws on the research that the American Cancer Society and others have continued to do since the time of Hammond and Horn. “The importance of continuing to document the high number of deaths due to cigarettes cannot be overestimated,” says Gapstur, whose team continues to conduct large long-term follow-up studies in the U.S.
Additionally, not every question about the effects of smoking on health has been answered yet. Gapstur and Jacobs say that questions remain about issues such as: exposure to secondhand smoke, particularly in childhood; the effects of e-cigarettes on smoking initiation and cessation; and which former smokers are at high enough risk to benefit from lung cancer screening.
As researchers continue to study smoking and health, additional anti-tobacco efforts are still needed, according to Tom Glynn, Ph.D., director of international cancer control for the American Cancer Society. “Nearly half a million Americans and 6 million people worldwide will die from tobacco use in 2014 – but we know what to do to stop that,” Glynn says.
He calls for implementing the World Health Organization’s global tobacco treaty, continuing to raise taxes on tobacco products, making smoke-free environments the norm rather than the exception, and ensuring science-based tobacco dependence treatment is available to everyone who wants to stop using tobacco. Glynn also wants “to encourage every country to develop the political and financial will to eliminate tobacco as a source of health and economic disruption.”
- Helpful resources
- For researchers
Tobacco and Cancer
Learn More About Lung Cancer
Learn how to apply for a research grant from the American Cancer Society .
American Cancer Society news stories are copyrighted material and are not intended to be used as press releases . For reprint requests, please see our Content Usage Policy .
Related News and Stories
- 1 of Every 4 Global Cancer Deaths Are Caused by Tobacco Use
- Lung Cancer Kills More People Worldwide Than Other Cancer Types
- New Lung Cancer Screening Guideline Increases Eligibility
Help us end cancer as we know it, for everyone.

The background image is A woman, who is visible out-of-focus, holds e-cigarettes.
Welcome to Penn State Center for Research on Tobacco and Health
Penn State Center for Research on Tobacco and Health’s mission is to be a national leader of scientific discovery that will translate into effective interventions and policies to reduce tobacco-caused harm in our communities.
The center comprises a multidisciplinary team of experts, including basic scientists, public health researchers and medical professionals, all dedicated to improving the lives of people touched by tobacco and nicotine addiction. It is based at Penn State College of Medicine and Penn State Health Milton S. Hershey Medical Center in Hershey, Pa.
More than 16 million Americans are living with a disease caused by smoking. Across the world, tobacco is the leading cause of preventable death. The center’s overall goal is to conduct innovative research that will inform future policymaking on tobacco and health, investigate the toxicology and addictiveness of new and existing tobacco products and discover new treatments for addiction.
Tobacco Center of Regulatory Sciences (TCORS)
Two hands with the palms facing up hold items. The right hand contains an electronic cigarette. The left holds five cigarettes.
The College is one of just seven sites across the country to receive the grant as part of the Food and Drug Administration (FDA) and National Institutes of Health’s (NIH) Tobacco Centers of Regulatory Science (TCORS) funding that was awarded in the fall of 2023 .
The TCORS award will fund a trio of studies, led by the College’s Center for Research on Tobacco and Health, that explore how the design of alternative tobacco products can affect their toxicity and addictiveness.
“Our center is unique in that we are addressing both the chemical toxicity of tobacco products (the part that causes harms directly to the human body), and the addictiveness of tobacco products (the characteristic that results in people using tobacco products for decades rather than a few months or years),” said Jonathan Foulds, PhD , one of the principle investigators. “It is the combination of these two factors that determines the overall health effects.”
Information for current/potential study participants
- Current studies
Some of the studies are for people who are not planning to quit, and some are for people interested in quitting in the next 30 days.
See if you qualify for any current studies
- Driving and parking directions

The Center for NMR Research is at 30 Long Lane in Hershey, Pa.

The Clinical Research Center is a dedicated space on the fourth floor of Penn State Health Milton S. Hershey Medical Center.
Study visits for people participating in smoking studies through the Center for Research on Tobacco and Health will either take place in the Clinical Research Center or the Center for NMR Research on the campus of Penn State Health Milton S. Hershey Medical Center and Penn State College of Medicine in Hershey, Pa.
- Smoking cessation resources
- Contact the center
Email: [email protected]
See facility details and driving and parking directions For those who smoke and want to quit, Penn State Center for Research on Tobacco and Health and Penn State Health offer information, options and free smoking cessation classes.
See smoking cessation resources Phone: 844-207-6392
Information for researchers
The background image is An abstract background image based on Penn State's signature shield shape
Penn State TCORS Career Enhancement Core
Training program.
The overall goal of the Penn State Tobacco Center of Regulatory Science (TCORS) Career Enhancement Training Program is to develop knowledge and skills in tobacco regulatory science (TRS) to advance promising scholars toward independent careers in TRS research. Our priorities are to facilitate a pipeline of TRS training for diverse investigators across career stages, foster specialized expertise in tobacco addiction and biomarkers of health and disease, enhance the regulatory impact of TRS research, and facilitate a culture of collaborative and multidisciplinary TRS research between TCORS faculty and trainees.
The training program is open to the following:
- SURIP is intended for college students who are interested in pursuing a career in the biological sciences.
- SURIP provides a variety of career development and scientific research seminars are offered weekly as part of SURIP. Each summer’s program concludes with the Summer Undergraduate Research Symposium, where students present their work.
- Tuition coverage and stipend provided on competitive basis.
- Contact Career Enhancement Core leadership to inform of application
- Medical students enrolled at Penn State College of Medicine at Hershey or University Park can apply for summer internships through the Medical Student Research Program .
- Open positions will be posted through the Penn State careers website .
- Complete application for current faculty
Scholars in the training program will participate in the following:
- Scholars will be matched with a faculty mentor to work on a TRS-related project. Scholars will develop an individual develop plan (IDP) to identify learning objectives and goals for the project. In addition, scholars will complete annual mentoring evaluations.
- Required coursework in tobacco regulatory science
- Optional coursework in grant writing (PHS 510) or secondary data analysis (PHS 507)
- Participate in Penn State TCORS monthly seminars
- Participate in Penn State TCORS writing group
- Participate in CASEL journal club
- Participate in cross-training events with scholars from other TCORS
- Attend/present at annual TRS conference in October in Bethesda, Md. (pre- and postdoctoral scholars only)
- Develop one presentation on area of expertise to be added to the shared library on the TRS Knowledge Center (pre- and postdoctoral scholars only)
Meet our current and past TCORS scholars
Pilot Grant Program
The Penn State TCORS Career Enhancement Core will offer two types of pilot award opportunities.
Internal Awards – for up to $50,000—to support rigorous and feasible TRS research proposals from postdoctoral fellows and new or early-career faculty that fit within or are complementary to the Penn State TCORS theme
Collaborative Awards – for up to $50,000 – to support multidisciplinary projects among faculty investigators, with special consideration for studies proposing collaboration between two or more TCORS or emerging issues responsive to the Center for Rapid Surveillance of Tobacco (CRST).
Pilots are expected to be completed in 2 years. All proposals must identify a TCORS faculty mentor to provide guidance on translation to tobacco regulation and to facilitate successful completion.
- Center history
The Penn State Center for Research on Tobacco and Health originally began in 2013 when investigators at Penn State (PIs: Joshua Muscat and Jonathan Foulds) were awarded one of 14 Tobacco Centers of Regulatory Science (TCORS), a five-year, $20 million center grant, from the U.S. Food and Drug Administration and the National Institutes of Health. The general purpose of the TCORS grants are to support scientific research to inform the regulation of tobacco products. The overarching goal of the Penn State TCORS was to understand the health impact of tobacco-harm reduction policies in vulnerable (e.g. low socioeconomic status, mental disorders) and minority populations.
The TCORS 2013 program included three separate projects:
- Switching to progressively reduced nicotine content cigarettes in smokers with lower socioeconomic status (PIs: Joshua Muscat and Kimberly Horn, George Washington University)
- Reduced nicotine cigarettes in smokers with mood and anxiety disorders (PIs: Jonathan Foulds and Eden Evins, Harvard University)
- Switching to reduced oxidant or nicotine content cigarettes in smokers (PI: John Richie)
In 2023, the Center for Research on Tobacco and Health was awarded one of seven TCORS grants (PIs: Joshua Muscat and Jonathan Foulds), which aims to better understand how physical design and chemical constituents affect the toxicity and addictiveness of nicotine and tobacco products. The TCORS 2023 program will draw on the expertise of many researchers at Penn State including biochemists, statisticians, clinical psychologists, health behaviorists and epidemiologists.
The TCORS 2023 program includes three separate projects:
- Translational Studies on Temperature and Solvent Effects on Electronic Cigarette-Derived Oxidants (PIs: Zachary Bitzer and Thomas Spratt)
- Oxidative Stress and Harmful Constituent Levels Associated with Little Cigars (PI: Joshua Muscat)
- Randomized Placebo-controlled Trial of Nicotine Pouches in Smokers (PIs: Jonathan Foulds and Jason Robinson, University of Texas MD Anderson)
A component of each of the TCORS grants is to incorporate training and funding opportunities for early career, non-tenured scientists interested in pursuing tobacco regulatory science research. Scholars in the TCORS 2013 program completed a series of courses on tobacco regulation, the epidemiology of smoking and biomarkers, and participated in networking events with scholars from other TCORS institutions. The program also supported several postdoctoral scholars who have now moved onto to scientific careers in FDA’s Center for Tobacco Products or as tenure-track professors.
Additionally, the TCORS 2013 program provided pilot funding to 15 Penn State investigators. Projects funded ranged from studies evaluating the impact of electronic cigarette use among HIV positive smokers to evaluating free radical production from charcoal filters.
The newly funded TCORS will again announce pilot award opportunities. Openings for pre-doctoral and post-doctoral positions will also be posted. Both of these mechanisms will advance the careers of upcoming and early stage researchers who are interested in pursuing tobacco regulatory science.
Finally, the Penn State Center for Research on Tobacco and Health is designed to facilitate and coordinate not only the goals and accomplishments of the TCORS grants, but also all research on nicotine and tobacco conducted by Penn State faculty. The goal of the Center is to produce synergy and create collaborations between interdisciplinary researchers who are interested in understanding addiction and reducing the health effects of nicotine and tobacco products.
Nicotine Dependence Index
The Penn State Nicotine Dependence Index was developed by Dr. Jonathan Foulds in 2011.
This 10-item scale (with scores ranging from 0 to 20) was developed to measure nicotine dependence across all nicotine product types, and an adapted version was the first dependence measure designed to evaluate electronic cigarette dependence.
The index is available for use by clinicians and researchers at other institutions using the proper citation.
MRI Electronic Aerosol Delivery System (MEADS)
The MRI Electronic Aerosol Delivery System was developed through a collaboration between the Center for Research on Tobacco and Health, the Center for NMR Research and University Park.
The device works in coordination with an olfactometer to deliver up to four e-cigarette aerosols for functional MRI experiments.
With questions on this device, contact Dr. Andrea Hobkirk or Dr. Zachary Bitzer.
See protocol paper in Substance Abuse: Research and Treatment
Laboratory space for the Center for Research on Tobacco and Health is available on the third floor of Penn State Cancer Institute.

The MRI laboratory is part of the Center for NMR Research at Penn State College of Medicine.

Penn State is also home to this human smoking and addiction laboratory space.

Penn State Center for Research on Tobacco and Health also makes use of this smoking health and behavior laboratory at Penn State University Park.
- Current research funding
- Publications
- In the news
Latest news on tobacco, nicotine, vaping and smoking
Study reveals lower risk of atrial fibrillation after quitting smoking
- Download PDF Copy
Quitting cigarettes can significantly lower a person's risk of atrial fibrillation (AFib) compared to those who continue to smoke, according to a study published today in JACC: Clinical Electrophysiology . The findings show that the benefits of quitting start right away, suggesting that it is possible to reverse the risk of negative health outcomes.
The findings provide a compelling new reason to show current smokers that it's not too late to quit and that having smoked in the past doesn't mean you're 'destined' to develop AFib. Even for the current and longtime smoker, AFib can still be avoided." Gregory Marcus, MD, MAS, senior author, cardiologist at the University of California, San Francisco
Smoking is greatly associated with an increased risk of AFib, an irregular and often rapid heart rhythm. It has potentially serious health consequences and is linked with a significant risk of stroke, heart failure and overall mortality. Rates of AFib are rising, creating a need to identify lifestyle changes that can reduce risk.
"There's strong evidence that smoking increases the risk of AFib, but the benefits of quitting smoking have been less certain," Marcus said. "We wanted to determine whether quitting smoking could lower a person's risk of developing AFib or if the risk would stay the same."
The team analyzed UK Biobank data on more than 146,700 current and former smokers. Participants' smoking habits and health outcomes were tracked for around 12 years.
They found that former smokers had around 13% lower risk of AFib than people who were still smoking. Surprisingly, researchers also found that those who quit smoking during the study had an 18% lower risk of AFib than people who smoke, showing a significantly lower risk than former smokers.
Related Stories
- Best ways to quit smoking: E-cigs, medications, and counseling proven effective in new Cochrane analysis
- Flavored e-cigarettes cut smoking rates and toxic exposure in high-risk groups
- Research shows free vapes in emergency rooms aid smoking cessation
"This is likely a testament to the potency of reducing atrial fibrillation risk pretty shortly after quitting," Marcus said.
Previous research that looked at the connection between smoking and AFib was observational, making it difficult to prove a causal relationship.
"While the current study is also observational, our findings lend credence to the idea that smoking may truly cause AFib," Marcus said.
Future research could focus on explaining the mechanisms underlying the relationship between smoking and AFib, potentially identifying new therapeutic targets to prevent and treat it.
Study limitations include the possibility of recall bias in self-reported smoking status, the variability of the number of completed serial lifestyle questionnaires, and unmeasured confounding that may have contributed to the results, such as participant lifestyle or access to support in preventative health.
American College of Cardiology
Posted in: Medical Research News | Medical Condition News
Tags: Atrial Fibrillation , Cardiology , Cardiovascular Disease , Education , Electrophysiology , Heart , Heart Failure , Imaging , Mortality , Research , Smoking , Stroke , UK Biobank
Suggested Reading

Cancel reply to comment
- Trending Stories
- Latest Interviews
- Top Health Articles

How can microdialysis benefit drug development
Ilona Vuist
In this interview, discover how Charles River uses the power of microdialysis for drug development as well as CNS therapeutics.

Global and Local Efforts to Take Action Against Hepatitis
Lindsey Hiebert and James Amugsi
In this interview, we explore global and local efforts to combat viral hepatitis with Lindsey Hiebert, Deputy Director of the Coalition for Global Hepatitis Elimination (CGHE), and James Amugsi, a Mandela Washington Fellow and Physician Assistant at Sandema Hospital in Ghana. Together, they provide valuable insights into the challenges, successes, and the importance of partnerships in the fight against hepatitis.

Addressing Important Cardiac Biology Questions with Shotgun Top-Down Proteomics
In this interview conducted at Pittcon 2024, we spoke to Professor John Yates about capturing cardiomyocyte cell-to-cell heterogeneity via shotgun top-down proteomics.

Latest News

Newsletters you may be interested in
Your AI Powered Scientific Assistant
Hi, I'm Azthena, you can trust me to find commercial scientific answers from News-Medical.net.
A few things you need to know before we start. Please read and accept to continue.
- Use of “Azthena” is subject to the terms and conditions of use as set out by OpenAI .
- Content provided on any AZoNetwork sites are subject to the site Terms & Conditions and Privacy Policy .
- Large Language Models can make mistakes. Consider checking important information.
Great. Ask your question.
Azthena may occasionally provide inaccurate responses. Read the full terms .
While we only use edited and approved content for Azthena answers, it may on occasions provide incorrect responses. Please confirm any data provided with the related suppliers or authors. We do not provide medical advice, if you search for medical information you must always consult a medical professional before acting on any information provided.
Your questions, but not your email details will be shared with OpenAI and retained for 30 days in accordance with their privacy principles.
Please do not ask questions that use sensitive or confidential information.
Read the full Terms & Conditions .
Provide Feedback

- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
September 9, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
Smoking before the age of 18 increases the risk of developing respiratory symptoms in your 20s, study finds
by European Respiratory Society

People who started smoking under the age of 18 are more likely to experience respiratory symptoms, such as wheezing and phlegm, in their 20s, according to research presented at the European Respiratory Society (ERS) Congress in Vienna, Austria.
The study also found that the majority of young smokers had taken up the habit before they turned 18, and that the more cigarettes they smoked overall, the higher the risk of respiratory symptoms.
Researchers say the study highlights the risks to children and teenagers from smoking , and shows how rapidly the effects of tobacco can be seen. This is important since, in Europe, an estimated 16.7% of males and 11.2% of females aged between 15 and 24 are daily smokers.
The research was presented by Dr. Linnea Hedman, associate professor of epidemiology and public health at Umeå University, Sweden.
Researchers recruited 3,430 eight-year-old children in northern Sweden and asked them to fill in questionnaires annually until they turned 19 and again when they reached the age of 28.
Overall, 22% said they were daily smokers at some point during the study. Of those who said they smoked, 29% started smoking when they were 15 or under, 35% started smoking when they were 16 or 17, and 35% started at 18 or older.
The researchers took into account other factors that can affect lung health, such as a family history of asthma or growing up in a home where others smoke. They found that smoking more cigarettes overall increased the risk of respiratory symptoms by the age of 28, with one 'packyear' increasing the risk by around 10% compared to non-smokers. A packyear is the equivalent of smoking one pack of 20 cigarettes per day for one year.
Starting smoking under the age of 18 increased the risk of respiratory symptoms by the age of 28 by around 80% compared to non-smokers. In people who took up smoking at 18 or later, the risk was around 50% higher than non-smokers.
The most common respiratory symptoms were wheezing, phlegm and coughing.
Dr. Hedman said, "In our study we found that smokers are very likely to have taken up the habit before they turned 18 and those who did start early were more likely to be suffering with breathing problems , especially wheezing and phlegm. These symptoms were also more common the more cigarettes people smoked.
"One explanation for our findings could be that children and teenagers who started smoking earlier continue to smoke for a longer time and therefore suffer with more symptoms. It could be that exposure to tobacco smoke at a young age increases the risk of respiratory symptoms because the lungs are still developing and more vulnerable to damage.
"This study shows that it does not necessarily take decades to develop respiratory symptoms from smoking; we can already see a significant association in young adulthood."
Dr. Hedman and her colleagues will continue to monitor the people taking part in the study. They are now measuring the participants' lung function to understand how exposure to tobacco smoke influences their respiratory health in the longer term.
Professor Des Cox is a member of the ERS Tobacco Control Committee and consultant in pediatric respiratory medicine at Children's Health Ireland, Crumlin, Dublin, Ireland and was not involved in the research.
He said, "Across Europe and the rest of the world, there are still a significant number of children and teenagers smoking cigarettes. We need regulations and support to help children and young people avoid or quit smoking.
"At the same time, we're starting to see more and more children and teenagers vaping. It's too early to know exactly what this is doing to their lungs. What we do know is that nicotine is highly addictive and the earlier you start, the longer you continue to use nicotine products.
"We want children and adults to breathe clean air. That's why the European Respiratory Society warns that all nicotine and tobacco products, including vapes and cigarettes, are highly addictive and harmful. We want the next generation to have a tobacco- and nicotine-free childhood."
Explore further
Feedback to editors

New insights could help prevent psychosis relapses in youth and young adults

New, rare type of small cell lung cancer identified

Can having a stroke change your sleep?

Discovery of a new tumor cell type in childhood cancer
2 hours ago

How the Parkinson's drug Levodopa causes psychiatric complications similar to drug abuse

Stress-induced events jumpstart sperm performance once the event has passed, research reveals

Cells that die during inflammation send wound-healing messages, study shows

A new type of RNA could enhance vaccines and cancer treatments

Study reveals how antibiotics contribute to inflammatory bowel disease risk
3 hours ago

Atrial fibrillation estimated to be three times more common than previously thought
Related stories.

Use of e-cigarettes plus tobacco cigarettes linked to higher risk of respiratory symptoms
Apr 23, 2021

Study shows second-hand vaping exposure very low compared to second-hand smoking
Jul 11, 2024

Smokers who start below age 20 become more addicted and find it difficult to quit, research suggests
Aug 25, 2023

Teenagers more likely to vape if their parents smoke
Sep 5, 2022

Study shows increases in smoking and vaping in Irish teens
Sep 20, 2021

'Social smokers' face disproportionate risk of death from lung disease and lung cancer
Sep 4, 2020
Recommended for you

Reductions seen in benzodiazepine dispensing when states relax medical, recreational cannabis access
4 hours ago

Wearable lung patch uses deep learning to detect asthma and COPD
5 hours ago

Study shows cardiovascular health benefits can begin shortly after quitting smoking

New biomarkers can help target treatment for chronic skin disease sarcoidosis

Scientists discover dual roles of antibodies in COVID-19 infections
Sep 10, 2024

Scientists discover novel orthonairovirus in man bitten by tick in China
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
- Create My Quit Plan
- How to Quit
- Smokefree App
- Smokefree Texting Programs
- Get Extra Help
- Getting Started
- Why You Should Quit
- Pick Your Path to Quit
- How to Stay Smokefree
- E-cigs, Menthol & Dip
- Nicotine Withdrawal
- Cravings & Triggers
- Handling Stress
- Manage Your Mood
- Slips & Relapses
- Slips Happen
- Tips for Slips
- Weight Gain & Appetite
- Get Ready to Quit Vaping
- Managing Your First Day Without Vaping
- Dealing With Vape Cravings
- Know Your Vaping Triggers
- Nicotine Withdrawal and Vaping
- Stress, Anxiety, and Vaping
- Vaping and Depression
- How to Support Your Quitter
- FAQs for Helping Someone Quit
Open the Search Form
- Tools & Tips
Join a Research Study
A research study tests or evaluates treatments—such as new or current medications, behavior treatments, medical equipment, clinical therapies, procedures, or programs—to determine if they are safe and effective.

Why Should I Participate?
If you are looking for a way to stop smoking, participating in a research study may be right for you. People in research studies can receive new treatments before they reach the public. You may also help other smokers by contributing to research that could lead to new treatment options in the future.
Who Conducts Research Studies?
There are countless smoking cessation research studies going on around the world to help determine the best, most effective ways to help people stop smoking and stay quit. A number of the studies being run in the United States are funded by the National Institutes of Health (NIH) and carried out by researchers outside of NIH, usually at universities or medical schools.
Where Can I Learn More About Research Studies?
To learn more about smoking research studies currently recruiting around the world, visit the clinicaltrials.gov database .
Studies Currently Recruiting
Multimodal neuroimaging genetic biomarkers of nicotine addiction severity.
Study Location: Baltimore, MD (Local Recruitment)
Quitting smoking is hard. Let us help you through it. If you are 18-60 years old and ready to quit smoking, we need you for a research study on nicotine dependence at the National Institute on Drug Abuse in Baltimore. The study’s treatment plan is customized to your individual needs and includes free nicotine replacement combined with one-on-one counseling. This is a program that offers a research/treatment combination.
- Earn up to $1690 for completing the study
- Receive compensation after each study visit
- Receive an MRI image of your brain on a t-shirt
- Evening and weekend study appointments available
We want you to succeed. Call today to see if you qualify at 1-866-START NOW or email at [email protected] .
Overcoming Nicotine Dependence to Enable Quitting (ON-DEQ Study)
Study Location: Chicago, IL
RUSH University Medical Center is conducting a research study to test the role of treatment components to help people increase their readiness to quit smoking. If you agree to participate in this study, you will be assigned at random to receive one of two types of counseling, which involves completing four weekly sessions with a study therapist. You may also be assigned to receive nicotine replacement therapy (NRT) sampling, containing both nicotine lozenges and patches. All study activities will be conducted by phone or online, and no in-person visits to RUSH University are required. In addition to treatment, you will be asked to complete eight online study assessments over the course of approximately eight months, and you will be paid up to $250 for completing all parts of the study.

Fact: The cilia in your lungs are one of the first things in your body to heal when you quit smoking.
If Plan A didn’t work, there are 25 other letters. Learn from your mistakes and try again.
It's a great day to start new goals or recommit to old ones.

Explore Quit Methods

Speak to an Expert

Free Resources for Quitting Smoking
Are you addicted to vaping.
Take our quiz to find out. You’ll also learn how vaping affects your life and what you can do about it.
- SYDNEY, NSW
- MELBOURNE, VIC
- HOBART, TAS
- BRISBANE, QLD
- ADELAIDE, SA
- CANBERRA, ACT
Vaping a gateway to smoking for Aussie teens, study shows

Social media influencers sway vaping attitudes

Send your stories to [email protected]
Auto news: Best 4WD and off-roaders coming to Australia in 2025.
Top Stories

Weighing Katie at school only would have made her sicker

Chance meeting on train paved way for 9/11 attacks

Trump gives himself '10 out of 10' in debate but suggests he doesn't want rematch

Couple finds someone else's ashes buried in their reserved cemetery plot
- ERS WEBSITE
- Respiratory Channel
- Who we are and what we do
- Contact ERS
- Leadership and committees
- Governance and transparency
- MEP Lung Health Group
- Tobacco control
- Environment and health
- EU policies and research
- Non-communicable diseases
- International Respiratory Coalition
- ERS membership
- Awards and Fellows
- Hall of fame
- Elections and open positions
- Assemblies and Groups
- ERS Respiratory Channel
- Disaster medicine resources
- Partner societies
- Conference of European Respiratory Societies (CERS)
- External events endorsement

- ERS Congress
- Registration
- Abstract and clinical cases
- Information for faculty, case submitters and abstract authors
- Venue, hotels and travel
- Practical Information A-Z – Congress 2024
- Continuing Medical Education (CME) credits
- Media Centre
- Contact information
- More past ERS Congresses
- ERS Satellites
- Lung Science Conference
- Respiratory Failure and Mechanical Ventilation Conference
- Sleep and Breathing
- Industry Channel
- View events calendar
- Research seminars
- Scientific workshops

- Airway diseases
- Pulmonary vascular diseases
- Sleep and breathing disorders
- Interstitial lung disease
- Respiratory critical care
- Thoracic oncology
- Paediatric respiratory diseases
- Respiratory infections
- Guidelines, statements and technical standards development programme
- Clinical Research Collaboration: application programme
- Research seminar application
- Fellowship programme
- Research Agency
- Pragmatic Trials Endorsement
- Ongoing Clinical Research Collaborations
- The ERS Translational Science Initiative
- Ongoing Task Forces
- Clinical practice guidelines methodology network
- All EU Projects

- Certified training programmes
- Learn online
- Faculty development modules
- HERMES examinations
- Medical education research
- Respiratory digests
- About all Fellowships
- Short Term Fellowships
- Long Term Fellowships
- RESPIRE Marie S. Curie
- Clinical Training
- CME and Accreditations
- Continuing Professional Development

- Publications
Home News Young vapers perform worse in exercise testing
Young vapers perform worse in exercise testing

8 September, 2024
Young people who vape perform worse than non-vapers in tests designed to measure their capacity for exercise, according to a study presented at the European Respiratory Society (ERS) Congress in Vienna, Austria [1]. The research also showed that the performance of young vapers was similar to that of young smokers.
The study adds to growing evidence that long-term use of vaping is harmful and challenges the idea that vaping could be a healthier alternative to smoking.
The research was presented by Dr Azmy Faisal, senior lecturer in cardiorespiratory physiology in the department of sport and exercise sciences at Manchester Metropolitan University, UK. He said: “Previous research has shown that vaping is linked to lung inflammation and damage, and harmful changes to the blood vessels. Although, some research suggests that vaping could be used to cut back or quit smoking, we don’t yet know what longer-term vaping use does to our bodies.”
The study included 60 people in their 20s who all had normal lung function according to spirometry testing. Twenty were non-smokers and non-vapers, 20 had been vaping for at least two years and 20 had been smoking for at least two years.
Each person took part in an incremental exercise test on a static bike. This is the gold-standard for testing physical ability and how well a person copes with exercise, looking at their heart, lungs, and muscles’ responses at harder and harder levels until they reach their maximum. They were also given blood tests and an ultrasound scan to analyse how well their arteries were functioning.
On average, the group of young vapers had lower ‘peak exercise capacity’ (186 watts) than the group who did not vape or smoke (226 watts) but similar capacity to the group of smokers (182 watts). This is a measure of the maximum amount of physical exertion that a person can achieve. At peak exercise, vapers and smokers were also less able to consume oxygen on average (2.7 litres per minute and 2.6 litres per minute) compared to the non-smoking non-vaping groups (3 litres per minute).
Both vapers and smokers showed signs that their blood vessels were not working as well as the non-smoking and non-vaping group, according to the blood tests and ultrasound scans. The smokers and the vapers were more out of breath, experienced intense leg fatigue and had higher levels of lactate in their blood, a sign of muscle fatigue, even before they reached their maximum level of exercise.
Dr Faisal said: “In this study, we looked at a group of young people with no apparent signs of lung damage. Among the people who had been vaping or smoking for at least two years, we saw important differences in how well they coped with exercise. The smokers and the vapers had measurably excess breathing while using the exercise bikes. They found it harder to breath, their muscles became more fatigued, and they were less fit overall. In this regard, our research indicated that vaping is no better than smoking.”
Dr Filippos Filippidis is Chair of the ERS Tobacco Control Committee, a reader in public health at Imperial College London and was not involved in the research. He said: “Vapes are being sold cheaply and in a variety of flavours to appeal to young people. As a result, we’re seeing more and more young people take up the habit without knowing what the long-term consequences could be to their health.
“Although it’s always a challenge to know if the associations we find in these studies are causal or a result of some other systematic differences between groups, people who vape need to be aware that using these products could make them less fit and able to take part in exercise. Doctors and policymakers also need to know about the risks of vaping, and we should be doing all we can to support children and young people to avoid or quit vaping.”
[1] Abstract no: OA1954 “Detrimental effects of electronic cigarettes on vascular function and ventilatory efficiency during exercise”, by Azmy Faisal et al ; Presented in session, “Exercise testing: what’s new in pulmonary physiology?” at 15:45–17:00 CEST on Sunday 8 September 2024. [ https://live.ersnet.org/programme/session/92866 ]
Privacy Overview
Thanks for visiting! GoodRx is not available outside of the United States. If you are trying to access this site from the United States and believe you have received this message in error, please reach out to [email protected] and let us know.

- News Releases
New research shows regular mobile phone use can increase the risk of cardiovascular diseases, especially in smokers and people with diabetes
A new study in the Canadian Journal of Cardiology investigates the association between mobile phone use, risk of heart diseases, and modifiable lifestyle factors
A new study in the Canadian Journal of Cardiology has found that regular mobile phone use was positively associated with incident cardiovascular diseases risk, especially in current smokers and individuals with diabetes.
Credit: Canadian Journal of Cardiology
Philadelphia, September 4, 2024 – A new study has found that regular mobile phone use was positively associated with incident cardiovascular diseases risk, especially in current smokers and individuals with diabetes. In addition, this association was partly attributed to poor sleep, psychological distress, and neuroticism. The article in the Canadian Journal of Cardiology , published by Elsevier, details the results of this large-scale prospective cohort study.
Yanjun Zhang, MD, Division of Nephrology, Nanfang Hospital, Southern Medical University, Guangzhou, China, explains, "Mobile phone use is a ubiquitous exposure in modern society, so exploring its impact on health has significant public health value. Radio-frequency electromagnetic fields (RF-EMF) emitted by mobile phones cause dysregulation of the hypothalamic-pituitary-adrenal axis, inflammatory responses, and oxidative stress, and are therefore expected to affect a variety of organs such as the heart and blood vessels. However, whether mobile phone use is associated with the risk of cardiovascular diseases remains uncertain."
Co-investigator Ziliang Ye, MD, Division of Nephrology, Nanfang Hospital, Southern Medical University, Guangzhou, China, adds, "We aimed to assess the prospective association of regular mobile phone use with incident cardiovascular diseases and explore the mediating effects of sleep and mental health. We found that compared with non-regular mobile phone users, regular mobile phone users had a significantly higher risk of incident cardiovascular diseases."
The study included 444,027 individuals from the UK Biobank without a history of cardiovascular diseases who self-reported on the frequency of their mobile phone use from 2006 to 2010. Regular mobile phone use was defined as at least one call per week. Using linked hospital and mortality records, the composite outcome of incident stroke, coronary heart disease, atrial fibrillation, and heart failure was ascertained over a median followup time of 12.3 years. Researchers also investigated the role of sleep patterns, psychological distress, and neuroticism.
Co-investigator Xianhui Qin, MD, Division of Nephrology, Nanfang Hospital, Southern Medical University, Guangzhou, China, notes, "We found that sleep patterns, psychological distress, and neuroticism may be potential mechanisms of the association between mobile phone use and cardiovascular diseases. A poor sleep pattern and poor mental health may adversely affect the development of cardiovascular diseases through disrupted circadian rhythm, endocrine and metabolic disruption, and increased inflammation. In addition, chronic exposure to RF-EMF radiation emitted from mobile phones could lead to oxidative stress and inflammatory response. Therefore, RF-EMF radiation exposure from mobile phones in combination with smoking and diabetes may have a synergistic effect in increasing cardiovascular diseases risk."
An accompanying editorial contextualizes the findings of the study. Given that the recruitment window of this study (2006-2010) occurred before the widespread use of modern smartphones, which are now more commonly used for other activities (e.g., entertainment, text messaging/email, social networking, etc.), the generalizability and current relevance of these findings require careful consideration.
Co-author of the editorial Nicholas Grubic, MSc, Dalla Lana School of Public Health, University of Toronto, ON, Canada, concludes, " While the current study suggests that using a mobile phone may moderately increase the risk of developing cardiovascular diseases, more conclusive evidence with valid measurements of mobile phone use is needed before this association becomes a concern for the general public. Maintaining responsible mobile phone habits should be a valuable component of an all-encompassing approach to supporting cardiovascular health. Before diving into hours of mindless ’doom-scrolling’ on your smartphone today, consider redirecting this time toward a more heart-healthy activity."
Canadian Journal of Cardiology
10.1016/j.cjca.2024.06.006
Method of Research
Data/statistical analysis
Subject of Research
Article title.
Regular Mobile Phone Use and Incident Cardiovascular Diseases: Mediating Effects of Sleep Patterns, Psychological Distress, and Neuroticism
Article Publication Date
Disclaimer: AAAS and EurekAlert! are not responsible for the accuracy of news releases posted to EurekAlert! by contributing institutions or for the use of any information through the EurekAlert system.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Family Med Prim Care
- v.10(3); 2021 Mar
A qualitative study on attitude towards smoking, quitting and tobacco control policies among current smokers of different socio-economic status
Lalitha rani chellappa.
1 Department of Public Health Dentistry, Saveetha Dental College, Saveetha Institute of Management and Technical Sciences, Saveetha University, No. 162, Poonamallee High Road, Chennai, Tamil Nadu, India
Arthi Balasubramaniam
Meignana arumugham indiran, pradeep kumar rathinavelu, introduction:.
Tobacco consumed as smoke and smokeless forms is an important preventable public health issue projected to be the single largest cause of mortality worldwide. The aim of the study was to qualitatively assess the attitudes towards smoking, quitting and tobacco control policies among current smokers of different socio-economic status.
Materials and Methods:
An in-depth interview for 10 current smokers and a focus group discussion comprising of 10 current smokers was conducted with a guide and moderator which was audio recorded. About 6, 8 and 6 subjects from white collar, blue collar, and black collar employee status participated in the study. Their tobacco consumption and dependence using the Fagerstrom Test for Nicotine Dependence scale (FTNDS) was assessed.
About 50% of the participants had low; 30% had moderate and 20% had high nicotine dependency. Most of the participants started smoking by peer influence and continued as it made them to socialize. Relapses during their quit attempt was mainly due to work stress. Participants heard about the control of tobacco act but were unsure of the features in it. They perceived that no changes will happen if government bans production and selling of tobacco products. Also anti-tobacco commercials in social media will have no use. Nicotine replacement therapy may help in quitting the habit.
Conclusion:
The study concluded that people in low socio-economic status had high nicotine dependency with inadequate knowledge on tobacco control policies. They strongly believe that an individual's self-restrain only can succeed him in quitting the habit.
Introduction
Tobacco remains as a single largest cause for heart diseases and stroke in India, with more than one million deaths/year.[ 1 ] India faces an enormous economic burden for treating tobacco-related diseases amounted to $907 and $285 million for smoke and smokeless tobacco respectively.[ 2 ] Control and prevention of tobacco use becomes a major public health issue in limiting morbidity and mortality.[ 3 ] The prevalence of adult current smokers and smokeless tobacco users is 24.3% and 25.9%, respectively. With increasing tobacco control measures (surveillance and monitoring, tobacco control policy, legislation, capacity building) by the Government of India, still prevention of smoking remains a major challenge.[ 4 ] Although the prevalence of tobacco users has been decreasing over last two decades, about 19% of adult males and 2% of adult females continue using tobacco currently. Evidence says that 55.4% and 49.6% of smoke and smokeless tobacco users planned to or were thinking about quitting.[ 5 ] However only <2% tobacco users have made an attempt to quit using mCessation program – Quit Tobacco For Life.[ 6 ] Though use of tobacco among the adults dropped from 35% in 2009–10 to 29% in 2016–17 still a high economic burden is posed on India.[ 7 ]
Studies have demonstrated that a brief physician-delivered intervention (as brief as three minutes) using cognitive behavioural therapy (CBT) for smoking cessation in primary care setting significantly increases patients' smoking cessation rates.[ 8 ] Smoking cessation produces immediate and substantial health benefits.[ 9 ] The nicotine replacement medications and psychotic drugs have produced reasonable results in smoking cessation among high tobacco dependence individuals.[ 10 ] Thus there is a need for population-based interventions to complement individual-based behavioural or pharmacological interventions, capacity building for smoking cessation and treatment of tobacco dependence.[ 11 ] Social support for quitting, training of health professionals and integration of smoking cessation in other health programmes are essential for successful implementation of tobacco cessation programmes.[ 12 ] Recognizing the importance of tobacco cessation, there are 19 tobacco cessation clinics (TCCs) in India with the support of the World Health Organization.[ 13 ]
The Quit Tobacco International (QTI) has embarked on a project of incorporating tobacco cessation intervention in the undergraduate medical curriculum in two countries: India and Indonesia. As part of this project in India, 15 course modules were developed, piloted, implemented and evaluated in various departments of five medical colleges in Kerala and Karnataka States.[ 14 ]
Recent study suggested that even after being diagnosed with Head and Neck Cancer, one third of the study population continued to use tobacco.[ 15 ] Thus, it becomes an integral part of health professionals to provide a structured approach to initiate smoking cessation, manage withdrawal symptoms, and provide long-term support.[ 16 ] However, these cessation programs are usually customised according to individuals. This necessitates an in-depth understanding of the perception towards smoking and quitting in bringing out a targeted behavioural change.
The aim of the study was to qualitatively assess the attitudes towards smoking, quitting and tobacco control policies among current smokers of different socio-economic status attending a private dental college in Chennai.
Materials and Methods
Qualitative in-depth interviews and focus group discussions were conducted among current smokers visiting a private dental college in Chennai, Tamil Nadu. Ethical clearance was obtained from Institutional ethics committee, Saveetha University with the number SRB/SDC/PHD-1802/19/03. Approval obtained on 19/4/2019. The study population included white collar, blue collar, and black collar employees according to Friedrich in 2013.[ 17 ] A white-collar worker is a salaried professional, typically referring to general office workers and management. Blue-collar worker is a member of the working class who performs manual labour and either earns an hourly wage or is paid piece rate for the amount of work done. Black collar worker is a manual labourer in industries.
The study included current tobacco users, using tobacco for more than a year and aged 18 years and above. Former smokers and those who were not willing to participate in the study were excluded. The snowballing sampling method was used to recruit the study participants. Written informed consent was obtained from the study participants and the anonymity of the participants was maintained. The study was conducted during December 2019 in the department of Public Health Dentistry in a private room. The participants had varying levels of motivation to quit in the future. Interview was carried out until new responses or new ideas were generated. A baseline data on tobacco consumption, dependence was assessed using the Fagerstrom Test for Nicotine Dependence scale (FTNDS).
In depth interview
The study included an initial in-depth interview for 10 participants with 3 from black and white collar group and 4 participants from blue collar group. In-depth interview was conducted by a moderator along with an assistant. An interview guide was formulated so that we could probe into various aspects of smoking behaviour. The information's given by the participants were audio-recorded. The interview lasted 30 – 45 minutes for each participant.
The areas of discussion included reasons to start smoking and to continue, their perception as smokers, attitude towards non-smokers and their knowledge regarding health effects of smoking. Further probing was done to obtain details regarding their quit attempts and anti- health warnings on multimedia such as television, newspaper, or the cigarettes packets. The last part of the discussion included their knowledge and attitude towards nicotine replacement therapy (NRT) and tobacco control policies in the country.
Focus group discussion
A focus group discussion was conducted comprising 10 current smokers. The participants involved in the in-depth interview were not included for the focus group discussion. About 3 participants from black collar, 4 from blue collar and 3 from white collar group participated. Like in-depth interview, there was one moderator and one assistant. The discussion lasted for one hour and was audio-recorded. The moderator prompted the topics and the discussion continued. The areas of discussion included knowledge and attitude about cigarettes and other tobacco products act (COTPA), attitude about the situation what will happen if India closes the production of tobacco products. The discussion was healthy and each individual participated in briefing their perception.
Data analysis was done in accordance with thematic framework analysis to allow themes to be generated from the data collected. The audio recordings were transcribed to their verbatim format. The recordings were read and familiarised multiple times to generate themes. The focus group guide helped to sort the emerging keys points and the new themes to be segregated according to the responses. Initial analysis was undertaken manually, and the responses from each participant were identified and charted under the respective key points. Finally, interpretative analysis was done to group together similar points and to identify recurrent themes which enabled the various aspects of smoking behaviour among the participants of the three groups.
Among the 20 participants, 6 were white collar, 8 were in blue collar and 6 were black collar employees. About 50% had low nicotine dependency; 30% had medium nicotine dependency and 20% had high nicotine dependency. Low dependency was seen among 40% and 20% of white and black collar employees respectively. Medium dependency was seen among 60% and 33.33% of white and blue collar employees. However, high nicotine dependency was observed among 80% of black collar and 66.67% of blue collar employees. The responses generated after the focus group discussion were segregated and the following themes were produced.
Reasons for start of smoking
Most of them started smoking at the age of 18 years. The main reason to start smoking was due to the influence of peers and friends. The reason was found similar in black and blue- collar employees while white collar employees had a different perception
- One of the black collar employees said “I saw my friends smoking, was curious to know what it is about and how it would feel”
- One of the blue-collar employee said “all my friends in my gang were using it and they asked me to use. I wanted to be included too”
- White collar employee said “in college, only when a guy smokes, he was considered matured, macho and can impress girl classmates”
Reasons to continue smoking
All the participants considered smoking as a stress buster and a major way to socialise. They could divert their mind from what was troubling them.
- “Whenever I have tension I want to smoke and relax. It gives relaxation and I would forget all the tension in association with drinking” - Black collar employee
- “It's a good pass time and to socialize with friends in tea shop” - Blue collar employee
- We received another dimension for the reason to continue from a white - collar employee.
- “I have smoking zone in my office and major decisions were made here. Also I get chances to interact with the higher officials” - white collar employee.
Knowledge regarding health effects and COTPA
When asked about the harmful effects of tobacco on health, all the three groups said they are aware of the ill effects of tobacco and it affects lungs. White and blue-collar employees learned from books and movies, black collar employees learned from movies and advertisements. And some of the participants have had relatives who had suffered of health problems due to constant tobacco use. They were not aware of the COTPA act and its regulations, however watched anti-tobacco advertisements and heard from people that smoking in public is prohibited. They all never smoke in front of women and children but do smoke in public. Their usual place is the local tea shop where women and children won't be there.
Aspects related to quitting attempts
- Everyone has attempted to quit tobacco. “whenever I feel financially low, I try to quit but relapsed because of tension”–blue collar employee
- One of the blue-collar employees said “I want to quit when I get married and start a family”.
- Stress was the main reason for relapse. One of the white-collar employees said that “I tried to quit for a month but I relapsed due to work pressure though had sufficient knowledge on ill-effects”
What will happen if tobacco is stopped manufacturing
We explained about Indian Tobacco Company (ITC) and its share in producing tobacco in the country. And we questioned what will happen if the country stops production and selling tobacco products
- The black collar employees were so lethargic about the question and said its hypothetical “We can only talk about but the government will never stop manufacturing cigarettes”
- “When government bans the cigarettes, people will go for other addictions of cheaper tobacco forms” – Blue collar employee
- The white-collar employees said that “high dependent people may go for other addiction but people in officer ranks may try to quit”
Anti - tobacco commercials
We asked about the anti-tobacco commercials which are shown on television, theatres and on the tobacco packets.
- The black collar employees were aware of the commercials and uncertain of the purpose of those commercials as they are run by the same government and companies which are selling them.
- One of the blue-collar employee said “It doesn't affect me”
- The white-collar employees said they feel guilty inside but -they couldn't quit it. One of the white-collar employee said “I convince myself that I know the limits of tobacco that will cause ill effects and I will stay in my limits”
Nicotine replacement therapy
We shared some knowledge about nicotine and its effects and how nicotine replacement therapy helps in quitting tobacco.
- “We are not aware and can't afford for such things” -Black collar employee said
- One of the blue-collar employees had an experience with NRT and he said that “I have tried one of NRT gums once but I don't like the taste of it and it doesn't satisfy me as cigarettes do”
- White-collar employees were more aware of NRT and none of them had tried and they were ready to try with proper professional advice.
Summary of the responses given by the participants for different categories
| Area of discussion | Black collar employees | Blue collar employees | White collar employees |
|---|---|---|---|
| Reasons for start of smoking | I saw my friends smoking and I was curious to know what it is about and how it would feel | all my friends in my gang were using it | Only when a guy smokes he was considered matured in college |
| Reasons to continue smoking | Whenever I have tension I just want to smoke and relax | It’s a good pass time | I have smoking zone in my office and very good friendships were built based on that |
| Knowledge regarding health effect of smoking and COTPA | They all know about the health effects of tobacco that it affects the lungs and causes cancer. Some of them has had their relatives and known people who had suffered from cancer due to smoking. They all say they never smoke in front of women and children | ||
| Aspects related to quitting attempts | Whenever I feel financially low, I try to quit but then relapse because of tension | I want to quit when I get married and start a family | I tried to quit for a month but then when the work pressure is too much I relapse |
| What will happen if tobacco is stopped manufacturing? | We can only talk about this with a paper and pen but the govt will never stop manufacturing the cigarettes | When government bans the cigarettes, people will go for other addictions or some will use this and start cheaper tobacco forms | The high dependent people may go for other addiction but people who are in officer ranks like me may try to quit |
| Anti-tobacco commercials | I am aware of it but then why is the govt selling it? | It doesn’t affect me | Whenever I notice it, I scold myself but the I couldn’t quit |
People who are highly addicted inhale it deeply into the brain and get high instantly and exhale via nose. People who medium dependent will exhale via mouth. That’s a way u can identify how addicted they are
Qualitative research pivots in apprehending a research query as a humanistic or idealistic approach. Though quantitative approach is viewed as a reliable method which can be made objectively and propagated by other researchers, qualitative method helps to understand people's beliefs, experiences, behaviour, attitudes, and interactions.[ 18 ] Although once viewed as philosophically incongruent with experimental research, qualitative research is now being recognized for its ability to add a new dimension into interventional studies that cannot be obtained through measurement of variables alone.[ 19 ] Qualitative research gives voice to the participants in the study permitting them to share their experiences of effects of the drug of interest in a clinical trial. This can open our eyes to new aspects and help modify the design of the clinical trial.[ 20 ]
In the present study, peer pressure was the main reason the participants started smoking. A study by Sharma et al . in 2016, it was found that main reason to start smoking was due to the influence of peer groups and friends, while a few felt it created a high esteem among the others.[ 21 ] The reason to continue smoking and relapse in quit attempts in the present study was stress which was similar to statement in the previous studies.[ 22 , 23 , 24 , 25 ]
High nicotine dependency was seen among black and blue-collar employees. This proves the role of socioeconomic status and education in nicotine dependency. Previous research suggests that people in socioeconomically deprived neighbourhoods smoke more than those in affluent neighbourhoods, independently of individual-level socioeconomic status.[ 26 , 27 ]
Tobacco cessation in primary care
Qualitative study is all about connecting to the psychological aspect of the participants that can play a role in the intervention. Early detection, diagnosis and treatment are important to increase the awareness of the population. Primary health centre physicians and dentists are the first contact of medicine. Easy accessibility of the oral cavity to examine renders it an ideal target for improved screening practices. Due to the modest investments of time and cost required by screening exams, primary care physicians assume a frontline role in the battle against tobacco and oral cancer.[ 28 ]
Regarding the health sector, more investment in training of health professionals from primary care to psychology, biopsies, in addition to intersectoral and multidisciplinary actions are necessary.[ 29 ] Further training is required at both undergraduate and postgraduate levels to increase awareness of tobacco usage, its associated risk factors to strengthen primary care practitioners' abilities.[ 30 ]
Findings of the study show that people in low socio-economic status had high nicotine dependency with inadequate knowledge on tobacco control policies. There is a need for interdisciplinary approach to prevent tobacco use that involves various disciples of medicine, with the support of government and the broader community. Dentists are one of the professionals who can detect the smoking habit by examining the oral cavity. A public health dentist, often are the primary contact of health worker for many of the low socio - economic groups. It is important for us to understand the various interventions and aspects of the nicotine intoxication and assist in cessation of the habit.
In the present study, among the 20 people participated in-depth interview and focus group discussions, 30% were white collar, 40% were blue collar and 30% included black collar employees. The results showed that 50% of the participants had low nicotine dependency; 30% had medium nicotine dependency and 20% had high nicotine dependency. During the focus group discussion and in depth interviews, most of the participants stated that they started the habit due to peer pressure and they were aware about the ill effects of tobacco use. Most of the participants relapsed from their quitting due to family or work tension. During focus group discussion, one of the participants from white collar employees who have had previous unsuccessful attempt in quitting said that “people who are highly addicted inhales it deeply into the brain, gets high instantly and exhale via nose”. People with medium dependency will exhale through mouth. All the participants were unaware of tobacco control policies.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Conflicts of interest.
There are no conflicts of interest.

IMAGES
COMMENTS
A systematic review of about 50 epidemiological studies found that smoking modestly raised the risk for Alzheimer's but had no effect on the development ... research to better understand how risks are perceived and internalized by individuals and governments is needed to ensure that epidemiological studies on the consequences of smoking are ...
Health impact of smoking. Table Table1 1 lists the main causes of death from smoking. Tobacco smoking is estimated to lead to the premature death of approximately 6 million people worldwide and 96,000 in the UK each year (Action on Smoking and Health, 2016b; World Health Organization, 2013).A 'premature death from smoking' is defined as a death from a smoking-related disease in an ...
In the present study, current smoking is defined as the current use of any smoked tobacco product on a daily or occasional basis. Health outcomes were initially selected using the World Cancer Research Fund criteria for convincing or probable evidence as described in Murray et al. 186. The 36 health outcomes that were selected based on existing ...
The first large, prospective study of smoking and mortality involving both women and men was Cancer Prevention Study I (CPS I), initiated by the American Cancer Society (ACS) in 1959. 8,9 The ...
A growing body of research points to the effectiveness of tobacco control measures 10,11,12; however, ... as indicated in this study, implementing complete smoking bans (that is, all public places ...
Study participants, 55 years of age or older, were drawn from five large U.S. cohorts for which information on smoking was obtained at least once during the follow-up period (2000 to 2011).
Smoking is a major cause of premature death worldwide. 1-3 Despite substantial declines in the prevalence of smoking by adults, estimates based on extrapolation from studies in the 1980s suggest ...
The findings of Thomson et al 1 support the importance of lifetime exposure to smoking cigarettes in determining the level of health risk and reiterate that the benefits of successfully quitting smoking may accrue to all smokers, whatever their age. In the study, among participants who had ever smoked, 54% reported that they had already quit ...
Former smokers showed lower hazard ratios (1.3 in both women and men). Short-term cessation for fewer than 3 years was associated with a lower excess risk of 95% in women and 90% in men younger than 40 years of age, with notable beneficial associations also in women and men 40 to 49 years of age (81% and 61%, respectively) and 50 to 59 years of ...
All studies included in our otitis media model were conducted in never-smoker populations (or classified as such given the age of the studied population (Methods and Supplementary Information ...
Key Points. Question Is smoking still decreasing among US adults and do the trends vary by age, income, and race and ethnicity?. Findings In this cross-sectional study of 353 555 adults responding to the 2011 to 2022 National Health Interview Surveys, adults younger than 40 years had dramatic declines in smoking prevalence during the last decade, especially among those with higher incomes.
FDA supports science and research to help us better understand tobacco use and associated risks so that we can reduce the public health burden of tobacco in the United States. Research programs ...
In a study in the USA, compared with a population of smokers with no psychiatric diagnosis, subjects with anxiety, depression and phobia showed an approximately twofold higher prevalence of ...
Cutting-edge neuroimaging technologies have identified brain changes associated with nicotine dependence and smoking. Using functional magnetic resonance imaging (fMRI), scientists can visualize smokers' brains as they respond to cigarette-associated cues that can trigger craving and relapse. 231 Such research may lead to a biomarker for ...
In Study 1, the mean of current and former smokers' perceptions of absolute risk of lung cancer among smokers was 48% (i.e., 480.1 smokers out of 1,000 smokers would get lung cancer); the median was 50% (see columns 1 and 2 of Table 1). 10.3% of respondents perceived absolute risks between 0% and 5.0%, and the remaining respondents gave ...
About the Journal. Nicotine & Tobacco Research aims to provide a forum for empirical findings, critical reviews, and conceptual papers on the many aspects of nicotine and tobacco, including research from the biobehavioral, neurobiological, molecular biologic, epidemiological, prevention, and treatment arenas. Find out more here.
Terry published the final report January 11, 1964 - 50 years ago. It concluded that: "Cigarette smoking is a health hazard of sufficient importance in the United States to warrant appropriate remedial action.". That strong judgment fueled stop-smoking efforts across the United States.
Contact information. If you do not or cannot complete one of the interest forms but would like to speak to someone about the available tobacco studies, please call 713-792-2265. How I quit smoking and gained a new life. I was just 11 when I started smoking in the 1980s. Finding cigarettes was easy.
At least two studies have been performed to determine the role of oxidative stress in increasing leukocyte-endothelial interactions that precede the development of atherosclerosis in smokers. One study showed that a high intake of vitamin C by smokers significantly reduced the adhesiveness of their monocytes to endothelial cells . However, in a ...
Interested participants may also call 844-207-6392 for details. The Center for NMR Research is at 30 Long Lane in Hershey, Pa. The Clinical Research Center is a dedicated space on the fourth floor of Penn State Health Milton S. Hershey Medical Center. Study visits for people participating in smoking studies through the Center for Research on ...
Surprisingly, researchers also found that those who quit smoking during the study had an 18% lower risk of AFib than people who smoke, showing a significantly lower risk than former smokers.
The study also found that the majority of young smokers had taken up the habit before they turned 18, and that the more cigarettes they smoked overall, the higher the risk of respiratory symptoms.
The study's treatment plan is customized to your individual needs and includes free nicotine replacement combined with one-on-one counseling. This is a program that offers a research/treatment combination. Earn up to $1690 for completing the study. Receive compensation after each study visit. Receive an MRI image of your brain on a t-shirt.
The study draws on survey responses from more than 5100 teenagers collected in 2023, before Australia's tough new laws that effectively make vaping illegal without a prescription came into effect ...
The research also showed that the performance of young vapers was similar to that of young smokers. The study adds to growing evidence that long-term use of vaping is harmful and challenges the idea that vaping could be a healthier alternative to smoking. The research was presented by Dr Azmy Faisal, senior lecturer in cardiorespiratory ...
Studies suggest that smoking rates are also higher in people with substance use disorders and mental health issues [10-12]. Although smoking prevalence has declined overall across Canada, smoking rates vary across the country, with Prince Edward Island reporting the lowest (12%) and Newfoundland and Labrador reporting the highest (20%) rates .
What does the research say about semaglutide for smoking cessation? There's not a lot of research available on whether semaglutide can help people stop smoking. But there's some animal research in this area. In these studies, rats given oral semaglutide were less likely to seek out nicotine. They also didn't experience overeating from ...
Philadelphia, September 4, 2024 - A new study has found that regular mobile phone use was positively associated with incident cardiovascular diseases risk, especially in current smokers and ...
In the present study, peer pressure was the main reason the participants started smoking. A study by Sharma et al. in 2016, ... Previous research suggests that people in socioeconomically deprived neighbourhoods smoke more than those in affluent neighbourhoods, independently of individual-level socioeconomic status.[26,27]
Research shows vapers aged 12 are 29 times more likely to smoke. Australia is losing its world-leading status with a disturbing new trend among young people that has reversed years of good work.